Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Effective clinical evaluation of patients with disorders of the female pelvic floor, such as pelvic organ prolapse (POP) and stress urinary incontinence (SUI), requires a clear understanding of female pelvic anatomy. Defects of vaginal support include anterior vaginal prolapse (cystocele), posterior vaginal prolapse (rectocele and enterocele), and apical uterine prolapse. Symptoms of POP generally affect quality of life, but when complete uterine prolapse (procidentia) occurs, ureteral obstruction and kidney damage may result.
A staging system has been developed for POP so that outcomes of surgical and nonsurgical treatment can be quantified, followed, and improved. Medical management of mild to moderate cases of POP includes pelvic muscle exercises and the use of pessaries. Surgical procedures include anterior and posterior repairs (colporrhaphy) using existing natural tissue and synthetic mesh materials, vaginal vault suspension (colpopexy) for apical vaginal prolapse, and complete vaginal closure procedures (colpocleisis) for some women who no longer desire coital function. Robot-assisted procedures are now used for some of these interventions.
Urinary incontinence is defined as the involuntary loss of urine that is a social or hygienic problem. It is estimated that as many as 50% of women have some urinary incontinence at some time during their lives. SUI occurs in response to physical exertion, coughing, or sneezing. After appropriate testing to document SUI, surgical procedures include retropubic urethropexy, suburethral sling placement, or bulking injections.
Overactive bladder (OAB) and urge urinary incontinence (UUI) are used interchangeably to describe incontinence that occurs when there is a strong urge to pass urine with a decreased ability to prevent passage. Treatments include behavior modification (bladder training), medications, electrical stimulation, or injections.
Overflow incontinence and urinary fistulas may also be causes of involuntary passing of urine. Neuropathies account for most of the cases of overflow incontinence, whereas pelvic surgery and radiation damage cause 95% of fistulas. Surgical repair of fistulas is almost always needed. Pelvic pain disorders include painful bladder and myofascial pelvic pain syndrome.
An accurate knowledge of the anatomy of the female pelvic floor enables the student to understand pelvic organ prolapse and its management. Female pelvic medicine and reconstructive surgery (FPMRS) is the newest board-certified subspecialty within the specialties of obstetrics and gynecology as well as urology. This new certification process recognizes the importance of disorders of the female pelvic floor and the increased knowledge and skills necessary to evaluate and treat these disorders.
The bony pelvis acts like a basket, supporting the muscular attachments, pelvic organs, vessels, and nerves contained within it. The pelvic organs, including the vagina, uterus, bladder, urethra, and rectum, are supported within the pelvis by the bilaterally paired and posteriorly fused levator ani muscles. The anterior separation between the levator ani is called the levator hiatus . Inferiorly, the levator hiatus is covered by the urogenital diaphragm. The urethra, vagina, and rectum pass through the levator hiatus and urogenital diaphragm as they exit the pelvis. The endopelvic fascia is a visceral pelvic fascia that invests the pelvic organs and forms bilateral condensations referred to as ligaments (i.e., pubourethral, cardinal, and uterosacral ligaments). These ligaments attach the organs to the fascia of the pelvic side walls and bony pelvis. Damage to the vagina and its support system allows the urethra, bladder, rectum, and small bowel to herniate and protrude into the vaginal canal.
The perineal body is a central point for the attachment of the perineal musculature. Although the contents of the abdominal cavity bear down on the pelvic organs, they remain suspended in relation to each other and to the underlying levator sling and perineal body.
Pelvic organ prolapse (POP) refers to the protrusion of the pelvic organs into the vaginal canal or beyond the vaginal opening. It occurs because of a weakness in the endopelvic fascia investing the vagina, along with its ligamentous supports. Defects in vaginal support may occur in isolation (e.g., anterior vaginal wall only), but they are more commonly combined. The nomenclature of POP has evolved such that older terms such as cystocele, rectocele, and enterocele have been replaced by more anatomically precise terms ( Figure 23-1 ).
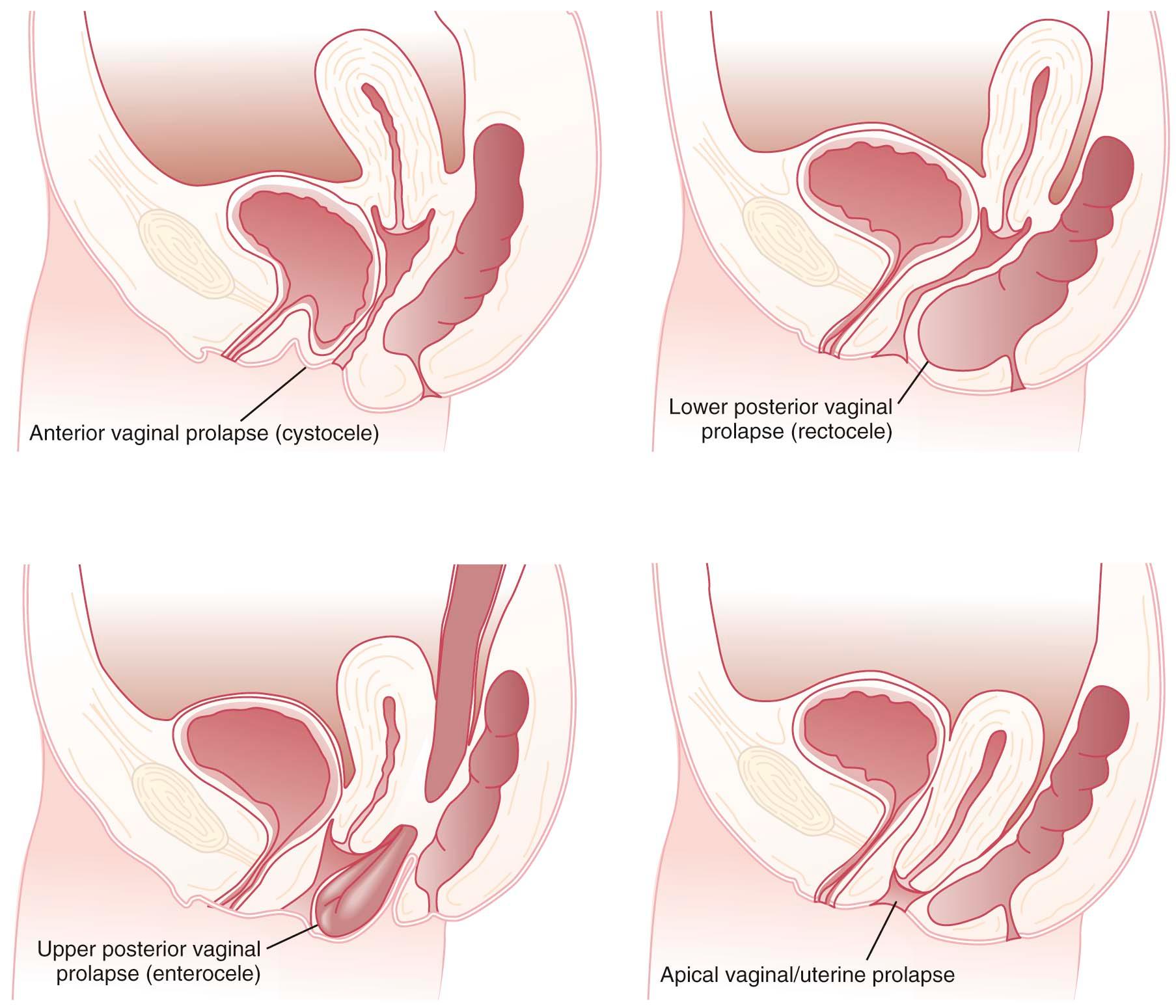
The anterior vagina is the most common site of vaginal prolapse. Women with this type of defect will describe symptoms of vaginal fullness, heaviness, pressure, and/or discomfort that often progress over the course of the day and are most noticeable after prolonged standing or straining. Women may have to apply manual pressure to empty their bladder completely. Other symptoms include stress urinary incontinence (SUI), urinary urgency, and frequency. Significant anterior vaginal wall prolapse that protrudes beyond the vaginal opening (hymen) can cause urethral obstruction caused by kinking, resulting in urinary retention or incomplete bladder emptying.
Posterior vaginal defects occur when there is weakness in the rectovaginal septum. Symptoms can be indistinguishable from other types of prolapse because the discomfort, pressure, and the sense of a vaginal bulge are nonspecific. When difficulties with bowel function and defecation occur, lower posterior vaginal prolapse is likely. Straining or the need to manually splint for complete bowel elimination may occur. Upper posterior vaginal wall prolapse is nearly always associated with herniation of the pouch of Douglas, and because this is likely to contain loops of bowel, it is called an enterocele .
Although vaginal prolapse can occur without uterine prolapse, the uterus cannot descend without carrying the upper or apical portion of the vagina with it.
Complete procidentia (uterine prolapse through the vaginal hymen) represents failure of all the vaginal supports ( Figure 23-2 ). Hypertrophy, elongation, congestion, and edema of the cervix may sometimes cause a large protrusion of tissue beyond the hymen that may be mistaken for a complete procidentia. Vaginal vault prolapse or eversion of the vagina may be seen after vaginal or abdominal hysterectomy and represents failure of the supports around the upper vagina.

Symptoms of POP mainly affect a woman's quality of life. However, significant sequelae of POP can occur in neglected cases of procidentia, which may be complicated by excessive purulent discharge, decubitus ulceration, and bleeding. Ureteral obstruction with hydronephrosis is also a possible result of complete procidentia.
The pelvic fascia, ligaments, and muscles may become attenuated from excessive stretching during pregnancy, labor, and difficult vaginal delivery, especially with forceps or vacuum assistance. Asian and black women appear less likely than white women to develop prolapse.
Increased intraabdominal pressure resulting from a chronic cough, ascites, repeated lifting of heavy weights, or habitual straining as a result of constipation may predispose women to prolapse. Atrophy of the supporting tissues with aging, especially after menopause, also plays an important role in the initiation or worsening of pelvic relaxation. Iatrogenic factors include failure to adequately correct all pelvic support defects at the time of pelvic surgery, such as hysterectomy.
Vaginal examination is facilitated by using a single-blade speculum. While the posterior vaginal wall is being depressed, the patient is asked to strain down. This demonstrates the descent of the anterior vaginal wall consistent with prolapse and urethral displacement. Similarly, retraction of the anterior vaginal wall during straining will accentuate posterior vaginal defects and uncover an enterocele and rectocele if present. Rectal and vaginal examinations are often useful to demonstrate a rectocele and to distinguish it from an enterocele.
The preferred method for describing and documenting the severity of POP is the Pelvic Organ Prolapse Quantification (POP-Q) system. The extent of prolapse is evaluated and measured relative to the hymen, which is a fixed anatomic landmark. The anatomic positions of the six defined points for measurement are denoted in centimeters above the hymen (negative number) or centimeters below the hymen (positive number). The plane at the level of the hymen is defined as zero ( Figure 23-3 ).
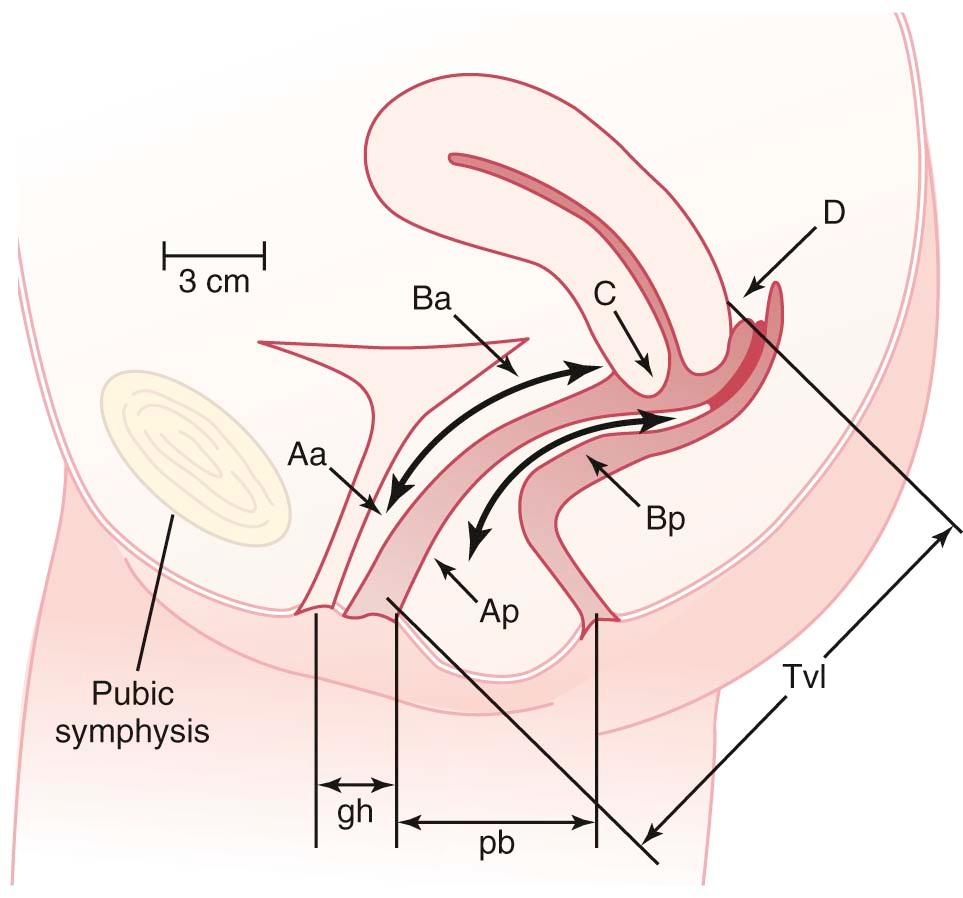
Stages of POP can be assigned according to the most severe portion of the prolapse after the full extent of the protrusion has been determined. An ordinal system is used for measurements of different points along the vaginal canal, which allows for better communication between clinicians. This staging system enables more objective tracking of surgical outcomes.
Prophylactic measures to mitigate the symptoms of POP include identifying and treating chronic respiratory and metabolic disorders, correction of constipation and intraabdominal disorders that may cause repetitive increases in intraabdominal pressure, and, for menopausal women, administration of estrogen. Failure to recognize and treat significant support defects at the time of concomitant gynecologic surgery may lead to progression of existing prolapse and the development of urinary incontinence or retention and urinary tract infections (UTIs).
When only a mild degree of pelvic relaxation is present, pelvic floor muscle exercises may improve the tone of the pelvic floor musculature. Pessaries ( Figure 23-4 ), which provide intravaginal support, may be used to correct prolapse by internally supporting the vagina. They can be considered when the patient is medically unfit or refuses surgery or during pregnancy and the postpartum period. They are also useful to promote healing of a decubitus ulcer before surgery. In many patients, pessaries are the treatment of choice, as they are almost risk-free, immediately available, and useful for interim treatment in those wishing to delay surgery.
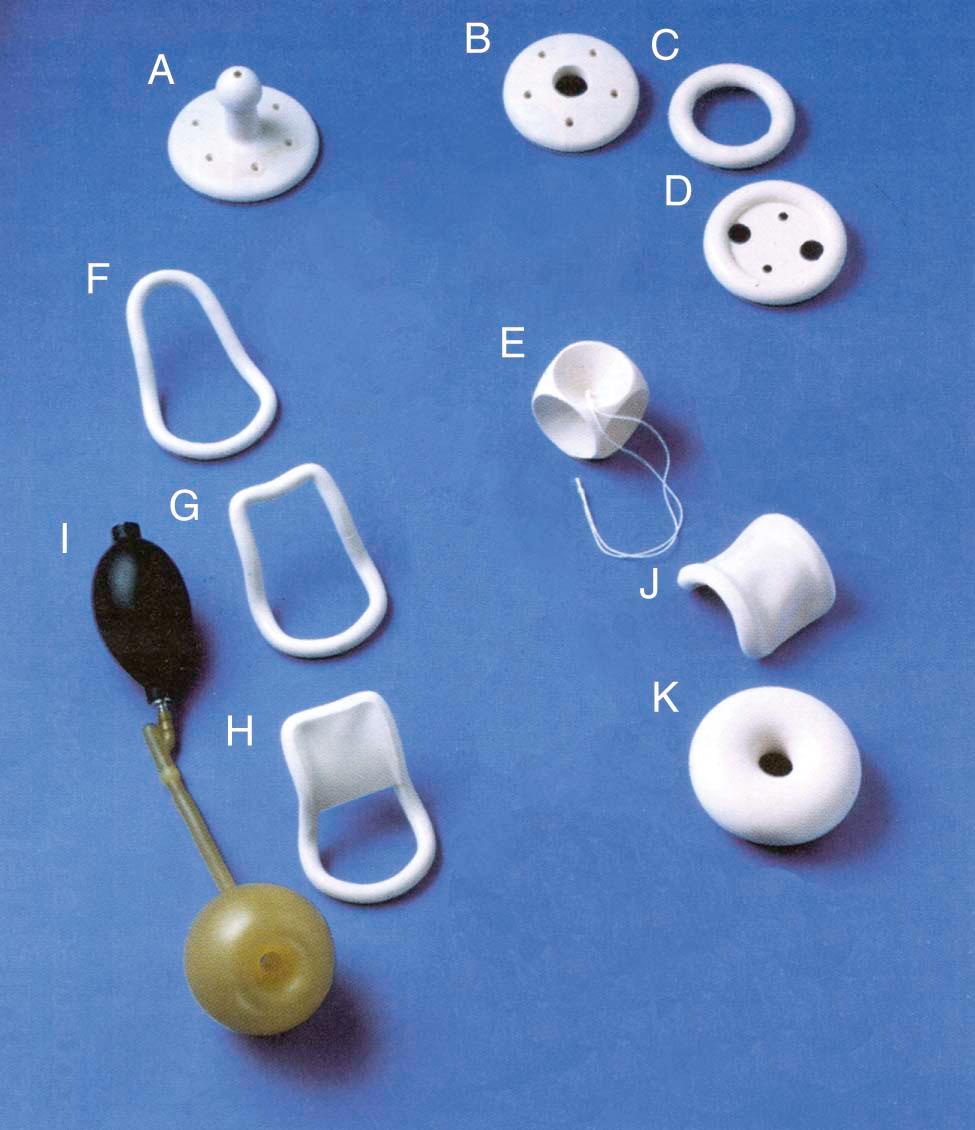
Pessaries require proper fitting and must be selected in the appropriate type and size. They should be removed, cleaned, and reinserted every 6 to 12 weeks. They may cause vaginal irritation and ulceration. Neglect may result in serious consequences, including fistula formation, impaction, bleeding, and infection. Many patients are capable of caring for their pessaries themselves. In those cases, the patient inserts, removes, and cleans her pessary several times each week, if not daily. It is similar to the care and use of a contraceptive diaphragm.
The main objectives of surgery are to relieve symptoms and restore normal anatomic relationships and visceral function. Preservation or restoration of satisfactory coital function, when desired, and a lasting operative result are also important goals.
Anterior colporrhaphy corrects anterior vaginal wall prolapse and helps support the urethra. It involves plication of the pubocervical fascia to support the bladder and urethra. When the anterior prolapse involves a direct detachment of lateral vaginal support, it is considered a paravaginal defect. Paravaginal defect repairs involve exposure of the retropubic space. Interrupted permanent sutures are used to reattach bilaterally the anterior superior vaginal sulci to the arcus tendineus fasciae (“white line”), extending from the ischial spine to the lower edge of the pubic ramus. When the defect is more central, a midline plication of endopelvic fascia is effective in adding support to the anterior vaginal wall. Polypropylene mesh may be used in appropriate patients to augment the weakened native tissue repair. In the presence of SUI, additional supportive measures are taken to achieve suspension of the bladder neck and proximal urethra.
Posterior colporrhaphy corrects a posterior vaginal wall prolapse and is similar in principle to anterior colporrhaphy. Site-specific posterior vaginal repairs can be performed after identification of the discrete endopelvic fascial breaks and reapproximation of this thicker tissue identified during rectal examination. Perineorrhaphy repairs a deficient perineal body. The outcomes of the site-specific repair are similar to the results of midline plication of the endopelvic fascia.
Recent modifications of these procedures involve the use of permanent suture or the addition of graft materials to augment the durability of the repair. These modifications can be accomplished using minimally invasive techniques such as endoscopic repair. Permanent mesh grafts are not recommended in the posterior compartment, because the incidence of complications is higher and outcomes are not as good as those achieved with repairs performed using native tissues.
When the uterus is present, hysterectomy may be performed to facilitate exposure of the apical support structures. Hysterectomy, however, is not an absolute requirement in settings where uterine removal is not otherwise indicated or desired. The repair of apical defects may require peritoneal entry for the repair of an enterocele. After identification of the enterocele, the contents are reduced, the neck of the peritoneal sac is ligated, and the defect is repaired by approximating the uterosacral ligaments and levator ani muscles to restore continuity in the endopelvic fascia. The uterosacral ligaments can be reattached to the cervix by either the vaginal or abdominal route.
Vaginal vault suspension (colpopexy) for apical prolapse is performed to secure a durable fixation point for the top of the vagina. This can be accomplished vaginally or abdominally by suspending the vaginal vault to the sacrum, the sacrospinous ligaments, the uterosacral ligaments, or other firm points of fixation. This can be done with natural existing tissues or with polypropylene mesh.
Robot-assisted surgery for POP may be performed when a stronger attachment is needed in a very active or relatively young patient or for a woman with a prior failed prolapse repair. Abdominal sacrocolpopexy with polypropylene mesh has been performed for over 30 years using an open incision, and more recently laparoscopically assisted procedures have been used. Since 2008, sacrocolpopexy has been performed with the aid of a surgical robot. This is a minimally invasive abdominal operation in which mesh is placed between the bladder and vagina, the rectum and the vagina, and over the apex of the vagina or the cervical stump. The mesh is supported by attaching it to the sacral promontory. The robot-assisted procedure is now considered to give the longest-lasting results for POP.
For women with advanced vaginal prolapse who no longer desire coital function, there are less invasive surgical options. A LeFort colpocleisis involves suturing the partially denuded anterior and posterior vaginal walls together in such a way that the uterus remains in situ and is supported above the partially occluded vagina. In women with posthysterectomy prolapse, a complete colpocleisis involves total obliteration of the vagina. These “obliterative” procedures have traditionally been reserved for elderly women who are not likely to tolerate more invasive reparative operations. Most of these women will get complete resolution of their symptoms with a repair that is much less invasive and is associated with fewer risks and complications.
Urinary incontinence is defined as the involuntary loss of urine that is a social or hygienic problem. Urinary incontinence has been reported to affect 15-50% of women. The problem increases in prevalence with age, rising above 50% in elderly persons in nursing homes. It is estimated that the direct financial cost of urinary incontinence in the United States is between $10 billion and $15 billion per year.
In the adult woman, the urethra is a muscular tube, 3 to 4 cm in length, lined proximally with transitional epithelium and distally with stratified squamous epithelium. It is surrounded mainly by smooth muscle. The striated muscular urethral sphincter, which surrounds the distal two-thirds of the urethra, contributes about 50% of the total urethral resistance and serves as a secondary defense against incontinence. It is also responsible for the interruption of urinary flow at the end of micturition.
The two posterior pubourethral ligaments provide a strong suspensory mechanism for the urethra and serve to hold it forward and in close proximity to the pubis under conditions of stress. They extend from the lower part of the pubic bone to the urethra at the junction of its middle and distal thirds.
The lower urinary tract is under the control of both parasympathetic and sympathetic nerves. The parasympathetic fibers originate in the sacral spinal cord segments S2 through S4. Stimulation of the pelvic parasympathetic nerves and administration of cholinergic drugs cause the detrusor muscle to contract. Anticholinergic drugs reduce vesical pressure and increase bladder capacity.
The sympathetic fibers originate from thoracolumbar segments (T10-L2) of the spinal cord. The sympathetic system has α- and β-adrenergic components. The β-fibers terminate primarily in the detrusor muscle, whereas the α-fibers terminate primarily in the urethra. α-Adrenergic stimulation contracts the bladder neck and the urethra and relaxes the detrusor muscle. β-Adrenergic stimulation relaxes the urethra and the detrusor muscle. The pudendal nerve (S2-S4) provides motor innervation to the striated urethral sphincter.
Afferent impulses from the bladder, trigone, and proximal urethra pass to the S2 through S4 levels of the spinal cord by means of the pelvic hypogastric nerves. The sensitivity of these nerve endings may be enhanced by acute infection, interstitial cystitis, radiation cystitis, and increased intravesical pressure. The latter may occur in the standing or bending-forward position or in association with obesity, pregnancy, or pelvic tumors.
Inhibitory impulses, probably relayed by the pudendal nerve, also pass to S2 through S4 following mechanical stimulation of the perineum and anal canal. Their passage may explain why pain in this region can cause urinary retention or urgency and frequency.
In infancy, the storage and expulsion of urine are automatic and controlled at the level of the sacral reflex arc. Later, connections to the higher centers become established, and by training and conditioning, this spinal reflex becomes socially influenced so that voiding can be voluntarily accomplished. Although organic neurologic diseases may interrupt the influence of the higher centers on the spinal reflex arc, patterns of micturition may also be profoundly altered by mental, environmental, and sociologic disturbances.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here