Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
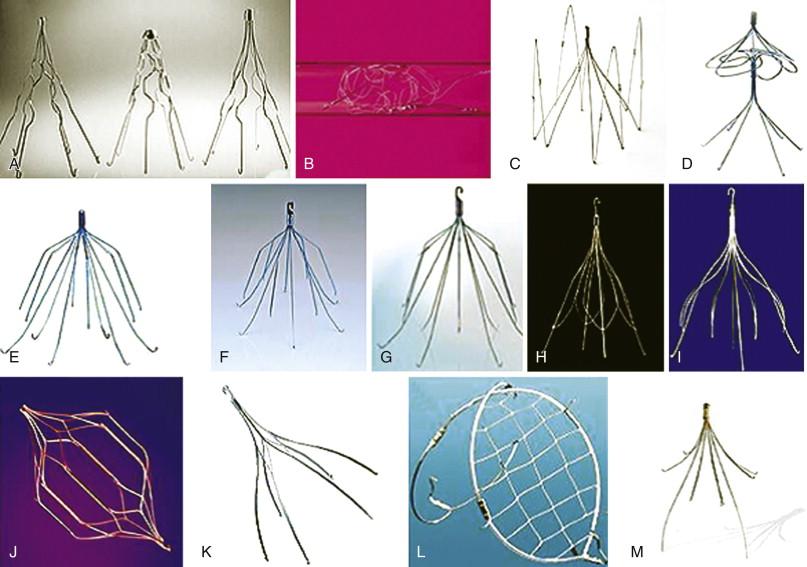
Vena cava interruption for prevention of pulmonary embolism (PE) was introduced in the 1950s and 1960s. Femoral vein and inferior vena cava (IVC) ligation, as well as partial interruption of the IVC using plastic clips, plication, and mechanical staplers, were explored but because of lower extremity venous congestion, vena cava occlusion, incomplete protection from pulmonary emboli, and the need for direct surgical exposure of the vena cava, these techniques were abandoned for less invasive options. The Mobin-Uddin umbrella filter, a silicone membrane with multiple holes to allow blood flow that could be delivered through a transvenous route, was introduced in 1967 but was associated with a high rate of vena cava thrombosis. In 1973 the Greenfield stainless-steel intravascular conical filter, which offered improved filtration without decreased flow, was developed and became the forerunner of all subsequent metallic filter designs. Although early filter devices required a large delivery catheter and were placed through open femoral vein exposure, improvements in device design and lower-profile delivery systems led to the development of permanent and retrievable percutaneously placed vena cava filters ( Table 54-1 and Fig. 54-1 ).
| Filter Device | Company | Material | Design | Access | Delivery Catheter Diameter (Fr) | Maximum Caval Diameter (mm) | Maximum Deployed Length (mm) | FDA-Approved Use |
|---|---|---|---|---|---|---|---|---|
| ALN optional filter | ALN | Stainless steel | Conical | Femoral/jugular/brachial | 7 | 28 | 55 | Optional |
| Option | Rex Medical Angiotech | Nitinol | Conical | Femoral/jugular | 5 | 30 | 55 | Optional |
| Eclipse | Bard Peripheral Vascular | Nitinol | Bilevel, conical | Femoral/jugular | Femoral 7 Jugular 10 |
28 | 47 | Optional |
| G2 X filter | Bard Peripheral Vascular | Nitinol | Bilevel, conical | Femoral/jugular | Femoral 7 Jugular 10 |
28 | 47 | Optional |
| G2 filter | Bard Peripheral Vascular | Nitinol | Bilevel, conical | Femoral/jugular | Femoral 7 Jugular 10 |
28 | 44 | Optional |
| Simon Nitinol filter | Bard Peripheral Vascular | Nitinol | Bilevel, conical | Femoral/jugular/brachial | 7 | 28 | 38 | Permanent |
| Meridian | Bard Peripheral Vascular | Nitinol | Bilevel, conical | Femoral/jugular | Femoral 8 Jugular 10 |
28 | 47 | Permanent or optional |
| Denali | Bard Peripheral Vascular | Nitinol | Bilevel, conical | Femoral/jugular | 8.4 | 28 | Permanent or optional | |
| Vena Tech LP filter | B. Braun/Vena Tech | Phynox | Conical | Femoral/jugular | 7 | 28 | 43 | Permanent |
| Vena Tech LGM filter | B. Braun/Vena Tech | Phynox | Conical | Femoral/jugular | 10 | 28 | 38 | Permanent |
| Stainless-steel Greenfield | Boston Scientific | Stainless steel | Conical | Femoral/jugular | 12 | 28 | 50 | Permanent |
| Titanium Greenfield | Boston Scientific | Titanium | Conical | Femoral/jugular | 12 | 28 | 50 | Permanent |
| Bird’s Nest | Cook Medical | Stainless steel | Variable | Femoral/jugular | 12 | 40 | 80 | Permanent |
| Celect | Cook Medical | Conichrome | Conical | Femoral/jugular | Femoral 8.5 Jugular 7 |
30 | 48 | Optional |
| Günther Tulip | Cook Medical | Conichrome | Conical | Femoral/jugular | Femoral 8.5 Jugular 7 |
30 | 50 | Optional |
| TrapEase | Cordis Corp. | Nitinol | Double basket | Femoral/jugular/brachial | 6 | 30 | 50 | Permanent |
| OPTEASE | Cordis Corp. | Nitinol | Double basket | Femoral/jugular/brachial | 6 | 30 | 54 | Optional |
| Crux Vena Cava Filter System | Crux Biomedical Inc. | Nitinol | Helical | Femoral/jugular | 9 | 17-28 | Depends on vena cava diameter | Permanent or optional |
| SafeFlo | Rafael Medical Technologies | Nitinol | Double-ring anchor with spiral filter element | Femoral/jugular | 6 | 27 | 60 | Permanent |
In the United States, deep vein thrombosis (DVT) occurs in approximately 1 per 1000 people each year. Nearly one third of patients with symptomatic untreated DVT present with PE. Anticoagulation is the treatment of choice for most cases of DVT, with evidence-based guidelines supporting the use of a vena cava filter when anticoagulation is not possible because of contraindications to anticoagulation or hemorrhagic complications, recurrent PE despite therapeutic anticoagulation, or an inability to achieve therapeutic anticoagulation.
Expanded indications have been based on clinical factors that place a patient at high risk for both PE and bleeding, prohibiting use of prophylactic anticoagulation. Likewise, relative indications for filter placement include poor compliance with anticoagulation, free-floating iliocaval thrombus, renal cell carcinoma with extension into the renal vein and vena cava, thrombolysis or thromboembolectomy of the iliofemoral veins or IVC, and risk of recurrent PE with preexisting pulmonary hypertension or limited cardiopulmonary reserve. Filter placement may also be considered after DVT in patients with cancer, burns, and pregnancy or for prophylaxis in multitrauma patients, including those with severe closed head injury (Glasgow Coma Scale score < 8), spinal cord injury, complex pelvic or multiple long-bone fractures, intraabdominal injury, pelvic or retroperitoneal hematoma, and ocular trauma. Contraindications to vena cava filter placement include chronic occlusion or significant compression of the vena cava or agenesis of the vena cava. The latter occurs when the right subcardinal vein fails to connect with the hepatic sinusoids during fetal development, which leads to infrahepatic interruption of the IVC segment with azygos continuation.
A review of the indications for filter placement and hemorrhagic risk should be conducted prior to filter placement. Based on the clinical scenario, either a permanent or a retrievable filter should be selected.
Central venous catheters that may be present at the proposed site of access or across the intended location for filter deployment should be removed.
Coagulopathy or other hematologic issues should be assessed. Discontinuation of anticoagulation before the procedure should be considered based on clinical indication and hemorrhagic risk profile.
Preprocedure review of duplex ultrasound or available computed tomography (CT) images should be performed to identify anatomic vena cava variants or other venous anomalies that could potentially alter the treatment plan. During filter placement, selective venography may also help to identify venous anomalies. In this regard accessory renal veins, retroaortic, and circumferential left renal vein anomalies (5%-7%) are the most common anatomic variation but do not affect filter position. Transposition of the vena cava to the left side with drainage into the left renal vein is rare (0.2%-0.5%) but necessitates accurate anatomic definition and could require a suprarenal filter. Duplication of the vena cava is also rare (0.2%-0.3%), with the right-sided IVC draining the right iliac vein and right renal vein, whereas the left-sided IVC drains the left iliac veins and joins the left renal vein where it crosses over into the right-sided vena cava. Undiagnosed duplication of the IVC may leave the duplicated vena cava unprotected against PE and would require either separate filters in each vena cava or a suprarenal filter, above the junction of the left renal vein and the right-sided vena cava. Agenesis of the vena cava is extremely rare, but when present, filter insertion should be avoided, although filter placement into an enlarged azygous segment has been described.
A preprocedure duplex ultrasound should be obtained to evaluate the presence of venous thrombosis at the intended percutaneous access site or extending into iliofemoral or vena cava. Jugular venous access may be needed if femoral vein access is not possible. Additional imaging should be performed just before positioning and deployment of a filter to assess whether there is thrombus in the vena cava. The presence of thrombus in the infrarenal IVC may necessitate suprarenal filter placement.
Ultrasound-guided percutaneous access is recommended to allow direct visualization of the access vein and real-time image guidance for the needle stick, as well as to avoid concomitant arterial injury.
The diameter of the IVC, including major and minor axes, should be measured either from venography, transabdominal duplex ultrasound, intravascular ultrasound (IVUS), or a preprocedure CT scan to assist in appropriate filter selection. Vena cava diameter measurements can vary depending on intravascular fluid status and respiratory variation. Vena cava geometry can also range from circular to elliptical. Both major and minor axes should be measured.
Accurate identification of both renal and common iliac veins is important before filter deployment. The tip of the filter should be positioned below the lowest renal vein after adequate clearance of the filter base from the iliac vein confluence.
An algorithm incorporating clinical indications, filter type, and preferred endovascular technique can be used to guide treatment ( Fig. 54-2 ).
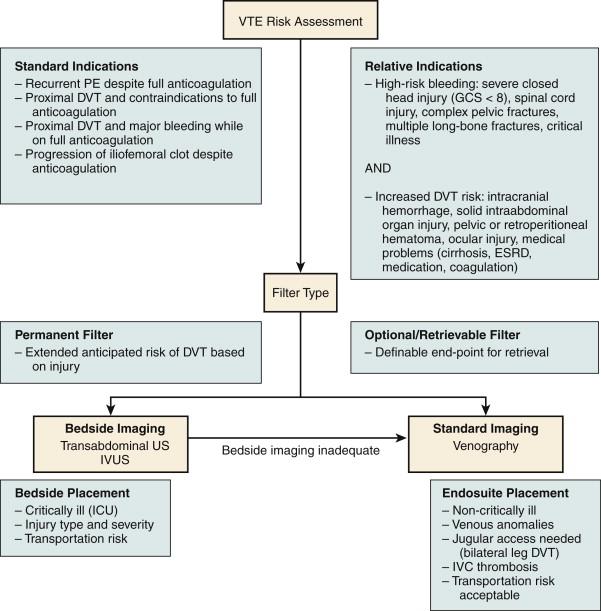
Vena cava anatomy. Before filter placement it is best to define the vena cava diameter, the location of the iliac vein confluence and renal veins, as well as the presence of vena cava and renal vein anomalies or thrombus in the vena cava.
Access site thrombosis. Ultrasonography-guided access can evaluate whether there is thrombus at the access site before puncture and also help to avoid concomitant arterial injury.
Limitations of imaging. Although the third lumbar vertebral body has been used as a landmark for filter deployment, bony lumbar vertebral anatomy alone is not adequate for proper filter placement as the renal veins and the iliac vein confluence may be found at this level in 5% to 10% of patients. Whether venography, transabdominal duplex ultrasound, or IVUS is used for placement, understanding the limitations of each modality is critical for accurate filter placement.
Filter deployment problems. Filter tilt, crossing of filter legs, entrapment of the filter device inside the filter delivery catheter, filter migration, and vena cava penetration can occur during filter deployment. A thorough understanding of catheter-based techniques, imaging, and specific filter delivery systems is required.
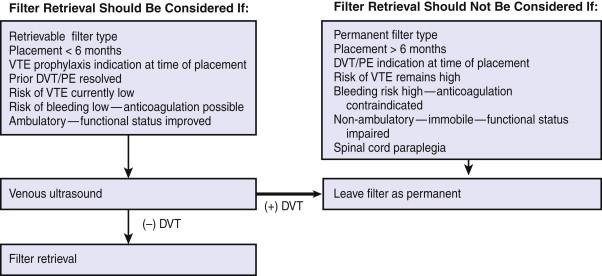
Permanent filters are designed to provide lifelong filtration, with features that allow maximal fixation to the vena cava intimal surface and promote tissue ingrowth. Optional or retrievable filters are similar to permanent filters but have additional features that limit tissue ingrowth to allow removal at a later interval. If removal is not indicated or desired, these filters can function as permanent filters ( Fig. 54-3 ). Current indications for filter retrieval include patients for whom the duration of risk for PE may be limited, particularly in young multitrauma or perinatal patients, as well as morbidly obese patients undergoing bariatric or orthopedic procedures.
Venography, with subsequent determination of the lowest renal vein and iliac vein confluence, assures appropriate filter position. In some instances further selective branch venography is required to delineate the anatomy if venous landmarks cannot be identified. Renal vein catheterization and imaging across the iliac confluence can aid in demonstrating aberrant anatomy, especially a duplicated caval system. A change of intended preoperative filter location may occur in up to 11% to 30% of patients after venography.
In immobilized or critically ill patients, bedside filter placement using transabdominal or IVUS may be preferred. Transabdominal ultrasound-guided filter placement is technically feasible in 86% to 88% of patients, with success rates of 98% when visualization is adequate. IVUS, which is not limited by body habitus, offers technical success rates of 96% to 99%.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here