Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Mastering the fundamental techniques of periocular surgery is essential for the Mohs and reconstructive surgeon. The eye holds immeasurable value, visual and aesthetic, that demand understanding and expertise to ensure successful surgical outcomes. The mobile nature of the eyelids and their bipolar suspension creates tensional forces that must be appreciated and actively managed during surgical repairs. Numerous surgical techniques have been described throughout the decades. In this chapter, fundamental principles and select reconstructive techniques that reliably produce optimal results and minimize complications are presented.
For most patients, a preoperative examination assessing visual acuity, intraocular pressure, and tear film/dryness is generally recommended within a year before surgery. Consultation with an oculoplastic surgeon is prudent for patients with preexisting eye disease and defects close to involving the lid margin. Imaging with computed tomography or magnetic resonance imaging may be indicated for tumors in the medial canthus and complex tumors that may extend into the orbit. Management or cessation of blood-thinning medications is indicated for tumor extirpations or repairs that extend into the orbital septum to minimize risks of retrobulbar hemorrhage. Meticulous intraoperative control of bleeding and postoperative observation and counseling are essential. Assessment and control of blood pressure in hypertensive patients is also important to minimize risks of bleeding. In addition, anxiolytic medications with adequate monitoring can be useful during periocular surgery.
Although many periocular repairs can be performed with standard facial repair trays, specialized instrumentation can be useful, particularly for defects involving the lid margins.
Specialized instrumentation for periocular surgical trays:
Corneal shields protect the globe and shield the light
Bishop-Harmon forceps for handling delicate tissue
Spring scissors for accurate cutting of fine tissues
Tenotomy scissors for cutting tarsus
Castroviejo needle drivers for grasping and placing fine sutures
Fine tissue hooks
Beaver blade and blade holders
Bipolar unit for hemostasis in a wet field
5-0 and 6-0 polyglactin sutures spatulated needles
6-0 polypropylene sutures
Proparacaine ophthalmic drops
Erythromycin ophthalmic ointment
Nonstick eye pads
The unique anatomy of the eyelids and supporting structures present unique challenges to the periocular surgeon. The eyelids are conceptually divided into anterior and posterior lamella for purposes of reconstruction. The posterior lamella, composed of mucosa and tarsus, also houses numerous glands vital for producing the tear film, which is essential for clear vision. The anterior lamella is composed of the orbicularis oculi muscle and skin, with minimal retinaculum in between. The orbicularis oculi is contiguous with the lateral canthal tendon, a fibrous tissue that tethers the tarsal plates to the bony orbit. The lateral canthal tendon attaches to the inside of the orbital rim at Whitnall tubercle, a bony prominence where additional suspensory ligaments, essential for opening and closing the lids, also converge. Whitnall tubercle can be palpated manually and is an important point of fixation for suspension and fixation of the of the lateral canthal tendon fundamental to many periocular repairs ( Fig. 12.1 ). The medial canthal tendon bifurcates into anterior and posterior limbs, which diverge around the lacrimal sac to facilitate the lacrimal pump before attaching to the anterior and posterior aspects of the bony lacrimal crest. Familiarity with the complex anatomy of the medial canthal region is essential to preserve lacrimal drainage.
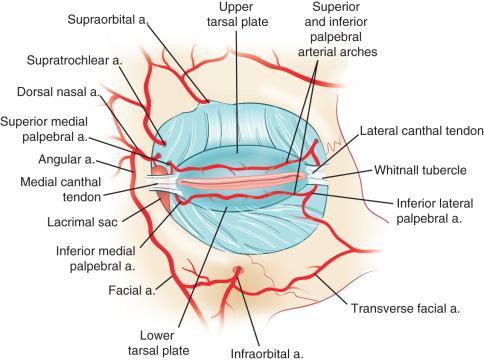
The vascular supply of the periorbital region is ample and facilitates a low infection rate and rapid healing of repairs in this area. The internal and external carotid arteries and veins provide vascular supply to the eyelids and surrounding tissue via numerous branches, including the dorsal nasal artery medially and the temporal and transverse facial arteries laterally that anastomose to form the marginal arcades of the eyelids. The sensory nerves of the eye emanate from ophthalmic and maxillary branches of the trigeminal nerve. Motor innervation required for both movement and constitutive tone of the periocular muscles is supplied by branches of the facial, oculomotor, and sympathetic nerves.
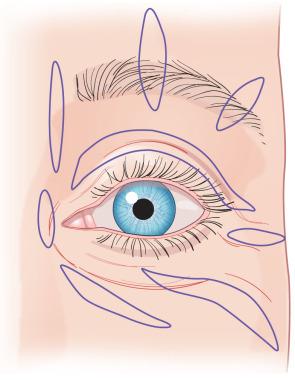
Preoperative, intraoperative, and postoperative assessments of the tensional forces around the eye are essential to prevent complications that may impact vision and cosmetic outcomes. Indeed, even the smallest tensional forces on the lid margin, created primarily or secondary to adjacent wound contraction, can lead to ectropion and webbing. The limits of tension can be assessed preoperatively by performing a “snap test,” in which the lid is pulled away from the globe and watching the rate of return, which correlates with the degree of laxity. Assessing maximal tension intraoperatively is also prudent, so that adjustments can be made and suspension sutures used to ensure tensional limitations are not exceeded. Forceps can be used to approximate wound edges prior to closure and tension assessed again after key sutures are placed. Maximal tension can be assessed by asking the patient to look up while opening the mouth widely (see Fig. 12.3 ). If the lid pulls away from the globe, then adjustments can be made before the surgery is completed. Additional support can be achieved intraoperatively by placing deep sutures in the cutaneous retinaculum and fascia to reinforce horizontal support and minimize downward pull on the eyelid. However, most importantly, the power of suspension sutures placed in the fascia, periosteum, and canthal support tissues to minimize tension around the eye cannot be overstated. Examples of periocular suspension sutures will be highlighted throughout this chapter.
There are many ways to approach the repair of defects located around the eye. Keeping incisions perpendicular to the lid margin and designing flaps that push tissue towards the lid margin and limit downward pull is the cornerstone of avoiding ectropion in periocular surgery ( Figs. 12.2 and 12.3 ). It is also important to oversize flaps and grafts adequately to accommodate for convexities, eye movement, and facial expression. The choice of closure often depends on a number of factors, including the size, depth, location of the defect and tissue reservoirs, skin laxity, and stability of the canthal tissues. Despite these variables, fundamental principles and techniques of reconstruction in the periocular area can be followed to optimize outcomes and avoid complications of webbing and ectropion (see Fig. 12.3 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here