Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term paraneoplastic syndrome is often used to refer to symptoms or signs resulting from dysfunction of organs or tissues caused by a cancer, but which are not a direct effect of invasion by the neoplasm or its metastases. Perhaps most accurately, the term is used in a restricted sense to describe specific neurologic disorders that occur with increased frequency in patients with certain cancers, and are not caused by invasion, infection, systemic metabolic disorders, vascular disease, or side effects of cancer therapy. Paraneoplastic syndromes may affect virtually any organ or tissue ( Table 27-1 ), including multiple regions within the nervous system ( Table 27-2 ). These disorders, also termed remote effects of cancer on the nervous system , detailed in Table 27-3 , are typically immune mediated, and encompass a clinically and pathologically more restricted group of disorders than the other nonmetastatic effects of cancer. In addition to paraneoplastic immune-mediated disorders, this chapter addresses the increasingly recognized group of immune-mediated neurologic syndromes which have similar clinical features to the more traditionally recognized paraneoplastic syndromes but occur without an associated cancer. These nonparaneoplastic immune-mediated syndromes are important to understand as they are often more responsive to immunotherapies than their closest counterpart paraneoplastic conditions.
| General Physiologic (Host-Reactive) Syndromes |
| Fever |
| Anorexia and cachexia |
| Fatigue and “weakness” |
| Dysgeusia |
| Hematologic and Vascular Syndromes |
| Anemia |
| Leukemoid reaction |
| Eosinophilia, basophilia |
| Thrombocytosis |
| Thrombocytopenia |
| Hypercoagulability (Trousseau syndrome) |
| Erythrocytosis |
| Hyperviscosity |
| Skin and Connective Tissue Syndromes |
| Acanthosis nigricans |
| Tripe palms |
| Erythemas |
| Pruritus |
| Vasculitis |
| Flushing |
| Sweet syndrome |
| Ichthyosis |
| Hypertrichosis |
| Pachydermoperiostosis |
| Melanosis, vitiligo |
| Endocrine-Metabolic Syndromes |
| Cushing syndrome |
| Hypoglycemia and hyperglycemia |
| Syndrome of inappropriate secretion of antidiuretic hormone (SIADH) |
| Carcinoid syndrome |
| Hypercalcemia and hypocalcemia |
| Systemic nodular panniculitis |
| Acromegaly |
| Gynecomastia |
| Hypernatremia |
| Gastrointestinal Syndromes |
| Protein-losing enteropathy |
| Malabsorption |
| Exudative enteropathy |
| Zollinger–Ellison syndrome |
| Collagen-Vascular Syndromes |
| Arthritides |
| Scleroderma |
| Lupus erythematosus |
| Amyloidosis |
| Palmar fasciitis |
| Renal Syndromes |
| Glomerulonephritis |
| Nephrotic syndrome |
| Renal failure |
| Hypokalemia |
| Bone Syndromes |
| Hypophosphatemic osteomalacia |
| Pulmonary osteoarthropathy |
| Clubbing |
| Synovitis |
| Disorder | Example(s) |
|---|---|
| Vascular disorders | Hemorrhage/infarction |
| Infections | Meningitis/abscess |
| Nutritional disorders | Wernicke encephalopathy |
| Metabolic disorders | Hypocalcemia |
| Side effects of therapy | |
| Surgery and other diagnostic or therapeutic procedures | Meningitis/CSF leak |
| Radiation therapy | Brain/spinal cord necrosis |
| Chemotherapy/small molecules | Peripheral neuropathy |
| Biologic therapy | PML |
| “Remote” or paraneoplastic syndromes | (see Table 27-3 ) |
| Brain |
| Limbic encephalitis * |
| Encephalomyelitis * |
| Hypothalamic encephalitis |
| Brainstem/basal ganglia encephalitis |
| Cerebellar degeneration * |
| Opsoclonus myoclonus * |
| Visual loss |
| Carcinoma/melanoma retinopathy * |
| Optic neuropathy |
| Spinal Cord |
| Myelitis/myelopathy |
| Demyelinating myelopathy |
| Neuromyelitis optica |
| Necrotizing myelopathy |
| Motor neuron syndromes |
| Subacute motor neuronopathy |
| Amyotrophic lateral sclerosis (ALS) |
| Stiff-person syndrome |
| Peripheral Nerve/Dorsal Root Ganglia |
| Subacute sensory neuronopathy * |
| Chronic/subacute sensory or sensorimotor neuropathy |
| Autonomic neuropathy * |
| Acute sensorimotor neuropathy (Guillain–Barré syndrome) |
| Plexitis (e.g., brachial neuritis) |
| Vasculitic neuropathy |
| Association with plasma cell dyscrasias |
| Neuromuscular Junction |
| Lambert–Eaton myasthenic syndrome * |
| Myasthenia gravis * |
| Neuromyotonia |
| Muscle |
| Dermatomyositis * |
| Polymyositis |
| Inclusion-body myositis |
| Necrotizing myopathy |
| Cachectic myopathy |
| Myotonia |
Several studies have addressed the frequency of paraneoplastic and nonparaneoplastic syndromes. Wide-ranging estimates from these studies are due to: (1) varied definitions; (2) the rigor used to exclude other causes of neurologic dysfunction; (3) the care with which the neurologic evaluation was performed; and (4) biases introduced by referral patterns. For example, the Lambert–Eaton myasthenic syndrome (LEMS) occurs in 3 percent or less of patients with small cell lung cancer (SCLC), but about 50 percent of SCLC patients have either subjective or objective muscle weakness. While less than 10 percent of cancer patients had a “neuromyopathy” on physical examination, abnormalities of peripheral nerve function were found by quantitative sensory testing in nearly half. Myopathic changes are found on muscle biopsy in one-third of patients with lung cancer. These neurologic symptoms can predate the detection of cancer; in patients with peripheral sensory neuropathy of unknown cause, for instance, nearly one-third in some studies developed cancer within 6 years.
True incidence figures for paraneoplastic syndromes are rare. Population-based data are available for myasthenia gravis, LEMS, and dermatomyositis. A total of 5 percent of myasthenia gravis patients have a paraneoplastic form. In another study, the annual incidence of LEMS was rare (0.4 per million persons), but was equally divided between those with SCLC and those with nonsmall cell lung cancer (NSCLC). For dermatomyositis, the overall age- and sex-adjusted incidence is around 10 per million persons; 20 percent have cancer. Nearly one-fifth in one study suffered from the amyopathic subtype (rash but no muscle weakness).
Other studies have addressed the percentage of patients with a given tumor likely to have a paraneoplastic syndrome. Myasthenia gravis occurs in 10 to 15 percent of patients with thymoma. LEMS has been found in about 3 percent of patients with lung cancer. Paraneoplastic peripheral neuropathy occurs in 10 percent of malignant monoclonal gammopathies, and in 50 percent of patients with osteosclerotic myeloma. Most known paraneoplastic syndromes are so uncommon that exact incidence figures cannot be established, but they probably occur in less than 0.01 percent of cancer patients.
A higher yield is found when patients whose symptoms suggest the possibility of a paraneoplastic syndrome have serum and cerebrospinal fluid (CSF) sent for examination for paraneoplastic antibodies. Using this approach, one-fourth of consecutive patients examined over 2 years have well-defined antineuronal autoantibodies.
Although the exact pathogenesis of most paraneoplastic syndromes has not been established, the consensus is that most, or perhaps all, neurologic paraneoplastic syndromes are immune-mediated. Evidence for this hypothesis includes the presence of autoantibodies that recognize antigens present in both the cancer and the normal nervous system. Some of these so-called paraneoplastic or onconeural antigens are also expressed in normal testes, an organ that, like the brain, is an immunologically privileged site. If the antigen cannot be identified in a cancer with a known serum paraneoplastic antibody, it may be that either the patient does not have a paraneoplastic syndrome or that some other cancer is present and caused the disorder. Examination of the CSF of patients with paraneoplastic syndromes involving the central nervous system (e.g., limbic encephalitis) usually reveals a pleocytosis, at least early in the course of the disease, with a persistently slightly elevated protein level, an increased IgG Index, and oligoclonal bands. Some of these oligoclonal bands in the CSF have been identified as paraneoplastic antibodies themselves. The relative specific level of the paraneoplastic antibody (expressed as a concentration of antibody against total IgG) is substantially higher in CSF than in the serum. This indicates that the antibody was synthesized by B cells within the central nervous system (CNS), rather than simply diffusing across the blood–brain barrier. The tumors of patients with paraneoplastic syndromes, although identical in histologic type to tumors of patients without neurologic features, are more likely to be infiltrated with inflammatory cells including T cells, B cells, and plasma cells. The nervous system is usually also infiltrated by inflammatory cells, and some paraneoplastic syndromes respond to treatment with immunosuppression.
The current concept of the pathogenesis of paraneoplastic syndromes is that the tumor ectopically expresses an antigen that is normally expressed in the nervous system. Onconeural antigens are present in the tumors of all patients with antibody-positive paraneoplastic syndromes. In some tumors, such as SCLC, onconeural antigens are present in all tumors, even in those patients who do not develop paraneoplastic antibodies or a paraneoplastic syndrome. The onconeural antigen in the tumor cell is probably recognized by the immune system when tumor cells spontaneously undergo apoptosis and the apoptotic bodies containing the antigen are phagocytized by antigen-presenting cells. Current evidence conflicts as to whether the antigens in the tumor are mutated or identical in structure to normal neural antigens. The former would provide a mechanism for loss of tolerance, leading to development of paraneoplastic antibodies. The body’s immune system attacks structures expressing the paraneoplastic antigen, resulting in two effects. First, the immune attack may control the growth of the tumor and in rare instances obliterate it. Second, the immune response also attacks the nervous system itself; both B and T cells can be found in the CNS of patients with CNS paraneoplastic syndromes. The B cells generally reside in the perivascular spaces and the T cells in both perivascular spaces and in the brain parenchyma. Often the granzyme-B-expressing cytotoxic T cells are closely opposed to neurons. Further, the T cells found in the nervous system are either mono- or oligoclonal and respond only to a specific antigen. Hence, these diseases appear to be T-cell driven.
By contrast, consensus suggests that autoantibodies which target the native extracellular domains of neuronal proteins are far more likely to be directly pathogenic, as they are likely to access their target antigen in vivo. Indeed, two paraneoplastic syndromes with antibodies that target the extracellular domains of proteins expressed at the human neuromuscular junction, LEMS and myasthenia gravis, were the first to meet formal criteria for an antibody-mediated autoimmune disease. Other paraneoplastic syndromes in which antibodies likely play a causal role include NMDA receptor antibody-associated encephalitis, CASPR2 antibody-associated Morvan syndrome, AMPAR-associated encephalitis, and autonomic neuropathy with antibodies to the ganglionic acetylcholine (ACh) receptor. In addition, a variety of syndromes with autoantibodies that target the extracellular domains of native neuroglial surface proteins have no tumor associations. These include autoantibodies against leucine-rich glioma inactivated 1 (LGI1), Iglon5, the GABA A receptor, aquaporin-4 (AQP4), and myelin oligodendrocyte glycoprotein (MOG).
Recommended criteria for the diagnosis of a neurologic paraneoplastic syndrome are listed in Table 27-4 . Alternative causes that might explain the clinical symptoms must be excluded. “Classic” refers to those neurologic disorders characteristic of a paraneoplastic syndrome as indicated in Table 27-5 . Hence, a clear clinical definition of the syndrome is required. “Onconeural” refers to antibodies that recognize antigens that are restricted to the nervous system (or testes) and to some cancers. Originally, when the antigens were unknown, two separate nomenclatures were devised to designate these antibodies. The nomenclature applied at Memorial Sloan-Kettering Cancer Center (e.g., Yo, Hu) refers to the first two letters of the last name of the index patient while the Mayo Clinic terminology (e.g., anti-PCA-1, anti-ANNA-1) refers to the staining pattern by immunohistochemistry. In Table 27-5 the latter system is identified in parentheses. Once these antigens have been identified, the antigen’s name is used to designate the antibody in question (e.g., NMDAR antibody). The term “well-characterized” refers to an antibody whose antigen has been robustly identified, typically by multiple laboratories.
| Definite PNS |
|
| Possible PNS |
|
| Antibody Target | Location | Antigen/Gene(s) | Extracellular or Intracellular Epitope | Usual Tumor or Site of Origin | Neurologic Disorder |
|---|---|---|---|---|---|
| Antibody Markers of Neurologic Paraneoplastic Syndromes, Requiring a Search for Tumor | |||||
| Hu (ANNA-1) | Nucleus>cytoplasm (all neurons) | HuD (Elavl4); Elavl2, 3 | Intracellular | SCLC, neuroblastoma, prostate | PEM, PSN, autonomic dysfunction |
| Yo (PCA-1) | Cytoplasm, Purkinje cells | CDR2, CDR2L | Intracellular | Ovary, breast, lung | PCD |
| Ri (ANNA-2) | Nucleus>cytoplasm (CNS neurons) | Nova 1,2 | Intracellular | Breast, gynecologic, lung, bladder | Ataxia/opsoclonus, brainstem encephalitis |
| CRMP5 (CV2) | Cytoplasm, oligodendrocytes, neurons | Intracellular | SCLC, thymoma | PEM, PCD, chorea, optic, sensory neuropathy | |
| Ma2 (ANNA-3) | Neurons (nucleolus) | Intracellular | Testis | Limbic, brainstem (diencephalic) encephalitis | |
| Amphiphysin | Presynaptic | Intracellular synaptic | Breast, SCLC | SPS | |
| Sox-1 (AGNA-1) | Nucleus of Bergman glia, other neurons | Intracellular | SCLC | LEMS | |
| Tr (PCA-Tr) | Cytoplasm, dendrites of Purkinje cells | DNER | Intracellular | Hodgkin | PCD |
| Recoverin | Photoreceptor, ganglion cells | Recoverin | Intracellular | SCLC | CAR |
| Antibodies Associated With Neurologic Dysfunction That Do Not Always Require a Search for Cancer | |||||
| AChR | Postsynaptic NMJ (electron immunohistochemistry) | AChR | Extracellular | Thymoma | MG |
| VGCC | Presynaptic NMJ | P/Q VGCC | Extracellular | SCLC | LEMS |
| NMDAR | Neuronal cell surface, hippocampus, other brain regions | NR1 subunit | Extracellular | Ovarian teratoma | Encephalitis |
| AMPAR | Neuronal cell surface | GluR1,2 subunits | Extracellular | Thymoma, breast, lung | LE |
| AChR | Postsynaptic NMJ | Skeletal muscle AChR | Extracellular | Thymoma | MG |
| nAChR | Postsynaptic ganglia | Ganglionic α3 subunit | Extracellular | SCLC, thymoma | Autonomic neuropathy |
| LGl1 | Neuropil | LGI1 | Extracellular, secreted molecule | Thymoma, rarely | LE |
| CASPR2 | Neuropil and juxtaparanode | Extracellular | Thymoma | Peripheral nerve hyperexcitability, Morvan syndrome | |
| GAD | Purkinje cell cytoplasm, nerve terminals, other neurons | Glutamic acid decarboxylase 65 and 67 | Intracellular | Several (renal, Hodgkin, SCLC) | SPS, cerebellar ataxia |
| Glycine receptor | Brainstem, spinal cord neurons | α1 subunit | Extracellular | Lung | PERM |
| GABA A R | Neuronal surface | α1/B3/y2 subunits | Extracellular | ? | SPS |
| GABA B R | Neuronal surface | B1/2 subunits | Extracellular | SCLC | LE |
| MuSK | Muscle | MuSK | Extracellular | Thymoma | MG |
| Antibodies in Neurologic Disorders From Single Case Reports or Small Series. Some Are Paraneoplastic | |||||
| PCA-2 | Purkinje cytoplasm and other neurons | Intracellular | SCLC | PCD | |
| Ma | Neurons (subnucleus) | Ma1 and Ma2 | Intracellular | Lung, others | PEM, brainstem |
| ANNA 3 | Nuclei, Purkinje cells | Intracellular | Lung | Sensory neuronopathy, PEM | |
| mGluR1, mGluR5 | Purkinje cells, Olfactory neurons, hippocampus | Metabotropic glutamate receptors | Extracellular | Hodgkin | PCD |
| Kelch-like protein 11 | Multifocal | KLHL11 | Intracellular | Testicular seminoma | Encephalitis |
| PDE10A | Basal ganglia | Intracellular | Varied | Varied | |
| Zic4 | Nuclei of cerebellar | Intracellular | SCLC | PCD | |
| PKC-gamma | Purkinje cells | Intracellular | NSCLC | PCD | |
| Gephyrin | Postsynaptic membranes | Intracellular | Unknown primary | SPS | |
| Synaptotagmin | Presynaptic junction | Intracellular, vesicle protein | ? | LEMS | |
| Synaptophysin | Presynaptic junction | Intracellular, vesicle protein | SCLC | Neuropathy | |
| BRKSK2 | Neuronal cytoplasm | Intracellular | SCLC | LE | |
| Adenylate kinase 5 | Neuronal cytoplasm | Intracellular | Nil | LE | |
| CARP VIII | Purkinje cells | Intracellular | Melanoma | PCD | |
| Homer 3 | Neuropil, cerebellum | Intracellular | None known | PCD | |
| Aquaporin 4 | Astrocyte foot process | M23>M1 isoform | Extracellular | Rare | Neuromyelitis optica |
The 5-year period identified in the criteria for the development of cancer is reasonable but problematic. Although in most patients with a paraneoplastic syndrome the cancer is identified within a year or so, in an occasional patient, even when the neurologic syndrome and the antibody clearly have been recognized, more than 5 years may elapse before the cancer is found. The inability to find a cancer, even after 5 years, does not mean that the patient does not have a paraneoplastic syndrome. There are rare, but well-documented, cases of a paraneoplastic syndrome being associated with spontaneous remission of a cancer. Also, there are occasional patients with high-titer, well-characterized paraneoplastic antibodies who almost certainly never have had nor will develop a cancer.
The only unequivocal method of determining whether a given patient has a paraneoplastic syndrome is by identifying an autoantibody that reacts with the portion of the nervous system suffering damage and a neoplasm whose cells express the same antigen. If the antigen is not found in the neoplasm, the patient either does not have a paraneoplastic syndrome or has another cancer—as yet unfound—that expresses the antigen, and a new search should be considered.
Several clinical features can assist in the diagnosis. Most paraneoplastic syndromes develop rapidly, progress over weeks to months, and then stabilize; syndromes that begin insidiously or are characterized by exacerbations and remissions are less likely to be paraneoplastic. Many paraneoplastic syndromes result in serious neurologic disability although those with antibodies to neuronal surface epitopes are often responsive to immunotherapies. Paraneoplastic syndromes affecting the CNS are typically associated with an inflammatory CSF, including pleocytosis, elevated levels of protein, increased CSF immunoglobulins, and unique oligoclonal bands; one of these features is present in nearly all patients with a CNS paraneoplastic syndrome. Magnetic resonance imaging (MRI) may be normal or have abnormalities consistent with the clinical findings (e.g., medial temporal lobe T2-weighted hyperintensity in patients with limbic encephalitis or cerebellar atrophy in patients with paraneoplastic cerebellar degeneration). When the MRI is normal, fluorodeoxyglucose positron emission tomography (PET) scans may reveal hypometabolism in the brain that is either diffuse or focal, although these findings are nonspecific. Several of the paraneoplastic syndromes (e.g., LEMS) are so stereotypic that the correct diagnosis can be strongly suspected even before additional diagnostic testing has excluded alternative diagnoses.
Many paraneoplastic syndromes are characterized by serum and CSF autoantibodies which react with both the areas of the nervous system involved and the underlying cancer. Some autoantibodies (e.g., Hu, Ri, and Yo antibodies) are highly specific for the presence of an underlying cancer and strongly suggest a specific cancer that can guide workup. For example, the Yo antibody is strongly associated with breast and gynecologic tumors and requires careful mammography as well as pelvic imaging. However, some paraneoplastic syndromes can be caused by many tumors, and therefore a more widespread search including total-body computed tomography (CT) or PET scan is frequently appropriate. Table 27-5 lists many of the antibodies that can be found in the serum of patients with paraneoplastic syndromes. Other autoantibodies (e.g., ACh receptor antibodies), however, are found in patients both with and without cancer. It is usually not necessary to measure antibodies in the CSF of patients in whom serum antibodies are negative. Yet, in the case of a few autoantibodies, since serum has a high total IgG level which inherently increases the test background, it is often useful to study CSF in conjunction. This is supported by the observation that patients with CNS paraneoplastic syndromes often show a higher relative concentration of the autoantibody in CSF than serum, indicating its intrathecal synthesis.
Most paraneoplastic antibodies are usually associated with specific paraneoplastic syndromes and a limited number of implicated cancers ( Table 27-5 ). For example, the Hu-antibody is more likely to cause encephalomyelitis and is usually associated with SCLC, whereas the CRMP5 antibody is more likely to be associated with cerebellar ataxia, chorea, optic neuritis, uveitis, and LEMS. Both of these antibodies are associated with SCLC, but only the CRMP5 antibody is associated with thymoma. Regardless of the tumor type, patients with the CRMP5 antibody survive significantly longer, a finding that does not appear to be related to a less severe neurologic disorder than those patients with the Hu antibody.
As discussed above, antigens can be divided into two groups: group 1 consists of intracellular antigens, either cytoplasmic or nuclear, and group 2 consists of antigens expressed on the surface of neurons whose extracellular domains are the autoantibody targets. This division identifies disorders that usually respond to treatment and in which antibodies are likely causal (group 2), and those that usually do not respond to treatment and where the pathogenesis is likely T-cell mediated (group 1).
Group 1 antigens that usually are paraneoplastic, including Hu, Yo, and several others, may occur only occasionally in patients without cancer. In one series of Hu antibody positive patients, 3 percent with clinical follow-up of more than 3 years did not develop an identifiable cancer, and there was no clinical differences between those patients who did and did not develop cancer. One possible explanation is that a cancer was present but spontaneously regressed. Both spontaneous regression of the cancer and antineuronal antibodies are thought to be more common in infants with neuroblastoma. Group 1 also consists of intracellular antigens that are cancer-specific but not usually helpful in diagnosis, including Sox 1 and Zic. Other intracellular antigens are associated with autoimmune disorders of the nervous system that are only sometimes paraneoplastic, including glutamic acid decarboxylase (GAD). Indeed, some authors prefer to classify GAD and amphiphysin in a separate group of intracellular synaptic antigens, in recognition of the potential for these autoantibodies to access their targets upon vesicle fusion with the presynaptic membrane.
Group 2 antigens can be divided into those surface antigens associated with autoimmune CNS syndromes that are often associated with an underlying tumor, such as the AMPAR and GABA B R, and those which are only sometimes paraneoplastic, including CASPR2 and the NMDAR. In addition, it is increasingly recognized that some cell surface targets have a very limited, if not absent, epidemiologic association with an underlying tumor; examples include LGI1 and Iglon5.
Overall, patients with autoantibodies to intracellular antigens respond less well to immunologic therapeutic interventions than those in group 2. Nevertheless, there are two general approaches to the treatment of paraneoplastic neurologic disorders. In many cases, effective therapy focuses on treatment of the underlying tumor. This aims to prevent progression of the disease and, in some instances, leads to improvement or, more rarely, complete amelioration of the neurologic symptoms. Effective treatment of the tumor may remove the inciting antigen and thus dampen the immune response causing the neurologic damage.
Because paraneoplastic syndromes are likely immune mediated, the second treatment approach is to suppress the immune response. Several different forms of immunosuppression, including corticosteroids, plasma exchange, intravenous immunoglobulin, cyclophosphamide, and cyclosporine or tacrolimus, have been used to treat paraneoplastic syndromes ( Table 27-6 ). This immunosuppression does not appear to worsen the outcome of the tumor, and may sometimes associate with stabilization or improvement of the syndrome, especially if administered early.
| Syndrome | Treatment |
|---|---|
| Syndromes That Usually Respond to Treatment * | |
| Lambert–Eaton myasthenic syndrome | IV immunoglobulin, plasma exchange, 2,3 diaminopyridine, immunosuppression † |
| Myasthenia gravis | IV immunoglobulin, plasma exchange, immunosuppression, anticholinesterases |
| Dermatomyositis | IV immunoglobulin, immunosuppression |
| Opsoclonus-myoclonus (pediatric) | IV immunoglobulin, corticosteroids, ACTH, rituximab |
| Neuropathy associated with osteosclerotic myeloma | Radiation, chemotherapy |
| NMDAR | First line: corticosteroids, IV immunoglobulin, plasma exchange; |
| Second line: cyclophosphamide, rituximab | |
| LGI1 | Corticosteroids, IV immunoglobulin, plasma exchange |
| Encephalitis with cell surface antigens other than NMDAR and LGI1 (e.g., AMPA receptor, GABA A/B receptor, CASPR2) | Corticosteroids, IV immunoglobulin, plasma exchange, cyclophosphamide |
| Syndromes That May Respond to Treatment * | |
| Stiff-person syndrome | IV immunoglobulin, rituximab, diazepam, baclofen |
| Neuromyotonia | IV immunoglobulin, plasma exchange, phenytoin, carbamazepine |
| Guillain–Barré/CIDP | IV immunoglobulin, plasma exchange |
| Vasculitis of nerve and muscle | Corticosteroids, cyclophosphamide |
| Opsoclonus-myoclonus (adults) | Corticosteroids, cyclophosphamide, protein A column, clonazepam, thiamine |
| MAG-antibody associated peripheral neuropathy (Waldenström macroglobulinemia) | IV immunoglobulin, plasma exchange, chlorambucil, cyclophosphamide, fludarabine, rituximab |
| Acute necrotizing myopathy | Immunosuppression |
* Syndromes that usually do not respond to treatment include encephalomyelitis, sensory neuronopathy, autonomic dysfunction, cerebellar degeneration, and cancer- and melanoma-associated retinopathy.
† Immunosuppression includes corticosteroids or azathioprine.
Despite these interventions, many patients with autoantibodies against group 1 antigens show limited improvement. By contrast, patients with autoantibodies against cell surface-exposed epitopes (e.g., the NMDAR or LGI1) are highly likely to respond to immunotherapy, maybe in part since many such patients do not have an underlying cancer. Treatment outcomes in these patients can frequently be almost complete. With regard to a potential third group of autoantibodies that lie intracellularly within synapses (e.g., GAD and amphiphysin antibodies), the patients may or may not have cancer and may respond well to immunosuppression.
Paraneoplastic syndromes that affect the nervous system are classified in Table 27-5 . Only some of the more common syndromes are considered in this chapter, and more extensive reviews are available elsewhere.
Limbic encephalitis is characterized by the acute-to-subacute onset of short-term memory loss, seizures, and behavioral abnormalities. The disorder has been reported in association with a variety of tumors including SCLC and ovarian teratoma. A clinically identical autoimmune disorder occurs in patients without cancer, and both the paraneoplastic and nonparaneoplastic forms of limbic encephalitis are associated with a variety of different autoantibodies.
Limbic encephalitis can begin with seizures and changes in mood and personality. Accompanying features include severe impairment of recent memory with relatively preserved remote memory. Patients are often agitated and confused and can show a range of behavioral features from depression and agitation to a florid delirium. Symptoms can begin quite abruptly or the onset may be more gradual, occurring over several weeks to even a few months. When behavioral changes dominate the symptomatology, particularly when the disorder affects young women, a diagnosis of primary psychiatric disease may occur before a correct diagnosis is made.
In addition to these features, patients may display other specific characteristics which can be highly suggestive, if not pathognomonic, of their underlying autoantibody. For example, patients with NMDAR-antibody encephalitis often exhibit a multifaceted psychiatric prodrome with features of both mood changes and psychosis, in addition to a complex movement disorder, dysautonomia, and coma. By contrast, patients with LGI1 antibodies exhibit a prodrome of remarkably frequent focal seizures with semiologies including thermal sensations, piloerection, and synchronous spasms of the arm and face, termed faciobrachial dystonic seizures (FBDS). The latter appear exclusive to patients with LGI1 antibodies. CASPR2 antibodies are associated with peripheral nerve hyperexcitability including Morvan syndrome, but some patients present with a pure encephalitis. CASPR2 antibodies may be associated with thymic tumors, especially in patients with peripheral nerve involvement.
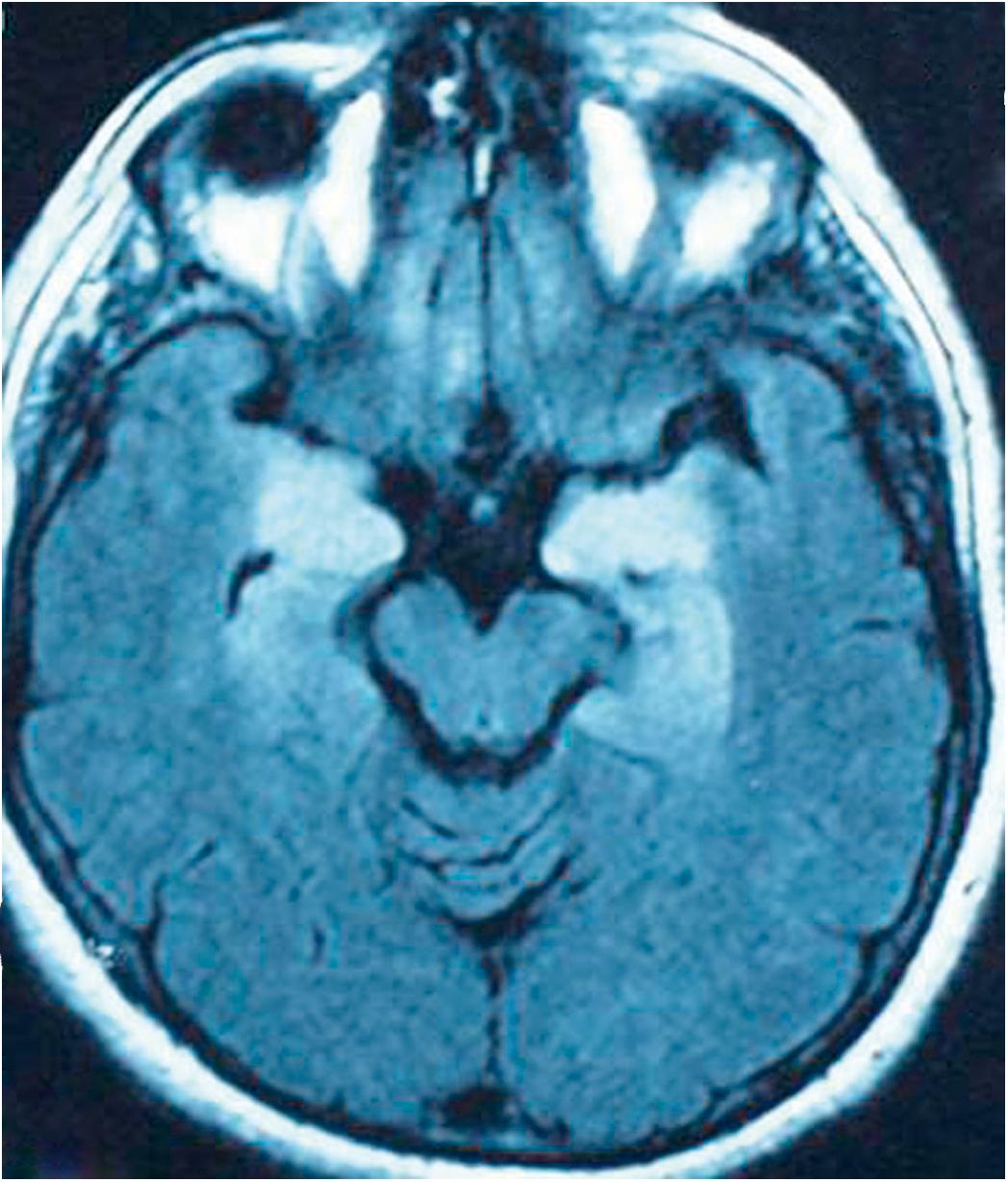
The CSF is often inflammatory, at least early in the course of the disease, although this finding can be variable between autoantibodies. The MRI may be subtle or normal although abnormalities, particularly medial temporal lobe hyperintensities on the T2-weighted or fluid-attenuated inversion recovery (FLAIR) sequences ( Fig. 27-1 ), are common. Electroencephalographic (EEG) findings include focal or generalized slowing and occasional epileptiform activity, particularly in the temporal areas. There are occasionally some more specific features: patients with LGI1 antibodies have especially frequent epileptiform discharges, often subclinical, and some of the more encephalopathic patients with NMDAR antibodies can have the EEG appearance termed “extreme delta brush.” Measurement of brain metabolism with PET or single-photon emission computerized tomography (SPECT) scanning demonstrates abnormalities in the medial temporal lobes. The areas may be either hypermetabolic due to seizure activity or inflammation or may be hypometabolic late in the course, related to neuronal degeneration. Very recently, strong HLA associations have been associated with LGI1 and CASPR2 antibody encephalopathies. Given their robust nature, particularly in the era of personalized medicine, these tests are likely to be part of a clinical work up of these patients.
The most important diagnostic test is measurement of autoantibodies. The commonest antibodies found in paraneoplastic limbic encephalitis are those which target Hu (SCLC), Ma2 (testicular cancer), CRMP5/CV2 (SCLC-thymoma), the NMDAR (ovarian teratoma), and the GABA B receptor (SCLC). Antibodies found in patients who frequently do not have cancer include antibodies against LGI1, CASPR2, and the GABA A receptor.
Typical limbic encephalopathy is characterized by the destruction of hippocampal neurons along with inflammatory infiltrates both in the perivascular spaces and in the brain parenchyma. In some patients, particularly those who die many years after the disorder begins, findings are consistent with sclerosis of the hippocampus, without inflammatory infiltrates, particularly in patients with Hodgkin disease. Whether inflammation was present at onset and disappeared over time is unclear. In fact, the literature has examples of a rapid evolution from limbic encephalitis to hippocampal sclerosis; this finding may have implications for a subset of patients with adult-onset medial temporal lobe epilepsy secondary to hippocampal sclerosis.
Overall, not accounting for nuances of the clinical presentation, two of the most important alternate diagnoses to consider are herpes simplex encephalitis and acute primary psychiatric presentations. Other diagnostic considerations include temporal lobe tumors, systemic lupus erythematosus, Hashimoto encephalopathy, human herpes virus type 6 (especially after bone marrow transplantation), and a variety of metabolic abnormalities causing delirium.
The other important diagnostic consideration is to differentiate paraneoplastic limbic encephalitis from nonparaneoplastic autoimmune limbic encephalitis. As these two disorders are often clinically indistinguishable, almost all patients require at least an initial search for an underlying neoplasm.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here