Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Unlike adults, most cardiac arrests in children arise from respiratory etiologies. Therefore, emphasis is first on oxygenation and ventilation.
Detection of a child’s pulse may be difficult; if a brachial pulse is not definitively present after 10 seconds of palpation, initiate cardiopulmonary resuscitation (CPR).
Hypotension is a late finding in pediatric shock and requires immediate intervention to prevent cardiac arrest. Progression from tachycardia to bradycardia in a child is often a harbinger of imminent arrest.
Although few studies support recommendations for exact rate, depths, and ratios of compressions to ventilations in pediatric CPR, emergency clinicians should perform rapid compressions over the lower sternum with minimal interruptions. The hand encircling technique is recommended for infants requiring chest compressions and the two-hand approach in mid sternum for older children. In the emergency department (ED), we recommend 15 compressions to 2 ventilations for children less than 8 years and 30 compressions to 2 ventilations for older children.
Verbal and quantitative feedback improves compressions and ventilations.
Advanced airway management (i.e., endotracheal intubation) may be harmful for children in arrest in the ED. If attempted, physicians should strive for minimal interruptions in compressions and to ventilate at 8 to 10 breaths/min. High quality bag-mask ventilation is a reasonable alternative to advanced airway maneuvers.
If ventricular fibrillation or pulseless ventricular tachycardia arise, defibrillate at 2 J/kg as soon as possible. While preparing the equipment and charging, continue to perform high quality compressions. Administer subsequent defibrillations at escalating energy doses of 4 J/kg and then 10 J/kg.
Early administration of epinephrine for non-perfusing rhythms may improve survival.
Empiric administration of medications to children in arrest worsens outcomes. Reserve medications for specific indications, for example, bicarbonate administration for hyperkalemia.
Knowledge of the child’s approximate weight is necessary to administer the appropriate medication doses and to utilize the appropriate equipment. Determine actual weight in kilogram and estimate weight based on parental report or the child’s length.
Prompt vascular access is critical in a resuscitation. Intraosseous access tends to be the easiest and fastest, but care should be taken that the needle is not residing in the subcutaneous tissue. Central venous access is resource intensive and not necessary in the first few hours of a resuscitation.
Except in specific circumstances, resuscitations greater than 30 minutes are unlikely to yield favorable outcomes for pediatric arrest.
After return of circulation, maintain normothermia and avoid hypotension.
Current definitions of sepsis are based on consensus and primarily for research purposes.
Systemic inflammatory response syndrome (SIRS) criteria are sensitive but not specific for identifying sepsis in children.
Hypotension should prompt administration of 20 to 60 mL/kg fluids and likely vasopressors.
Most children with septic shock have cold shock and therefore epinephrine (0.05 mcg/kg/min) is the first line vasopressor.
Protocols bundling intravenous fluids, antibiotics, and blood culture acquisition in septic children improve outcomes.
Brief resolved unexplained events (BRUEs) involve alterations in breathing, tone, or behavior that last less than 1 minute before resolving spontaneously. Children appear well on presentation to the ED, and there are no elements of the history that suggest a particular etiology for the event.
Low-risk BRUEs occur in children that were born greater than 32 weeks, are greater than 60 days of age, have had no prior BRUEs, and CPR was not required during the event. These children require an assessment and brief observation in the ED, little or no diagnostic testing, and may be discharged with close follow-up.
Pediatric cardiac arrest is rare, but the consequences are dire when considering lost years of life and productivity. The incidence and survival of pediatric cardiac arrest varies with the location of the arrest, the patient’s age, and the mechanism ( Table 158.1 ). Most cardiac arrests encountered in the emergency department (ED) occur outside the hospital, from medical causes in infants and traumatic causes in older children. In children, cardiac arrest is most prevalent in infants, occurring primarily in children less than 3 months of age. The incidence of atraumatic cardiac arrest in older children is 30 to 50 times less common than infants and adults. Overall, survival following cardiac arrest in children is low; however, it is improving, and certain groups have higher likelihoods of survival. Infants survive infrequently (6%) but older children survive (14%) comparably to adults (11%). The frequency of survival with good neurologic outcome has been estimated at 6% to 12%.
| Infant | Child | Adult | |
|---|---|---|---|
| Incidence (per 100,000) | 75 | 5 | 141 |
| Survival (%) | 6 | 14 | 11 |
| Etiology | Respiratory | Respiratory > Trauma | Cardiac |
| Rhythm | Asystole, bradycardia | Asystole | Ventricular fibrillation or tachycardia |
| Early Focus | Compressions, Ventilations | Defibrillation | |
| Location for pulse check | Brachial | Carotid | Carotid |
| Compression technique | Hands encircling chest | 2 hands | 2 hands |
| Compression depth | 1.5 inches | 2 inches | 2 inches |
| Defibrillation dose (monophasic) | 2J/kg, then 4J/kg, and then 10 J/kg | 200 J | |
| Epinephrine dose | 0.1 mg/mL | 0.1 mg/mL | |
Pediatric resuscitations are relatively rare, limiting clinicians’ proficiency. In a review of resuscitations at a busy pediatric ED, less than half of emergency physicians had completed any critical care procedures (e.g., cardioversion, intubation, intraosseous line placement) in the preceding year. No physicians had performed cardiac pacing, needle cricothyroidotomy, diagnostic peritoneal lavage, thoracentesis, arterial line placement, and venous cutdown line placement. In the absence of actual clinical experience, emergency clinicians often rely on didactic resuscitation courses. However, knowledge retention after these courses is poor. As a result, many emergency clinicians remain uncomfortable managing critically ill children. This discomfort can lead to insufficient interventions for fear of harming a child, or alternatively, excessive interventions that stress resources, families, and clinicians.
Most atraumatic cardiac arrests in children arise from respiratory etiologies, particularly respiratory failure, drowning, and asphyxia. Children commonly progress from respiratory failure to shock, and finally to bradycardia and loss of circulation. Pediatric advanced life support (PALS) guidelines have largely focused on the treatment of these respiratory emergencies. However, population-based studies suggest cardiac causes account for approximately a third of pediatric medical arrests. Another 21% of pediatric arrests follow trauma. These frequencies are in stark contrast to adults, where two-thirds of arrests are attributed to cardiac etiologies. The differences in the etiology of arrests between adults and children have significant implications for management; arrests from respiratory causes require an emphasis on ventilatory support, oxygen delivery, and maintenance of perfusion, whereas arrests from cardiac causes require a more directed emphasis on restoring perfusion and treatment of underlying dysrhythmias (see Table 158.1 ).
The most common presenting pediatric arrest rhythm is asystole, occurring in two-thirds of children. Pulseless electrical activity and bradycardia are the next most common presenting rhythms. Unlike adults, ventricular fibrillation and tachycardia are rare, occurring in 9% of children in cardiac arrest. These dysrhythmias can arise with prolonged resuscitation and are more common in adolescents and children with congenital heart disease.
With return of circulation after cardiac arrest, reperfusion induces a cascade of physiologic changes that increase morbidity. During the initial minutes after return of circulation, there is not adequate substrate for aerobic metabolism leading to accumulation of free radicals and cellular necrosis. Children may also develop a sepsis like syndrome, with increased cytokines and endotoxin producing capillary leak and coagulopathy. This may lead to hypotension and multiple organ dysfunction. In the hours following return of circulation, nearly half of children may also develop reversible myocardial dysfunction, producing pulmonary edema, hypotension, or arrhythmias.
The absence of a pulse, respiratory effort, and responsiveness constitute cardiac arrest. While identifying respiratory effort and responsiveness are relatively straightforward, detecting a pulse in a pediatric patient can be difficult. Physicians identified the presence of a pulse when one was not present in one quarter of children undergoing extracorporeal membrane oxygenation (ECMO). Moreover, emergency clinicians require extended time to determine if a pulse is present in a child, with an average of 9 (±6) seconds to detect a brachial pulse and 29 (±14) seconds to determine that a pulse was not present. Current guidelines suggest lay people should initiate cardiopulmonary resuscitation (CPR) in children without performing a pulse check; any child that is unresponsive and apneic should receive CPR. For emergency clinicians, if no pulse is detected in 10 seconds, CPR should be initiated without delay; the adverse effects of delayed CPR outweigh the effects of CPR for an apneic, unresponsive child with a weak pulse.
The ideal location for palpation of a child’s pulse is unclear. There are few studies comparing sites, and they are conducted in the operating room with conflicting results. In infants, the carotid pulse can be difficult to detect compared to the brachial or femoral pulse. In adolescents, the carotid is the easiest location to identify a pulse. In children in cardiac arrest, auscultation of the heart or palpation of the apical impulse can be misleading; patients with pulseless electrical activity can have an apical impulse or auscultated heartbeat without central pulses or adequate perfusion.
Anticipating impending cardiac arrest allows for early interventions that may prevent progression. Abnormal vital signs, based on age-specific norms, are often the best indicator of imminent arrest in an ill child. These values can be difficult to remember, but physicians can recognize several key features ( Box 158.1 ). While tachycardia and tachypnea are commonly present in children with relatively benign febrile illnesses, hypotension or ill appearance should prompt immediate intervention.
Systolic blood pressure <70 mm Hg + (2 × age in years) is hypotension (less than fifth percentile for age)
Respiratory rate >60 breaths/min is tachypnea
Declining respiratory rate in previously tachypneic patient can represent improvement or fatigue and imminent respiratory failure
Each 1°C (1.8°F) of fever increases heart rate by only 10 beats/min and respiratory rate by 2–5 breaths/min
Progressive increase or decrease precede desaturation and respiratory failure
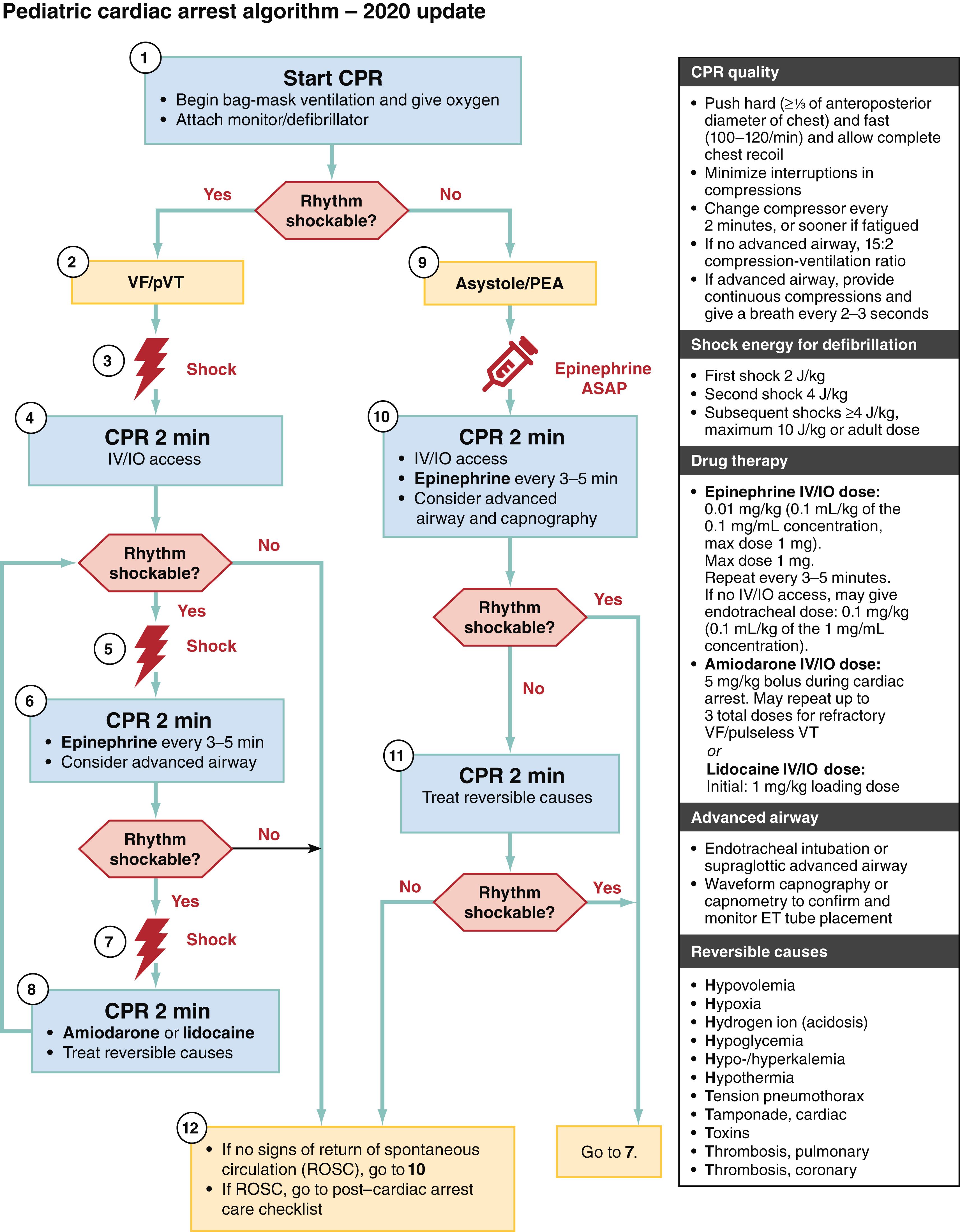
The paucity of pediatric out-of-hospital cardiac arrests limits available evidence on its management. Most pediatric guidelines are consensus-based and much is extrapolated from adult data. The American Heart Association (AHA) guidelines for management are illustrated in Fig. 158.1 . Neonatal resuscitation guidelines (see Chapter 159 ) should be used for newborns and for neonates within the first weeks of life, after which these pediatric guidelines are applicable for children until puberty (i.e., axillary hair in males and breasts in females).
During the initial no-flow state of cardiac arrest, the priority is initiation of flow. This priority has prompted a change in the sequence of “airway-breathing-compressions (A-B-C)” to “compressions-airway-breathing (C-A-B).” This avoids delays in the initiation of blood flow and may render bystanders to an arrest more likely to provide CPR. This is particularly helpful in children; bystander CPR improves pediatric survival but is infrequently administered. Although the A-B-C approach is still considered preferred in children, it is feasible to begin with the C-A-B approach and still provide timely ventilations; a simulated pediatric respiratory arrest model found no delays in the initiation of ventilations with the C-A-B approach compared to the A-B-C approach. Moreover, the C-A-B approach led to prompter recognition of cardiac arrest. If untrained bystanders are reluctant to provide ventilations, children with out-of-hospital cardiac arrest should still receive chest compressions without delay. In the ED, with multiple professionals available, compressions should be administered concurrently with ventilations.
High quality compressions improve outcomes but are rarely performed. When administered appropriately, compressions generate one-third of a child’s normal cardiac output and a coronary artery perfusion pressure of 10 mm Hg. In a prospective, observational study of in-hospital pediatric arrest, one half of children received the recommended rate of chest compressions and one fifth received the recommended depth per AHA guidelines. In an academic pediatric ED study, 87% of compressions exceeded 100 per minute. However, only 40% complied with recommended compression to ventilation ratios, and there were frequent pauses in compressions.
The location of compressions influences cardiac output. Infants’ hearts reside inferior to the lower third of their sternums. In these younger children, encircling the chest with both hands and compressing the lower part of the sternum with the thumbs while squeezing the thorax with the remaining fingers yields greater cardiac output than compression with two fingers. In video review of infant CPR, this approach yielded more accurate compression rates compared to a one handed technique. The AHA suggests utilizing the one hand approach to administer compressions to children 1 to 8 years old, but a study of simulated compressions suggested a two-handed technique, identical to that performed on adults, is easier and generates higher pressures. When feasible, a resuscitation board placed under children receiving chest compressions improves compressions; at a minimum, the child should be supine on a firm surface.
The ideal compression depth and rate is unknown, but the AHA recommends pushing “hard and fast.” Compressions should be deep enough to achieve optimal cardiac output without being so deep as to cause injuries to other vital organs. Attempts to increase depth excessively can result in leaning, which reduces coronary artery perfusion pressure and cardiac output. Guidelines suggest compressing the chest an estimated one-third of the anteroposterior diameter of the child. However, this estimating method has led to relatively deeper compressions than recommended in adults, and it can be extremely difficult to assess proportional anteroposterior compression depth during CPR. As a result, it is more practical to focus on absolute depths; we recommend 1½ inches in infants and 2 inches in older children.
Similarly, the exact rate of compressions to generate ideal cardiac output is unclear. Rates more than 100 compressions per minute improve cardiac output, coronary artery perfusion pressure, and survival compared with rates less than 90 compressions per minute in children. However, attempts to exceed 120 compressions per minute diminish perfusing pressures. High quality compressions diminish after 2 minutes. At this point, emergency clinicians may deny fatigue and be able to maintain the rate of compressions, but depth of compressions decreases substantially. This reduction in quality worsens with time. In adults, pauses in compressions yield substantial drops in coronary artery perfusion pressure, and pauses more than 20 seconds increase the odds of mortality by 50%. A recent study of in-hospital pediatric arrest found that brief pauses (median of 2.4 seconds) did not lead to significant reductions in intra-arterial pressures. Nevertheless, pauses in compressions should be minimized. When pauses are necessary to switch compressors, check rhythms, or provide defibrillation, they should be kept as brief as feasible.
Finally, the appropriate ratio of compression to ventilations is unknown. Animal models indicate the amount of ventilation required during CPR is much lower than with a normal perfusing rhythm, likely due to the lower cardiac output in CPR. The AHA recommends 30:2 compressions to ventilations for single rescuers and 15:2 for two rescuers. However, 15:2 ratios may yield insufficient compressions per minute in older children, and we recommend 30:2 ratios for children greater than 8 years. If an advanced airway is in place, ventilations should be delivered at 8 to 10 breaths per minute and should not interrupt compressions. Overventilation can be dangerous, but is common; in an observational study at a busy pediatric ED, 70% of CPR involved ventilations in excess of recommendations.
Notably, although resuscitation guidelines provide exact rates, depths, and ratios of compressions to ventilations, these recommendations are largely based on consensus. There are no randomized control studies comparing the impact of exact ratios, frequencies, or depths of compressions on survival. Rather than focusing on strict adherence to exact guidelines, we recommend focusing on promptly recognizing the need for compressions and then administering rapid compressions over the lower sternum with minimal interruptions. Practice is critical to maintaining quality, as most individual clinicians have limited real patient experience; in a busy pediatric ED, clinicians averaged 3 minutes of compressions per year. ,
The AHA recommends feedback, as it improves the quality of compressions. Quantitative feedback is most helpful because qualitative assessments can be difficult. During simulated arrests, emergency clinicians significantly overestimated compression depth and rate while underestimating pauses. Accelerometers and force sensors provide real-time data on compression rate and force. These feedback devices improve adherence with compression guidelines amongst children in simulated cardiac arrest. The presence of a coach providing verbal feedback augments feedback devices in simulated arrests. End-tidal carbon dioxide (ETCO 2 ) also serves as an adjunct measure of the adequacy of compressions. , In the low-flow state of CPR, the flow of venous blood to the lungs serves as the rate-limiting step for the elimination of CO 2 as opposed to ventilation. As a result, exhaled CO 2 increases with cardiac output, and the AHA recommends titration to greater than 20 mm Hg, although an observational study of in-hospital pediatric arrest found levels greater than 20 mm Hg were not associated with survival. Despite proven benefits, less than 5% of hospitals employ feedback devices regularly during resuscitation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here