Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Venous thromboembolism (VTE) is a significant national health problem, with approximately 900,000 individuals affected annually. When compared with whites, African Americans have a 40% higher incidence of VTE. Despite improvements in prophylaxis and treatment of VTE, the incidence of this disease has not changed significantly over the past 25 years. Deep vein thrombosis (DVT) affects around 380,000 patients annually, and pulmonary embolism (PE) is diagnosed yearly in at least 520,000 patients. Treatment costs to the U.S. health care system reach billions of dollars per year just for the acute treatment of venous thrombosis. The national importance of venous thromboembolism to our health care system has been documented in the Surgeon General’s Call to Action to Prevent Deep Venous Thrombosis and Pulmonary Embolism. This Call to Action specifically requested a multiagency approach to developing evidence-based practice guidelines to combat this disease.
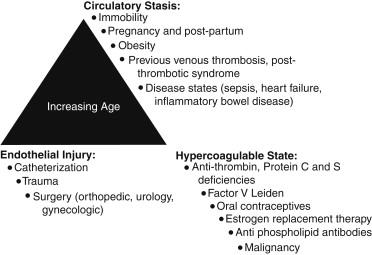
The factors that could lead to or interact with one another to lead to VTE include blood stasis, endothelial injury, and blood hypercoagulability. Of these three factors, vein wall endothelial injury triggers a local inflammatory response, which promotes a prothrombotic state driven by tissue factor, adhesion molecules, hemostatic factors, and proinflammatory cytokines that support acute VTE. In 1974, it was first hypothesized that vascular inflammation and thrombosis are interrelated. The original hypothesis suggested that prothrombotic factors lead to the activation of leukocytes and platelets. This process promotes thrombus amplification via adherence and layering of the activated platelets and leukocytes. Risk factors for acute VTE include increasing age, pregnancy, prolonged periods of immobility, estrogen therapy, surgery and trauma, malignancies, hypercoagulable states, cardiovascular disease (myocardial infarction, congestive heart failure), inflammatory diseases, obesity, and for VTE recurrence male gender ( Figure 1 ).
The aging process is an important common denominator in the development of VTE. The incidence of DVT is 2 to 7 times higher in those older than 55 years as compared to younger age groups, and the incidence increases 74% per decade of age over 45 years. With aging, the anatomy of the venous vessel wall is adversely modified. Thickening of venous valve cusps caused by increases in valve collagen and intimal thickening with age has been documented.
The vascular inflammatory response is initially protective by nature; its role is to promote the recruitment of inflammatory cells for the removal of microorganisms and endotoxins. However, local and systemic inflammation can produce a prothrombotic environment driven by platelet activation, tissue factor, prothrombotic microparticles (MPs), adhesion molecules, hemostatic factors, and proinflammatory cytokines.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here