Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The incidence of childhood cancer has been steadily increasing over the last few decades, from approximately 13 per 100,000 in 1975 to over 17 per 100,000 in 2005. While pediatric malignancies account for only 1% of all cancers diagnosed each year, cancer is the leading cause of death by disease in children aged 1–19 years. In the United States alone, each year an estimated 15,780 children and adolescents are diagnosed with cancer, and more than 40,000 children require cancer treatment. Despite the improvement in the cure rate, approximately 12% of children diagnosed with cancer do not survive, and cancer remains responsible for more deaths (57%) than all other diseases combined in children.
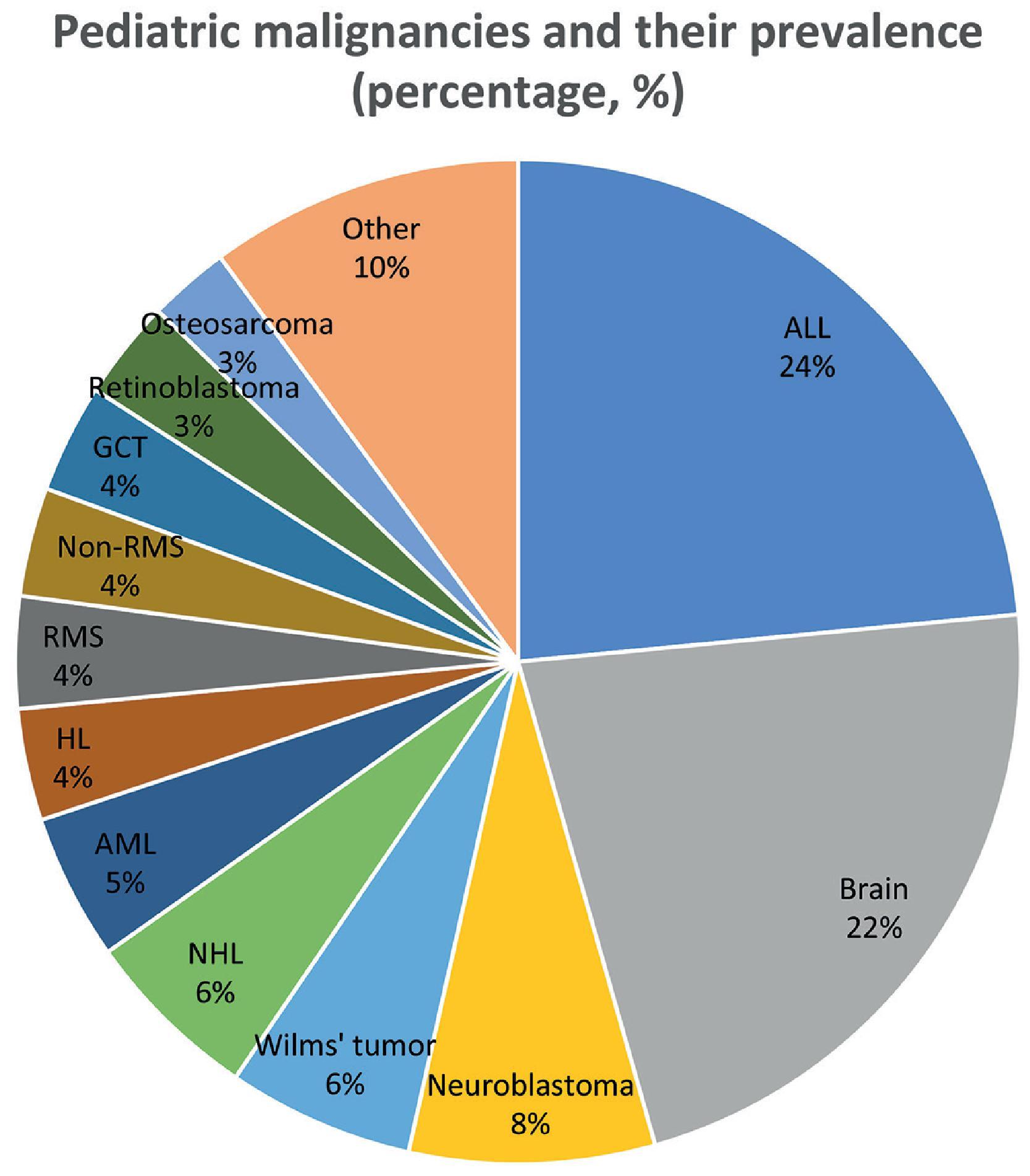
The incidence rate of cancer in children varies between races, with Caucasians followed by Hispanics having the highest incidence, while African Americans have the lowest incidence. Incidence rates also vary between high- and low-income countries. Countries with the lowest income have fewer medical resources, lack advanced diagnostic tools, and have limited access to cancer therapy. In addition, these countries have higher environmental exposures such as secondhand tobacco exposure, carcinogens in air pollution such as asbestos and silica dust, and unpurified water containing traces of carcinogens. The incidence of cancer in children also varies according to age and sex. Overall, leukemia is the most common cancer among children and adolescents, while neuroblastoma, Wilms tumor, and retinoblastoma predominate in infancy. Pediatric cancers, except for Wilms tumor, are slightly predominant in males. Fig. 45.1 shows rhe common pediatric malignancies and their incidence.
The majority of pediatric cancers have no known cause or risk factor, and only 10% can be linked to a familial or genetic factor. Specific prenatal and postnatal exposures have also been implicated in some childhood cancers. While a wide range of environmental agents has been thought to be oncogenic, thus far, only prior chemotherapy and high-dose radiation have been proven to be causal. Certain genetic and inherited conditions, such as Downs syndrome, Li Fraumeni syndrome, Beckwith-Wiedmann syndrome, neurofibromatosis, and cancer predisposition syndromes, have a higher risk of particular malignancies, requiring these patients to be screened for these malignancies periodically ( Fig. 45.1 ).
The survival rates of pediatric malignancies have improved significantly over the past 50 years, from less than 40% to as high as 80%. The mainstay of treatment for pediatric solid tumors (neural or nonneural) is chemotherapy for the overall reduction in tumor burden, along with a modality of local control. Local control is often achieved by surgical resection, radiation therapy, or a combination of both. The primary survival contributors have been early diagnosis and significant discoveries of new chemotherapeutic agents, which now constitute the standards of care for most of these malignancies.
Tables 45.1 and 45.2 summarize the classes of chemotherapy and radiotherapy for cancer treatment modalities, respectively.
| Chemotherapy Class | Drug | Mechanism of Action |
|---|---|---|
| Antimetabolites | ||
| Antifolates | Methotrexate | Inhibition of dihydrofolate reductase (DHFR) |
| Purine antagonists | Cytarabine, 5-fluorouracil, gemcitabine | Addition of faulty purine analogs between DNA base pairs |
| Pyrimidine antagonists | Fludarabine | Addition of faulty pyrimidine analogs between DNA base pairs |
| Purine analog | 6-Mercaptopurine | Inhibition of DNA polymerase leading to DNA breaks |
| Tubular interactive agents | ||
| Vinca alkaloids | Vincristine, vinblastine | Destruction of tubulin in microtubules leading to mitotic arrest |
| Alkylating agents | ||
| Oxazaphosphorines | Cyclophosphamide, ifosfamide | Intercalate DNA double strand |
| Nitrogen mustards | Busulfan, melphalan | Intercalate DNA double strand |
| Platinum complexes | Cisplatin, carboplatin | Intercalate DNA double strand |
| Topoisomerase inhibitors | ||
| Topoisomerase I inhibitors | Topotecan, irinotecan | Single-strand DNA breaks from inhibition of topoisomerase I |
| Topoisomerase II inhibitors | Etoposide | Double-strand DNA breaks from inhibition of topoisomerase II |
| Anthracyclines | Doxorubicin, daunorubicin | Formation of free radicals that lead to DNA breaks |
| Antibiotics | Bleomycin, actinomycin | |
| Enzymes | l-Asparaginase | Cleavage of amino acid l-asparagine |
| Tyrosine kinase inhibitors | Imatinib, dasatinib | Prevent activation and phosphorylation of tyrosine kinase |
| Photon Therapy | Proton Therapy |
|---|---|
| X-ray, a source of energy without mass | Heavy part of the atom |
| Higher entrance and exit dose | Relatively low entrance dose, no exit dose |
| Scattered spillage beyond the tissue/region of interest | Ability to tailor peak intensity in target tissue, and minimal spillage beyond tissue of interest |
| Higher dose and gradual dose gradient in tissue | Lower dose and steep dose gradient in tissue |
| Heterogeneous dose within the tumor | Homogeneous dose within the tumor |
| Increased risk of second malignancies and late effect | Very sensitive to tumor motion regression |
| Lower cost | Much higher cost |
The field of surgical oncology has also undergone significant advances over the last few decades, with a shift in focus to finding surgical procedures with maximal therapeutic impact while limiting late effects on quality of life, which has improved outcomes. Unfortunately, many children who survive cancer still suffer from long-term sequelae of cancer treatments, with conditions such as mental disabilities, organ dysfunction, and secondary cancers. Developing more innovative and less damaging therapies is therefore crucial for pediatric malignancies. Cancers that are metastatic at diagnosis, those that do not respond to standard treatment, or progress/relapse despite appropriate treatment have poor survival rates (<20%).
Acute lymphoblastic leukemia (ALL) is the most common cancer diagnosis in children. It accounts for 20% of all cancers diagnosed in children and young adults. An estimated 3000 new cases of childhood ALL are diagnosed each year in the United States. After a peak incidence of 90 cases per million per year at the age of 2–3 years, ALL incidence rates decrease steadily into adolescence. Initial complete remission rates are achieved in 95% of patients. Survival in childhood ALL is approaching 90% through the application of reliable prognostic factors permitting risk-stratification-based treatment protocols. Unfortunately, relapse occurs in approximately 20% of cases, with higher relapse rates in older patients and infants less than 1 year of age. The standard of care therapy for ALL is based on different phases and spans a total duration of 2–3 years of chemotherapeutic regimens. Traditionally, risk stratification is based on patient age, leukemic blast count at diagnosis, and high-risk genetic markers (e.g., BCR-ABL fusion or MLL rearrangement). Despite excellent outcomes overall, patients with relapsed ALL outnumber nearly all other childhood malignancies. With traditional intensive combination chemotherapy and allogeneic hematopoietic stem cell transplantation, 30%–40% of all children with relapsed ALL can be cured.
Acute myeloid leukemia (AML) is the second most common type of leukemia in children, accounting for 15% of cases. It has a bimodal pattern of incidence, with most patients either being diagnosed in the first 2 years of life or during teenage years. Unfortunately, survival is poorer than that for ALL, with approximately two-thirds of patients surviving for at least 5 years. AML is associated with chromosomal abnormalities, including translocations (e.g., PML-RARA t15;17), gain or loss of chromosomes (chromosome 16), and other abnormalities (FLT3, MLL). The disease is characterized by leukemic cells proliferating in the bone marrow, which then interferes with the production of normal blood cells, leading to infections, bleeding, and other symptoms and complications. Similar to ALL, treatment risk grouping is based on molecular findings and the response to induction treatment. The relapse rate is high, with approximately 30% of children relapsing in the first 5 years. Treatment depends on the subtype and usually has a shorter duration but higher intensity than that of ALL. Most patients with relapsed disease are considered for stem cell transplantation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here