Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The peripheral nervous system (PNS) is the direct extension of the central nervous system (CNS), and it is capable of consciously monitoring and reacting to primarily external stimuli. Dysfunction of this system can lead to an inability of patients to consciously interact with their environment or to receive signals that do not accurately represent their environment.
It can be broken down into two subsystems:
The autonomic nervous system (ANS), which is not regulated by conscious control and is involuntary.
The somatic nervous system, which contains afferent sensory nerves and efferent motor nerves (which are mostly voluntary) from the CNS.
The ANS generally helps maintain healthy homeostasis, influencing physiology independent of conscious awareness. The ANS receives information from the other body systems (the internal environment) and from the surroundings (the external environment) and automatically adjusts the activity of the sympathetic and parasympathetic nervous systems to match the overall needs of the body. The function of the ANS is critical to adapting to various stimuli, and its dysfunction may have a profoundly negative influence, contributing significantly to disease.
The PNS is comprised of efferent nerves traveling from the CNS to (primarily) muscle for motor actuation and afferent nerves traveling from (primarily) sensory receptors to the CNS for interpretation.
The PNS is generally differentiated from the CNS in the following ways:
It is not contained within the bony confines of the skull and spinal vertebra.
It is not protected by the blood-brain barrier. Therefore toxic injury from circulating substances can more easily affect the PNS.
There are thirteen pairs of nerves that exit the brain, called cranial nerves (CNs). We will focus on the twelve clinically relevant CN pairs ( Table 4.1 ) (see Fast Fact Box 4.1 ).
| CN# | Name | Exit From Skull | Nuclei | Role | Function | Example of Clinical Relevance |
|---|---|---|---|---|---|---|
| I | Olfactory | Cribriform plate | Anterior olfactory nucleus (forebrain) | S |
|
Infection of cells that support olfactory bulb neurons by SARS-CoV-2 virus can cause anosmia (loss of sense of smell) in patients with COVID-19. Strong connections between sense of smell, memory, aggression and other emotions may be related to connections to the amygdala, thalamus, hippocampus, hypothalamus, and frontal cortex directly. |
| II | Optic | Optic canal | Lateral geniculate nucleus (thalamus) | S |
|
CN II is the only location where the CNS can be visualized (through an ophthalmoscope). Blurring of optic disc margins on fundoscopic exam (papilledema) may indicate accelerated hypertension, cerebral edema from increased intracranial pressure, a CNS mass/space occupying lesion. CNS inflammatory diseases (e.g., multiple sclerosis) may present as optic neuritis on fundoscopic exam and may cause blindness. |
| III | Oculomotor | Superior orbital fissure | Oculomotor nucleus, Edinger-Westphal nucleus | M |
|
Diplopia (double vision) results from dysfunction of the extraocular muscles according to the innervation by the oculomotor nerve. CN III palsy can be seen in diabetic neuropathy, granulomatous neuropathy (sarcoidosis, tuberculosis) or from an aneurysm in the adjacent Circle of Willis such as the posterior communicating artery. If diplopia is acute in an adult, an intracranial hemorrhage may be imminent and must be evaluated immediately. A long history of CN III palsy may be due to migraine. Anisocoria results when dysfunction of one CN III results in pupillary dilation. |
| IV | Trochlear | Superior orbital fissure | Trochlear nucleus | M |
|
Diplopia resulting from dysfunction of CV IV is most severe when gazing downward as when a patient is walking down stairs. |
| V |
|
V 1 : Superior orbital fissure V 2 : Foramen rotundum V 3 : Foramen ovale |
Principal sensory trigeminal nucleus, Spinal trigeminal nucleus, Mesencephalic trigeminal nucleus, Trigeminal motor nucleus | B |
|
Herpes Zoster infection (shingles) can affect the sensory component of CN V. If the tip of the nose has the shingles rash, there is concern for branch V2 and ocular involvement. Muscles of mastication. Cornea reflex (with CN X): touching the cornea may stimulate parasympathetic output from CN X and slow the heart rate, causing syncope. Smelling salts, which contain ammonia, can be detected by patients with defects of CN I function because such compounds are sensed by neurons in CN V. |
| VI | Abducens | Superior orbital fissure | Abducens nucleus | M |
|
Esotropia (movement of the affected eye towards the midline) and diplopia. CN VI is the longest of the CNs, crosses the tentorium, and can be affected by Circle of Willis aneurysms. |
| VII | Facial | Internal acoustic meatus | Facial nucleus, Solitary nucleus, Superior salivary nucleus | B |
|
Hyperacusis (increased sensitivity to or pain from sound) may occur when the stapedius muscle is paralyzed. Ramsey-Hunt syndrome is due to Herpes Zoster infection and manifests as shingles rash in the ear and motor weakness of the face. Bell’s Palsy is a peripheral CN VII motor neuropathy leading to facial weakness (inability smile, frown, loss of nasolabial fold). When the ipsilateral forehead is affected, the dysfunction is peripheral, but when a stroke affects CN VII centrally, the muscles of the forehead are spared because there is nerve cell cross over (bilateral innervation). |
| VIII | Vestibulocochlear | Internal acoustic meatus | Vestibular nuclei, Cochlear nuclei | S |
|
Vestibular dysfunction. Cold and warm water infusion into the ear of a comatose patient allows the examiner to evaluate the integrity of CN’s VIII (afferent branch) and CN’s III and VI (efferent branch) by inducing eye movements. A normal response to cold water is movement of both eyes toward the irrigated ear, but if there is a lesion in the reflex arc, the cold water will drive one or both eyes away from the irrigated ear to the contralateral side. Warm water has the reverse effects. The mnemonic for this abnormality is COWS = Cold Opposite, Warm Same. |
| IX | Glossopharyngeal | Jugular foramen | Inferior salivary nucleus, Solitary nucleus, Nucleus ambiguus | B |
|
Swallowing and dysphagia. Loss of gag reflex. |
| X | Vagus | Jugular foramen | Dorsal motor vagal nucleus, Solitary nucleus, Nucleus ambiguus | B |
|
Loss of function of CN X leads to resting tachycardia (increased heart rate). Stimulation of CN X leads to vasovagal response that may be seen in the corneal reflex as well as in response to pain, manifesting as bradycardia (slow heart rate), nausea, and diaphoresis (sweating). |
| XI | Accessory | Jugular foramen Ascending fibers-foramen magnum | Spinal accessory nucleus, Nucleus ambiguus | M |
|
Weakness due to neck or shoulder injury can lead to impaired shoulder shrug. |
| XII | Hypoglossal | Hypoglossal canal | Hypoglossal nucleus | M |
|
Weakness causes the tongue to deviate toward the side with the lesion, which could be due to infection, neoplasia, or trauma. Tongue atrophy seen with chronic CN XII dysfunction. |
One of the cranial nerve (CN) pairs, the nervus terminalis or CN zero (CN 0), serves a controversial role in humans. Originating from the septal nuclei and traveling very close to the olfactory nerves (CN I), this nerve pair is thought to be either a vestigial structure or to sense pheromones. CN 0 will be precluded from further discussion in this text.
Although all the nerves in Table 4.1 are considered CNs, they are not all technically part of the PNS. Neither CN I nor CN II originates in the brainstem and thus is technically part of the CNS.
CN I feeds directly into the limbic-associated cortex rather than relaying through the thalamus.
CN II (and the retina) is an extension of the diencephalon.
Note that parasympathetic innervation arises from CN III, VII, IX, and X, whereas sympathetic innervation is primarily from the sympathetic chain ganglion off of the spinal nerves. In addition to the functions listed in Table 4.1 , CN V 3 , VII and X also innervate the outside of the tympanic membrane, and IX innervates the inner tympanic membrane and the middle ear. CN IX and X also play a key role in baroreception and chemoreception: CN IX carries sensory innervation from the carotid body at the bifurcation of the internal and external carotid arteries, and CN X carries sensory innervation from the stretch receptors in the walls of the aortic arch and from chemoreceptors in the aortic bodies adjacent to the arch.
A major exception to the rule that general and special sensation is carried by afferent fibers and motor outputs are carried by efferent fibers is CN VIII. CN VIII has a special somatic efferent branch that actually carries signals that aid in a special sensation (hearing) from the brain to the cochlea and vestibular end organs.
Spinal nerves originate from the spinal cord. As mentioned in Chapter [3], there are 31 pairs of spinal nerves:
8 cervical (C1–C8)
12 thoracic (T1–T12)
5 lumbar (L1–L5)
5 sacral (S1–S5)
1 coccygeal (Co)
In general, the cervical nerves provide movement and sensation to the arms, neck, and upper portion of the trunk, and they also control breathing. The thoracic nerves provide movement and sensation to the trunk and abdomen. The lumbosacral nerves provide movement and sensation to the legs, bladder, bowel, and sexual organs.
Spinal nerves can carry sympathetic, parasympathetic, motor, and sensory information.
The ANS controls the sympathetic and parasympathetic innervations without conscious effort.
The somatic nervous system consciously controls motor innervations to muscle.
The somatic nervous system uses specialized receptors to sense the world.
The afferent fibers of the spinal nerves carry sensory information including:
Light touch
Vibration
Pain
Temperature
The specialized sensory receptors are innervated by several types of sensory nerve fibers including: Aβ (type II), Aδ (type III), and C (type IV) fibers.
Aβ fibers are thickly myelinated, 6 to 12 μm in diameter, fast (33–75 m/s), and are sensitive to cutaneous mechanoreceptors.
Aδ fibers are thinly myelinated, 1 to 5 μm in diameter, have a low activation threshold, are moderately fast (5–30 m/s), and are sensitive to temperature and mechanical (free nerve ending receptors) stimuli, and some nociceptors (pain receptors).
C fibers are unmyelinated, 0.2 to 1.5 μm in diameter, slow (<1 m/s), and carry nociceptors (and some warmth receptors).
To initially measure general sensation, such as light touch and vibration (carried by the dorsal columns), a set of specialized sensory receptors ( Table 4.2 ) are needed in the skin, which convey information to the sensory neuron whose cell body is in the dorsal root ganglion.
Fig. 4.1 illustrates where many of these sensory receptors are found in the skin.
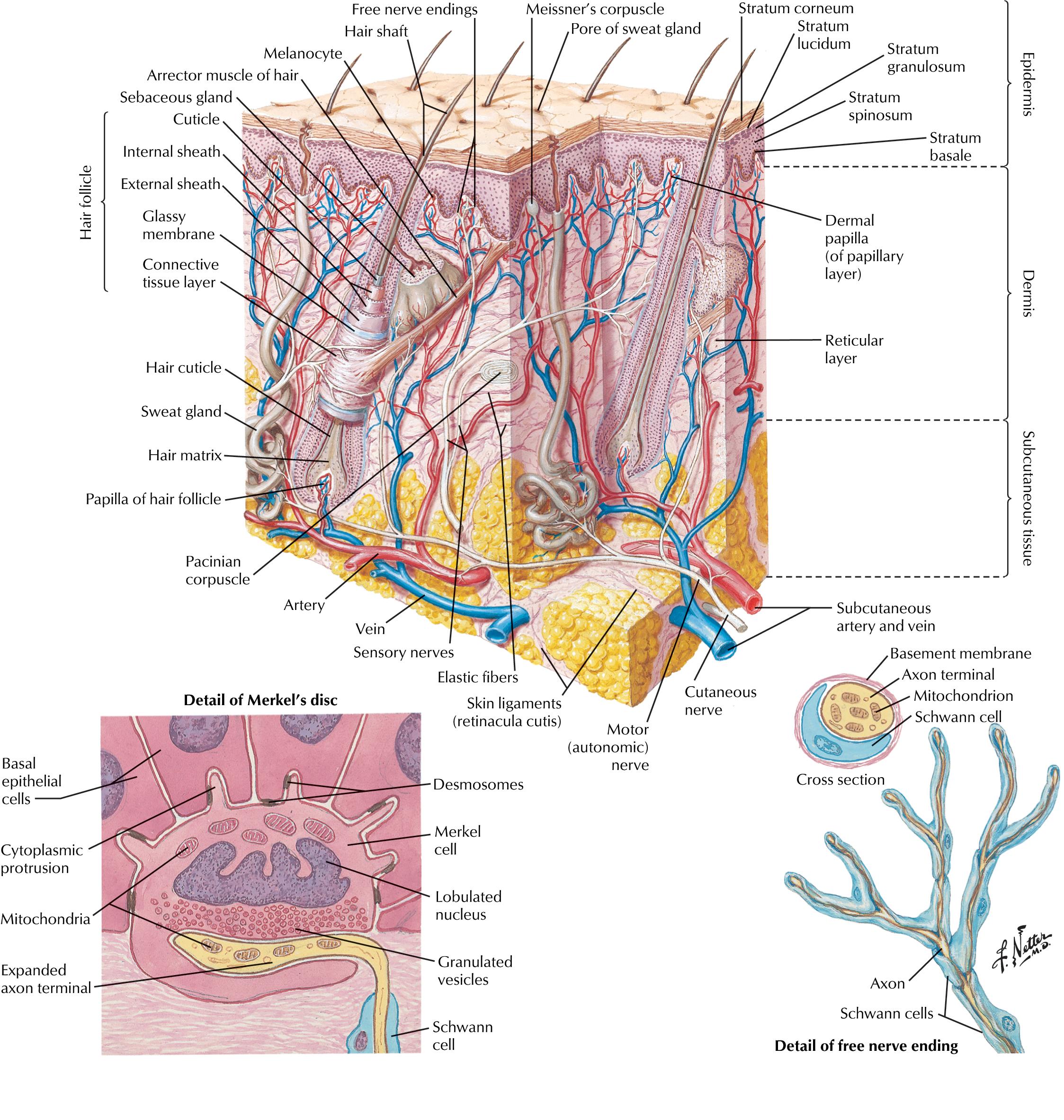
General sensation and proprioception are more rapidly adapted for than heat and pain because they are carried on the faster Aβ and Aδ fibers (as opposed to the slower C fibers).
| Sensory Nerve Ending | Adaptation Speed | Receptive Field Size | Terminal Location | Type of Sensation |
|---|---|---|---|---|
| Meissner’s corpuscles | Fast | Small | Superficial | Vibration |
| Merkel’s discs | Slow | Small | Superficial | Pressure |
| Pacinian corpuscles | Fast | Large | Deep | Pressure, vibration |
| Ruffini ending | Slow | Large | Deep | Pressure |
Pain is a highly subjective phenomenon and can be caused by a variety of pathologies including injury, disease, or even mental suffering.
First pain is sharp and immediate. It is modulated by intermediately fast Aδ fibers. This type of pain can be thought of as “good” acute pain because it acts as a warning signal to respond to a harmful stimulus (such as placing your hand on a hot stove).
Second pain is a delayed, diffuse, longer lasting sensation that is modulated by the slower C fibers. This pain is the chronic “bad” pain that is usually associated with pathology or damage that remains even after the stimulus that caused the acute pain is removed (see Clinical Correlation Box 4.1 ).
Referred pain, or improper sensation of pain in an incorrect region of the body, may occur because of imprecise topographic mapping of multiple afferent inputs to the same dorsal horn neurons or mixing of nerve fibers. For example, the pain of a kidney stone may be “referred” to the groin in addition to classic flank pain.
Pain and temperature are not only both carried by the spinothalamic tract into the CNS, but can also be sensed by the same specialized receptors. Extreme heat or extreme cold can both trigger the sensation of pain.
Specialized nerve endings also serve in many of the special senses relayed by the CNs and interpreted by specific topographic maps in the cerebral cortex. These senses include vision, hearing, olfaction, and taste.
Although the specific pathways for each of these special senses is outside the scope of this text, Table 4.3 gives a general overview of the specific receptors that are used to detect these various special senses, as well as the neural pathways these signals traverse and the specialized intermediate neuron types and thalamic nuclei used to transmit the signal to the specialized region of the cortex that interprets the sensory signal.
| Stimulus | Light | Sound | Temperature, Pain Sensation | Odor |
|---|---|---|---|---|
| Receptor | Rhodopsin | Unknown | Heat: TRPV1/2 Cold: TRPM8, TRPA1 |
G-Protein coupled olfactory receptors |
| Primary sensory cell | Photoreceptor | Inner hair cell | Dorsal root ganglion cell | Olfactory sensory neurons |
| Relay neuron | Bipolar cell | Spiral ganglion cell | Spinal cord neurons | Mitral/ tuft cells |
| Thalamic nucleus | Lateral geniculate nucleus | Medial geniculate nucleus | Ventral posterolateral nucleus | None, goes straight to cerebrum |
The ANS connects to the entire body, collecting information from and distributing instructions to the skin and organs, such as the eyes, and the visceral organs, such as the heart and blood vessels, lungs, gastrointestinal (GI) tract, bladder, and reproductive organs.
The ANS is composed of two divisions:
Sympathetic nervous system.
Parasympathetic nervous system.
Their distinct structures support different but complementary functions, which are described later. Many consider the complex neuronal network of the GI enteric nervous system (ENS) to be a third division of the ANS because it, too, generally works unconsciously (see Ch. 25 for a description of the ENS).
The ANS shares many basic structural and functional characteristics with the neurologic system involved in the control of skeletal muscle, the motor system. For example, the general structure of a nerve cell and the initiation and propagation of action potentials in the ANS resemble those of the motor system. The primary distinction is that the motor system is under conscious control, whereas the ANS works largely unconsciously. In the following section, it is useful to compare and contrast the structure and function of the ANS with those of the motor system.
Recall that like all homeostatic systems, the ANS must monitor the target tissues, transmit information on function back to the CNS via afferent pathways, integrate this information in central control centers, and then instruct the target tissues via efferent pathways.
The major tissues influenced by the ANS are:
Smooth muscles (such as those of blood vessel walls, the alimentary canal, and the urinary bladder);
Glands (such as the sweat glands and those of the respiratory and GI tract);
Cardiac muscle and cardiac electrical conduction system.
Specialized endings of afferent ANS nerves gather and communicate information from target tissues including the skin, internal organs, and associated blood vessels.
Chemoreceptors send signals about variables, such as the pH and partial pressure of oxygen, in their tissues.
Mechanoreceptors or baroreceptors, measure wall tension and thus pressure in blood vessels and viscera, such as the GI and urinary tracts.
Nociceptors serve relay signals interpreted as pain when viscera are damaged and/or overdistended, which are notably not unconscious (unlike the rest of the ANS).
ANS afferent neurons have long processes that go from their specialized endings in peripheral tissues to their cell bodies in the dorsal root ganglia of the spinal cord. Information is transmitted to the spinal cord by short axons where it can be processed, integrated with other signals, and acted on via autonomic reflexes of varying complexity.
Once signals are processed and appropriate responses are “decided,” they are transmitted via efferent ANS nerves, the most prominent of which is the vagus nerve (CN X).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here