Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The relationship between spontaneous cerebrospinal fluid (CSF) leak and intracranial hypertension has been recognized for nearly two centuries, following the description of a child with hydrocephalus and CSF rhinorrhea in 1826. However, it was not until 1968 when Ommaya et al. suggested a system for classifying nontraumatic spontaneous CSF rhinorrhea that recognized high-pressure leaks as its own category, including known associations with intracranial tumors and hydrocephalus. Ommaya et al. also recognized a group of patients with congenital skull base anomalies, focal atrophy, and osteomyelitic erosion, which they classed as having normal-pressure leaks. Radiographic findings of an empty sella was reported in two patients in this category, but the association with idiopathic intracranial hypertension (IIH) was not recognized at the time.
In the late 20th century, several case reports and case series began to report an association between spontaneous CSF leak and IIH, leading to the recognition of IIH as a separate subcategory of high-pressure leaks. Empty sella continued to be viewed as a distinct entity under the category of normal pressure leaks in the classification criteria at the time. As a result of the advancements made within the field of medical imaging in the past three decades, empty sella is frequently recognized as a magnetic resonance imaging (MRI) sign of IIH and is commonly reported in patients with spontaneous CSF leak. However, empty sella is not a specific sign of IIH and is seen in up to one-third of patients undergoing brain imaging for any clinical indication.
This chapter reviews the evidence for a relationship between spontaneous CSF leak and IIH and discusses the proposed pathophysiology for spontaneous CSF leak in these patients.
Idiopathic intracranial hypertension, historically known by other names, including benign intracranial hypertension and pseudotumor cerebri , is a disorder of unknown etiology that results in isolated intracranial hypertension and its associated signs and symptoms, including papilledema, vision loss, headache, and pulsatile tinnitus. The diagnostic criteria for IIH have evolved since the original Dandy requirements in 1937 and include clinical, neuroimaging, and CSF examination criteria, as well as confirmation of elevated CSF opening pressure on lumbar puncture ( Box 15.1 ).
Required for the diagnosis of IIH
Papilledema
Normal neurologic examination results except for cranial nerve abnormalities
Neuroimaging: normal brain parenchyma without evidence of hydrocephalus, mass, or structural lesion and no abnormal meningeal enhancement on MRI, with and without gadolinium, for typical patients (obese women), and MRI, with and without contrast, and MRV for others; if MRI is unavailable or contraindicated, contrast-enhanced CT may be used
Normal CSF composition
Elevated lumbar puncture CSF opening pressure (≥25 cm CSF in adults and ≥28 cm CSF in children [25 cm CSF if the child is not sedated and not obese]) in a properly performed lumbar puncture
Diagnosis of IIH is definite if the patient fulfils criteria A–E. The diagnosis is considered probable if criteria A–D are met but the measured CSF pressure is lower than specified for a definite diagnosis.
A striking overlap exists in the demographic, clinical, and radiologic characteristics of patients with IIH and those with spontaneous CSF leaks. Both conditions mainly affect women (~70%–80%) and obese patients. , Paralleling the global obesity epidemic, the annual incidence of IIH increased by twofold between 2002 and 2016 in the United Kingdom, in line with increasing body mass index (BMI) rates. In the United States, a significant increase in the incidence of IIH was observed between 1997 and 2016. Similarly, the rate of craniotomy for spontaneous CSF leak repair in the US rose twofold between 2002 and 2012. The rate was twice as high in regions with the highest obesity rate compared with the lowest obesity rate. During the same period, there was no change in the rate of repair for nonspontaneous CSF leak. Patients with spontaneous CSF leak are older than patients with IIH, perhaps because of delayed presentation because CSF leak may act as a “safety valve” against raised ICP and relieve the signs and symptoms of IIH. ,
Patients with spontaneous CSF leaks may also present with signs and symptoms of intracranial hypertension. The pooled prevalences of headache and pulsatile tinnitus in patients with spontaneous CSF leaks were 60% and 20%, respectively, compared with 90% and 60% in patients with IIH. The lower prevalence of headache and pulsatile tinnitus observed in patients with spontaneous CSF leak is not surprising, given that CSF leak may relieve ICP and the signs and symptoms of IIH. CSF leak likely also explains the low prevalence of papilledema before leak repair, which is approximately 5% using pooled data from larger case series. However, it is also possible that the lower prevalence of signs and symptoms of intracranial hypertension may be attributable underreporting or lack of funduscopic examination before leak repair. A recent study of 36 patients with spontaneous CSF leak who underwent systematic neuro-ophthalmologic examination found at least 14% with evidence of papilledema or resolved papilledema before surgery.
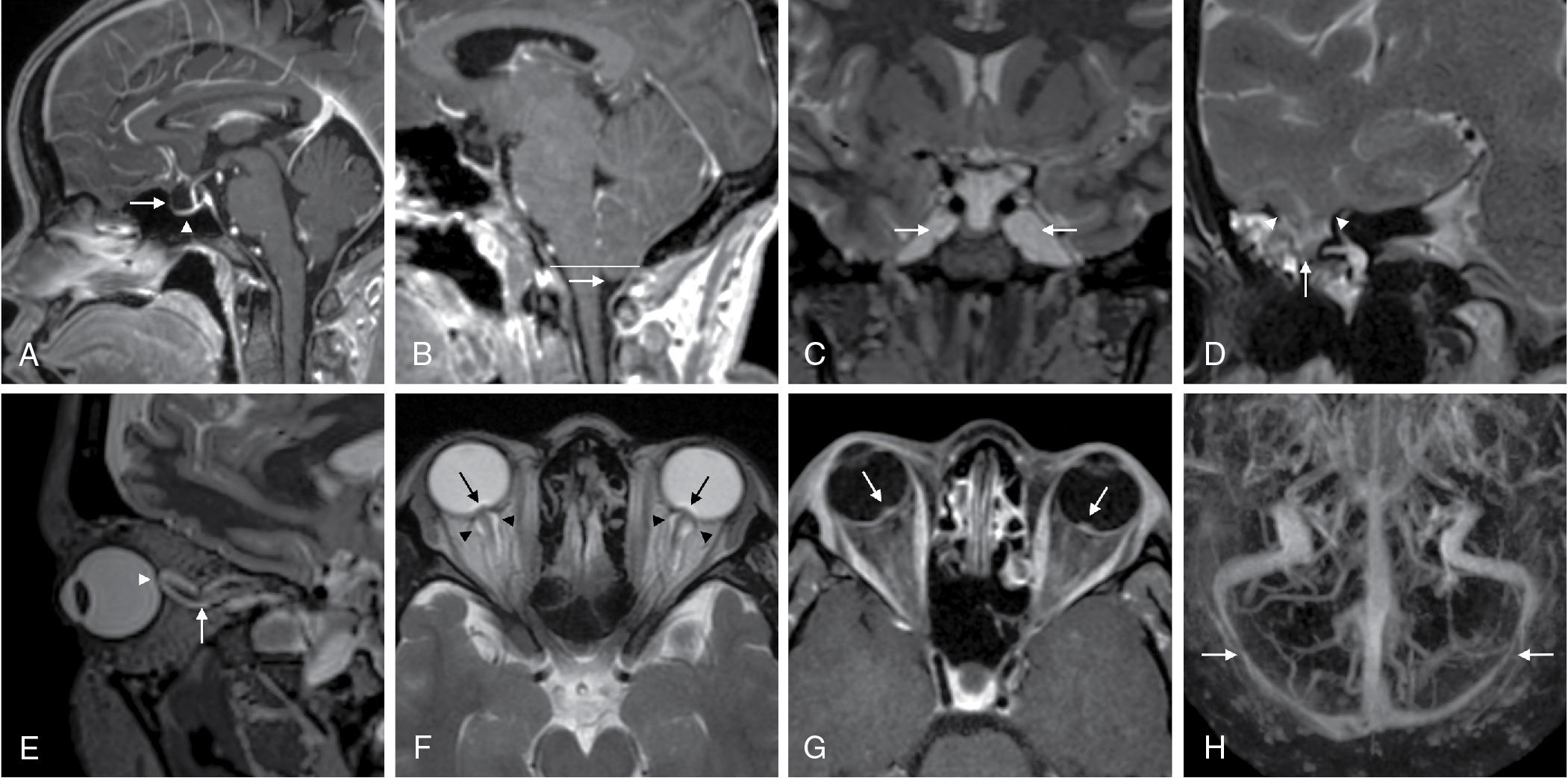
Radiologic signs in IIH include those attributed to osseous erosion such as empty sella, meningoceles, encephaloceles, and enlarged Meckel caves, as well as those attributed to mechanical deformation of the perioptic tissues secondary to raised ICP such as posterior scleral flattening and optic nerve tortuosity ( Fig. 15.1 ). A study comparing patients with spontaneous CSF leak and an unmatched group with definite IIH found that the prevalence of completely empty sella and encephaloceles were significantly higher in CSF leak patients (31% and 90%, respectively) compared with IIH patients (9% and 24%, respectively). The prevalence of optic nerve head protrusion and enhancement, posterior scleral flattening, and prominent perioptic CSF space was significantly higher in IIH patients. As emphasized earlier, this is likely because CSF leak acts as a “safety valve” against raised ICP, relieving mechanical deformation of the perioptic tissues, while signs of osseous erosion persist even after ICP normalizes.
There has only been one study to date that has sought to determine the prevalence of IIH in patients with spontaneous CSF leak, through systematic neuro-ophthalmologic evaluation including fundus examination and pre- and postleak repair. The prevalence of presumed or definite IIH at any time was found to be 27.8% (10 of 36 patients) based on the most recent IIH diagnostic criteria. , Most of these patients (16.7%, 6 patients) had a preexisting diagnosis or presumed diagnosis of IIH. A minority (6%, 2 patients) were diagnosed with IIH after they developed CSF leak, including 1 patient who developed new-onset papilledema after surgical repair of the leak. Diagnosing IIH is very difficult in patients with spontaneous CSF leak who often do not have papilledema. However, one study showed that patients with CSF leak with transverse venous sinus stenosis on brain magnetic resonance venography have a higher risk of developing symptoms and signs of intracranial hypertension after CSF leak repair, suggesting that finding transverse venous sinus stenosis preoperatively may potentially alter perioperative management.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here