Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Clinicians should quickly recognize severe airway obstruction and hypoxia to allow fast intervention, which should include a rapid progression to emergency invasive airway access as opposed to multiple attempts to intubate the trachea.
Proper identification of airway anatomy is the first step in successful performance of percutaneous invasive airway techniques and the avoidance of complications.
The airway practitioner should always consider the danger of piercing the posterior wall of the trachea and midline neck blood vessels during percutaneous invasive airway techniques.
Cricothyrotomy, whether by surgical or percutaneous technique, is the technique of choice to secure the airway in cannot intubate/cannot oxygenate (CICO) emergencies and in impending airway obstruction.
Training should be maintained by performing at least one procedure twice each year on live or cadaveric models or specialized manikins.
Providers may become and remain skilled in accessing the cricothyroid membrane (CTM) by routinely using the transtracheal block to anesthetize the airways in the context of awake and spontaneous breathing flexible intubation scope (FIS)-assisted intubations.
Translaryngeal insufflation of oxygen requires a high-pressure oxygen source unless catheters greater than 3 mm in inner diameter (ID) are used.
Ventrain and other similar devices (as they become available) that assist exhalation with active aspiration may be safer to use in situations of complete upper airway obstruction when transtracheal jet ventilation (TTJV) appears to be the only option available. However, more data are needed on the safe use of these devices, which are still not widely available.
Only commercial-grade devices should be used for these life-saving techniques.
Attempts at using a surgical technique to bypass an obstructed upper airway and restore breathing have been described in several ancient cultures since the Egyptian First Dynasty (c. 3200 bce ). In modern times (1546), the Italian physician Antonio Musa Brasavola performed the first recorded tracheostomy on a patient who was dying of suffocation due to a submandibular abscess. , Over the next two centuries, tracheostomies continued to be performed in similar emergent situations; however, these procedures never gained popularity as they were poorly understood and associated with a low rate of success and a high rate of severe complications. In America, tracheostomies were not introduced until the 19th century. Famously, the first president of the United Sates, George Washington, died on December 14, 1799, of complications of an upper respiratory tract infection; three physicians at his bedside debated whether an emergent tracheotomy could save his life but eventually decided not to perform one as it was deemed too dangerous. , Throughout the 19th century, these procedures, although seen as “life-saving,” continued to be rarely performed with no standardized surgical technique or a clear understanding of the etiology of the most severe complications. In 1909, Dr. Chevalier Jackson, a laryngologist at the Jefferson Medical School in Philadelphia, first described the surgical techniques and critical considerations related to performing “high tracheostomies,” or cricothyrotomies, opening the way to a better understanding of the causes of failure and complications of these delicate procedures.
Today, emergency airway access through the cricothyroid membrane (CTM), otherwise referred to as emergent cricothyrotomy, is considered an essential rescue technique in the “cannot intubate/cannot oxygenate” (CICO) situation. Although advancements in modern airway management have made resorting to invasive procedures a rare event, the CICO scenario still occurs. Unfortunately, although cricothyrotomy is considered the rescue technique of choice in perioperative CICO situations, this procedure still carries a high failure rate when performed by anesthesiologists rather than head and neck surgeons. Lack of training or availability of appropriate equipment may be to blame, but more research is needed to better understand and address issues in this area. By equipping the clinician with minimally invasive, effective alternatives to routine upper airway management, the potential for rescuing a failed airway and preventing devastating adverse outcomes is substantially increased.
Adverse outcomes related to respiratory events account for one of the two largest classes of injury in the American Society of Anesthesiologists (ASA) Closed Claims Project. As reported in the 2006 Closed Claims analysis, the two major categories of anesthesia-related events or mechanisms causing death or brain damage between 1975 and 2000 were respiratory and cardiovascular. Between 1986 and 2000, more than 1411 damaging events associated with death and permanent brain damage were reported, of which 503 events (36%) were respiratory in nature. Three mechanisms of injury were responsible for most of the adverse respiratory events: difficult endotracheal tube (ETT) placement (23%), inadequate ventilation (22%), and esophageal intubation (13%). Airway management-related and respiratory events remained the most represented category of complications overall in an analysis of 4549 anesthesia claims from 1990 to 2007 in the same database. In an analysis of claims against the National Health System in England between 1995 and 2007, airway and respiratory claims accounted for 12% of anesthesia-related claims, 53% of deaths, 27% of costs, and 10 of the 50 most expensive claims in the dataset. These claims most frequently described events at induction of anesthesia, involved airway management with an ETT, and typically led to hypoxia with subsequent death or brain injury. Similarly, an analysis of closed civil legal cases between 2007 and 2016 from the Canadian Medical Protective Association involving specialist anesthesiologists found 46 of the 406 (11%) cases to be airway related. In this case series, faulty judgment, inappropriate evaluation of the airway, and lack of proper planning for difficulty were common errors encountered that led to failed airway management and subsequent patient harm, brain injury, or death. Clinicians involved in airway management, and in particular anesthesiologists, must be acutely aware of the dire consequences of failing to plan appropriately and not acquiring or maintaining the necessary skills and equipment to deal with airway emergencies.
In the operating room (OR), intensive care unit (ICU), other hospital areas, and the prehospital setting, three difficult situations can be observed during attempts to control the airway: (1) the airway can be easily controlled by mask ventilation, but tracheal intubation is not possible; (2) the airway cannot be mask ventilated but can be intubated; and (3) rarely, the airway cannot be mask ventilated or intubated (i.e., the CICO scenario). Between 5 and 35 of every 10,000 patients (0.05% to 0.35%) reportedly cannot be tracheally intubated, and approximately 0.01 to 2.0 of every 10,000 patients are difficult to both mask ventilate and intubate. ,
The ASA, Difficult Airway Society, and Advanced Trauma Life Support guidelines, as well as other expert organizations, concur that, although invasive airway access is rarely practiced, any clinician who practices advanced airway management must possess this skill. , , The ASA Guidelines for Management of the Difficult Airway provide a difficult airway (DA) algorithm and propose strategies for evaluating, preparing for, and managing a patient with a DA. This algorithm describes emergency and nonemergency pathways for managing the airway if intubation fails and suggests that equipment suitable for “emergency surgical airway access” (i.e., surgical or percutaneous tracheostomy or cricothyrotomy) be among the contents of a readily available portable storage unit for DA management.
Surgical cricothyrotomy has long been a standard of emergency invasive airway rescue; however, its use has declined, in part because of advances in noninvasive airway devices such as supraglottic airways (SGAs) and video laryngoscopes (VLs), the adoption of rapid sequence intubation (RSI) in the emergency department, and increased requirements for trainee supervision. Percutaneous techniques for invasive airway access, the focus of this chapter, increasingly replaced surgical cricothyrotomy for many years; this is likely because many anesthesiologists prefer percutaneous to surgical techniques given the familiarity with similar techniques for other procedures (e.g., central venous catheterization). However, a return to greater use of open surgical techniques has recently been widely advocated, based on a higher success rate, , particularly after the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society (NAP4) called attention to the high failure rate of percutaneous cricothyrotomies performed by anesthesiologists. Whether the failures described in NAP4 were caused by anesthesiologists’ lack of training, the use of inappropriate equipment, equipment design problems, or technical failures needs further study.
Cricothyrotomy is a technique for providing an opening in the space between the anterior inferior border of the thyroid cartilage and the anterior superior border of the cricoid cartilage for the purpose of gaining access to the airway. This area is the most accessible part of the respiratory tree below the glottis. , Based on the urgency of the clinical situation, the procedure can be performed emergently or electively. Emergent cricothyrotomy may be done in the prehospital setting, emergency room, ICU, or OR. Elective cricothyrotomy is usually performed before a surgical procedure in the OR. Depending on the technique used, the procedure may also be classified as surgical or nonsurgical. The nonsurgical approach can be achieved by needle puncture or percutaneously over a guidewire, with or without a CTM incision.
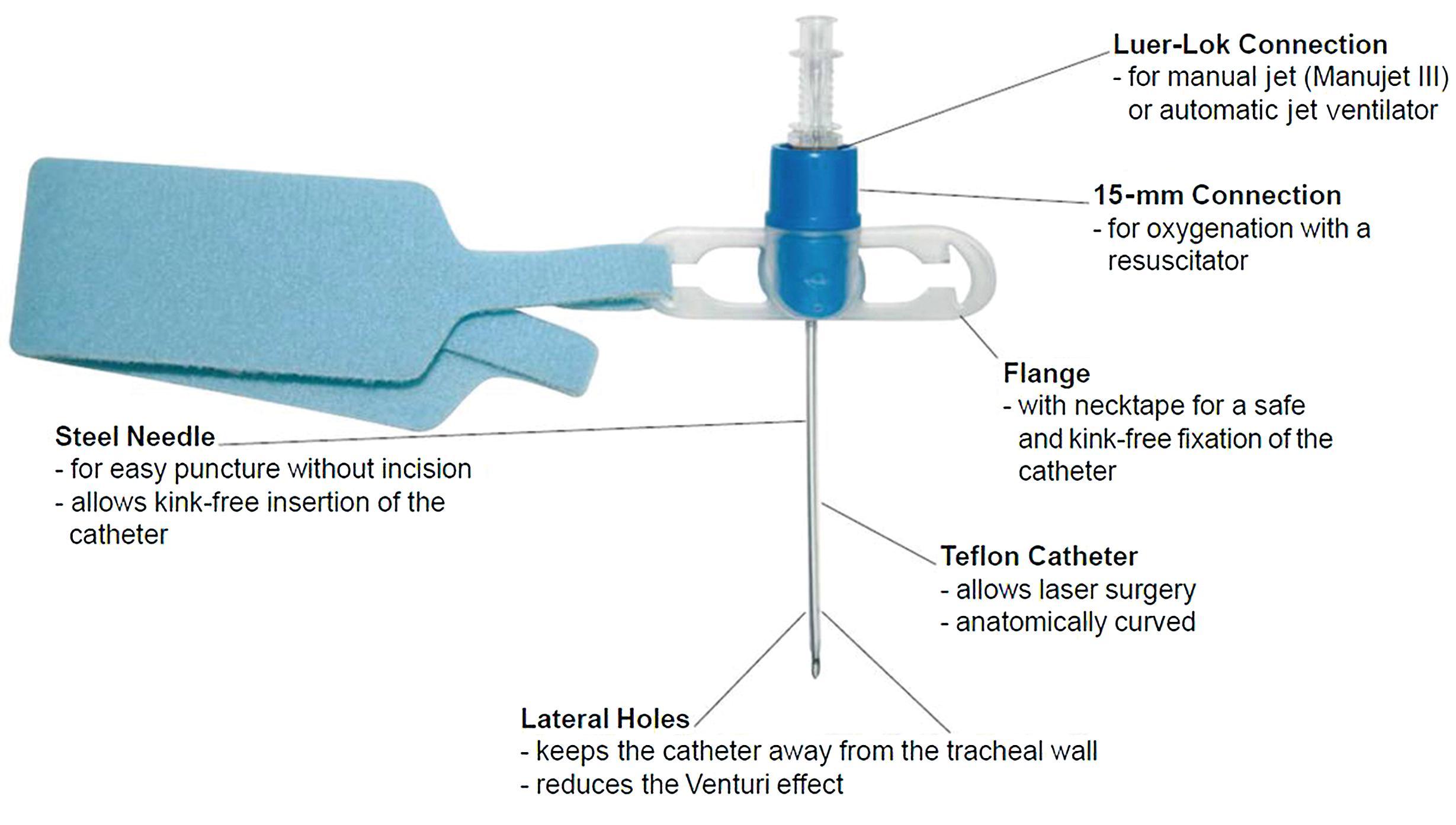
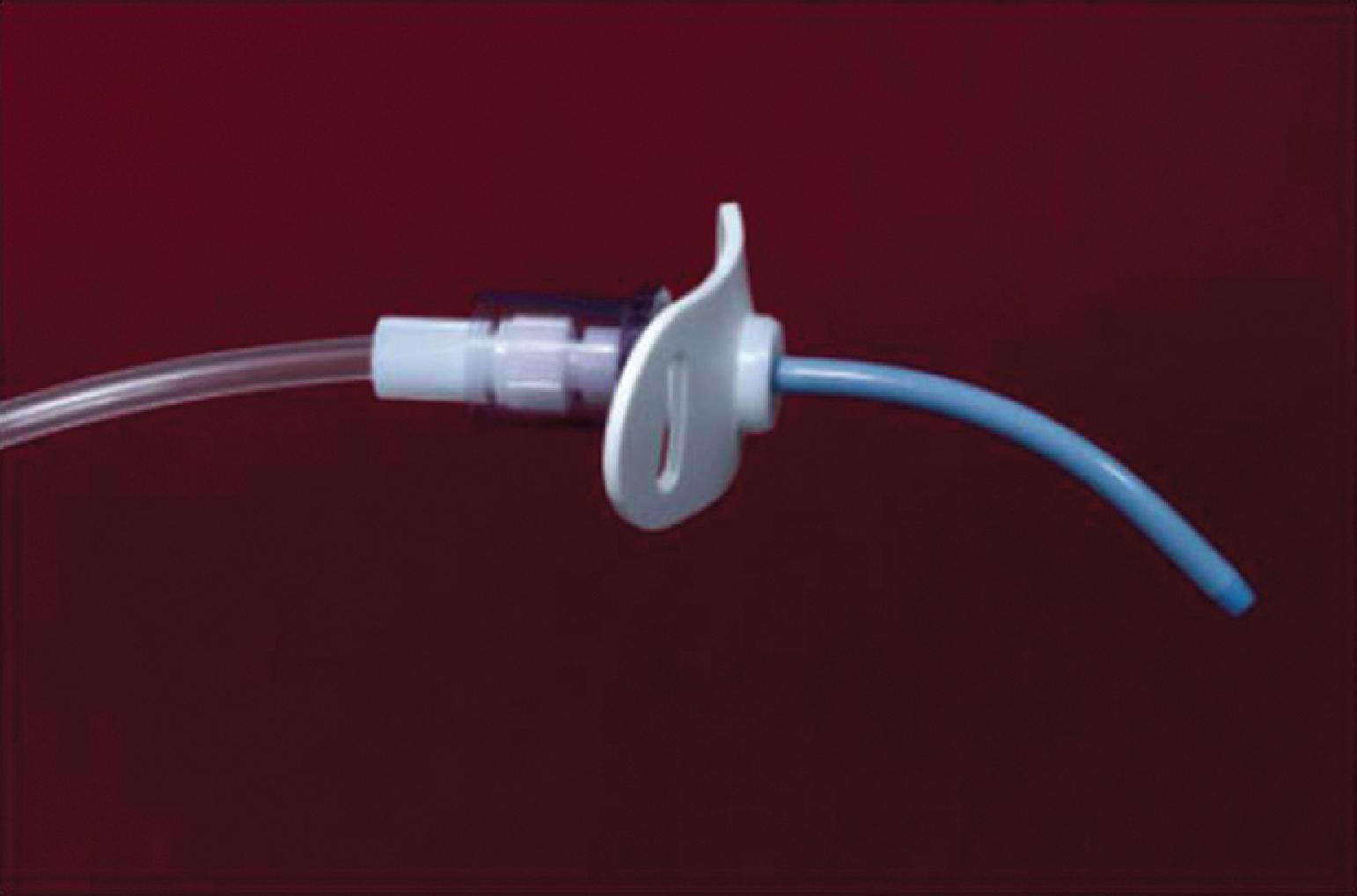
A practical classification of cricothyrotomy techniques includes three categories. The first category includes narrow-bore (≤9-French or 3-mm inner diameter [ID]) cannula-type devices placed directly through the CTM using an over-the-needle technique; the cannula is then used for transtracheal catheter ventilation or, more accurately, transcricoid ventilation. The Cook Transtracheal Airway Catheter ( Fig. 28.1 ) and the Ravussin cannula ( Fig. 28.2 ) are examples of these devices. Devices such as the Arndt cricothyrotomy catheter are narrow bore ( Fig. 28.3 ) but are inserted as described for the second category.

The second category includes techniques that require the introduction of a guidewire inserted through a needle or catheter and followed by dilation of the cricothyroid space (i.e., a Seldinger technique). The needle or catheter placement may be preceded by an incision of the skin and of the CTM. An airway catheter is introduced over the dilator threaded over the guidewire. These techniques allow insertion of an airway considerably larger than the initial needle or catheter, often of sufficient ID to allow ventilation with conventional ventilation devices, suctioning, and spontaneous ventilation. These techniques are known as percutaneous dilatational cricothyrotomy (PDC).
The third category is surgical cricothyrotomy, which involves the use of a scalpel and other surgical instruments to create an opening between the skin and the cricothyroid space. It is discussed in Chapter 29 .
The term transtracheal jet ventilation (TTJV) is used to describe a ventilation technique in which rapid access to the airway at the level of the CTM is followed by jet ventilation through a narrow-bore cannula or catheter. TTJV is primarily used as an emergency technique, but it has also been used electively as a bridge to more secure airway control and in the context of upper airway surgery. A number of different terms and acronyms are used in the literature to describe this same technique. Terms such as percutaneous (or simply trans- ), laryngeal (versus tracheal ), and insufflation or oxygenation (versus ventilation ) may all be appropriate.
A CICO emergency has been defined as the inability to restore alveolar oxygenation by means of any nonsurgical technique (i.e., face mask, ETT, or SGA device). It is a primary responsibility of physicians skilled in advanced airway management to be able to promptly recognize and manage a CICO scenario by means of an invasive airway access technique. A typical pattern of events and pitfalls has been recognized in the development of CICO, where several attempts to intubate the trachea by multiple providers initially occur in a cannot intubate/ can oxygenate scenario. This situation deceptively encourages providers to persist with attempts to secure the airway by intubation or SGA positioning until inflammation and edema of the airway lead to obstruction and impossibility to oxygenate.
Following a high-profile case of perioperative death in a CICO scenario that developed in this manner, several national and international airway societies have revised airway management guidelines to emphasize a final common “emergency” pathway that culminates in emergency invasive airway access. , , The importance of avoiding delays in addressing the CICO scenario with an emergency invasive airway is also stressed in the Vortex approach. The Vortex approach is a cognitive aid, or high-acuity implementation tool, designed to support teamwork and decision-making during airway emergencies. It is based on the analogy of a funnel, which represents the diminishing time and options available as one spirals deeper into the emergency, after exhausting all viable options (see Chapter 11 ). Once emergency invasive airway access has been obtained, oxygenation and ventilation through a narrow-bore catheter presents challenges and risks of complications that will be discussed in detail later in this chapter.
The safe and rapid performance of cricothyrotomy requires a thorough knowledge of cricothyroid anatomy ( Fig. 28.4A ) and its relation to other structures in the anterior neck. , In adults, the CTM is approximately 10 mm long and 22 mm wide and is composed mostly of yellow elastic tissue. It covers the cricothyroid space and is located in the anterior neck between the thyroid cartilage superiorly and the cricoid cartilage inferiorly. The cricothyroid space can be readily identified by palpating a slight dip or indentation in the skin immediately below the laryngeal prominence.
![Fig. 28.4, (A) Dissection anatomy of the anterior neck. (B) External landmarks. From cephalad to caudad, the thyroid notch, inferior border of the thyroid cartilage, superior border of the cricoid cartilage, and sternal notch are marked. (C) External landmarks. From cephalad to caudad, the hyoid bone, thyroid cartilage, and cricoid cartilage are marked. ([A] From De Leyn P, Bedert L, Delcroix M. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg . 2007;32:412–421.) Fig. 28.4, (A) Dissection anatomy of the anterior neck. (B) External landmarks. From cephalad to caudad, the thyroid notch, inferior border of the thyroid cartilage, superior border of the cricoid cartilage, and sternal notch are marked. (C) External landmarks. From cephalad to caudad, the hyoid bone, thyroid cartilage, and cricoid cartilage are marked. ([A] From De Leyn P, Bedert L, Delcroix M. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg . 2007;32:412–421.)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PercutaneousEmergencyAirwayAccess/3_3s20B978032379538800028X.jpg)
The CTM consists of a central anterior triangular portion (the conus elasticus) and two lateral parts. The thicker and stronger conus elasticus narrows above and broadens below, connecting the thyroid to the cricoid cartilage. It lies subcutaneously in the midline and is often crossed horizontally in its upper third by the superior cricothyroid vessels. Characteristically, the CTM does not calcify with age and lies immediately underneath the skin.
Variations in the anatomy and dimensions of the CTM are common. The anterior cricothyroid space is trapezoidal and has a cross-sectional area of approximately 2.9 cm . The mean distance between the anterior borders of the inferior thyroid cartilage and the superior cricoid cartilage is 9 mm (range, 5 to 12 mm), whereas the width of the anterior cricothyroid space ranges from 27 to 32 mm. The cricothyroid space is not much larger than 7 mm in its vertical dimension, and that space may be narrowed further by contraction of the cricothyroid muscle. The vertical distance between the undersurface of the true vocal cords and the lower anterior edge of the thyroid cartilage is between 5 and 11 mm. The vertical height of the CTM from the superior border of the cricoid cartilage to the inferior border of the thyroid cartilage in the midline varies from 8 to 19 mm (mean, 13.69 mm), a somewhat greater distance that can probably be explained by the fresh rather than fixed state of specimens.
The arterial and venous vessel patterns in the neck area surrounding the CTM also vary considerably. Although the arteries always lie deep to the pretracheal fascia and are easily avoided during a skin incision, veins may be found in the pretracheal fascia and between the pretracheal and superficial cervical fascia. Vascular structures may cross vertically and anterior to the CTM, predisposing them to damage during cricothyrotomy. A small cricothyroid artery, which is a branch of the superior thyroid artery, commonly crosses the upper portion of the CTM, anastomosing with the artery on the other side.
To minimize the possibility of bleeding, the CTM should be incised at its inferior third portion. The two lateral parts are thinner, lie close to the laryngeal mucosa, and extend from the superior border of the cricoid cartilage to the inferior margin of the true vocal cords. On either side, the CTM is bordered by the cricothyroid muscle. Lateral to the membrane are venous branches from the inferior thyroid and anterior jugular veins. Because the vocal cords usually lie 1 cm above the cricothyroid space, they are not commonly injured, even during emergency cricothyrotomy. The anterior jugular veins run vertically in the lateral aspect of the neck and are rarely injured, but branches may occasionally course over the cricothyroid space and be damaged during the procedure.
External visible and palpable anatomic landmarks are used to locate the CTM. The laryngeal prominence (i.e., thyroid cartilage or Adam’s apple) and the hyoid bone above it are readily palpable. The CTM usually lies 1 to 1.5 fingerbreadths below the laryngeal prominence. The cricoid cartilage is usually felt below the CTM.
The importance of these landmarks is emphasized because of the disastrous consequences of placing a cricothyrotomy tube into the thyrohyoid space instead of the cricothyroid space. Conscious effort to identify these landmarks reduces the possibility of committing this preventable error ( Fig. 28.4B and C ). When the normal anatomy is distorted, identification of these landmarks is difficult. In these cases, the suprasternal notch may be used as an alternative or additional marker. The small finger of the right hand should be placed in the patient’s suprasternal notch, followed by placement of the ring, long, and index fingers adjacent to each other in a stepwise fashion up the neck, with each finger touching the one below it. When the head is in the neutral position, the index finger is usually on or near the CTM.
The use of ultrasonography has been proposed to improve identification of landmarks, as well anatomic variations and vascular structures (see Chapter 3 ). , However, in emergencies, its utilization and practical usefulness are debatable, depending on immediate availability and providers’ skill.
Cricothyrotomy is considered by many to be the standard approach to airway management when orotracheal or nasotracheal intubation approaches have failed and oxygenation and ventilation are not achievable by other means. , In the emergency room or prehospital setting, , cricothyrotomy is indicated for immediate airway control in patients with maxillofacial, cervical spine, head, and/or neck trauma and in patients in whom tracheal intubation is impossible to perform or contraindicated. It is also used for the immediate relief of upper airway obstruction. In the OR and in the ICU, the technique is indicated when conventional methods of intubation fail, such as in patients with traumatic facial injuries in whom other techniques of airway access are difficult or impossible to perform. Cricothyrotomy can also be used as an alternative to tracheostomy in patients with recent sternotomy who require invasive airway access because the incision does not communicate with the mediastinal tissue planes. A cricothyrotomy catheter may be fitted with a Luer-Lok connection (for jet ventilation) or with an anesthesia circuit-size (15 mm) connector for thoracic and other procedures involving the airways, especially the trachea, larynx, epiglottis, and base of the tongue.
Emergency cricothyrotomy has largely replaced emergency tracheostomy in the emergency department because of its simplicity, rapidity, and minimal morbidity, whereas debate continues on the value of percutaneous techniques as opposed to surgical approaches. , The performance of emergency tracheostomy is limited and indicated only when laryngeal trauma may be accompanied by local edema, hemorrhage, subcutaneous emphysema, and damage to the thyroid or cricothyroid cartilage, precluding the performance of a cricothyrotomy.
Absolute and relative contraindications to cricothyrotomy are rare, considering that it is a life-saving, emergency procedure in a CICO scenario. Patients who have been intubated translaryngeally for more than 3 days (or 7 days or longer, according to different investigators) should not undergo cricothyrotomy because of the propensity to develop subglottic stenosis. Those with preexisting laryngeal diseases, such as cancer, acute or chronic inflammation, or epiglottitis, have a higher morbidity rate when cricothyrotomy is performed. Distortion of the normal neck anatomy by disease or injury may render the technique impossible. Normal anatomic landmarks may be distorted, making identification of the CTM difficult. Bleeding diatheses or history of coagulopathy predispose the patient to hemorrhage, making the procedure extremely dangerous.
Cricothyrotomy is difficult to perform in pediatric patients because the larynx is smaller and the airway contains less fibrous supporting tissue and has only loose mucous membrane attachments in the airway inlet. Because of this technical limitation, cricothyrotomy should be performed with extreme caution in children younger than 10 years and should not be performed at all in children younger than 6 years unless a wire can be placed in the cricothyroid space and placement within the trachea can be verified. In this age group, emergency tracheostomy under controlled conditions is the preferred choice. Johansen and colleagues described an exceedingly high failure rate (83%) in an experimental swine model of the juvenile population, likely attributable to the lack of circumferential support offered by the immature cricoid cartilage.
Physicians who are unfamiliar or inexperienced with the technique are discouraged from performing the procedure without adequate supervision from a more senior or knowledgeable member of the medical team. Inexperience has been implicated as the most important factor contributing to cricothyrotomy complications. Accuracy in identifying anatomic landmarks significantly depends on the physician’s experience but is poor overall, justifying the percutaneous technique in emergency conditions but supporting the use of ultrasound or video-enhanced visualization during elective procedures.
The most common indications for performing TTJV are rescue oxygenation in a CICO situation (emergent indication), airway rescue in complete upper airway obstruction (emergent indication), supplemental oxygenation during difficult tracheal intubation (elective indication), and ventilation during upper airway surgery (elective indication). Here, we will briefly discuss the emergent indications of TTJV use.
The primary indication for TTJV through a narrow-bore cannula is rescue oxygenation in an emergent CICO scenario. However, in a CICO scenario complicated by upper airway obstruction, TTJV may have relative or absolute contraindications, depending on the location and degree of obstruction. Barotrauma as a result of air trapping is the major risk associated with the use of TTJV and manifests when the gas that is insufflated at high pressure does not have a path for egress due to an obstructed upper airway. A recent systematic review of the use of TTJV in CICO emergencies concluded that TTJV in this scenario is associated with a high risk of device failure and barotrauma, suggesting that support for the use of this technique in the CICO emergency should be reconsidered.
TTJV in the setting of complete airway obstruction can lead to a dramatic increase in intrathoracic pressure, resulting in barotrauma and hemodynamic collapse. Because of these potentially fatal complications, TTJV is considered contraindicated in this setting, although it may be appropriate as a temporary last resort measure if a mechanism to assist with gas egress in the exhalation phase is implemented (see further discussion below). Data are sparse in support of the use of TTJV in complete upper airway obstruction, primarily based on animal studies, lung models, or case reports of emergent situations in which the technique proved useful despite significant safety concerns for the high risk of barotrauma. Low-flow translaryngeal rescue insufflation of oxygen of as little as 2 L per minute has been shown to maintain oxygenation in a large animal model (34-kg pigs) and may be a short-term rescue option when definitive surgical airway control is anticipated.
Recently, the concept of an active expiratory phase has been applied to TTJV by introduction of the Ventrain system (Ventinova Medical B.V., Eindhoven, Netherlands), a rescue oxygenation device with expiratory assistance based on the Venturi effect. Expiratory ventilation assistance devices, such as the Ventrain, combine high-pressure lung ventilation with active aspiration of gas during exhalation. An experimental device based on the same principle has been found to reduce the time required for an injected tidal volume to be expired via a narrow-bore cannula and also increase the effective minute ventilation. Expiratory ventilation assistance is less effective when the upper airway is unobstructed, possibly because of preferential entrainment of ambient air into the TTJV catheter via the lower-resistance upper airway path and, consequently, reduced removal of alveolar gases.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here