Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
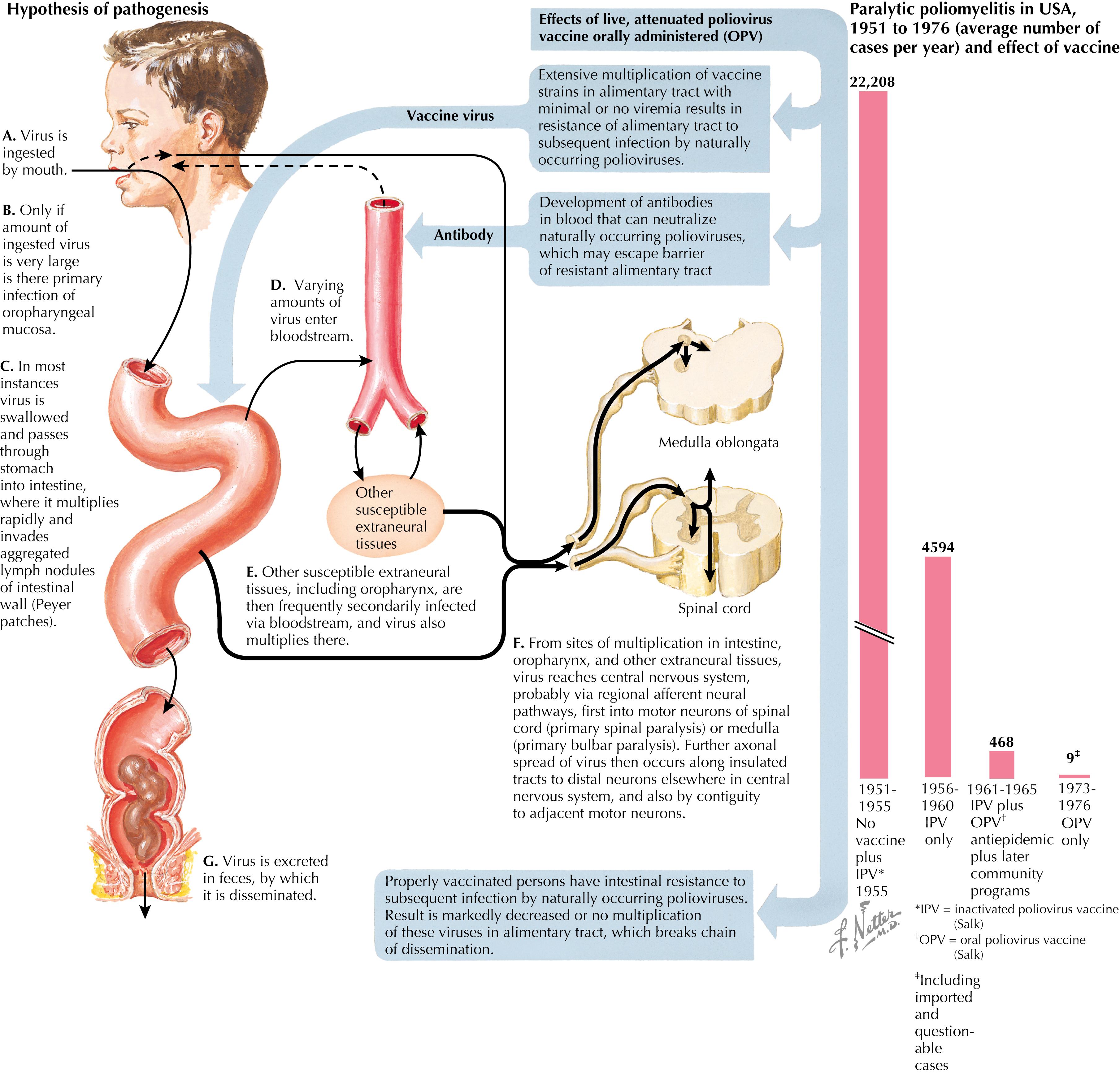
In the early 20th century, poliomyelitis was one of the most feared illnesses of humans, in part because it affected previously healthy individuals with little or no warning and could result in devastating paralysis. Although the disease was once endemic worldwide, with vaccines eradication has been achieved in all but two countries. In current times, acute flaccid paralysis (AFP) is associated with vaccine-derived poliovirus strains or other viral agents more commonly than wild-type polio virus. However, with disruption of proper sanitation or maintenance of vaccination within the population, outbreaks can quickly reemerge.
A 3-year-old male from Syria presents to the local health clinic for progressive leg weakness for 2 days. Yesterday, he collapsed after getting out of bed and has not been able to stand. His parents report a recent febrile illness with diarrhea that self-resolved. Prior to this illness, he appeared healthy. Due to recent unrest and violence in the region, the family relocated to a rural area where healthcare, including vaccines, is limited due to the civil war. His parents recall no vaccines administered in the past 2 years.
Exam revealed a thin child who appeared in pain but was without acute distress. Cranial nerves were intact, and he was controlling oral secretions with normal breathing. He was unable to move his left leg, and he only had 3/5 strength in his right leg. The lower extremity patellar and Achilles reflexes were 0/4 on the left and 2/4 on the right. He was transferred to a referral hospital for management. Stool polymerase chain reaction (PCR) ultimately confirmed poliomyelitis due to a circulating vaccine-derived poliovirus strain. After 6 months of physical therapy, he started to regain strength and function.
COMMENT: Oral polio vaccine (OPV) is used in mass vaccination campaigns worldwide because of ease in administration and fecal shedding of the vaccine viruses by vaccine recipients can promote herd immunity in the community. Rarely, the circulating vaccine-derived polioviruses (cVDPVs) cause paralytic polio.
Polioviruses are positive-sense, single-stranded ribonucleic acid (RNA) viruses that belong to the Enterovirus C species of the Picornaviridae family. They include three antigenically distinct serotypes (1, 2, and 3), with serotype 1 as the most common serotype leading to infection. The polioviruses were previously ubiquitous throughout the world and are highly infectious, spreading through contaminated fecal or respiratory secretions via the fecal-oral route. Humans are the only known natural hosts and reservoir. Although replication in other primates can occur, only humans are infected. Outbreaks were most common in summer and fall in temperate climates, whereas tropical climates have episodes year-round.
Poliomyelitis, often referred to as polio, was recognized by ancient Egyptians, as evidenced in hieroglyphics depicting people with deformed limbs. Throughout history, a majority of the infections were subclinical. Most of these infections occurred in infants and were attenuated by maternal antibodies, leading to subclinical disease but widespread immunity. With the improvement of sanitation in the United States, fewer infants were exposed to the virus and therefore not immune. This created a pool of susceptible individuals, specifically older children and adults, resulting in sporadic epidemics that occurred every few years, quickly increasing in frequency and size. The largest outbreak in the United States occurred in 1952, when nearly 58,000 cases of polio were diagnosed. In developing countries, polio remained endemic into the latter half of the 20th century. With improved sanitation in these regions, epidemics began to occur similar to the pattern observed in the turn-of-the-century United States.
The introduction of polio vaccines dramatically reduced the incidence of polio worldwide. The last case of naturally occurring polio in the United States was reported in 1979. The Western Hemisphere was certified free of wild-type poliovirus (WTPV) in 1994. In October 2019, the Polio Global Eradication Initiative announced that polio is on the verge of eradication, with only two countries (Pakistan and Afghanistan) reporting indigenous WTPV. Of the three serotypes of poliovirus, only serotype 1 remains endemic.
The OPV is a live-attenuated vaccine that has been used worldwide, but there is a risk in 1 in 2.5 million doses to develop vaccine-associated paralytic poliomyelitis (VAPP). The use of OPV also led to the development of cVDPVs, which have been the cause of numerous outbreaks of polio illnesses in parts of Africa, the Middle East, and Southeast Asia.
In the prevaccine era, virtually all infants were exposed to the polioviruses by the age of 6 months, although very few developed the paralytic disease. Risk factors for the infection progressing to paralytic disease include young age, pregnancy, antibody deficiency states, male gender (prepuberty), strenuous exercise, and preceding limb injury within 4 weeks of infection. In adults, women have an increased risk of infection but do not necessarily have an increased risk of paralysis.
Even in the postvaccine era, approximately 70% of infections are asymptomatic. Clinically inapparent infections are defined as isolation of a poliovirus from stool or throat with concomitant fourfold rise in antibody titers. Less than 1% of infections progress to the weakness and paralysis seen in paralytic poliomyelitis. The incubation period is 3 to 6 days; however, symptom onset varies depending on clinical presentation.
During the incubation period, the virus replicates in the lymphatic tissue, first in the tonsils and lymph nodes of the neck, then in the Peyer patches of the small intestine. After several days, a primary minor viremia occurs, with systemic spread of the poliovirus in the blood to muscle, fat, bone marrow, liver, and spleen ( Fig. 7.1 ). This period is typically asymptomatic, but up to 24% of patients have a mild illness with gastrointestinal symptoms or a respiratory influenza-like illness. These individuals will typically recover in 5 to 10 days, without the development of antibodies to neutralize the virus. In 1% of patients, a secondary major viremia occurs, and the poliovirus spreads to the central nervous system (CNS) and causes an aseptic meningitis. This presents with a severe headache and meningeal irritation but also has a full recovery in 5 to 10 days.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here