Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The authors gratefully acknowledge Pamela Murray and Gina Succato for all of their work on previous versions of this chapter, as well as for contributing all the photographs not otherwise attributed.
Supplemental videos are available at expertconsult.com .
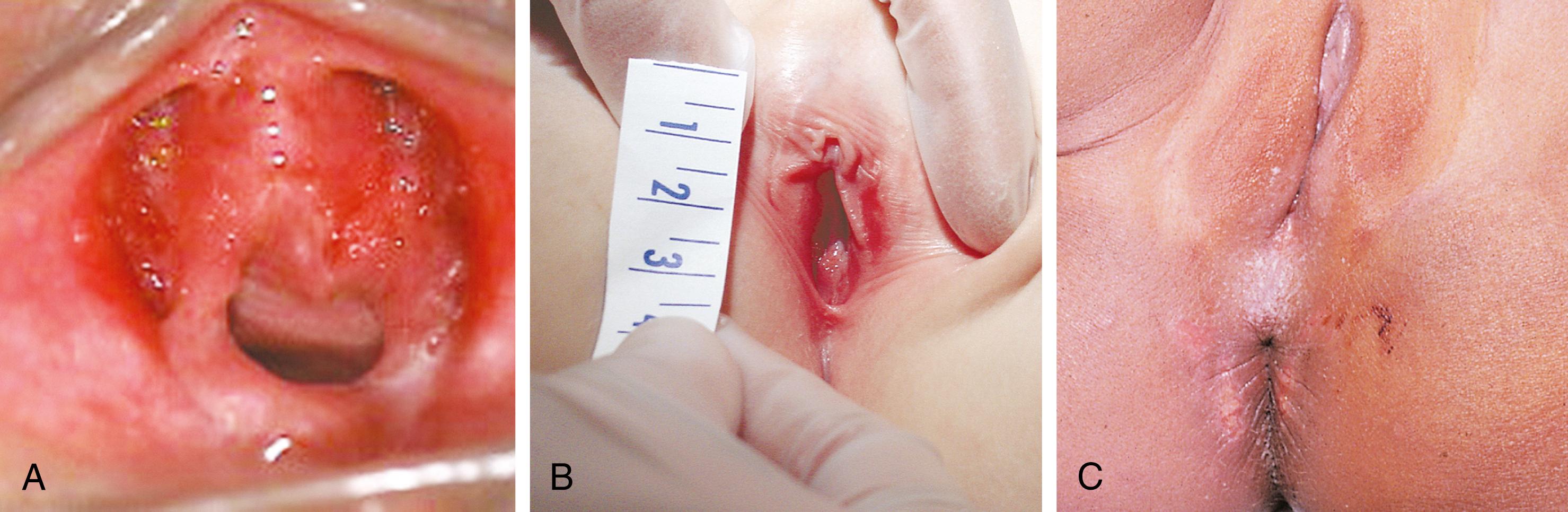
In the newborn, the physical appearance of the genitalia reflects stimulation by maternal sex hormones ( Fig. 19.1 ). Separation of the labia minora reveals thick, redundant hymenal folds that often hide the small central vaginal opening and urethral meatus. The mucosa is moist, vaginal pH is acidic, and a milky discharge is often seen. Vaginal bleeding during the first week of life is common. It is caused by withdrawal of maternal estrogen after delivery, and parents can be reassured that this is normal. Breast development, with palpable breast tissue, engorgement, and less commonly a clear or cloudy discharge, is observed in full-term neonates of both sexes (see Chapter 2 ). These findings gradually subside over several months. During this period, infants are at increased risk for developing breast inflammation and infection (see Chapter 13 ). Local trauma may increase the likelihood of infection.
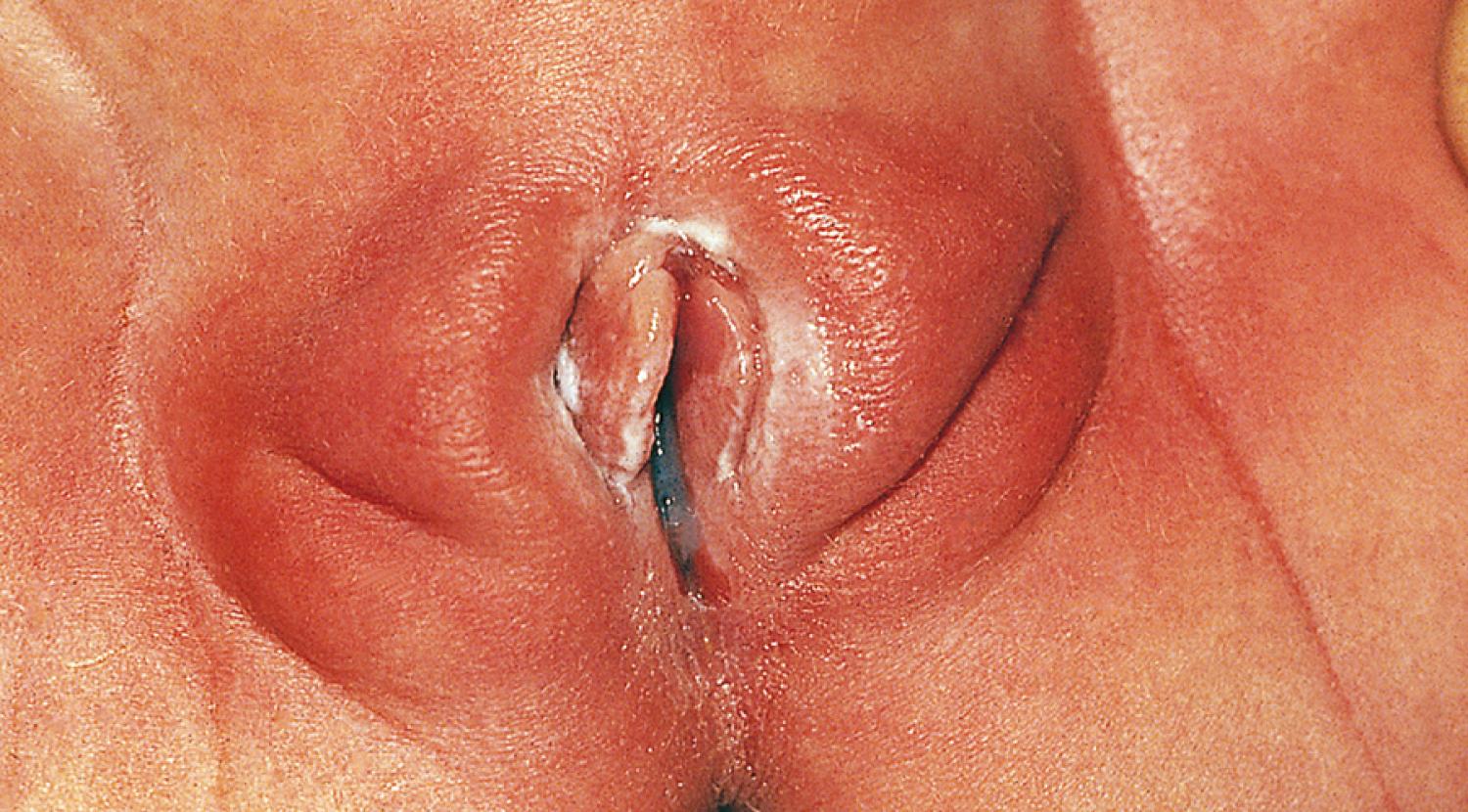
The effect of maternal hormones on the female genitalia gradually disappears; the labia majora lose their fullness, and the labia minora and hymen become thinner and flatter. Separation of the labia minora usually exposes the vaginal opening ( Fig. 19.2A and B ). As the young infant matures, the labia cover less of the vaginal vestibule, particularly when the infant or child is sitting, and thus offer incomplete protection from external sources of irritation. The mucosa has a glistening, reddish pink hue that sometimes is mistaken for inflammation by observers unaccustomed to examining prepubertal genitalia. Vaginal pH is now neutral or alkaline, and secretions are minimal.

Physiologic changes also cause variations in the appearance of the hymenal tissues during childhood. During early infancy, the tissues are relatively thick and can be redundant ( Fig. 19.3A and B ). Usually in the first months of life, the hymen becomes thin and translucent, with smooth edges (see Figs. 19.2 and 19.3C–E ). When the child enters puberty, the hymen again thickens under the influence of estrogen.
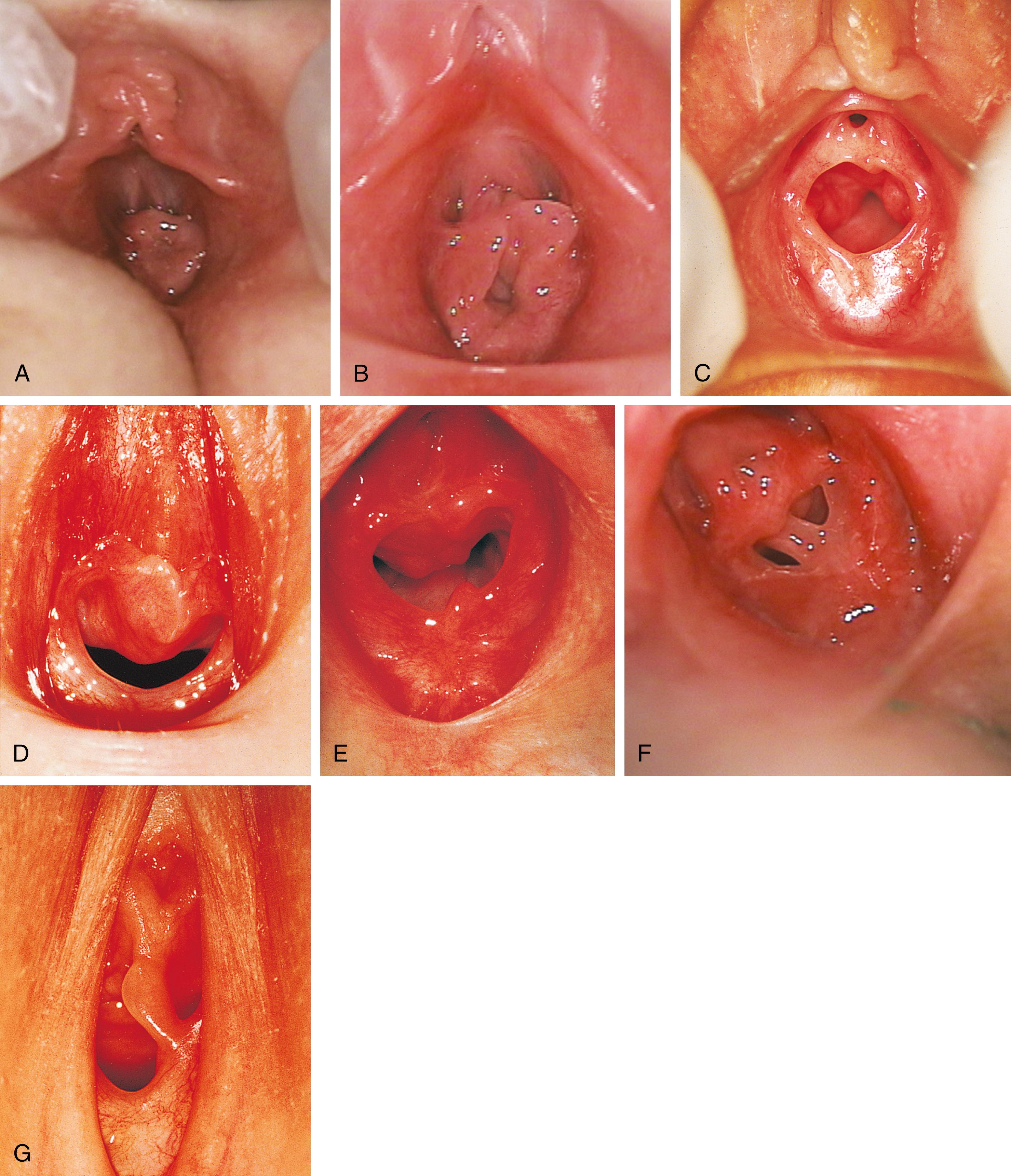
The shape of the vaginal orifice also varies. Annular (see Fig. 19.3C ), crescentic (see Fig. 19.3D and E ), teardrop shaped, and fimbriated (with fingerlike projections around the hymenal rim) hymens are all normal variations. On rare occasions, there is a completely imperforate hymen; more commonly there is a septated hymen (see Fig. 19.3F and G ) or a fenestrated hymen with small perforations.
From about 6 to 8 weeks old until puberty the perineum, perivaginal tissues, and pelvic supporting structures are relatively rigid and inelastic. This factor increases the likelihood of tearing as a result of trauma. In addition, before the onset of puberty, the ovaries are positioned above the pelvic brim ( Table 19.1 ). This intraabdominal location accounts for the fact that ovarian disorders in childhood frequently present with abdominal, rather than pelvic, signs and symptoms.
| Newborn | Early Childhood | Peripuberty (9–13 Years Old) | Post Menarche (>13 Years Old) | |
|---|---|---|---|---|
| Ovarian size and location | Not palpable | Pelvic brim | Within pelvis | 1.5 × 2.5 × 4 cm |
| Ovarian volume (mL) | 0.3–1.7 | 0.3–1.9 | 2–8 | 8–20 |
| Uterine length (cm) | 2.5–4.0 | 2.0–3.0 | 3.2–5.4 | 8.0 (nulliparous) (8 × 5 × 2.5) |
| Corpus-to-cervix ratio | 1:2 | 1:1 | 2:1 | 2–3:1 |
| Vaginal length (cm) | 4 | 4–5 | 7–8.5 | 10–12 |
| Hymen orifice diameter (mm) | 1–4 | 1–6 | 5–10 | 10 |
| Hymen thickness | Thick | Thin | Thickening | Variable |
| Clitoris width (mm) | 5 | 2–5 | 2–5 | 5–10 |
| Clitoris length (mm) | 10–15 | 10–20 | 10–20 | 15–20 |
| Labia minora | Smooth | Smooth, flat | Progressive increase in size and prominence | Tanner stages IV to V completed |
| Labia majora | Hairless, prominent | Hairless, thin | Hair growth, labial growth | Separation and differentiation of labia minora and majora |
| Vaginal secretions | White or clear, copious | Minimal | White or clear, variable amount, at times profuse | White or clear, varies by individual and with cycle |
| pH | 5.5–7.0 | 6.5–7.5 | 4.5–5.5 | 3.5–4.5 |
| Normal flora | Maternal enteric | Nonpathogenic flora including staphylococci and coliforms | Mixed vaginal flora | Lactobacilli dominant |
| Hormonal influence | Maternal hormones | Minimal sex steroids | Low and variable levels of endogenous estrogens and androgens | High levels of endogenous cyclic hormones |
With the onset of puberty, the mons pubis begins to fill out and hair begins to grow in the midline. Fat deposition fills out the labia majora. The labia minora thicken, become softer and more rounded, and asymmetry and variations in size and shape become more noticeable, particularly in patients who remove their pubic hair.
Patients whose labia minora protrude beyond the labia majora ( Fig. 19.4 ) often wonder if their genitals are normal. Asymmetry of the labia is common, and there is wide variation in the appearance and size of healthy labia. Clinicians and patients may wish to refer to published depictions of this variation, such as The Great Wall of Vagina ( http://www.greatwallofvagina.co.uk/home ). Typically the maximal width between the midline and lateral free edge of the labia minora measures less than 3 to 5 cm. Patients with labial hypertrophy may present with pain, irritation, chronic infection, problems with personal hygiene (e.g., during menses), or problems with sexual or physical activity. Most symptoms can be alleviated by addressing personal hygiene and appropriate choice of clothing to minimize friction. Sometimes use of an anti-chafe product can help to prevent abrasions. There is controversy surrounding labiaplasty and its relation to female genital mutilation. According to ACOG, surgical correction for patients under 18 should be considered for those with significant congenital malformation or persistent symptoms caused by labial anatomy. Unnecessary alteration of the labia in patients under 18 is against federal law. In most cases, a careful examination followed by reassurance and discussion of the variations in normal anatomy are all that is required.

Other normal changes during puberty include slight enlargement of the clitoris. The hymen also thickens, and its central orifice enlarges. The vaginal mucosa thickens and softens and becomes moist and pink as secretions increase and pH levels drop. Perineal and pelvic tissues become more elastic, and the ovaries gradually descend into the pelvis. In the months preceding menarche, physiologic leukorrhea increases. It consists of a white discharge containing mature epithelial cells and vaginal secretions stimulated by estrogen. In some patients, the unopposed estrogen secretion of puberty stimulates leukorrhea so profuse that it becomes concerning and irritating, because the perineum is often moist.
The developmental aspects of gynecologic anatomy and physiology are summarized in Table 19.1 . There is variation in the range of normal reproductive organ size as seen on ultrasound. The following have been proposed as upper values for prepubertal patients: uterine length, 4.5 cm; uterine thickness, 1 cm; and ovarian volume, 4 to 5 mL. The Tanner stages of pubertal development are presented in Chapter 9 .
The American Academy of Pediatrics (AAP) recommends that inspection of the external genitalia be part of every general physical examination. Careful perineal inspection during the first several well-child visits allows early identification of congenital anomalies of the labia and hymen. Anomalies of these external structures are rare but, if present, can be associated with anomalies of the urethra and bladder. Evidence of virilization in the newborn, especially when accompanied by hyperpigmentation, should prompt immediate laboratory investigation for evidence of salt-losing adrenal hyperplasia and warrants urgent endocrinology referral.
The proximal vagina, uterus, cervix, and fallopian tubes are derived from the Mullerian or paramesonephric ducts and develop concurrently with the urinary tract. Thus, patients with renal or urinary tract abnormalities are at greater risk for having associated anomalies of internal genital structures. Ultrasonography is very useful in evaluating neonates for suspected upper genital tract anomalies; these structures are relatively large during the neonatal period because of the influence of maternal hormones and higher levels of gonadotropins. Later in infancy and during early childhood, they are occasionally difficult to detect because of their small size. Hence, failure to visualize internal genital structures in prepubertal patients does not equate with agenesis, and in such cases, magnetic resonance imaging (MRI) can clarify the presence or absence of pelvic organs.
Patients who have specific complaints at acute care visits also warrant inspection of the genitalia in addition to abdominal, inguinal, and (when indicated) rectal examination. These complaints include abdominal pain; dysuria, urinary frequency, urgency, incontinence, or enuresis; constipation or encopresis; perineal pruritus, pain, or other abnormal sensation; vaginal discharge or bleeding before menarche; and suspected or acknowledged sexual abuse. Sexual abuse in the pediatric patient warrants referral to a clinician with the specialized knowledge, skills, and equipment appropriate to this evaluation. Careful documentation of the history is vital, because physical examination is likely to be normal. Any signs of injury that are noted should be fully described in words and photographed whenever possible. On occasion, colposcopic, radiologic, or internal examination is indicated.
Whether the patient is being seen for a routine checkup or for a specific problem, the gynecologic portion of the assessment should occur only after establishing rapport to avoid frightening the child. Because parents and health care providers communicate their own comfort levels to children both verbally and nonverbally, a discussion of any parental anxieties and the clinician’s self-awareness of his or her own attitudes can facilitate successful examination. The use of pictures and language familiar to the child and family may further enhance cooperation but interspersing anatomically correct vocabulary can also be educational. External inspection of the genitals can take place during routine physicals after the abdominal and inguinal exam. The AAP recommends the exam to be performed in the presence of a parent or guardian. The clinician should explain the exam and its reasoning to the child and caregiver. The clinician can request the help of the child as well. Having the support of the caregiver can reassure children.
Young infants can be assessed easily on an examination table after being positioned by the examiner. Drapes generally are unnecessary for toddlers and preschoolers because they are isolating and often perceived as threatening. However, similar to adolescents, school-age children may find drapes helpful in reducing embarrassment. An older infant, toddler, or preschool child may be more relaxed when examined on the parent’s lap, with the parent assisting by gently holding the child in either the frog-leg or lithotomy position ( Fig. 19.5A and B ). School-age children usually can be examined on the table in the frog-leg, lithotomy, or knee-chest position. Knee-chest positioning can provide excellent visualization of the hymen and the distal vagina ( Fig. 19.6 ), but some patients may feel threatened by being examined from behind. An alternative means of achieving visualization of the distal vagina is with the patient supine and performing the Valsalva maneuver (i.e., asking the child to push down as if they were going to pass a stool). This often produces distention of the distal vagina and hymenal orifice, facilitating visualization and atraumatic collection of specimens.

Use of good focused lighting is essential. In the office setting the otoscope provides excellent focused light and low magnification, which is sufficient for most examinations. Some young children fear it because of prior painful experiences during otoscopy. Given this, the patient should be reassured ahead of time that no speculum will be attached and that they will not be forcibly restrained. Preliminary “examination” of the umbilicus may help allay anxiety.
Once the patient is properly positioned, visualization of the introitus, hymen, and lower portion of the vagina is facilitated by maneuvers that separate the labia. These maneuvers should be explained first, and the child reassured that the examiner is “just going to look.” If the patient desires or is mildly anxious, they may place their hands beneath the examiner’s, or the parent may be enlisted to perform the maneuver. Some patients prefer to separate their labia themselves. The maneuvers include labial traction and separation (see Fig. 19.2 ). When using a handheld light (otoscope), a second set of hands (parent or nurse) may be needed to maximize labial separation and focus the light. Care must be taken to ensure that excess traction is not applied during these maneuvers because it can result in painful tearing of labial adhesions, if present.
If the patient is unusually anxious about the procedure and cannot be reassured, the examination should be deferred to a later date. On occasion, use of relaxation techniques, an oral benzodiazepine, conscious sedation, or anesthesia may be needed for an adequate evaluation. At no time should a frightened, struggling child be physically restrained and forced to undergo examination; the yield is minimal and the experience is physically and emotionally traumatic.
On inspection, the clinician can readily ascertain the presence or absence of pubic hair; note the appearance and configuration of the labia majora, labia minora, clitoris, urethra, hymen, vaginal orifice, and anus; note the color of the mucosa and the presence or absence of rash, discharge, or unusual odor; and often visualize the distal vagina. Vaginoscopy is required only occasionally in the prepubertal child in order to perform a complete evaluation for complaints such as vaginal bleeding with or without evidence of trauma, discharge resistant to routine therapy, a suspected vaginal foreign body, and suspected vaginal tumors. Because of the high potential for inflicting pain, especially if the patient moves suddenly, vaginoscopy generally is best performed under anesthesia or sedation. Some older school-age children may tolerate internal examination by a highly skilled examiner without sedation if preparation is careful. Again, a traumatic experience should be avoided. Useful information can be gathered by use of sonography or MRI. Computed tomography (CT) involves greater radiation exposure and provides poorer resolution of pelvic structures and thus should be used only to provide information not obtainable by other imaging studies.
If a prepubertal child with vaginal discharge or perineal or urinary complaints is to be evaluated, it is advisable to ask the family not to bathe the patient or to apply any creams for at least 12 hours before the examination. The patient should always be prepared for the procedure with simple and truthful explanations. In the presence of ulcers, herpes cultures or specimens for a polymerase chain reaction (PCR) test should be obtained from the base of unroofed fresh vesicles or ulcers. Routine bacterial cultures, including those for gonococci, can be collected from any visible discharge on the perineum in the prepubertal child. If specimens must be collected because of a history of vaginal discharge, having the patient perform a Valsalva maneuver may move discharge into the introitus. If this fails, specimens can be collected with little discomfort with a Dacron wire swab premoistened with sterile nonbacteriostatic saline.
It can be helpful to allow the patient to handle a moistened swab and touch themself with it. The swab is inserted gently through the vaginal opening, taking care to avoid contact with the hymen, which is exquisitely sensitive. Dry cotton-tipped swabs should be avoided because of their size and because they tend to abrade the thin vaginal mucosa of the prepubertal child. If collection is likely to be difficult because of pain or anxiety or because the hymenal orifice is very small, application of a topical anesthetic to the perineal and hymenal area beforehand can be beneficial. Although topical lidocaine preparations work within 5 to 10 minutes, they can produce transient discomfort before the onset of anesthetic action, reducing cooperation in some patients. When time permits, use of a newer topical anesthetic cream (e.g., eutectic mixture of local anesthetics [EMLA] or lidocaine [LMX]) is an excellent alternative. Table 19.2 lists the specimens that may be considered in evaluating patients with symptoms of vulvitis, vaginitis, or vaginal discharge. If testing for sexually transmitted infections (STIs) is indicated due to concerns of possible child sexual abuse, please refer to Chapter 6 .
| Laboratory Study/Specimen | Diagnostic Utility |
|---|---|
| Saline wet mount | Inflammatory cells, yeast, trichomonads, clue cells, lactobacilli, mature and immature epithelial cells, sperm |
| KOH | Yeast, “whiff test” for bacterial vaginosis (also can be positive with Trichomonas ) |
| Vaginal pH | Elevated in bacterial vaginosis (also can be elevated with Trichomonas ); obtain from lateral or anterior vaginal wall, not from pooled secretions or saline-diluted specimen |
| Vaginal specimens | Routine culture a for nonvenereal pathogens |
| Culture for enteric bacteria, including Shigella (Cary-Blair medium) | |
| NAAT for gonorrhea, Trichomonas, Chlamydia | |
| Culture for gonorrhea, a Trichomonas, Chlamydia (if forensic evidence or bacterial sensitivities are needed) | |
| Cervical specimens | NAAT for gonorrhea, Chlamydia or Trichomonas Culture for gonorrhea, a Trichomonas, Chlamydia (if forensic evidence or bacterial sensitivities are needed) |
| Pap smear/ThinPrep | Squamous intraepithelial lesions; consequences of HPV, including precancerous and cancerous lesions; cell maturation index (estrogenization) |
| Genital ulcer/lesion specimen | HSV culture or PCR (if suspect chancroid use moistened swab at base of lesion and transport as rapidly as possible; send to reference laboratory to test for Haemophilus ducreyi ) |
| Biopsy | Dysplastic, atrophic, or unusual lesions of vulva, vagina, and cervix |
| Urine specimen | Urinalysis; urine culture; gonorrhea, Chlamydia, or Trichomonas NAAT |
| Perianal specimen | Pinworms and eggs: Parent obtains sample during night (or first thing in morning before patient bathes) by pressing firmly over anal area with a pinworm paddle (optically clear polystyrene paddle connected to cap of a transport container) or a 1-inch strip of cellophane tape (which is then affixed to a glass slide) |
| Serologic tests | Syphilis (RPR, VDRL, and Treponema -specific testing), HIV, and HSV |
The practice of routine inspection of the external genitalia at each well-child visit beyond infancy facilitates early diagnosis of any problems that may arise and allows evaluation of physical growth and secondary sex characteristics. This also creates an opportunity to discuss normal anatomy and behaviors, including masturbation; to distinguish acceptable from unacceptable (exploitative or abusive) forms of touching; and to help overcome the reluctance of some parents and children to express concerns about the genitalia. Making assessment and counseling a routine part of well-child care may help reduce anxiety and embarrassment for the child when genital or pelvic examinations are required.
A gynecologic examination should be considered for any patient with a variety of specific complaints and concerns, including those listed in Box 19.1 . This examination should include careful inspection of the external genitalia and regional lymph nodes, and palpation of the uterus and adnexa when indicated. In some cases, assessment of internal pelvic structures may require radiologic imaging. For example, if menarche is delayed or menstrual periods are unusually problematic (e.g., excessive pain or unusually irregular flow patterns), ultrasound evaluation can be useful. In most cases, ultrasound imaging in a pediatric radiology suite is preferable to a point of care study.
Abnormal vaginal discharge
Pain
Pelvic
Perineal
Dysuria
Dyspareunia (pain or other difficulty with intercourse)
Abdominal (unexplained)
Suspected sexual abuse
Concerns with pubertal development
No secondary sexual development by 13 years old
No menarche if start of puberty more than 2 years ago
No menarche by 15 years old
Abnormal timing or sequence of pubertal development
Anatomic abnormalities on genital inspection
Increased body hair, severe acne, or masculinization
Menstrual disturbances
Dysmenorrhea not responsive to standard treatment
Amenorrhea or oligomenorrhea
Abnormal uterine bleeding or polymenorrhea
Sexual activity
Routine health care for sexually active individual
Sexual contact with partner with a suspected or confirmed STD or related genital symptoms
The gynecologic examination is an important part of routine health care for sexually active adolescents (see Box 19.1 ) and should be considered at 12-month intervals or with greater frequency if indicated based on community and behavioral risk factors. Use of a speculum is typically not required but is useful in situations that necessitate visual inspection of the vaginal cavity or cervix, including those listed in Box 19.2 . In the absence of the aforementioned indications, a speculum exam could first be considered at 21 years old. At this age, women should undergo their first cervical cytology screening, using liquid-based cytology or traditional Papanicolaou (Pap) smear, according to recommendations from the American College of Obstetricians and Gynecologists ( ). Transmasculine patients who still have a cervix should undergo routine Pap testing but may require additional measures (e.g., lubricant or pretreatment with estrogen cream) to ensure comfort during examination.
Papanicolaou (Pap) smear (patients 21 years old and older; earlier in sexually active immune-compromised patients)
Persistent unexplained bleeding
Persistent vaginal discharge
Suspected injury
Suspected foreign body
Suspected anatomic abnormality (e.g., vaginal septum, duplicated cervix)
Sexual assault
A thorough and directed history precedes the examination. A comprehensive outline is suggested in Table 19.3 . Adequate time should be devoted to interviewing the patient alone, which provides an opportunity to ask questions about voluntary and involuntary sexual activity and to explore other concerns that may be difficult to discuss in the presence of a parent or guardian. A similar opportunity should be given to the parents to express any concerns that they are reluctant to share in their child’s presence.
| Category of Information | Specific Information Required |
|---|---|
| General | |
| Home | Who lives there and quality of relationships; sources of conflict and support |
| Education/employment | School, grades, curriculum, repeated grades, goals, behavioral or learning difficulties; volunteer activities; if working—type, occupational hazards, hours, literacy/numeracy |
| Eating | Nutritional content (specifically calcium, vitamin D, iron, fat, fiber, folate), body image, eating behaviors/patterns, recent changes in weight |
| Activities | Exercise, peer activities, friends, hobbies |
| Drugs | Caffeine, tobacco/nicotine, alcohol, marijuana, crack, cocaine, heroin/opioids, hallucinogens, hormones, pills, injectable drugs; rehabilitation or treatment history |
| Depression/suicide | Depression, anxiety, psychiatric treatment, medications, major losses or disruptions, counseling history, self-injurious behavior, suicide ideation and history of attempts |
| Safety abuse/exploitation | Physical, sexual, or emotional; family, relationship, peer, school, and community violence, and trafficking and/or exploitation |
| Sexual, Obstetric, and Gynecologic History | |
| Menstrual | Menarche (age), cycles (length, duration, quantity of flow, use of pads or tampons), first day of last menstrual period, dysmenorrhea and associated disability, PMS, abnormal bleeding, mid-cycle pain (mittelschmerz) and spotting, douching, feminine hygiene product use (including scented products and deodorants) |
| STI | Herpes; gonorrhea; Chlamydia; syphilis; PID; pubic lice (“crabs”); HPV (venereal warts, abnormal Pap smears); Trichomonas; HIV; hepatitis A, B, and C; undiagnosed pelvic pain; HPV immunization status |
| Pap | Abnormal results, colposcopy, biopsies, treatments, follow-up |
| Urologic | Urinary tract infection or kidney problems, enuresis, incontinence, dysuria, urgency, frequency |
| Vaginal discharge | Color, odor, quantity, duration, pruritus |
| Vaginal infections | Yeast, bacterial vaginosis, trichomoniasis |
| Obstetric | Previous pregnancies and outcomes, fertility plans, and concerns |
| Sexual behavior | Last and other recent intercourse and protection; specific HIV risk to self and partners; sexual experience and age at onset; sexual practices, condom use; anatomy of sexual partners; number of partners, lifetime and recent |
| Gender and sexuality | Sex assigned at birth, presence of intersex disorder, gender identity, gender expression, romantic attraction, sexual orientation; satisfaction with sexual experience; sexual problems with self or partner |
| Contraceptive | Current and past methods, satisfaction, consistency of use, problems, future plans for pregnancy/parenthood |
| Past medical history | Prior sources of care (routine, episodic, and emergency); immunization status including hepatitis A and B and HPV; rubella and varicella status; hypertension; migraines with aura or neurologic signs; thromboembolic events |
| Medications/treatment | History of self-treatment with over-the-counter or prescription medications, antibiotics in particular, and any integrative therapies or medications |
| Family history | Thromboembolic events at an early age or associated with pregnancy or with hormonal contraceptives; disease or death caused by alcohol, drugs, tobacco; gynecologic or obstetric problems; age at childbearing; endocrine problems (especially thyroid); bleeding problems (especially OB/GYN-related bleeding, mucus membrane bleeding, or need for blood transfusion); congenital malformations; mental retardation; miscarriages and stillbirths |
A young patient’s initial experience with a pelvic examination may greatly affect the ease with which they experience routine gynecologic care and sexual relations throughout adult life. Hence, the examiner’s approach should be sympathetic, unhurried, and sensitive to the modesty of the patient. When patients have had gynecologic examinations in the past, it is helpful to ask them about their prior experience to avoid rekindling any emotional or physical trauma.
Young women should be given the choice of being examined with or without an accompanying person in the room. Some patients, particularly early adolescents, may be conflicted between their modesty and their desire for support from a friend or relative. Suggesting that the support person must stay at the head of the table and using drapes that allow visual (eye) contact between patient and examiner is often the most comfortable compromise. Chaperones should be offered to all patients and their presence is considered standard when the examiner is male, is a trainee, or when there is a history of sexual abuse.
The pelvic examination is done after other components of the physical examination. The patient should empty her bladder beforehand, and a urine specimen can be collected at this time if needed for testing. Raising the head of the examining table 20 to 45 degrees helps relax abdominal muscles and facilitates maintenance of visual contact with the patient. Before beginning, the examiner should carefully explain the various parts of the examination: inspection of the external genitalia, speculum examination of the vagina and cervix (with specimen collection), and bimanual palpation. Use of anatomic drawings and/or models can be helpful and educational. Throughout the procedure, clinicians should explain what they are seeing and provide reassurance and education. This should help the patient relax and can also confirm normal anatomic findings and provide examples of accurate vocabulary for reproductive anatomy and function. A hand mirror held by the patient is often useful for similar reasons.
The patient should be assisted into the lithotomy position at the end of the examination table. Non-latex gloves should be worn for both external and internal examinations. Patient comfort may be increased by identifying and then touching distal areas first and moving proximally (e.g., knees, thighs, groin, labia, introitus). Next, the external genitalia are inspected. Pubic hair distribution should be noted as should the presence of any nits, lice, skin or vulvar lesions, or vaginal discharge on the perineum. The introital opening is examined and palpated if there is swelling in the region of the Bartholin glands. Clitoral size is assessed. The urethral opening is then inspected for erythema or discharge. Any purulent material obtained should be tested for gonorrhea, Chlamydia, and Trichomonas.
If a speculum examination is required, successful examination depends on adequate patient preparation and use of appropriate instruments, including a good light source. For virginal adolescents, the narrow-bladed Huffman speculum (½ × 4¼ inches) is recommended. Although long enough to expose the cervix, its narrow blades are usually inserted easily through the virginal introitus. Most sexually active adolescents can be examined with the straight-sided Pederson speculum (⅞ × 4 inches); however, the Huffman speculum should be considered as an alternative for a first pelvic examination or for particularly anxious patients. The duck-billed Graves speculum (1⅜ × 3¾ inches) is useful in parous patients ( Fig. 19.7 ). Obese patients may require a Graves speculum or a longer Pederson (1 × 4¾ inches) for adequate visualization of the cervix. Metal speculums may be preferred, because they are easier to manipulate and are available in a greater range of lengths and widths; disposable plastic specula with intrinsic lights are now widely available and can be purchased in a range of sizes.

The patient should be shown the speculum and allowed to touch it if they desire. Patients experiencing their first pelvic examination should be reassured that only the blades of the speculum will be inserted. Comparing the size of an open speculum to a finger or tampon often is reassuring. The patient should be told that they will feel “a sense of pressure,” not pain, during speculum insertion and should be reminded to breathe regularly because tensing abdominal or pelvic muscles can produce discomfort and make the examination more difficult to perform. A history of inability to use a tampon suggests an increased possibility of a physical or emotional barrier to a successful speculum exam.
The examiner may then gently insert the gloved index finger into the vagina to assess the size of the introital opening and to locate the cervix. Vaginal muscle tone can be assessed by asking the patient to “tighten their muscles” around the examiner’s finger. Conscious relaxation can be practiced by asking the patient to relax those same muscles and to push their buttocks onto the examining table. Both plastic and metal speculums should be moistened with warm water or water-based lubricant to increase comfort and ease of insertion. With the index finger partially withdrawn but gently pressing on the vaginal floor, the speculum is inserted over the finger into the vagina, taking care to avoid catching pubic hairs or the labia in the mechanism of the speculum. This is done at an oblique angle along the posterior wall to accommodate the vertical introitus and avoid traumatizing the urethra, which lies above the anterior vaginal wall. Another technique that effectively assists insertion involves using the middle and index fingers to stretch the posterior labial folds down and out before inserting the speculum. With the speculum in place, the vaginal walls are inspected for erythema, lesions, and quality and quantity of discharge, and specimens are collected (see the Specimen Collection section, later).
After specimens have been collected the speculum is removed, and the bimanual (vaginal/abdominal) examination is performed. Water-based lubricant is placed on the two gloved fingers to be used before inserting them carefully through the introitus into the vagina. The examiner should note the size, consistency, position, and mobility of the uterus and check for tenderness on cervical or fundal motion. The adnexa should be palpated for evidence of enlargement or excess tenderness.
Once the examination is completed, the patient should be helped out of the lithotomy position, given tissues to wipe away any lubricant or discharge, and allowed privacy to get dressed. At the conclusion of the visit, the examiner can present the results of point-of-care testing (such as microscopic evaluation of wet mount and potassium hydroxide [KOH] preparation). The use of handouts with pictures or drawings can enhance the patient’s understanding of the results. This is also an opportunity to encourage communication between the patient and their parent, as appropriate to the circumstance.
Adolescents should be advised not to douche or to use tampons or feminine hygiene products before a gynecologic examination. When testing for Neisseria gonorrhoeae and Chlamydia trachomatis, the newer nucleic acid amplification tests (NAATs) detect minute quantities of pathogen DNA/RNA and thus are highly sensitive and specific; they also offer the advantage that specimens may be collected from a variety of sites (vaginal wall, urine, urethra, cervix). To obtain a vaginal sample for gonococcus (GC) and C. trachomatis NAAT, slide the swab 4 to 5 cm into the vagina and rotate it for greater than 10 seconds, moistening it against the walls of the vagina. In cases of symptomatic gonococcal infection where there are concerns about antibiotic resistance, one must perform a culture with sensitivities, which are not part of NAAT testing, to ensure proper antibiotic selection. (See later for guidance on collecting specimens during a speculum examination.)
The vaginal pH level can be measured by moistening a cotton-tipped swab on the lateral vaginal wall and rolling it on pH paper (with an appropriate range of pH 3.6 to 6.1). Vaginal pH levels are elevated in bacterial vaginosis and tend to be increased with Trichomonas and decreased with candida infections. Vaginal secretions should be obtained with a cotton or Dacron swab and placed in a tube with 1 mL of nonbacteriostatic normal saline for wet mount and KOH examination. The swabs for GC and C. trachomatis NAAT and for wet mount may be obtained by the patient (“self-swab”) if the patient prefers and additional examination is not required.
To review the wet mount, a drop of the saline solution containing vaginal secretions is examined under low (×10) and high (×40) power for distribution of epithelial cells, leukocytes, yeast forms, Trichomonas organisms, sperm, and clue cells. A drop of 10% KOH is added to a second drop of the saline solution. This preparation is immediately “whiff tested” for the presence of the acrid odor associated with amines that is found in bacterial vaginosis and often in patients with trichomoniasis. After this, viewing of the KOH preparation facilitates identification of yeast.
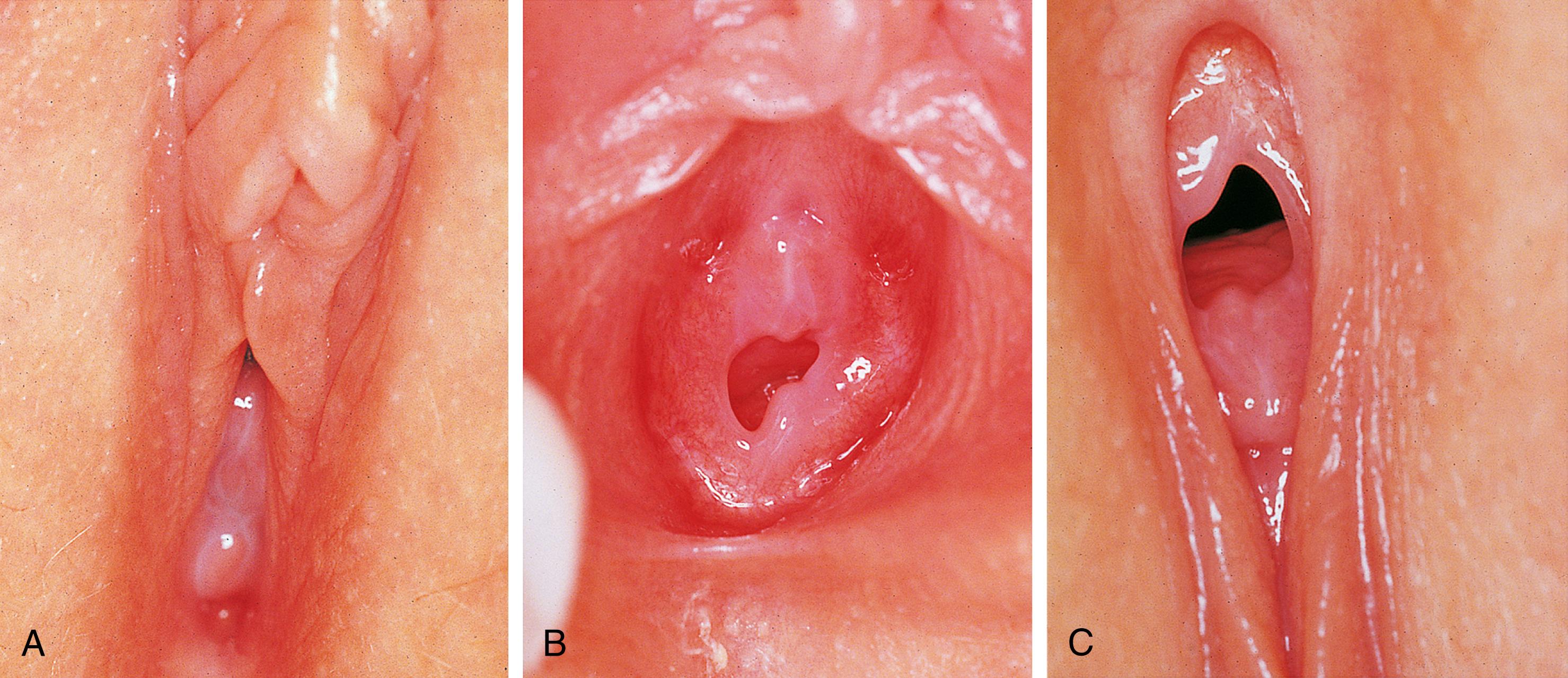
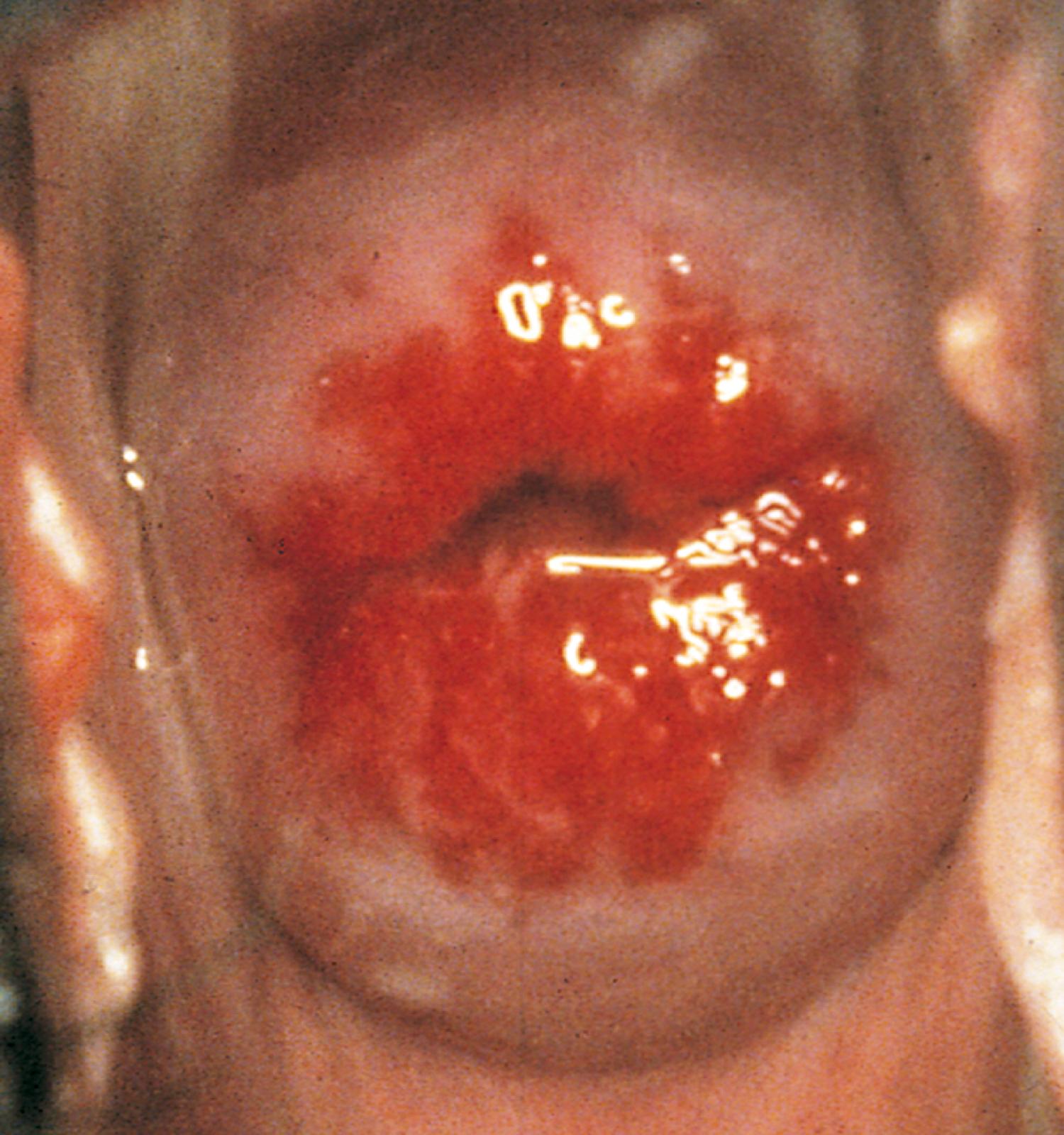
If a speculum examination is required (see Box 19.2 ), the vaginal pH is measured by holding pH paper (described previously) against the lateral vaginal wall, away from pooled secretions. Visible vaginal secretions from the posterior vaginal pool should be obtained with a cotton or Dacron swab for wet mount. Before obtaining samples from the cervix, any surface mucus should be gently removed with cotton swabs. The normal nulliparous cervix usually has a small round os ( Fig. 19.8 ). Any cervical lesions seen, such as cysts, warts, polyps, or vesicles, should be noted. An ectropion (or eversion) of the endocervical columnar epithelium onto the cervical surface is common and normal in adolescents ( Fig. 19.9 ). Ectropion should be distinguished from cervicitis, the latter being suggested by erythema, friability, and/or mucopurulent cervical discharge (see Fig. 19.34 ). If a gonorrhea culture is necessary (to test for antibiotic sensitivities), insert a sterile swab into the endocervical canal, rotate it for at least 10 seconds, and then immediately place it into a selective transport or culture medium. Either medium must be at room temperature before inoculation. Gonorrhea-specific media prevent bacterial overgrowth by other species and allow a longer transport time.
Cervical cytology (Pap) screening using liquid-based cytology to check for cervical dysplasia (a precursor of cervical cancer) is done by rotating a plastic Ayre spatula circumferentially (360 degrees) around the cervical os, including the entire squamocolumnar junction. A sample from the endocervical canal is collected with a Cytobrush (or a cotton swab if the patient is pregnant). Each sample is swished in liquid ThinPrep solution or fixed onto a glass slide according to laboratory protocol. Cervical cytology results can be uninterpretable in the presence of inflammation and bleeding; therefore, it is preferable to defer collection until infections are treated and menstrual bleeding has finished. However, concerns about patient follow-up or urgent clinical needs can justify collection of specimens at less optimal times. A number of strains of human papillomavirus (HPV) have been identified as causative in cervical cancer, as well as genital warts. All adolescents should be encouraged to complete their HPV vaccination series. However, currently available vaccines against HPV do not cover all strains associated with cervical cancer. Therefore, a Pap smear every 3 years is indicated starting at 21 years old. Immunocompromised women under 21 years old with human immunodeficiency virus (HIV), solid organ transplant, hematopoietic stem cell transplant as well as systemic lupus erythematous, inflammatory bowel disease, and rheumatoid arthritis on immunosuppressants should have their first Pap within 1 year of sexual activity onset, and annually for the first three years. The Centers for Disease Control and Prevention (CDC) advises that HPV typing is not indicated in women under the age of 30.
The most common form of “vaginal obstruction” in prepubertal patients is really a pseudo-obstruction or partial obstruction produced by reversible “fusion” of the labia minora as a result of labial adhesions. On inspection, the clinician finds a smooth, flat membrane with a thin lucent central line overlying the introitus. It is postulated that inflammation and erosion of the superficial layers of the mucosa—whether caused by infection, dermatitis, or mechanical trauma—result in agglutination of the apposed labia minora by fibrous tissue on healing. The process typically begins posteriorly and extends forward. In most cases, the fused portion is less than 1 cm in length, but on occasion it can extend to cover the vaginal vestibule and rarely the urethra ( Fig. 19.10 ). Even when fusion is extensive, urine and vaginal secretions are able to exit through the opening anteriorly. However, some urine may become trapped behind the adhesions after toileting. This may cause further irritation, perpetuating the condition or fostering extension of the adhesions. Although most labial adhesions are asymptomatic, some patients have symptoms of lower urinary tract and vulvar inflammation.
If resolution of the fused labia is desired, the condition readily responds to application of estrogen cream along the line of fusion twice daily for 2 weeks followed by nightly application for an additional week. On occasion, the course needs to be extended for an additional 2 weeks, or an increased volume of estrogen cream is advised. After the labia have separated, a zinc oxide–based cream should be applied nightly for several months to prevent recurrence. The parent should be informed that topical estrogen may cause transient hyperpigmentation of the labia and the areolae and an increase in breast tissue but that these changes regress once therapy is completed. An estrogen withdrawal bleed (similar to that seen in the neonate) occasionally occurs. Removal of irritants, treatment of infections, and instructions on good perineal hygiene help prevent recurrence of adhesions. Nonetheless, refusion can occur, although repeated treatment is not necessary if the child is asymptomatic. As an alternative or adjuvant to estrogen, some experts recommend twice daily topical application of 0.05% betamethasone dipropionate ointment for 4 to 6 weeks.
Manual separation of fused labia is painful, traumatic, and frequently followed by a recurrence. Hence, this practice should be abandoned. True fusion—adhesions present in the first months of life or adhesions that do not respond to the prescribed therapy—requires further evaluation for abnormalities in sexual differentiation or androgen production.
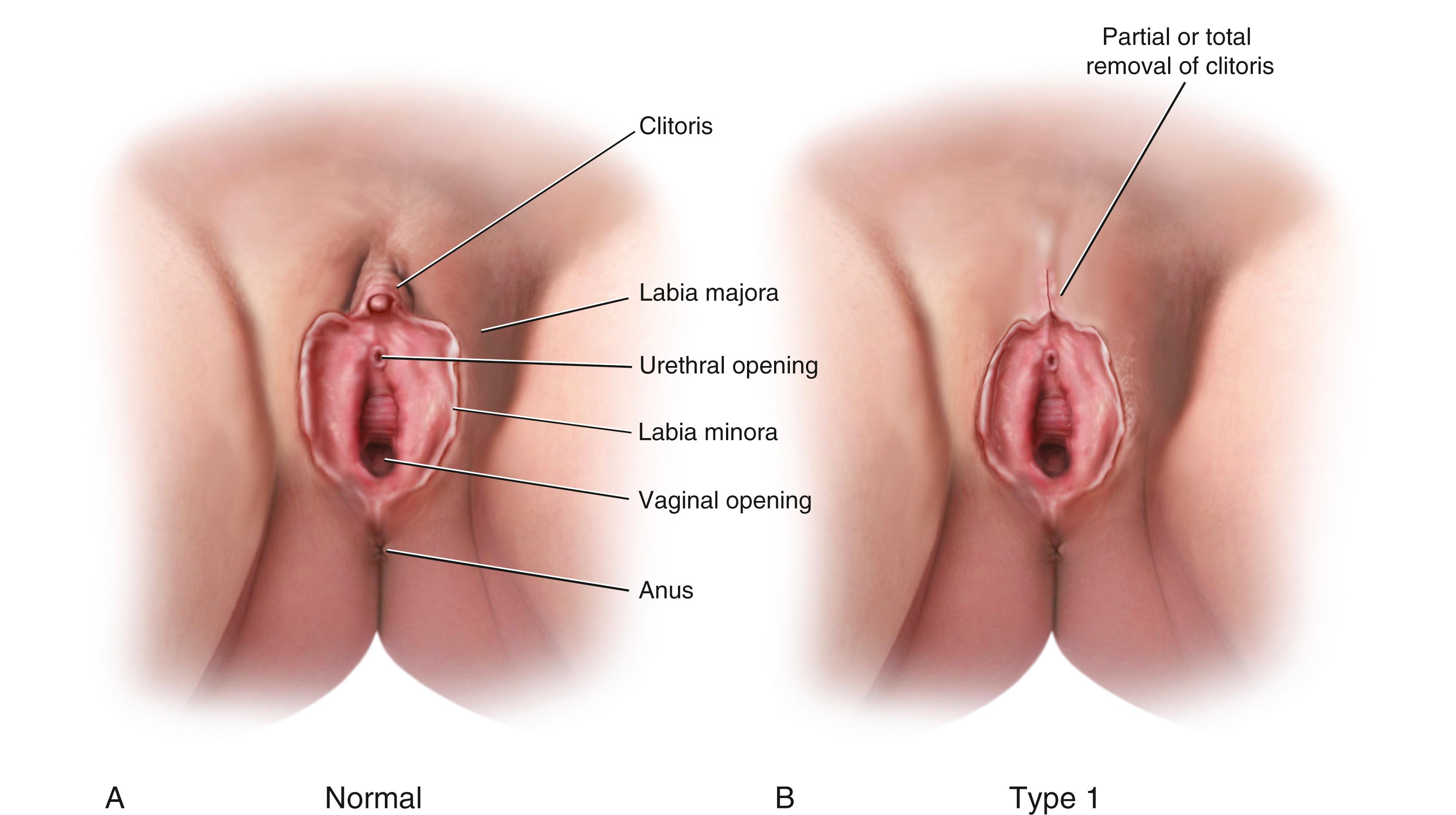
Female genital mutilation/cutting (FGM/C) is another cause of genital tract obstruction seen with increasing frequency by pediatricians, especially those who care for patients from Africa, the Middle East, and Asia. This ritual cutting and alteration of female genitalia has no known medical benefits and carries potentially life-threatening short- and long-term health consequences. Fig. 19.11 illustrates the various types of FGM/C. Further information about this topic can be found at the World Health Organization (WHO) website (see the Websites section at the end of this chapter). The WHO is working to eliminate this practice, considering it a human rights violation. However, pediatricians who encounter patients who have undergone these procedures must be sensitive both to the complex religious and sociocultural norms that motivate families to practice FGM/C, as well as to the consequences to the individual patient.
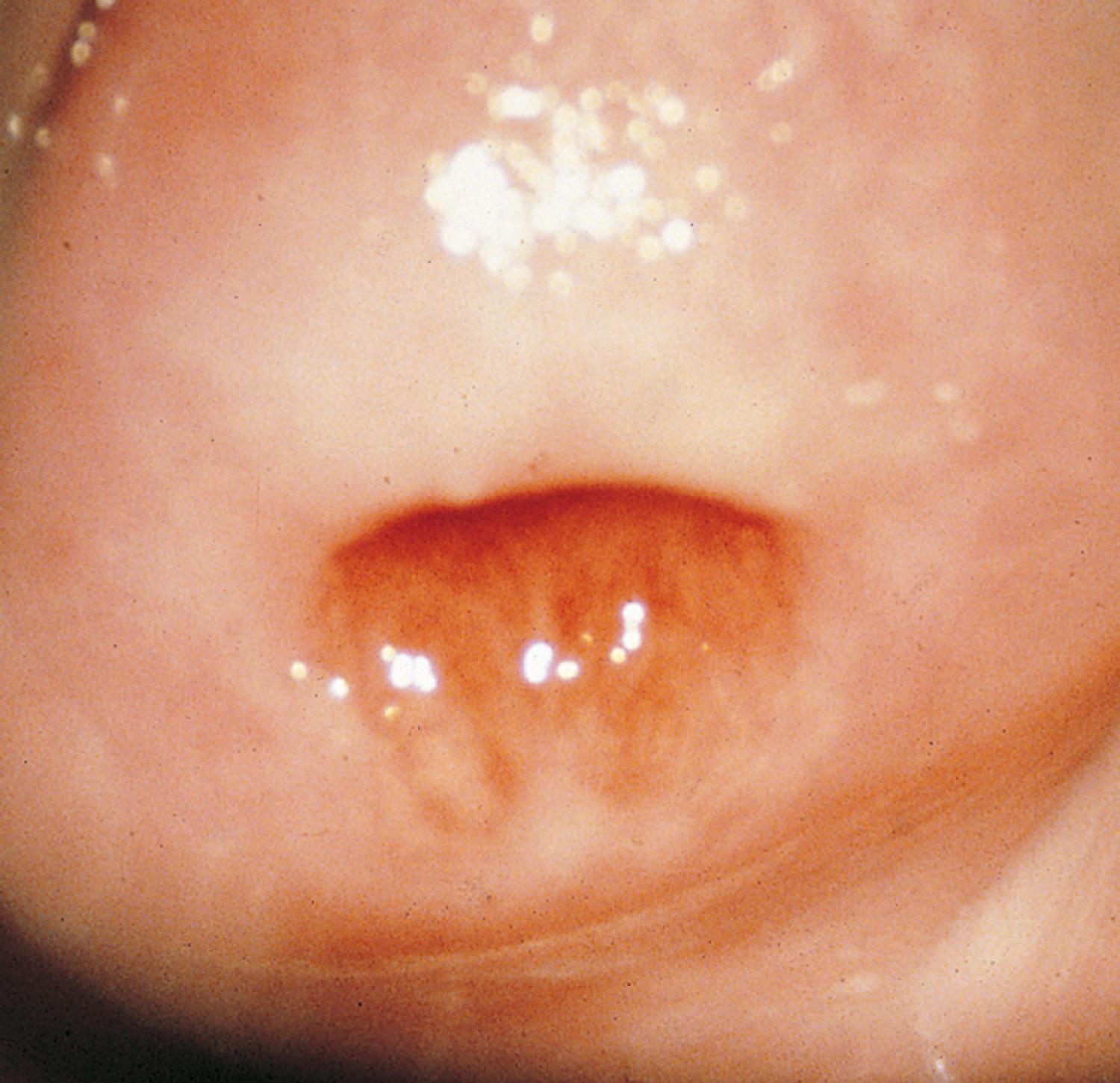
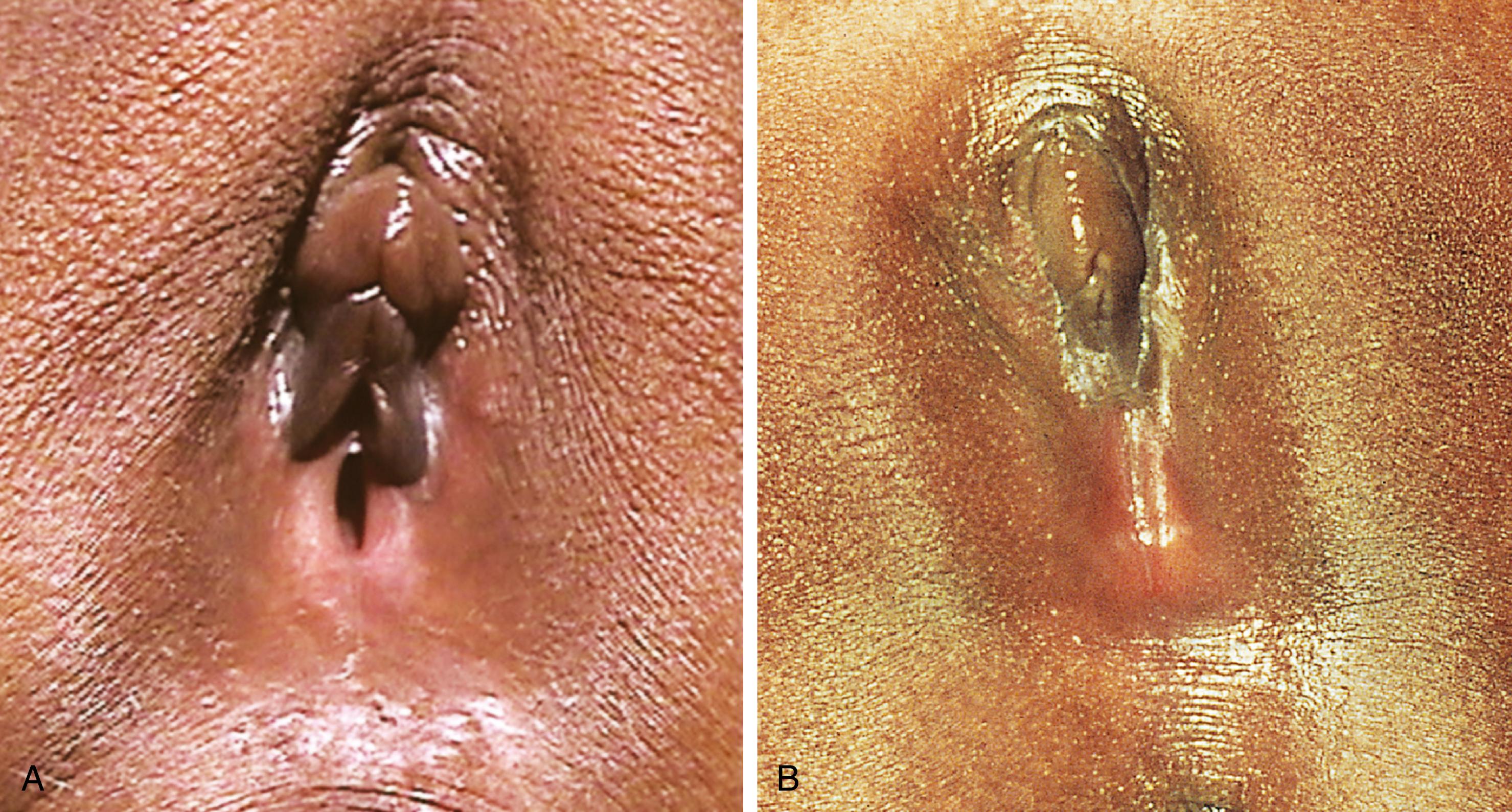
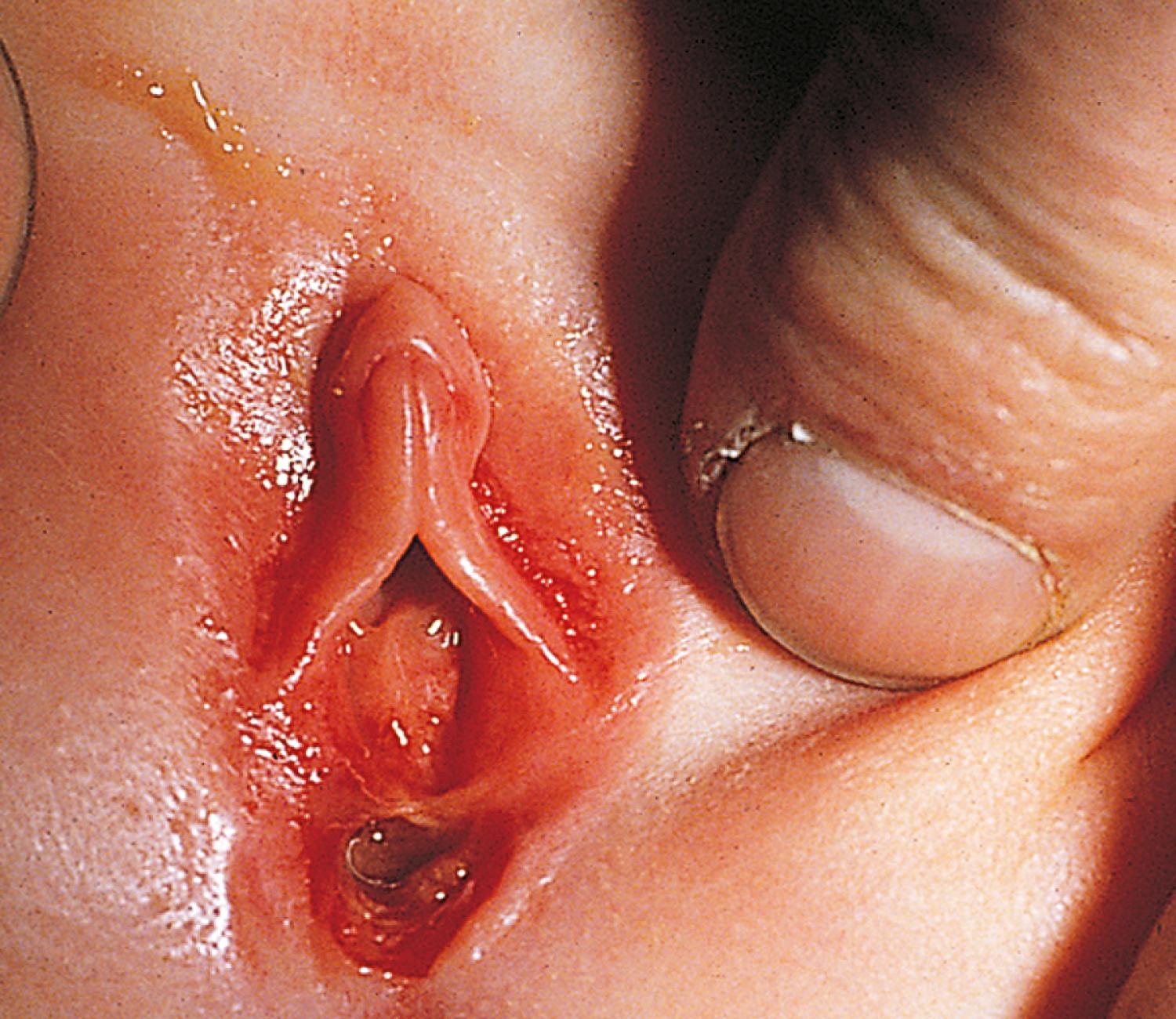
The congenital anomaly referred to as imperforate hymen consists of a thick imperforate membrane located just inside the hymenal ring. This is the most common truly obstructive abnormality. It is frequently missed on the newborn examination because of the redundancy of hymenal folds. However, it may become evident by 8 to 12 weeks old on careful perineal inspection, appearing as a thin, transparent hymenal membrane that bulges when the infant cries or strains. On occasion, young infants have copious vaginal secretions secondary to stimulation by maternal hormones; as a result of this anomaly, they develop hydrocolpos. In such cases, the infant may have midline swelling of the lower abdomen (especially noticeable when the bladder is full) that feels cystic on palpation. Perineal inspection reveals a whitish, bulging membrane at the introitus. The cystic mass may also be palpable on rectal examination. In the presence of a neonatal withdrawal bleed or trauma, a hematocolpos may develop. This presents as a red or purplish bulge ( Fig. 19.12 ). Treatment of an imperforate hymen consists of incision of the membrane to allow drainage, followed by excision of redundant tissue.

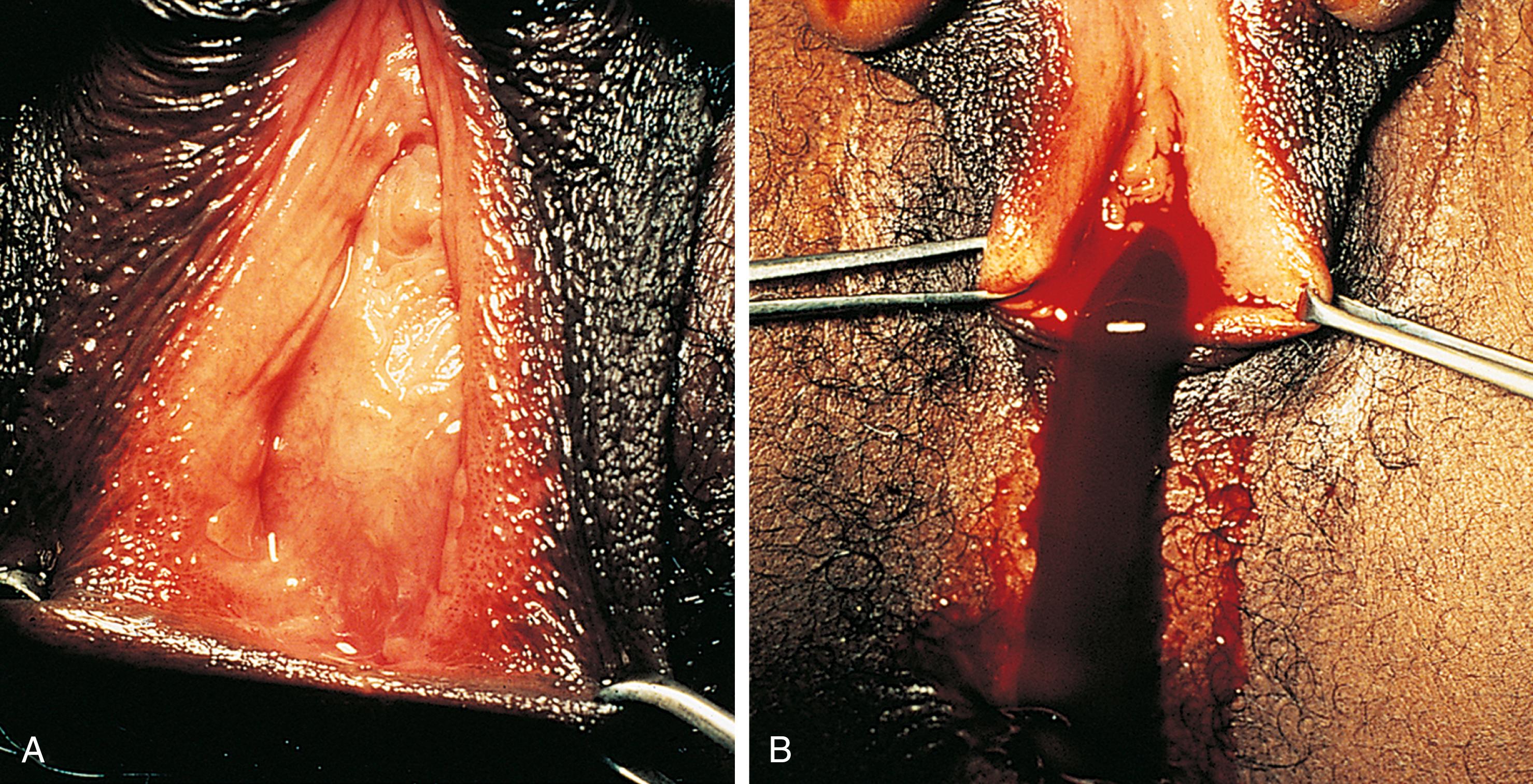
If their condition goes undetected, the patient with an imperforate hymen usually develops hematocolpos in late puberty. The major complaints are intermittent lower abdominal and back pain which rapidly progress in severity and duration. Over time, difficulty in urination and defecation may develop, and a lower abdominal swelling may become noticeable. The patient has well-developed secondary sex characteristics but has had no menstrual periods. Perineal inspection reveals a thick, tense, bulging membrane, often bluish in color, at the introitus ( Fig. 19.13A ). A low cystic swelling is palpable anteriorly on rectal examination. Operative incision allows drainage of the accumulated blood and vaginal secretions (see Fig. 19.13B ) and is followed by excision of the membrane. Other partially obstructive hymenal abnormalities may allow menstrual blood to flow but later cause difficulty inserting tampons or initiating intercourse. Because hymens are not of Mullerian origin, imperforate hymens are not associated with other genitourinary abnormalities.
Other forms of genital tract obstruction ( Box 19.3 ) are rare. In most cases, early routine genital inspection reveals the absence of a vaginal orifice, enabling early delineation of the anomaly and thus facilitating treatment. Proximal obstructing anomalies may not be apparent on physical examination. If missed in infancy or childhood, partial or complete obstruction can present with a wide range of signs and symptoms, such as those listed in Box 19.4 . As noted earlier, ultrasonography is useful in the initial evaluation of for suspected genital tract obstruction, bearing in mind its limitations in visualization of internal reproductive structures after the neonatal period and before puberty, which is when they are very small given minimal amounts of estrogen and gonadotropins. When structures are not seen or when further anatomic detail is required, an MRI is indicated.
Labial fusion (underlying endocrine pathology)
Labial adhesions (partial obstruction)
Female genital cutting sequelae
Imperforate hymen
Vaginal atresia (failure to canalize the vaginal plate)
Vaginal (with or without uterine) agenesis, including Mayer-Rokitansky-Kuster-Hauser syndrome (Mullerian aplasia); congenital absence of the vagina and uterus
Transverse vaginal septum at the junction of the upper one-third and lower two-thirds of the vagina
Longitudinal vaginal septum
Androgen insensitivity (testicular feminization syndrome)
Obstructing Mullerian malformations, with elements of duplication, agenesis, and/or incomplete fusion
Tumors of the upper and lower genital tracts; other pelvic masses
Vaginal, pelvic, or abdominal pain (especially cyclic)
Dysmenorrhea
Urinary tract symptoms
Primary amenorrhea
Irregular vaginal bleeding
Purulent vaginal discharge
Difficulty using tampons
Difficulty initiating intercourse
Dyspareunia
Vaginal, pelvic, or abdominal mass
Hydrocolpos (mucus in vagina)
Hematocolpos (blood in vagina)
Pyohematocolpos (pus and blood in vagina)
Hematometra (blood within the uterus)
The genital structures and pelvic supporting tissues of prepubertal patients are smaller and more rigid than they become during puberty. This inelastic anatomy significantly increases the risks that trauma will result in tearing and/or internal extension of injury. As a result, serious internal injuries of the vagina, rectum, urethra, bladder, and peritoneal structures may underlie deceptively mild external abnormalities, as described later. In contrast to prepubertal patients, adolescents are more likely to have contusions than tears and are less likely to have internal extension of injury unless the applied force is great.
The role of the primary care or emergency physician is to take a thorough history in order to fully understand the mechanism and likely extent of injuries. It is important to pay careful attention to vital signs and to perform as thorough an examination of the abdomen, urethra, hymen, lower vagina, perineal body, and rectum as is feasible while minimizing the patient’s physical discomfort and emotional distress. Specifically, patients should receive appropriate pain medication and emotional support. They should also be protected from multiple examinations, which is a particular risk with consultation from multiple subspecialists, transfer to other institutions, and in teaching hospitals. When history, external inspection, or urinalysis suggests that injuries may be more than superficial, internal examination under anesthesia (by a pediatric surgeon or gynecologist) should be arranged. This enables meticulous inspection, wound exploration, and repair under optimal conditions without further traumatizing the child. Similarly, for the adolescent who is too anxious for a thorough examination, or whose injuries are extensive, examination under sedation or anesthesia is preferred.
For patients whose injuries are related to sexual abuse or assault, all attempts should be made to engage a patient advocate and a pediatric or adult sexual assault nurse examiner. As noted in Chapter 6 , victims of sexual abuse may disclose abuse but more often complain of unexplained bleeding or pain with no history of trauma, and the time of presentation is often significantly delayed.
The majority of superficial perineal trauma cases are the result of mild, blunt force from a straddle injury, minor falls, or sexual abuse. A clear history of the preceding incident (often witnessed) is usually given, and findings fit the reported mechanism of injury. However, accidentally incurred superficial abrasions may not be noticed by parents until the child cries on urination, complains of dysuria, or blood is noticed on the child’s underwear or toilet paper.
Typical lesions include superficial abrasions, mild contusions, and occasionally superficial lacerations ( Fig. 19.14 ). The junction of the labia minora and majora is the site most frequently involved; however, tears of the labia majora or perineal body are not uncommon. In contrast to accidental injuries, those that result from sexual abuse tend to be more posteriorly located and typically involve tears of the posterior portion of the hymen, the posterior fourchette, or perineal body ( Fig. 19.15 ; see Fig. 19.14C and Chapter 6 ).
Patients with superficial injuries may experience mild perineal discomfort and pain on urination but otherwise are asymptomatic. Most of these injuries can be managed supportively with systemic analgesia, topical bacteriostatic and/or anesthetic ointments, warm baths, and careful perineal cleansing. Application of the anesthetic ointment or any barrier emollient before urinating reduces the severity of dysuria, as does urinating in a tub of water. If urinary retention continues to be a problem, use of a topical anesthetic ointment for a few days may be necessary possibly accompanied by systemic pain medication.
Urethral prolapse and lichen sclerosus may cause bleeding and therefore be mistaken for trauma or abuse. See the Common Perineal Conditions section (later) and see Figs. 19.22 and 19.23 .
Moderately forceful blunt trauma often results in perineal tears and hematoma formation ( Fig. 19.16 ). Hematomas of the perineum appear as tender, tense, round swellings with purplish discoloration. Periurethral hematomas may interfere with urination. Vaginal hematomas can result from submucosal tears of the vagina or even mucosal separation with resultant vaginal bleeding or vaginal hematoma formation. The pain of a vaginal hematoma usually is perceived as perineal and/or vaginal but at times is referred to the rectum or buttocks. Inspection through the vaginal orifice reveals a bluish swelling involving one of the lateral walls. This may also be evident as a tender swelling anterolaterally on rectal examination.

Moderate and severe penetrating injuries can be caused by falls onto sharp objects (“picket fence injury”), rape, sexual molestation with phallus-shaped objects, and auto accidents. More extensive injuries are typically associated with significant bleeding. However, even extensive tears may produce minimal pain and blood loss ( Fig. 19.17 ).

Whether the mechanism of injury involves blunt force or penetration, internal extension of injury is possible and can be associated with external genital findings that are deceptively minor in appearance. Internal injury should be suspected when children complain of lower abdominal and perineal pain, which may radiate down the leg. Concerning physical findings include bleeding through the vaginal orifice; a vaginal hematoma; rectal bleeding, rectal tenderness, or abnormal sphincter tone; gross hematuria or inability to urinate; abdominal tenderness especially with guarding or rebound; or hypovolemia, which may not be evident immediately following the injury. All such patients warrant prompt hemodynamic stabilization followed by appropriate imaging, surgical exploration, and repair in the operating room. This obviates the need for extensive examination in the office or emergency department.
Strictly defined, the term vulvovaginitis denotes an inflammatory process involving both the vulva and the vagina. In practice, however, the term prepubertal vulvovaginitis is used less precisely to refer to patients who describe symptoms of dysuria, vulvar pain or itching, or vaginal discharge but who may lack signs of inflammation or who have evidence of only vulvar or vaginal involvement. Vulvovaginal complaints are relatively common in prepubertal patients in part because the labia do not fully cover and thus do not completely protect the vaginal vestibule from friction and external irritants, especially when the child is sitting or squatting. In addition, the unestrogenized vaginal epithelium is thin, relatively friable, and easily traumatized. Transient irritation without discharge is common in the young child as a result of exposure to chemical irritants and inconsistent hygiene. Frictional irritation and poor aeration are also common and can be exacerbated by obesity. Finally, young children are less careful about cleansing their perineum after toileting and avoiding contamination with stool.
Causes of vulvovaginitis are most easily classified into noninfectious and infectious subgroups, with the latter subclassified into nonsexually and sexually transmitted infections. Table 19.4 presents the most common causes of noninfectious vulvovaginitis with specific historic clues suggestive of each condition. Box 19.5 presents the infectious causes. Nonsexually transmitted bacterial pathogens and the herpes simplex viruses (HSVs) often are spread to the vulvovaginal area from another site (e.g., nose, mouth, throat, skin, or gastrointestinal tract) by the patient’s hands. Candida organisms, although a common cause of diaper dermatitis, rarely cause vulvovaginitis in the prepubertal child who is no longer wearing diapers, with the exception of children receiving systemic antibiotics or steroids, or who have underlying diabetes mellitus. In the prepubertal child, vulvovaginitis caused by sexually transmitted pathogens is almost always acquired through sexual contact (see Chapter 6 ). In contrast to adolescents and adults, prepubertal patients are at little risk for internal extension of vulvovaginal infections (cervicitis and pelvic inflammatory disease [PID]) because the unestrogenized genital tract does not support the ascent of infection through the cervix, uterus, and fallopian tubes.
| Condition | Historical Clues |
|---|---|
| Poor hygiene | Recent toilet independence; infrequent bathing, handwashing, and clothing changes; soiled underwear |
| Poor perineal aeration | Tight clothing, nylon underwear, tights, and leotards; wet bathing suits; hot tubs; obesity |
| Frictional trauma | Tight clothing, sports, sand from sandbox or beach play, excessive masturbation or sexual abuse, obesity, hair removal |
| Chemical irritants | See products listed in Box 19.6 |
| Contact dermatitis | Poison ivy; see also Box 19.6 |
| Vaginal foreign bodies | Wiping habits, excessive masturbation or self-exploration, sexual abuse, use of condoms, tampons, or sex toys |
| Parasites, insect bites, infestations | Home environment, pets, sandboxes, travel, camping, exposure to woods or beach |
| Medication-related | Topical steroid or hormone creams, antibiotics, chemotherapy |
| Generalized skin disorders | History of pruritus, chronic skin lesions, prior diagnosis |
| Anatomic anomalies | Vesicovaginal or rectovaginal fistula, ectopic ureter, spina bifida, cloacal anomalies, urogenital anomalies |
| Neoplasms | Discharge, bleeding, bulging abdomen, change in bowel or bladder function, premature puberty, rapid androgenization |
| Systemic illness (Stevens-Johnson syndrome, Crohn disease with perineal fistulas and ulcers, toxic shock syndrome) | Prior infection or medication use; tampon use; evidence from other physical findings including rash, failure to gain weight or height, abdominal pain, diarrhea |
Group A β-hemolytic streptococci
Streptococcus pneumonia
Staphylococci
Candida species a
a Infection rare before puberty.
Herpes simplex virus (HSV) types 1 and 2
Epstein-Barr virus
Varicella-zoster virus
Cytomegalovirus
Escherichia coli
Shigella species
Enterobius vermicularis
Yersinia species
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here