Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Successful treatment of pediatric solid tumors requires collaborative management by the disciplines of surgery, oncology, and radiotherapy. Multimodal therapy achieves the highest rate of cure in many solid tumors and often minimizes long-term morbidity. Smooth collaboration provides optimal care. The role of the surgeon varies greatly depending on the primary tumor, its site, and the presence or absence of metastatic disease. Surgeons should be involved in decisions regarding primary resection versus biopsy with neoadjuvant chemotherapy and delayed resection. The surgeon's knowledge of the risks of primary resection is critical; the method of biopsy is also very important. Inappropriate initial excisional biopsies with positive pathologic margins will require more extensive subsequent resection than if an initial incisional biopsy were performed. Similarly, inappropriate biopsies such as thoracoscopic biopsy of a chest wall Ewing sarcoma or a percutaneous or open biopsy of a Wilms tumor needlessly contaminate the thoracic and abdominal cavities, respectively, and require more intensive therapies, particularly the use of radiation therapy. A growing emphasis on minimizing the morbidity of therapy is required, because the survival for infants and children with many solid tumors is quite high. It is important, therefore, to avoid any diagnostic or therapeutic missteps that require more intensive therapy.
Surgery is critical in the staging of pediatric solid tumors. This is well established in Wilms tumor. In a classic study by Beimann Othersen and the National Wilms Tumor Study Group (NWTSG), surgeons had a 31.3% false-negative rate in their clinical assessment of lymph-node involvement with tumor by gross inspection and a false-positive rate of 18.1%. It should be stressed that in Wilms tumor the protocols of the NWTSG and the Children's Oncology Group (COG) determine the intensity of chemotherapy as well as whether or not abdominal radiotherapy is utilized. Patients with pulmonary metastases (stage IV) with local stage I or stage II tumors receive intensified chemotherapy and pulmonary radiation but no abdominal radiation.
The vital importance of adequate lymph-node biopsy has been demonstrated in several studies. An increased incidence of local relapse occurred in children enrolled in the NWTSG-4 study if no biopsy was performed of the abdominal lymph nodes, particularly in stage-I cases. This finding suggests that inadequate treatment of local disease in children without lymph-node biopsy results in an increased rate of local relapse. Although lymph-node biopsy is essential in children with Wilms tumor, an extensive retroperitoneal lymph-node resection has not been demonstrated to improve local control.
Lymph-node biopsy in patients with rhabdomyosarcoma is critical as well. The incidence of lymph-node involvement in rhabdomyosarcoma is determined by the primary site. Children without evidence of distant metastases have an overall 10% incidence of lymph-node involvement. It is most common in tumors arising in the prostate (41%), paratesticular (26%), and genitourinary sites (24%). Lesions in the extremities have an intermediate rate of 12%, whereas the orbit (0%), truncal sites (3%), and nonorbital head and neck (7%) have the lowest rate of lymphatic dissemination. In the extremity and genitourinary sites, assessment of lymph-node involvement is essential to ensure that radiation fields are appropriately designed and sufficiently inclusive. Whether the sentinel lymph-node biopsy technique optimizes the identification of nodal spread in rhabdomyosarcoma has not been established, but it has been reported to be feasible in pediatric patients with minimal morbidity. Although lymph-node biopsy is critical to identify the extent of spread, a lymph-node dissection should generally not be performed, because it may produce lymphedema that complicates radiotherapy and subsequent surgical resection of the primary tumor.
Radiographic assessment is inadequate for staging rhabdomyosarcoma as it is in Wilms tumor. In the Intergroup Rhabdomyosarcoma Study III (IRS-III), 121 boys with paratesticular rhabdomyosarcoma had a retroperitoneal lymph-node dissection to evaluate nodal status. The lymph nodes were assessed to be clinically negative based on computed tomography (CT) scan in 18% of the boys, 14% of whom had positive nodes when biopsy or retroperitoneal lymph-node dissection was performed. In the boys with clinically positive lymph nodes based on the CT scans, 94% were confirmed to be positive pathologically. Retroperitoneal relapse occurred in only two of the 121 boys, one of whom had pathologically negative lymph nodes and did not receive radiotherapy. Thus CT was very accurate if lymph-node abnormalities were identified, but it was not extremely sensitive in identifying nodal involvement. In a subsequent study, Weiner and colleagues reported an increased incidence of retroperitoneal relapse in children treated during IRS-IV. The use of abdominal radiation in this study was based on thin-cut CT scans in 98% of cases as compared with children treated during the preceding IRS-III, in which 94% had retroperitoneal biopsy or lymph-node dissection. In the subsequent study, IRS-IV, a decrease in stage-2 disease (positive lymph nodes) from 35% to 17% occurred when the staging was based on radiographic findings. This resulted in a decrease in the use of abdominal radiation in this cohort. The result was a fourfold increase in retroperitoneal lymph-node relapse. Another example of how critical adequate staging is to avoid local failure.
This chapter discusses some of the critical surgical issues in the treatment of infants, children, and adolescents with solid tumors. The use of anesthesia in patients with an anterior mediastinal mass, appropriate methods of biopsy, the role of neoadjuvant chemotherapy, limb salvage procedures for osseous tumors, and the management of pulmonary metastases are addressed.
Patients presenting with an anterior mediastinal mass pose a therapeutic challenge to the anesthesiologist and the surgeon. Correct diagnosis of the tumor provides the greatest chance of cure. There are, however, a plethora of reports in the anesthesia and surgical literature of patients with an anterior mediastinal mass suffering respiratory collapse upon the induction of general anesthesia. This occurrence has led to an understandable reluctance among anesthesiologists to use general anesthesia in this setting. Respiratory symptoms are a poor index of the risk of respiratory collapse, with the clear exception of orthopnea, which suggests a high risk that respiratory collapse will occur. An initial attempt to establish the radiographic parameters that would correlate with respiratory collapse upon induction of general anesthesia involved a retrospective evaluation of 74 adults with Hodgkin disease. In this study, the authors used the ratio of the transverse diameter of the mediastinal mass and the transverse diameter of the chest as the critical parameter. They found the incidence of respiratory collapse was 2.1% with a mediastinal mass less than 31% of the transverse diameter, compared with 10.5% for a mass with a ratio of 32% to 44% and 33.3% for a mass with a ratio greater than 45%. Similar results were reported by Turoff and associates.
Thorne Griscom and colleagues demonstrated that CT scan can accurately determine the tracheal dimensions in children and adolescents, and he established the normative values in children. Azizkhan first used this methodology in reviewing 50 children with anterior mediastinal masses. He found that 15 patients in his cohort had “marked” tracheal compression that was defined as a tracheal cross-sectional area less than 66% of predicted. When general anesthesia was induced in eight of these 13 patients, total airway obstruction occurred in five, all of whom had 50% or less of the predicted tracheal area. It was suggested, based on these findings, that general anesthesia should be avoided in children with less than 66% of the predicted tracheal area.
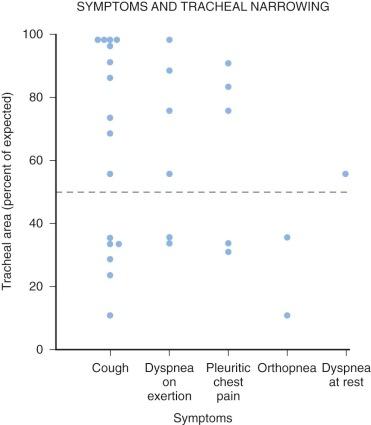
In a retrospective study at Boston Children's Hospital, 42 patients were identified who had an anterior mediastinal mass and a CT scan and underwent a surgical procedure. These patients were divided into those with tracheal area greater than 75% of expected (19 cases), those with 50% to 75% predicted area (16 cases), those with 25% to 50% (5 cases), and those with less than 25% (2 cases). One clear finding of that study was that the presence or absence of respiratory symptoms did not correlate well with the degree of tracheal narrowing shown by CT scan, except for orthopnea ( Fig. 49-1 ). General anesthesia with spontaneous ventilation was performed in four patients (with tracheal areas 33%, 73%, 76%, and 98% of predicted). General endotracheal anesthesia with paralysis was used in the remaining 32 patients, only three of whom had tracheal area of less than 50% of predicted (30%, 26%, and 24%). One patient received preoperative radiation therapy (26%). None of these 32 patients had symptoms of orthopnea or dyspnea at rest, and only one had dyspnea on exertion. All tolerated anesthesia without difficulty, and no patients suffered respiratory or cardiovascular collapse. Adequate material for pathologic diagnosis was obtained in all cases. It was concluded in this study that general anesthesia was safe in patients with tracheal areas greater than or equal to 50% of predicted.
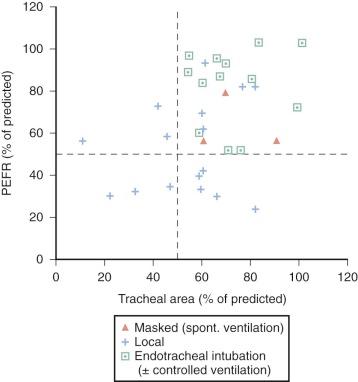
In a subsequent prospective study, 31 children with a mediastinal mass were evaluated with both CT scan and pulmonary function tests. Although the use of pulmonary function tests had been proposed by multiple investigators as a method to assess anesthetic risk, little evaluation of this modality had been performed. Miller and Hyatt evaluated the flow volume loop curves in a series of patients with intrathoracic and extrathoracic obstruction resulting from strictures of the trachea, malignant tumors, or bilateral vocal cord paralysis. The predominant distortion of the flow loops for intrathoracic obstruction was a marked reduction in the maximum expiratory flow rate. Hence in this prospective study, the peak expiratory flow rate was used as a critical factor. Patients with either a peak expiratory flow rate of less than 50% of predicted or a tracheal area of less than 50% of predicted had local anesthesia for their procedures. General endotracheal anesthesia was used only in patients with greater than 50% of predicted for both parameters. All patients in this study did well when general anesthesia was applied ( Fig. 49-2 ). Further analysis of this cohort revealed that patients with a tracheal area greater than 50% but a peak expiratory flow rate (PEFR) less than 50% had one of two problems: either a very low total lung capacity (38% and 55% of predicted) resulting from the massive size of the tumor or moderate to severe bronchial narrowing by qualitative estimation (four of these five patients) ( Fig. 49-3 ).

In a subsequent study by King and coauthors, 51 children with Hodgkin lymphoma and non-Hodgkin lymphoma (NHL) were evaluated. Respiratory symptoms were present in 49% of the children in this series and were more prevalent in children with non-Hodgkin lymphoma (76%) than in those with Hodgkin lymphoma (30%). The extent of aberration in the pulmonary function test was also worse in those with non-Hodgkin lymphoma. The first-second forced expiratory volume (FEV 1 ) was more affected in the group with NHL (mean value of 63 +/− 27% of predicted) compared with the children with Hodgkin lymphoma (mean value of 87 +/− 16% of predicted).
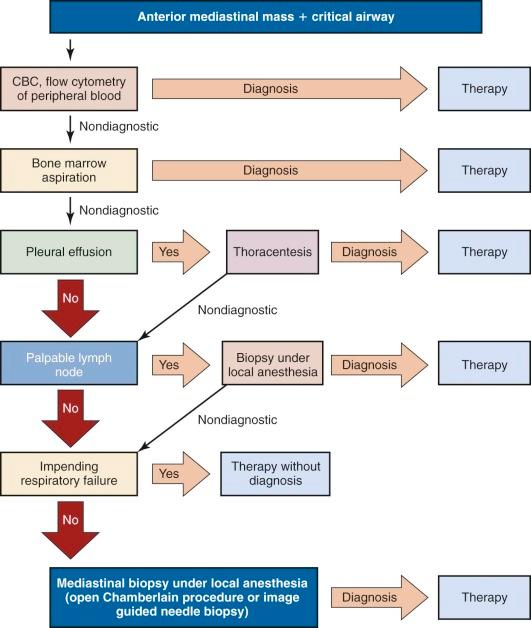
Patients with severe obstruction have one of three therapeutic options available. Patients can be treated in a preliminary fashion with either radiation therapy or steroids/chemotherapy for the most likely diagnosis based on the clinical findings ( Fig. 49-4 ). In a series of young adults who underwent a postradiation biopsy of an anterior mediastinal mass, a histologic diagnosis could not be obtained in eight of 10 patients because of extensive necrosis. In some cases, one area of tumor can be shielded for subsequent biopsy while the bulk of the tumor receives radiation. Non-Hodgkin lymphoma (NHL) is also extremely responsive to steroid therapy. Pretreatment with steroids also often obscures the histologic diagnosis.

The second option is aspiration of a pleural effusion if present. Patients with lymphoblastic lymphoma have a higher incidence of an associated pleural effusion (71%) than children with Hodgkin lymphoma (11.4%). Aspiration of the effusion in patients with lymphoblastic lymphoma is often diagnostic. Cells in the effusion can be assayed by immunocytochemical studies as well as by cytogenetic evaluation, immunophenotyping, and cytology.
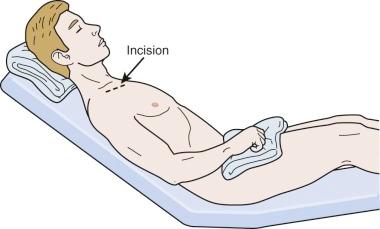
Third, in children with significant respiratory compromise and no pleural effusion and no lymph nodes palpable outside the chest, either a percutaneous needle biopsy under radiographic guidance or an open anterior thoracotomy (Chamberlin procedure) can be performed successfully when the child is under local anesthesia. Children should be seated in a semiupright position and spontaneously ventilating to maximize their pulmonary function ( Fig. 49-5 ). This position also decreases venous congestion if it is present. Spontaneous ventilation minimizes collapse of the trachea by the negative pressure exerted by the chest wall. It has also been shown that in children, image-guided percutaneous needle biopsy can in most instances provide a diagnosis. The major challenges have been in children with Hodgkin lymphoma, where initial biopsy was able to provide a conclusive diagnosis in only 50% of the children (six of 12). An algorithm for safe management of these children and adolescents is shown in Figure 49-6 . Following these guidelines for the use of general and local anesthesia and the biopsy techniques discussed, a biopsy can be obtained safely in essentially all children and adolescents with an anterior mediastinal mass.
A biopsy serves as the basis of diagnosis and treatment of a tumor. It will establish the prognosis and define the multimodality therapy required for cure. Beyond establishing the diagnosis, a biopsy may be required for several other important purposes in the delivery of modern oncological care: to confirm the presence of metastatic disease; to determine the response to treatment; and to document the presence of complications from treatment, especially suspicious lesions that may be infectious in nature and pose a significant risk to a patient with immunosuppression.
Five principles must be followed when considering a biopsy. First, to minimize the psychological and physical stress for the patient and family, the need for a biopsy, how it will be performed, and the possible complications must be discussed with the patient and family.
Second, a preprocedure conference between the oncologist, pathologist, radiologist, and surgeon must ensue to determine the best biopsy technique to obtain the required amount of tissue and that the tissue is processed appropriately (light microscopy, electron microscopy, cytogenetic and other biogenic marker evaluation, and immunohistochemical analysis) to provide the maximum information.
Third, the precise biopsy route and site must be selected to facilitate future therapy. The wrong incision or biopsy site can greatly complicate the subsequent “local” therapy, whether it be resection or radiotherapy. Factors that must be considered are local tissue trauma, risk of tumor spillage or hemorrhage, and minimal violation of anatomic planes.
Fourth, the patient's general state of health, past medical history, and immune status must also be considered to fully assess the physiologic impact of anesthesia and biopsy, including risk of hemorrhagic and respiratory collapse.
Lastly, the possibility of combining several invasive procedures into one anesthetic should be considered. For example, a patient that requires a biopsy of a lesion may also need central venous access or a bone marrow biopsy and aspirate, and these procedures could all be combined. Although the grouping of procedures is not always possible, it is an option that the oncologic team needs to discuss in advance and then present a uniform plan to the patient and parents.
The type of biopsy a patient requires varies greatly and is dependent upon the site of the mass, the characteristics of the lesion itself (cystic or solid), the condition of the patient, and the diagnostic possibilities. Once the decision has been made to proceed with a biopsy, the first technical question that must be answered is the amount of tissue required and what biopsy technique will avoid increasing the stage of the patient or complicate future therapy. The fundamental separation of techniques is into small- or large-specimen biopsies.
Small-specimen biopsies are those that are acquired through the use of hollow needles that sample an aspirate (fine needle aspiration [FNA]) or core (core needle biopsy [CNB]) of the tissue. They are often obtained with imaging assistance (ultrasound, fluoroscopy, or CT). The advantages of small-specimen biopsies are that they can often be performed with minimal or no anesthesia and are less invasive than an open procedure. Cost is also generally less for this approach, and recovery time for the patient is quicker. The disadvantages to this approach, however, are that the amount of tissue returned is quite small, which may create challenges in establishing a diagnosis or may not provide adequate tissue to complete the necessary secondary tests to adequately define the lesion. Furthermore, if imaging modalities are used to assist in this form of biopsy, then radiation exposure will occur if CT or fluoroscopy is used as opposed to magnetic resonance imaging (MRI) or ultrasound. This issue of radiation exposure is of extreme importance in the pediatric population, because there is an increased risk of developing a malignancy from radiation exposure. In addition, there is the possibility of tumor spread in needle tracts or hemorrhage. The risk of sampling error in which the specimen harvested may not adequately represent the entirety of the mass is always a concern with biopsies, and the smaller the sample, the larger the concern. Despite these limitations, small-specimen biopsies are an accepted standard of practice in pediatric oncology, and their use will be described in detail in the following section.
FNA specimens are acquired by using a 20- to 25-gauge needle connected to a standard syringe with the plunge partially withdrawn ( Fig. 49-7 ) . The needle is inserted directly into the lesion guided by palpation or with image guidance ( Fig. 49-8 ). Multiple passes are taken from the lesion as suction is applied to the syringe. Upon removing the needle, the contents of the syringe and needle are placed directly onto slides for cytological analysis. Multiple biopsies (3 on average) can be taken with this approach from the same lesion at the same time, and the cytological results are available for almost immediate review. However, no histologic assessment is possible using this technique, thus causing difficulty in diagnosing certain tumors with cytologic appearances that are quite similar, such as the small, round, blue cell tumors.

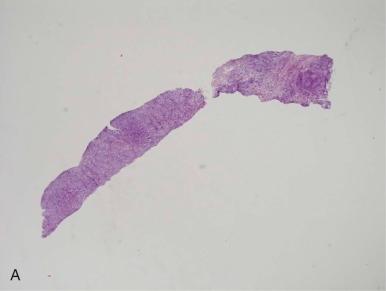
Histopathologic analysis is possible with a CNB. CNB specimens are retrieved using larger, hollow-bore needles (13- to 20-gauge) attached to spring-loaded devices that allow for one-step tissue harvest and extraction ( Fig. 49- 9 ). Image guidance is often used during this procedure, just as it is for the acquisition of FNA samples. The CNB device is often inserted through a coaxial sheath or cylinder that allows the operator to instill a coagulant into the tissue defects made by the CNB device to reduce the incidence of hemorrhage and tumor spillage ( Fig. 49-10 ). Generally multiple specimens (10 or more) from different areas of the lesion are gathered with this technique to minimize sampling error and to provide more tissue for complete pathological analysis. A representative example of the microscopic appearance of the biopsy specimens for FNA and CNB is shown in Fig. 49-11 . Imaging techniques can often distinguish areas with viable versus necrotic tissue to help identify the area best to biopsy.


The results and outcomes of small-specimen biopsies from almost any organ in the body have been reported extensively in adult patients with excellent diagnostic accuracy and minimal procedural morbidity. However, small-specimen biopsy techniques and comparison of these techniques in pediatric oncology patients, especially with abdominal lesions, have only recently gained widespread acceptance and usage.
Hugosson and colleagues in 1999 reviewed their series of image-guided percutaneous small-specimen biopsies in children from 1992 through 1996. A total of 90 biopsies (53 FNA, 37 CNB) were taken in 75 patients (mean age of 6.9 years). They compared the use of FNA with CNB (1.2 mm core specimens) under ultrasound guidance. Their cohort had many different malignant processes, and they obtained biopsies from the liver, kidney, adrenal gland, spleen, pelvic masses, and enlarged abdominal lymph nodes. Their FNA diagnostic accuracy was 77% (73% for malignant lesions and 83% for benign lesions) and 95% for CNB (93% malignant lesions and 100% for benign lesions). The complication rate was 8%. They concluded that CNB is a more accurate technique with a similar complication rate to FNA. These results were echoed by Hussain and colleagues, who examined their institutional experience on image-guided percutaneous biopsies (using CNB) in children (mean age, 4 years-old). Ninety-four percent of their cohort had abdominal or pelvic masses. Their reported diagnostic accuracy was 88%, and the initial diagnosis was subsequently confirmed by whole-specimen pathologic analysis. Their complication rate was approximately 8%, and they also concluded that CNB was generally successful in diagnosing tumors in children.
Sklair-Levy and colleagues published their institution's 10-year experience in small-specimen biopsies on pediatric patients. They performed 69 (62 CNB) biopsies in 57 patients using image guidance. Their diagnostic accuracy was 88.7% (55 of 62 patients). For malignant lesions, CNB had an accuracy of 98% as an isolated diagnostic technique in solid malignant tumors, although seven CNBs had to be repeated because the initial results were nondiagnostic. All seven repeated CNBs were correct on subsequent evaluation. They performed seven FNAs with a diagnostic accuracy of only 28%, and these patients then underwent surgical excision of the lesion in question. Although this accuracy rate is far lower than previously reported, none of the lesions in question were abdominal or pelvic masses, and the majority of these lesions were enlarged lymph nodes. Therefore direct comparison of the utility and diagnostic accuracy of FNA in this situation is not possible. Their accuracy with primary, metastatic, or recurrent lesions was in excess of 94% for all tumor types except lymphomas, for which they were correct only 60% of the time. Interestingly, they did not have a single complication.
A more comprehensive study was published by Skoldenberg and colleagues. They examined their institution's results with 147 CNBs in 110 children (mean age 4 years) from all anatomic sites (61 abdominal and pelvic lesions of the total 110 children). An overall accuracy of 89% was achieved for the CNBs performed. Twenty-four children required 37 additional biopsies for a nondiagnostic first specimen (12), a question of recurrence (22), and an insufficient quantity of tissue for all the diagnostic studies needed (3). They reported a sensitivity of 82% and a positive predictive value of 98.8%. A complication rate of 7% (10 of 141 cases) was seen, of which half were hemorrhagic in nature. Fourteen of the patients required narcotics for pain management postprocedure. A statistically significant difference in the occurrence of postprocedure pain was noted in older children. The authors strongly encourage the use of CNB in the diagnosis of pediatric malignancy, and they tout its superiority to FNA.
St. Jude's Children's Research Hospital published their experience of CNB in pediatric solid tumors over 5 years. Two hundred and two CNBs were performed using image guidance and anesthesia. Ultrasound was the predominant mode of imaging assistance (124 of 202), and the biopsies were performed to evaluate both primary and metastatic sites of disease. One hundred and three primary CNBs were performed with a 96.9% sensitivity, a 100% specificity, and an accuracy of 98%. For metastatic or recurrent lesions, they measured a sensitivity of 83.1%, a specificity of 100%, and an accuracy of 87.9%. There were no false positive results. In the cohort of patients with abdominal and pelvic tumors, the sensitivity and accuracy of CNB was 100%. They had a complication rate of 13.4%, with hemorrhage being the most common. Their results and experience across all anatomic regions and pathologic lesions demonstrate that small-specimen biopsies should be considered the initial diagnostic procedure of choice. Therefore solid masses in the pediatric population should be approached where indicated with image-guided small-specimen biopsies, especially using the CNB technique.
Finally, Sebire and Roebuck reported the results from a systematic literature review they conducted to determine the utility, success, and complications from image-guided CNBs. Echoing similar studies, they report that 94% of all procedures obtained adequate tissue for evaluation, and of that group an accurate diagnosis by histopathologic analysis was achieved in 94% with only a 1% complication rate.
Large-specimen tissue biopsies involve the removal of all (excisional) or part (incisional) of a lesion using an open or minimally invasive surgery (MIS) technique. This method of biopsy should not be confused with a formal extirpative procedure, because the surgeon does not remove either part or all of the entire mass with concerns about adequate margins of resection. The goal of these procedures is to remove a piece or all of the mass in question to provide tissue for a diagnosis, not for local control of the primary site. Large-specimen biopsies are also performed in anatomic areas or on lesions where image-guided small-specimen biopsies are more difficult because of proximity to major vessels or nerves, the lesions are very vascular, or the lesions cannot be reached without damaging overlying organs and structures (i.e., retroperitoneal lymph nodes). Large-specimen biopsies may be performed sequentially with a small-specimen biopsy using the same anesthetic if there is any doubt regarding the adequacy for a histopathologic diagnosis of the FNA or CNB.
Several disadvantages of large-specimen biopsies are a longer procedural and anesthetic time, recovery time, and need for hospitalization. They can delay the initiation of adjuvant therapies and are more costly. Assuming there are no complications, the vast majority of pediatric patients who have a small-specimen biopsy performed on a solid abdominal mass do not stay more than 8 hours postprocedure, as evidenced in recent large studies. The same cannot be said for large-specimen biopsies. Finally, operative exploration for large-specimen sampling can complicate definitive local-control therapies, especially from an operative standpoint. Violating the thoracic or peritoneal cavities induces adhesion formation that can complicate the subsequent resection.
Although significant disadvantages to large specimen biopsies exist, there are marked advantages. First, large biopsy samples are obtained, and multiple areas are sampled within the lesion, decreasing the likelihood of sampling error. Second, a detailed macroscopic evaluation of the lesion in question and all surrounding structures can be performed to search for extension or metastasis from the tumor. Third, radiation exposure is avoided for the patient and the healthcare team. Finally, hemostasis and tumor sampling is controlled and confirmed directly before closing the incision to minimize the complications of tumor spillage and hemorrhage.
In the last decade, several groups have reported success using a MIS approach for either incisional or excisional large specimen biopsies. The MIS approach relies on the same basic tenets of surgical discipline as does an open procedure, but it uses smaller incisions and advanced technology to achieve these goals. An operating telescope capable of excellent image resolution and magnification is used to display a picture on closed-circuit monitors. Dissection and biopsy is performed with long, fine instruments introduced through a percutaneously placed 2- to 12-mm canula. When operating in the peritoneal cavity, carbon dioxide gas (CO 2 ) is introduced by an insufflation apparatus that distends the abdominal wall to provide adequate space to assess the abdominal structures. The pressure is kept as low as possible, consistent with adequate exposure. An important point that must be discussed with the anesthesiologist is the degree of respiratory impairment that CO 2 insufflation may induce, especially in pediatric patients with extremely compliant diaphragms. If at any point the child becomes physiologically unstable, the CO 2 gas is released and the procedure is terminated. Advantages of the MIS approach are decreased postoperative pain from the small incisions, a shorter postoperative stay, improved cosmetic results, and an earlier return of bowel function. A complication rate in the pediatric population of 4% or less has been reported in a recent large series, but this rate is clearly related to the experience of the surgeon.
In 1973 Gans and Berci described their successful experiences with MIS in pediatric patients, but their procedures were not related to tumors. In fact, it was not until Holcomb and colleagues' report from the Surgical Discipline Committee of the Children's Cancer Group (CCG) in 1995 that the MIS approach was formally reviewed for its efficacy in oncology. In this study from 15 participating centers, 25 abdominal and 63 thoracic explorations were undertaken for the purposes of diagnosis (primary, relapsed, and metastatic lesions), staging, assessment of resectability, and the evaluation of treatment complications. All abdominal lesions (16), and 50 of 51 thoracic lesions that required biopsy were successfully diagnosed. There were no perioperative mortalities, and only seven complications—all in the thoracic cohort.
A prospective trial sponsored by the National Institutes of Health (NIH) concerning the use of MIS in pediatric oncology patients was begun by the combined Surgical Discipline Committees of the CCG and the Pediatric Oncology Group (POG) in 1996. The study failed for lack of accrual, and it was closed after 2 years. A questionnaire soliciting reasons for the failure of this study documented that lack of familiarity with the MIS technique by both the surgeon and the institution, surgeon and pediatric oncologist bias against the MIS technique, and the failure to submit the necessary paperwork to local institutional review boards for study approval were statistically significant factors in the study's failure. Despite these results, MIS is gaining acceptance in pediatric oncology, especially for the diagnosis of lesions.
Spurbeck and colleagues at the St. Jude's Children's Research Hospital recently published their experience with MIS in pediatric oncology patients from 1995 through 2000. One hundred and one patients underwent 113 operations (64 abdominal and 49 thoracic procedures). Abdominal biopsies were attempted in 25 patients and were successful in 23 (92%). Evaluation of resectability was determined successfully in two other cases, and seven extirpative procedures were performed. There were three complications in the abdominal group, and four MIS procedures were converted to open procedures. There were three complications reported in the abdominal cohort. The thoracoscopic procedures had similar rates of success, conversion, and complications. They reported no port-site recurrences or metastases in either the abdominal or thoracic cohorts of their study. Although a feared complication, the incidence of port-site recurrence is rare in thoracic cases (a single report by Sartorelli and colleagues). However, abdominal port-site recurrence rates are higher but depend on the tumor involved. Needless to say, these are retrospective data spanning many institutions, surgeons, tumors, and techniques. The conclusions reached by Spurbeck and colleagues attest to the safety and efficacy of MIS techniques in the successful diagnosis of pediatric tumors, but its use in the formal extirpation of tumors remains to be established.
A recent analysis by de Lijster and colleagues attempted to define the role for and success of MIS techniques versus open procedures in pediatric abdominal and thoracic tumors, but they discovered that there were no randomized controlled or controlled clinical trials on this topic in the literature. Hence no formal recommendation could be made as to the effectiveness, superiority or equivalency of MIS techniques versus open procedures in childhood tumors. Obviously this topic deserves greater scrutiny and investigation through the development and completion of a rigorous controlled trial as has been done in adults.
Biopsy of a soft-tissue or bone tumor in an extremity should be considered the first interventional procedure in limb salvage. Although the technical aspects are quite simple, the decision-making process is not. At risk are not only the patient's limb, but also overall disease control and outcome.
As noted, biopsy is truly a multidisciplinary process involving medical oncologists, surgeons, radiologists, pathologists, and radiation oncologists. Accuracy and outcome of biopsy procedures are improved when each of these specialists has a knowledge of musculoskeletal tumors and limb salvage principles. This is often best accomplished at tertiary centers with experience in the management of sarcomas.
The first step in planning a biopsy is performing a complete work-up. Based on history and physical examination findings, suspicion is raised about a tumor. Plain radiographs are often diagnostic of a bone malignancy and are crucial. MRI is also essential for both bone and soft-tissue tumors to define the extent of the tumor itself and involvement of neighboring compartments and neurovascular structures. It should be performed before biopsy to avoid artifact signal. Ultrasound is helpful to determine whether a soft-tissue mass is cystic or solid, but MRI is the gold standard for the evaluation of a suspicious mass.
Based on the findings from the work-up, a differential diagnosis can be established through collaboration at a multidisciplinary conference. All the specialists involved should be aware of the potential of a malignancy so that proper techniques are used for the procedure itself and for handling of the tissue. The biopsy approach is selected by the surgeon based on knowledge of limb-salvage surgery. The biopsy tract should be along the planned incision for limb salvage so that the entire tract can be excised later with the resection of the tumor. This is critical, because errors in placement of the biopsy incision can contaminate neurovascular and other important structures, making limb salvage impossible or necessitating large soft-tissue flaps for coverage. The tumor should be approached in the most direct manner and through a muscle, not in between muscles, to decrease contamination of normal tissue.
Biopsy of an extremity tumor can be performed by open or closed (CNB) techniques ( Table 49-1 ). Open biopsy offers the advantage of a larger tissue sample so that adequate pathologic evaluation can be performed. However, the major disadvantages are a higher risk of contamination of critical structures and complications such as bleeding, infection, and pathologic fracture. It is also more expensive and requires more time. Incisional biopsy is performed by entering into the tumor itself and removing a small section of it. The pseudocapsule is repaired, and careful hemostasis is obtained to try to decrease tumor-cell spillage or creation of a hematoma. Excisional biopsy involves removing the whole tumor in one piece. This is rarely indicated for extremity tumors, because resection surgery for malignant tumors is so vastly different from that for benign tumors. Also, most musculoskeletal tumors are treated with neoadjuvant therapy before excision. This approach is used for two reasons. First, it will increase the ability to perform limb-salvage surgery. Second, it provides an in vivo assay of response to standard chemotherapy (see Neoadjuvant Therapy for Solid Tumors ).
| Open | Needle | |
|---|---|---|
| Sample size | Larger | Smaller |
| Accuracy | Higher or equivalent | Lower or equivalent |
| Morbidity | Higher | Lower |
| Risk of contamination | Higher | Lower |
| Complications | Higher | Lower |
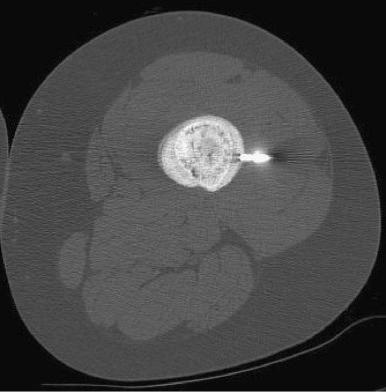
Needle biopsy on the other hand is associated with less morbidity for the patient. It carries a lower risk of complications and contamination and is often simpler to perform. However, the smaller tissue sample size is a disadvantage and decreases the accuracy rate of the diagnosis. Use of a large-bore needle to remove a core of the tumor is thus usually more advantageous than FNA, as discussed. Sampling error is another disadvantage of CNB. Image-guidance with CT ( Fig. 49-12 ) or ultrasound improves accuracy and decreases sampling error, but it is imperative that the surgeon discuss the approach with the radiologist performing the procedure. There is a risk of local recurrence if the needle biopsy tract is not excised with the tumor, but the risk is probably less than with open biopsy.
Pathologic analysis also requires specific knowledge of musculoskeletal tumors, especially with smaller sample sizes. The specialist obtaining the biopsy should discuss the case with the pathologist. A frozen section at the time of biopsy is essential, not for definitive diagnosis, but to ensure sufficient neoplastic tissue is available to the pathologist to make a diagnosis. Proper tissue handling is also crucial for the pathologist to be able to arrive at the correct diagnosis. Hematoxylin and eosin staining as well as most immunohistochemistry can be performed on tissue placed in standard formaldehyde. However, electron microscopy, cytogenetic investigation, tissue culture, flow cytometry, and immunofluorescence all require special handling and often fresh tissue. The discovery of specific cytogenetic abnormalities in certain tumors (e.g.,, t[11;22] in Ewing sarcoma [EWS] and t[2;13] in alveolar rhabdomyosarcoma) has increased the ability of pathologists to make the diagnosis with small tissue samples, but they must be processed in the correct manner.
Combined discussion of the pathology completes the biopsy process. The multidisciplinary team caring for the patient can then review all of the staging studies with the known diagnosis in mind and arrive at a recommendation for treatment.
Cooperative group trials by the NWTSG in North America, the International Society of Paediatric Oncology (SIOP) in Europe, and the United Kingdom Children's Cancer Group (UKCCG) have provided a great wealth of information regarding the optimal management of Wilms tumor. A major difference in approach exists between SIOP and NWTSG. In North America, primary resection followed by chemotherapy and radiotherapy is favored. In the SIOP studies, children generally first receive either chemotherapy or radiotherapy followed by resection. This approach has been driven by a high incidence of operative tumor rupture in their early series. In SIOP 1 the use of preoperative radiation therapy (20 Gy) was randomized versus primary resection. The rate of intraoperative rupture decreased from 33% to 4% with the use of radiation. Survival was not affected, and the incidence of local recurrence was not reported. The frequency of operative rupture that occurred in NWTS 1 and 2 were 22% and 12%, respectively. In a subsequent SIOP study, preoperative therapy was randomized between abdominal radiation (20 Gy) and actinomycin D compared with those receiving vincristine and actinomycin D. The frequency of rupture was 9% and 6%, respectively.
In SIOP 6, which started in 1980, all patients received initial preoperative chemotherapy (vincristine and actinomycin D). Radiotherapy was given after resection to children with stage II N1 and stage III disease. Children with stage II N0 disease were randomized to receive either 20 Gy abdominal radiotherapy or no radiation. All children received vincristine and actinomycin D for 38 weeks. The radiotherapy randomization was halted after 123 children were randomized, 64 to radiotherapy and 59 to chemotherapy alone. Six of the 59 children who did not receive radiotherapy had local recurrences, whereas no recurrences occurred in the group who did. These findings suggest that prenephrectomy treatment altered the pathologic findings that would have led to a diagnosis of stage II N1 or stage III disease (i.e., lymph-node involvement or capsular penetration), resulting in the standard administration of local radiation. No statistical difference in survival has been seen in these children after extended follow-up observation, because those who relapsed had treatment alternatives.
In SIOP 9, which began in 1987, preoperative therapy was randomized between 4 and 8 weeks' duration. The goal was to produce a larger proportion of stage I tumors. In this study, postoperative radiotherapy for children whose disease was stage II N0 was replaced with an anthracycline (epirubicin or doxorubicin). Preoperative treatment for patients without distant metastases consisted of four weekly courses of vincristine and three 2-day courses of actinomycin D every 2 weeks versus 8 weeks of the identical therapy. There was no advantage seen from the extended therapy in terms of staging at resection (stage I, 64% versus 62%) or in intraoperative tumor rupture (1% versus 3%). Therapy after resection was based on the pathologic findings. In SIOP 9, the surgery-related complications were reported to be 8%.
In both the NWTSG protocols and those of the COG, primary surgical resection is generally recommended. There are certain generally accepted situations where preoperative therapy is appropriate. These include the occurrence of Wilms tumor in a solitary kidney, bilateral renal tumors, and respiratory distress from extensive metastatic disease in the lungs. In these cases pretreatment biopsy should be obtained, and percutaneous biopsies are often used. Although needle tract seeding has been reported, this is quite rare in Wilms tumor. The aim of neoadjuvant treatment in the bilateral tumors and solitary kidney is to preserve the maximum amount of renal parenchyma and function. Current COG protocols for bilateral renal tumors have intensified the neoadjuvant therapy to include three agents (vincristine, actinomycin D, and doxorubicin) with each cycle of therapy. The duration of therapy has also been limited to avoid incremental increases in the intensity of therapy when further regression in the size of the tumor is unlikely.
The efficacy of preoperative treatment to achieve partial nephrectomy in patients with unilateral Wilms tumors has been evaluated by several centers. McLorie and associates in Toronto obtained percutaneous biopsy in 31 children with Wilms tumors. Multiagent chemotherapy was then administered for 4 to 6 weeks. Partial nephrectomy was performed in nine children (four with unilateral tumors and five with bilateral tumors). Two of these children suffered an intraabdominal relapse, and only four of the 30 unilateral tumors (13.3%) were amenable to partial nephrectomy. Hence in unilateral cases not identified by prospective radiographic imaging in patients with syndromes, a partial nephrectomy is rarely possible even with preoperative therapy. Another assessment of the feasibility of partial nephrectomies was performed at St. Jude Children's Research Hospital. The preoperative CT scans of 43 children with nonmetastatic unilateral Wilms tumor were reviewed. The criteria used to define those tumors suitable for partial nephrectomy were involvement by the tumor of one pole and less than one third of the kidney, a functioning kidney, no involvement of the collecting system or renal vein, and clear margins between the tumor and surrounding structures. Only two of 43 scans (4.7%) met the criteria, suggesting that a partial nephrectomy was feasible. The primary concerns regarding the administration of preoperative chemotherapy (as in the studies of Kozzi and associates and Moorman-Voestermans and co-workers) to create “resectable” small tumors is that these children may be curable by surgical resection alone without subjecting them to the toxicity of additional treatments.
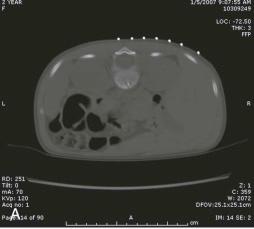
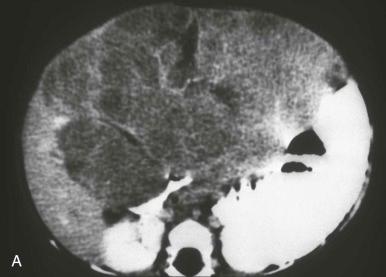
The surgical resectability of Wilms tumors has been poorly correlated with radiographic studies. In fact, extremely large tumors can be stage II lesions and be fairly safely resected ( Fig. 49-13 ). The surgical recommendations in the NWTSG studies have been that if resection of the tumor would involve resection of adjacent organs (i.e., liver, pancreas, or spleen) because of adherence, biopsies should be obtained and subsequent chemotherapy applied before resection, because such resections are associated with an increased rate of complication ( Fig. 49-14 ). Complications in the NWTSG-4 study have been assessed. Complications occurred in 12.7% of a random sample of 534 of the 3335 patients enrolled on the study. Intestinal obstruction was the most common complication (5.1%), followed by extensive hemorrhage (1.9%), wound infection (1.9%), and vascular injury (1.5%). Factors associated with an increased incidence of complication included intravascular extension into the inferior vena cava or atrium and nephrectomy performed through a flank or paramedian incision. Tumor diameter greater than or equal to 10 cm was also associated with increased complications. In SIOP 9, complications occurred in 8% of 598 patients. These patients were pretreated with vincristine, actinomycin D, and epirubicin or doxorubicin before nephrectomy. Their complications included small bowel obstruction in 3.7% and tumor rupture in 2.8%. The latter is not reported as a complication in the NWTSG reviews.


Surgery plays a primary role in the treatment of low-stage neuroblastoma. Tumors that the surgeon deems readily resectable should generally have a primary resection for staging and to establish both the diagnosis and the biologic risk factors of the tumor. In many children with small tumors and favorable biologic factors, surgery is the only therapy required. Resection is generally accepted before administration of chemotherapy for most thoracic, pelvic, and cervical primaries and limited abdominal lesions that do not extend across the midline. This approach is used to avoid the toxicity of chemotherapy, and in many patients with low-stage favorable biology tumors, resection alone is curative. In those situations where resection would entail removal of vital organs or where there is extensive lymph-node extension, preliminary treatment with adjuvant chemotherapy, particularly in the biologically adverse tumors, would be most appropriate. In patients with favorable biologic features, even subtotal resection may be the only therapy required.
Of note, however, is the report by Nuchtern and colleagues documenting the results of the COG trial on expectant management in infants (younger than age 6 months) with small adrenal masses. Eighty-seven cases were enrolled, and four patients were elected for upfront surgery. Of the remaining cohort, only 16 other patients had their adrenal lesions resected, with neuroblastoma diagnosed in 10 children, low-grade adrenocortical tumors in two, adrenal hemorrhage in two, and extrapulmonary pulmonary sequestrations in two. The overall, 3-year survival rate in the entire cohort was 100%, with a neuroblastoma event-free survival (EFS) of almost 98%. These results are quite encouraging in defining a cohort of children who can be spared any treatment for small adrenal-based neuroblastomas, but the suitable application of these data to nonadrenal primary sites, larger tumors, and in older children remains to be determined.
Regrettably, the majority of infants and children have metastatic disease at diagnosis. In these cases, the diagnosis and biologic features must be established. Tissue may be obtained by either laparotomy or thoracotomy, as well as by laparoscopy and thoracoscopy. In older patients with metastatic disease where Shimada staging is not required to determine the patient's treatment, needle biopsy from either bone marrow or the primary metastatic tumor provides adequate material for both pathology and biologic grading. For patients in whom the Shimada criteria are critical to determine their therapeutic treatment, open or minimal access surgery is required to obtain adequate tissue.
In patients with extensive abdominal primary tumors, adjuvant therapy has been useful. It is well recognized by surgeons that preoperative chemotherapy decreases the vascularity and friability of the tumor and facilitates resection, particularly in developing the dissection plane between the tumor and the great vessels. Lymph-node involvement surrounding the aorta, vena cava, and renal vessels is often seen in children with advanced stage abdominal adrenal or paravertebral primaries ( Fig. 49-15 ).

Although two studies have shown no difference in the surgical complication rate between initial and postinduction resection, others have demonstrated a higher incidence of complications, including nephrectomy in the group undergoing primary resection. Furthermore in patients with high-risk tumors who often require autologous bone-marrow transplant, preservation of the ipsilateral kidney during the resection is critical. A neoadjuvant approach has contributed to decreased operative complications requiring nephrectomy.
A multiinstitutional review of children treated over an 11-year interval demonstrated a 14.9% incidence of nephrectomy or renal infarction as a result of surgery for local control (52 of 349 children). There was a 25% incidence among those with initial resection (29 children) and a 9.9% incidence in the postchemotherapy resection (23 children). Children with initial resection had more than a twofold increase in their risk of nephrectomy. Hence the approach for neuroblastoma regarding primary lesions is quite different from that in Wilms tumor. The other determining factor is that the pathologic staging information is not as critical for determining local control in neuroblastoma as in Wilms tumor, and essentially all of these children with large primary lesions require adjuvant chemotherapy and radiation. Hence administration preoperatively in no way increases the chance that chemotherapy will be required and is generally recommended in most current protocols.
Of note, however, is the report from Simon and colleagues reporting the results of the German cooperative trial NB97 that evaluated the role of surgery (upfront and postneoadjuvant therapy) in patients older than 18 months with stage IV disease. In this study, 278 patients were evaluated, and their data report that neither upfront surgery nor operations performed postneoadjuvant chemotherapy positively impacted EFS, local progression-free survival (LPFS), or overall survival (OS). They concluded their manuscript by calling into question the role and utility of surgery in this patient cohort secondary to the lack of compelling data supporting effective local control or survival rates. Obviously, more data are required to definitively answer these questions.
Surgery is the cornerstone in the treatment of hepatoblastoma, and children are rarely cured without resection. Neoadjuvant and adjuvant chemotherapy facilitates its feasibility and success. Historically, resection with complete removal of all radiographically identifiable disease cured only 25% of children; 50% of children who presented with hepatoblastoma had resectable lesions, and of those only 50% survived. Failure was attributed to occult metastatic disease not identified radiographically, and Weinblatt and colleagues reported the early success of neoadjuvant chemotherapy to convert unresectable liver tumors to resectable lesions with more than 75% of the lesions becoming resectable in both series ( Fig. 49-16 ). Only children with tumors with pure fetal histology do not require adjuvant therapy. Subsequent reports document the utility of various chemotherapeutic regimens in hepatoblastoma to treat unresectable lesions or residual disease. These reports establish the efficacy of doxorubicin, cisplatin, vincristine, and 5-fluorouracil alone or in various combinations. Cisplatin has been shown to be as efficacious as cisplatin with doxorubicin for standard-risk hepatoblastoma. Furthermore both adjuvant and neoadjuvant regimens in combination with surgery achieved survival rates greater than 65% and tumor response rates greater than 90%. Although the regimens varied, most patients received at least two cycles before definitive surgery. The extent of tumor necrosis has also been shown to predict survival, as does negative surgical margins. The critical need for resection of the primary tumor before the development of chemoresistance was demonstrated by von Schweinitz and colleagues. They documented tumor regrowth as early as after the fourth course of therapy in 6 of 11 patients. Five-year survival rates for all patients with hepatoblastoma increased in just 2 decades to over 85% with the use of neoadjuvant and adjuvant chemotherapy.
Since 2000, a defined treatment protocol consisting of neoadjuvant chemotherapy and surgical resection or early orthotopic transplant evaluation for those patients with tumors that are too extensive to resect has been developed and reported by the SIOP Liver Tumor Group (SIOPEL). This regimen was termed PLADO, and it consisted of a pretreatment imaging-defined staging protocol (PRETEXT), pretreatment diagnostic biopsy (core needle or incisional biopsy), neoadjuvant chemotherapy of continuous infusion cisplatin (day 1) followed by continuous infusion of doxorubicin (days 2 and 3), surgical resection after 4 to 6 cycles 12 to 20 weeks from diagnosis, and orthotopic liver transplant (OLTX) evaluation and referral for tumors confined to the liver that remained unresectable despite chemotherapy. The only tumors resected primarily were those deemed to be confined to a single section of the liver (i.e., right anterior, right posterior, left medial, left lateral; PRETEXT stage I). The overall 5-year survival rate was 75% for the entire cohort and 85% for those following the complete protocol, including neoadjuvant chemotherapy regardless of PRETEXT stage. PRETEXT stages I through IV had OS rates of 100%, 91%, 58%, and 57%, respectively, which compares favorably with survival rates achieved by Ortega and colleagues through a CCG/POG cooperative trial comparing multimodality treatment protocols utilizing different chemotherapeutic regimens. Surgical mortality was 6%, and overall mortality was 24%. Twenty percent of patients had pulmonary metastases. Ninety-two percent of patients had a complete resection with this protocol, and there were 10 patients who relapsed: five with local recurrences and five with pulmonary metastases. SIOPEL's use of OLTX as primary treatment for local control was published by Otte and colleagues. Those patients whose tumors involved all sectors of the liver or were intimately involved with either the hepatic or portal veins but had no evidence of metastatic disease and demonstrated some response to neoadjuvant chemotherapy were considered for a primary OLTX. Another cohort of patients who had intrahepatic recurrences of disease after resection or incomplete resections was eligible for rescue OLTX. Ten-year survival rates for the primary and rescue OLTX groups were 85% and 40%, respectively. The authors advocated, based on their results, for the following: 1) total resection of all gross disease including the retrohepatic vena cavae if needed; 2) the use of preoperative chemotherapy to control extrahepatic micrometastases and promote primary tumor regression; 3) transplantation for patients with synchronous pulmonary metastases if they had responded to neoadjuvant therapy; 4) no transplantation for those patients with evidence of metastatic disease present at surgery; 5) limiting the interval between diagnosis and OLTX to account for the rise of chemoresistance and the availability of donors (cadaveric or living); and 5) questioning the need of post-OLTX chemotherapy in the setting of a patient with immunosuppression. Although their cohort was small (12), they reviewed the world's experience with OLTX for hepatoblastoma in the same report, and the results were similar. As a corollary to this report, Austin and colleagues reported on the experience of the United Network of Organ Sharing (UNOS) for 152 OLTXs performed in 135 patients in the setting of hepatoblastoma. Their actuarial 1-, 5-, and 10-year survival rates were 79%, 69%, and 66%, respectively. More than 54% of patients died of recurrent disease, and the only statistically significant predictors of favorable outcome were the preoperative condition of the patient (intensive care unit [ICU] hospitalization versus non-ICU hospitalization versus no hospitalization) and the era when the patient received the transplant (before or after December 31, 1994). These reports document not only the feasibility but also the success of OLTX as a component in the multimodality treatment of hepatoblastoma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here