Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
While cutaneous malignancies are the most common cancer of the head and neck region, the most common cancer arising from the mucosa is squamous cell carcinoma (HNSCC).
5-year survival outcomes for head and neck cancer patients have improved across all ages and all sites, except the larynx, increasing from 55% to 66% from 1992 to 2006.
Once diagnosed, head and neck cancer patients are referred for discussion at a multidisciplinary meeting (MDM).
The tumor diagnosis, staging, strengths and limitations of treatment options are discussed in the context of the patient’s comorbidities, functional status, psychosocial background, and the patient’s wishes, with the goal being to find the optimal management plan for each patient
Treatment principles are based on tumor type and anatomic site as described below.
![]()
![]() Access video and video lecture content for this chapter online at Elsevier eBooks+
Access video and video lecture content for this chapter online at Elsevier eBooks+
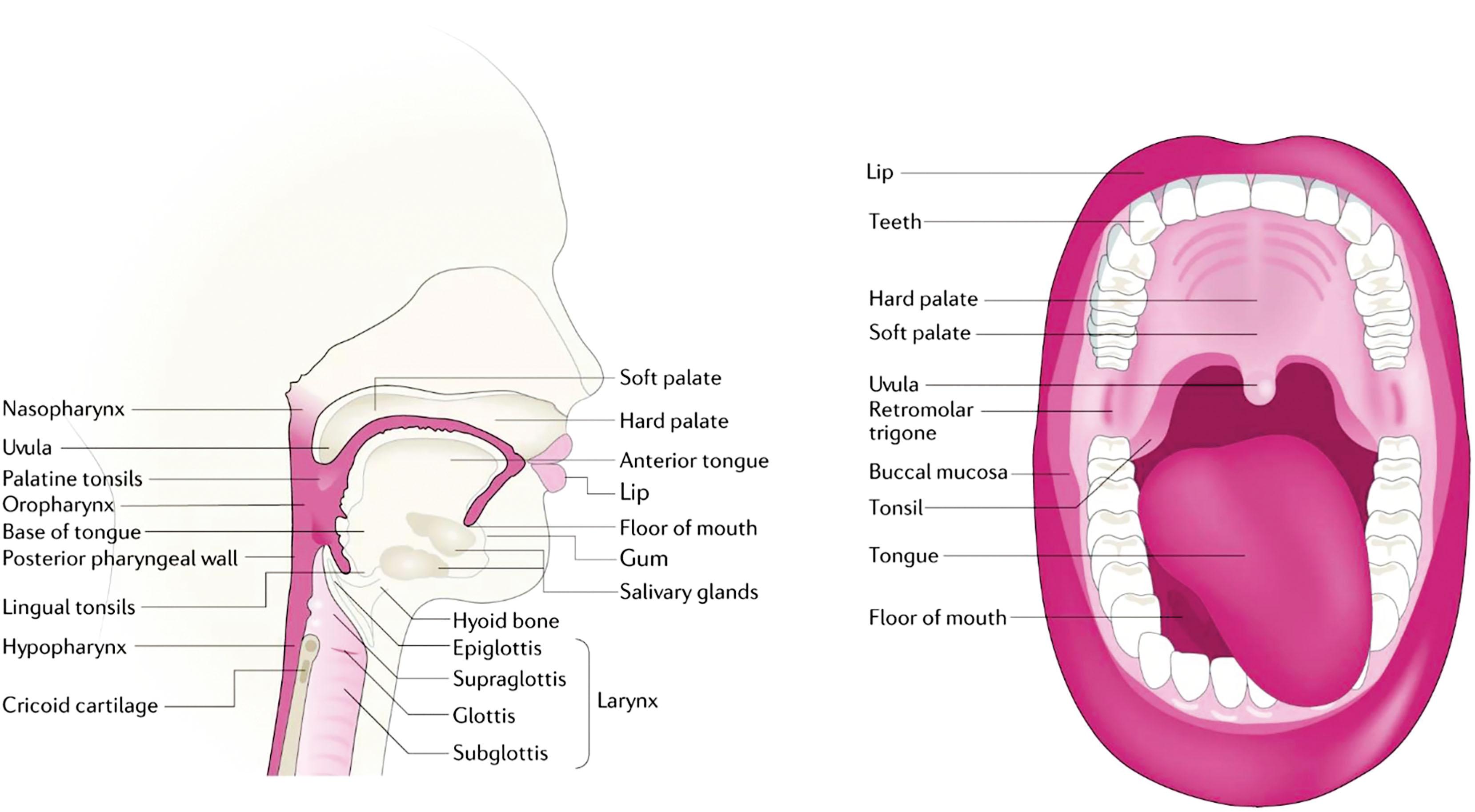
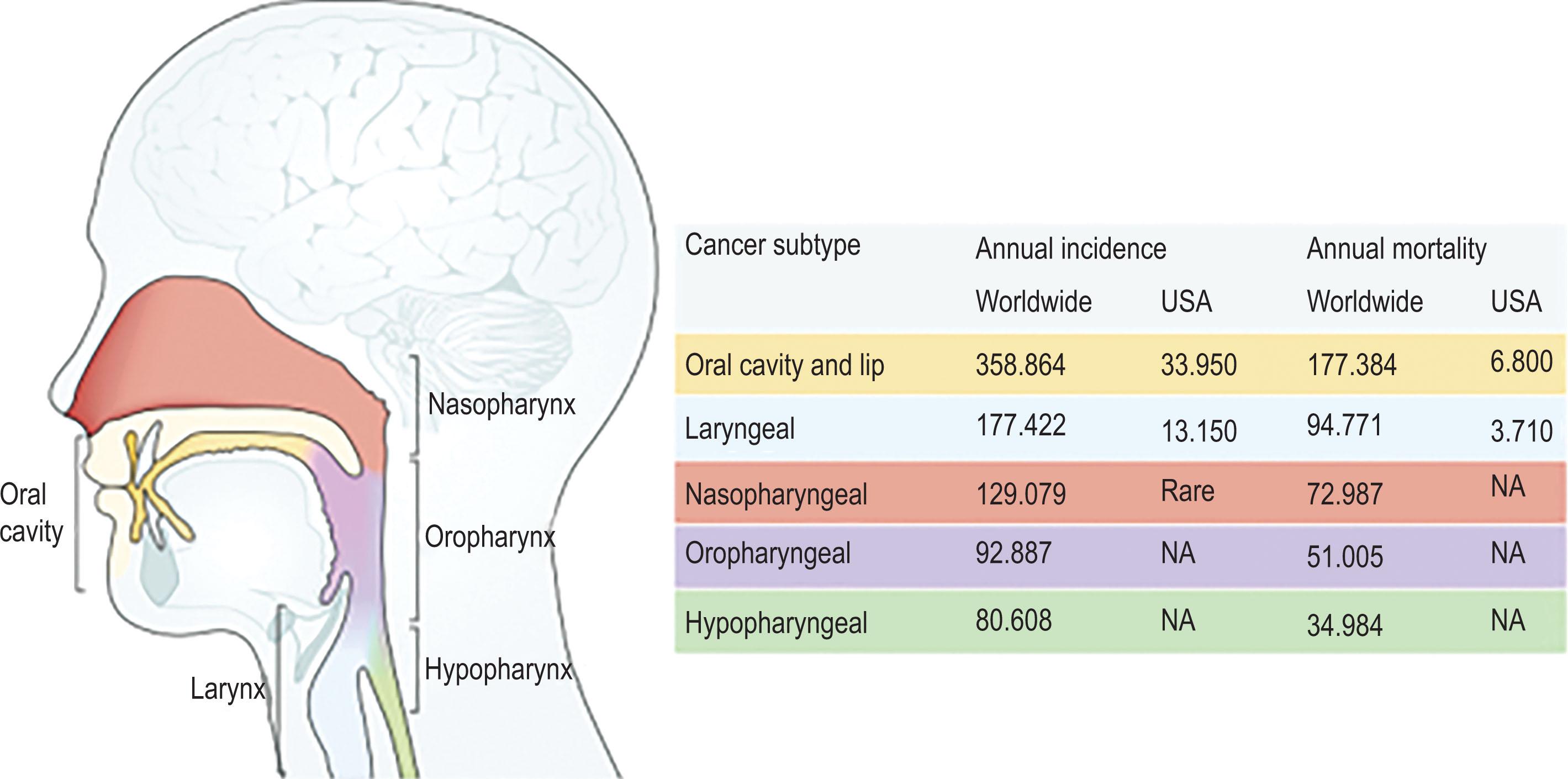
By convention the term head and neck cancer relates to malignant tumors arising from the mucosal epithelium of the upper aerodigestive tract, extending from the lip vermilion to the larynx including the oral cavity, pharynx and the paranasal sinuses ( Fig. 8.1 ). While cutaneous malignancies are by far the most common cancer of the head and neck region overall, the most common cancer arising from the mucosa is squamous cell carcinoma (HNSCC). Less commonly, adenocarcinoma, mucosal melanomas, salivary gland tumors, lymphomas and sarcomas are encountered. Sub-types of mucosal SCC include human papilloma virus (HPV)-negative, HPV-positive, and verrucous SCC. These anatomical regions perform a diverse array of vital functions including breathing, airway protection, and swallowing, and are integral to many aspects associated with quality of life such as speech, smell, taste, and appearance, making head and neck cancer and its treatment potentially both functionally and aesthetically morbid. That survivors of head and neck cancer have the second highest rate of suicide attest to this.
Mucosal SCC arising in the head and neck region is the eighth most common cancer in developed countries with its overall prevalence expected to increase by 30% by 2030 owing to the rising incidence of HPV-positive oropharyngeal disease. Males are more than twice as commonly affected than females (2–4 : 1). While HPV-negative SCC is more commonly diagnosed in older (>55 years) people of lower socioeconomic background, HPV-positive disease typically presents earlier (<50 years) in a higher socioeconomic demographic ( Fig. 8.2 ). Major risk factors include environmental carcinogens tobacco and alcohol (smokers who are also drinkers have 30 times increased risk of developing mucosal SCC) while ultraviolet (UV) exposure strongly predisposes to lip SCC. In South and East Asia, mucosal SCC related to Areca (‘Betel’) nut chewing is endemic. Oncogenic viruses, notably HPV infection (type 16 more so than type 18 and others) of the lingual and pharyngeal tonsils, are associated with two-thirds of oropharyngeal SCC while Epstein–Barr virus (EBV) infection is associated with nasopharyngeal carcinoma. Those with rare genetic syndromes such as Fanconi’s anemia and dyskeratosis congenita, are also at high risk of developing mucosal SCC in addition to cancers elsewhere. Minor risk factors include poor oral hygiene, poor nutrition, and irritation from dentures. With the aerodigestive tract being a single continuous entity, those who have been diagnosed with one mucosal SCC are at risk of synchronous and metachronous mucosal, lung, and esophageal cancers, which are the second leading cause of death in head and neck cancer patients.
Survival outcomes for head and neck cancer patients has improved marginally over recent decades, with 5-year survival across all ages and all sites, except the larynx, increasing from 55% (between 1992 and1996) to 66% (between 2002 and 2006) according to the SEERs registry. Tumor stage and HPV status are the most important prognostic factors in head and neck cancer.
Mucosal SCC likely arises from adult stem or progenitor cells in the mucosal epithelium lining the upper aerodigestive tract. Invasive disease most commonly arises de novo without any antecedent lesion although a step-wise progression from normal mucosa through hyperplasia, dysplasia, carcinoma in situ and invasive carcinoma may be seen with SCC arising from leukoplakia and erythroplakia. HPV-negative SCC is strongly associated with tobacco, which contains dozens of carcinogens that form reactive metabolites predisposing to DNA injury (i.e., mutations, deletions, amplifications) in critical genes involved in tumor suppression (e.g., TP53 , CDKN2A ) or pathway signalling (e.g., PI3K-AKT-mTOR). The most recognized carcinogens in tobacco are polycyclic aromatic hydrocarbons and nitrosamines. Acetaldehyde is the best known carcinogen in alcohol and it may have a synergistic effect in smokers by acting as a solvent for tobacco carcinogens. The term “field cancerization” captures the concept of widespread damage to the aerodigestive tract caused by inhaled carcinogens and explains the relatively high incidence of synchronous and metachronous primary cancers seen in mucosal SCC. Given that mucosal SCC is a heterogenous tumor it is likely that independent oncogenic processes will give rise to multiple distinct tumor populations. On the other hand, HPV-positive SCC is a unique tumor entity accounting for more than two-thirds of oropharyngeal SCC, and a minority at other head and neck sites. Although there are over 1000 HPV subtypes, type 16 is the major oncogenic virus associated with the development of SCC. It infects the squamous epithelium of the lingual and palatine crypts where it is incorporated into cellular DNA leading to the transcription of two oncoproteins, E6 and E7, which in turn inactivate p53 and RB1 proteins predisposing to the unregulated proliferation of mutant, and potentially cancerous cells. It follows that in contrast to HPV-negative SCC, the TP53 gene (encoding for p53) is normal in HPV-positive SCC. The average latency period from HPV infection to the development of HPV-positive cancer is 10–30 years. Widespread vaccination with FDA approved vaccines against HPV types 16 and 18 could reduce the incidence of the disease in the future but with the prolonged latency period and slow uptake of vaccination this is decades away. HPV-positive SCC has an increasing prevalence (twenty-first century epidemic), but relatively better prognosis as it is more chemo- and radiosensitive. There is hope that a better understanding of tumor biology might be found through improved understanding of tumor epi/genetics, tumor microenvironment, mechanisms of immune evasion and metastasis, and enable tailored treatment regimens with improved oncological outcomes and reduced morbidity.
Advanced age is not associated with increased surgical complications but, because the elderly population generally has more comorbidities and less physiological reserve, they are at higher risk of perioperative complications, namely cardiovascular and pulmonary events. Presenting symptoms generally reflect the site and depth of the involved tissues. It follows then that lip and oral cavity SCC present earlier with painful or bleeding non-healing ulcers. In other sites of the upper aerodigestive tract small volume disease is commonly occult, and presentation delayed until the disease is locoregionally advanced causing symptoms such as hemoptysis, dysphagia, odynophagia, ear pain (oropharynx), hoarseness (hypopharynx), or nasal obstruction and motor/sensory changes relating to cranial nerve involvement (nasopharynx). A painless neck lump may be the only presenting complaint with HPV-positive oropharyngeal and EBV-positive nasopharyngeal SCC ( Fig. 8.3 ). The latter should be suspected in any Southeast Asian patient presenting with a neck lump. A history of rapidly progressive symptoms suggests a more aggressive disease process which should be particularly concerning in the immunocompromised patient. Previous head and neck surgeries and radiotherapy complicate management and salvage surgeries are associated with increased surgical morbidity. The history should also screen for risk factors, aim to identify comorbidities, establish the patient’s nutritional and functional status as well as social circumstances, all of which will guide treatment options and planning besides having prognostic implications.

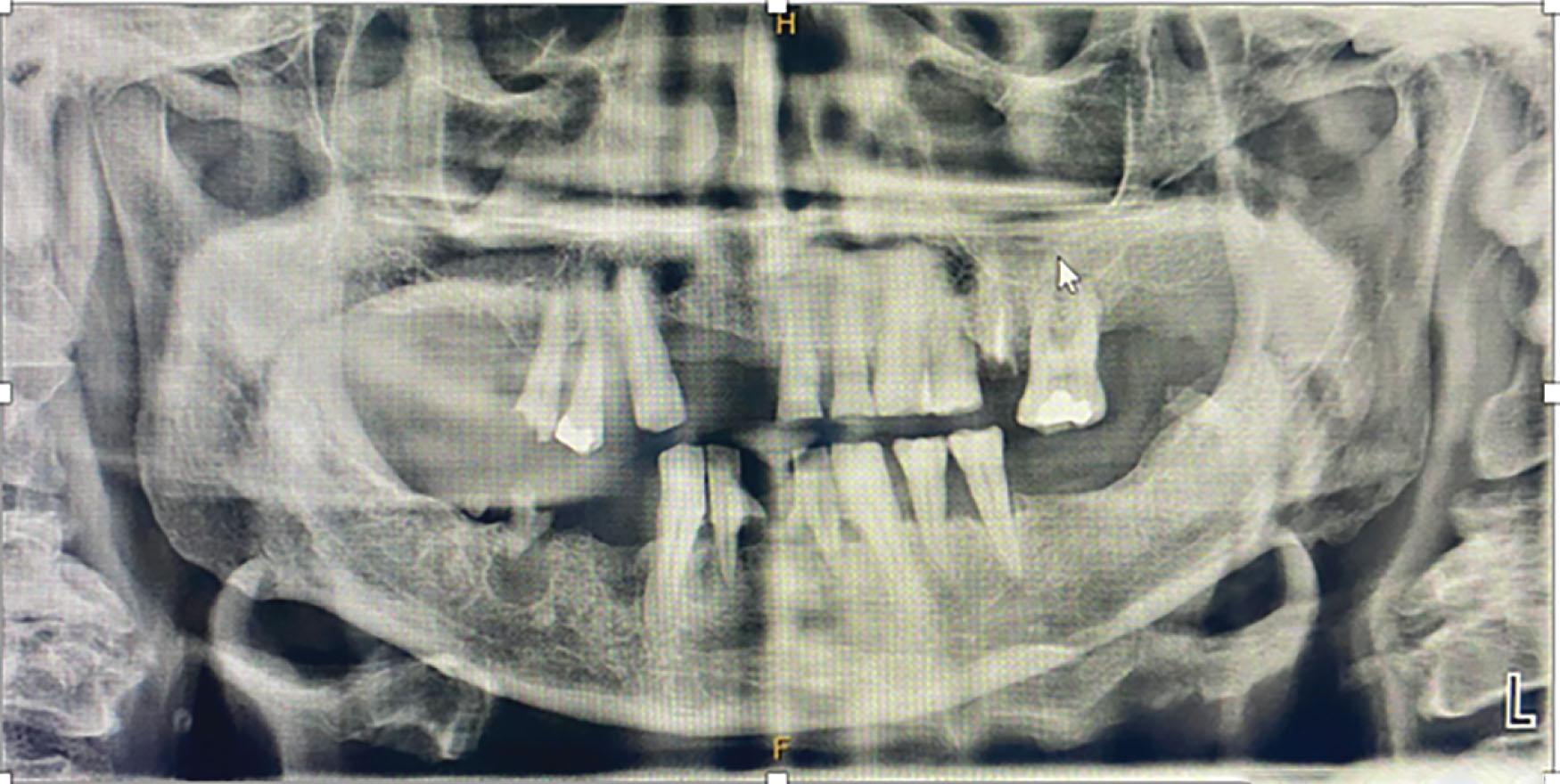
After the skin, the oral cavity is the most easily accessible area of the head and neck region to examine. With a headlight and tongue depressor each of the anatomical subsites of the oral cavity should be carefully inspected and any irregularity/tumor examined with particular attention paid to the appearance, site, size, depth and functional impairment. Palpation can reveal more about the extent of the tumor than inspection and is essential in the assessment of oral cavity SCC as depth of invasion (DOI) affects T classification. While inside the mouth dental assessment should be performed routinely, as tooth decay and periodontal disease are common in this patient demographic. Preoperative orthopantomogram (OPG) is complementary and should help guide decisions about prophylactic removal of teeth at the time of surgical ablation to avoid subsequent dental disease complicating treatment (e.g., osteoradionecrosis) ( Fig. 8.4 ). Systematic examination of the cranial nerves, parotid gland, and cervical lymph nodes follows. The latter is performed standing, and from behind the patient with their neck slightly flexed to relax the strap muscles, the purpose being to identify the site, size, number of any malignant cervical lymph nodes, and whether any underlying structures, such as accessory nerve, are involved. Compared with imaging studies clinical examination of the cervical lymph nodes is in general inferior but remains important to surgical planning. For suspect lymph nodes fine-needle aspiration cytology (FNAC) is the investigation of choice. It has been shown to be reliable, particularly if performed under ultrasound guidance, and accurate with a high sensitivity (89.6%) and specificity (96.5%). The examination of the head and neck region is not complete without fiberoptic endoscopy to inspect the nasal cavity, pharynx, base of tongue and larynx for synchronous tumors. Specific manoeuvres to improve visualisation include asking the patient to exhale against a closed mouth causing the cheeks to blow outwards (piriform fossa) and say ‘eee’ (vocal cord symmetry and mobility). Finally, the cardiovascular, respiratory and gastrointestinal systems are examined to screen patients for distant metastases and medical issues which might affect their fitness for surgery. Head and neck cancer patients are often cachectic owing to a combination of disease-related impairments of mastication and swallowing as well as poor lifestyle choices (i.e., smoking, alcohol, and an inadequate diet). Malnutrition compromises wound healing and predisposes to infection so formal nutritional assessment should be considered along with preoperative supplementation if it is identified. Patients who might be expected to have a delayed return to swallowing post-treatment, such as following laryngectomy, may require a percutaneous enteral gastrostomy (PEG). In patients at risk of upper airway obstruction or aspiration, particularly if they have poor pulmonary reserve preoperatively, a tracheostomy should be planned.
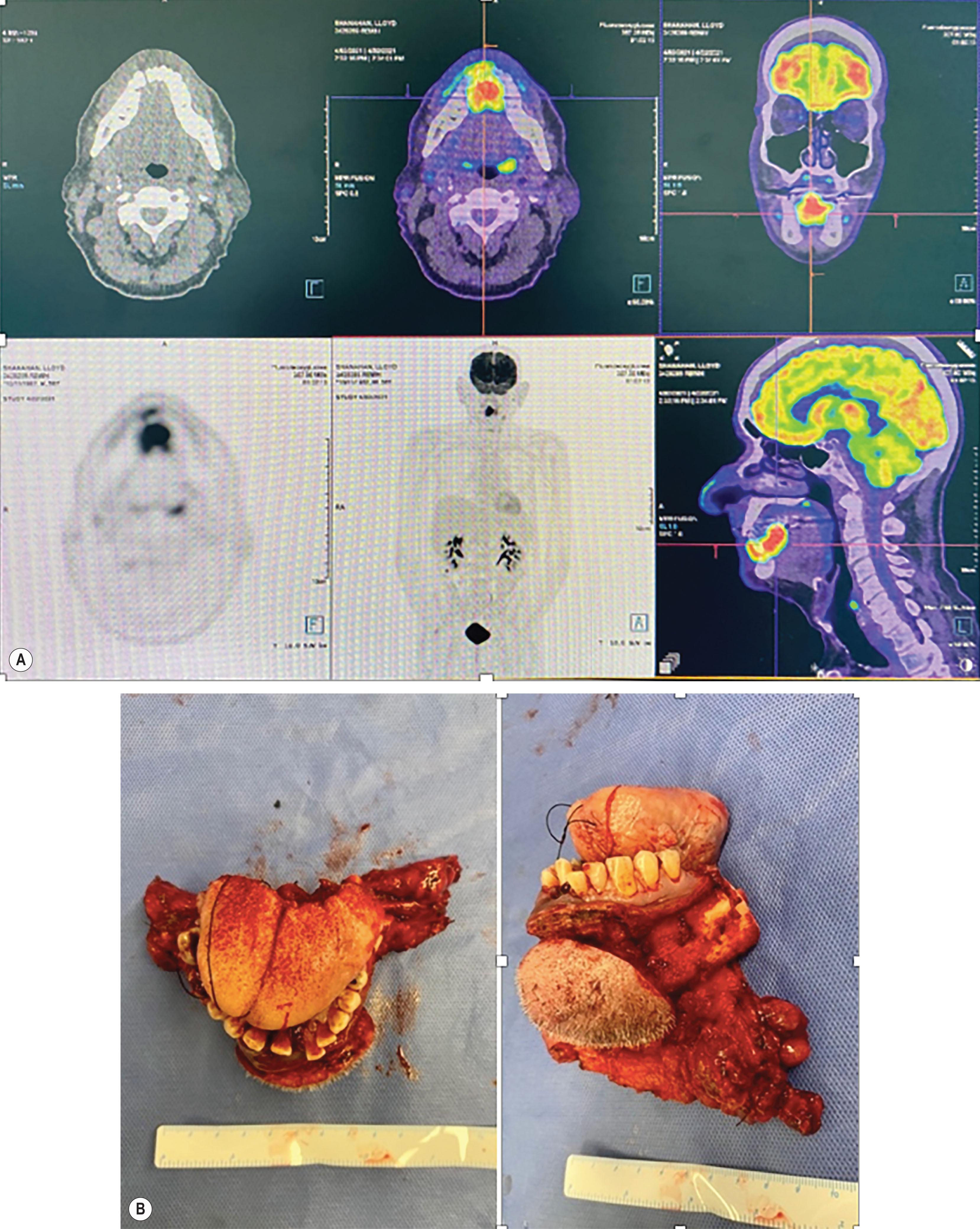
Imaging is central to the staging and planning of treatment of head and neck cancer. Physical examination combined with contrast-enhanced computed tomography (CT) of the head, neck, and chest is sufficient in most instances for diagnostic and staging purposes. The superior soft tissue resolution available with magnetic resonance imaging (MRI) is desirable for further delineating disease extent in the parotid, oropharynx, larynx, and base of skull, as well as identifying perineural invasion and dural involvement. However, it is generally a less available resource, and with long scanning times making it susceptible to motion artefact, may be less effective in head and neck cancer patients who have breathing and swallowing issues when lying supine. In contrast, despite concerns about radiation exposure and its susceptibility to metallic artefact (e.g., dental fillings and metal implants), CT is fast, easily obtained, and provides superior evidence of bone (and cartilage) invasion with adequate soft-tissue definition (with 2 mm slices) in most circumstances. It is also a reliable and accurate tool for diagnosing cervical lymph node metastases, based on size (>10 mm in minimum axial dimension) and appearance (central necrosis) criteria, as well as the presence of extracapsular spread. Furthermore, when integrated with the physiological data obtained with positron-emitting tomography (PET), PET/CT provides a superior tool than either CT or MRI to identify cervical or distant metastases, with a meta-analysis showing 91% sensitivity and 87% specificity for synchronous primaries and unknown primaries ( Fig. 8.5 ). False-negatives with PET/CT can occur with superficial mucosal lesions (making panendoscopy critical), occult cervical metastases <5 mm (therefore it does not replace neck dissection when indicated), and unknown primaries near the pharyngeal lymphoid tissues with high background physiologic activity. As already mentioned, OPG completes the radiological work-up.
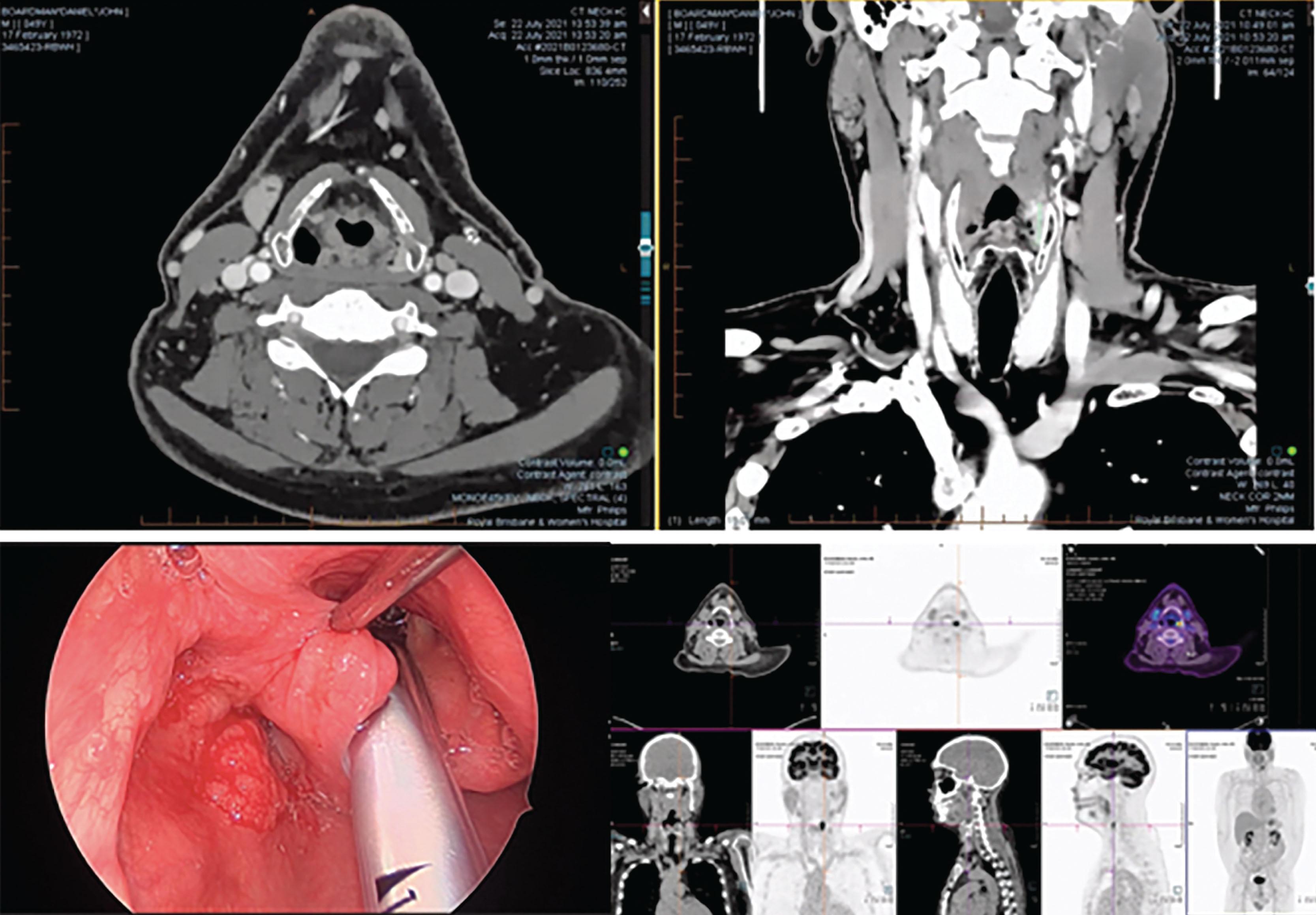
Examination under anesthesia (EUA), using a rigid endoscope, may be necessary in the workup of a head and neck cancer patient as it provides the surgeon with the opportunity to carefully assess tumors not detectable on physical examination and make a surgical plan whilst affording the opportunity to obtain a tissue biopsy for histologic diagnosis (see Fig. 8.5 ). Routine panendoscopy (laryngoscopy, bronchoscopy, esophagoscopy, or “triple endoscopy”) used to be performed for all head and neck cancer to exclude synchronous tumors, however this remains controversial. Those opposed to it argue it is resource-intensive and unnecessary with advanced imaging techniques guided by patient symptoms being equally effective. Instead, they suggest panendoscopy only in high-risk patients (i.e., heavy smoker or drinker) with tumors strongly associated with synchronous tumors (i.e., oropharynx), or suspicious lesions identified on imaging. For unknown primary tumors, panendoscopy remains an essential component of the workup as sites at high risk of occult disease (i.e., nasopharynx, tonsil, tongue base, piriform fossa) need to be closely inspected for subtle lesions, and blind biopsies performed. More than 90% of tumors of unknown primary are HPV- or EBV-positive oropharyngeal or nasopharyngeal tumors.
Histological confirmation of the diagnosis is essential prior to the commencement of any cancer treatment. A representative sample(s) of tumor must be obtained to enable the pathologist to provide not only a diagnosis but also any additional information needed to accurately stage the tumor, including depth of invasion (DOI), perineural invasion, lymphovascular invasion and p16 status. Practical tips for achieving this include using a 3–4 mm punch biopsy and avoiding the center of the tumor which may be necrotic, and the peripheries which may show dysplasia only. All imaging should be acquired prior to biopsy as the associated edema may inaccurately upstage the tumor.
Histologically , HPV-negative SCC tends to be moderately-to-well differentiated resembling the normal stratified epithelium of the aerodigestive tract with mature cells with occasional keratinization irregularities (“keratin pearls”) while HPV-positive SCC tend to be poorly differentiated. H&E is usually adequate, however IHC using pancytokeratin antibodies (e.g., cytokeratin 5, 6, p63) may be required. Testing of HPV status is indicated for all oropharyngeal tumors, or those with an unknown primary. Most commonly this is done with IHC stain for the cell cycle protein p16INK4A, other techniques include the detection of E6 and E7 mRNA and HPV DNA.
Head and neck cancers are commonly staged using the tumor, node, metastases (TNM) staging system, developed in 2002 by the American Joint Committee on Cancer (AJCC) and the Union Internationale Contre le Cancer (UICC), which serves to standardize the assessment of tumor burden, prognostication, and management. Clinical information gathered from the physical examination, radiology, pathology, and intraoperative findings is used to establish a patient’s TNM classification which then translates into early , Stage I–II, or advanced , Stage III–IV, disease ( Table 8.1 ). Almost universally, nodal or distant metastases are associated with advanced disease with the exception of nasopharyngeal and thyroid tumors and HPV-positive oropharyngeal SCC, which have their relatively better prognoses reflected by downstaging under AJCC 8th edition. A notable shortcoming of the TNM staging system is that it does not distinguish between a locally advanced primary tumor without metastases and a small primary tumor with metastases, both of which may have very different prognoses. Finally, pathological staging, unlike clinical staging, is only achievable after surgical ablation.
| TNM classification | Staging | 5-year overall survival |
|---|---|---|
| T1–2, N0, M0 | Stage I–II | 84% |
| T3, N0, M0 or T1–3, N1, M0 | Stage III | 65% |
| T4, N0, M0 or T1–4 ± N2-3 ± M1 | Stage IV | 39% |
T– relates to the site, size, depth of the primary tumor, and involvement of surrounding structures with the definition for T1–4 varying according to the anatomical subsite of the tumor; N– relates to the site, size, number, and extent of cervical node involvement; and M– relates to the presence or otherwise of distant metastases; Tx indicates the tumor cannot be assessed; T0 indicates no known primary tumor; Tis refers to in situ carcinoma.
Key updates to the head and neck section in the 8th edition AJCC Staging Manual included the addition of DOI to the T status of oral cavity SCC, a separate section for HPV-positive oropharyngeal SCC to better reflect its improved prognosis, changes to the T and N status of nasopharyngeal SCC, and the addition of extranodal extension to the N status.
Preventative measures are currently key to reducing the incidence of mucosal SCC. This includes reduced smoking and consumption of alcohol and Areca nut, improved oral hygiene, and regular dental review. Vaccination against HPV infection is likely to significantly reduce the incidence of mucosal SCC but with the focus of current vaccination programs on the adolescent population in the US, herd immunity remains a generation away. No screening (secondary prevention) measures have yet been shown to improve diagnosis or survival.
Once diagnosed, head and neck cancer patients are discussed at a multidisciplinary meeting (MDM) consisting of head and neck and reconstructive surgeons, radiation oncologists, medical oncologists, dentists, speech pathologists, nutritionists, and specialist clinical nurses. The tumor diagnosis, staging, strengths, and limitations of treatment options are weighed up in the context of the patient’s comorbidities, functional status, psychosocial background, and the patient’s wishes, with the goal being to find the optimal management plan for each patient ( Table 8.2 ).
| Tumor factors | Patient factors | Treatment options |
|---|---|---|
|
|
|
In general, localized small volume or stage I–II disease is amenable to single modality treatment. Both surgery and radiotherapy provide similar oncological outcomes (70–90% 5-year overall survival), although no randomized data have compared the two. Surgery, however, has several practical advantages: it involves a single treatment, relatively quick recovery, and depending on the site of the tumor may be associated with low morbidity and functional impairment. Additionally, it allows for pathological staging and margin assessment. With advancements in less invasive surgical techniques, such as transoral robotic surgery (TORS) and transoral laser microsurgery, surgery may have an expanding role in the treatment of pharyngeal and laryngeal tumors previously considered mostly the domain of non-surgical modalities, as open surgery was associated with unacceptable morbidity (e.g., non-union and osteoradionecrosis with mandibulotomy). This is an evolving area and careful patient and tumor selection with closer examination of the primary tumor under anesthesia along with formal assessment of its functional impact using nasopharyngoscopy and barium swallow studies is necessary. Radiation also can be reasonably well tolerated in the short term but the prolonged duration of treatment (6–8 weeks), and in particular long-term side effects that are difficult to treat, can make it less desirable. Patients who are not fit for surgery may be candidates for radiation.
Most head and neck cancers, however, present late (>60%) with locally advanced disease involving adjacent structures and/or nodal or distant metastases. In advanced or stage III–IV disease combined modality treatment is indicated as locoregional failure and distant metastases are high. Various treatment regimens are described – surgery with adjuvant radiotherapy with or with chemotherapy, primary chemoradiation, induction chemotherapy followed by surgery and radiotherapy – but these are subject to change as the availability and understanding of new technologies (e.g., TORS, IMRT [intensity-modulated radiation therapy]), medical therapy (e.g., immune checkpoint inhibitors) and cancer biology evolves. Current management recommendations generally reflect treatment efficacy and the relative morbidity of the different treatment modalities at each tumor site. For lip and oral cavity SCC surgical access and ablation are well tolerated, in large part due to the success of reconstructive techniques (see The oral cavity section, below). The same cannot be said for pharyngeal and laryngeal disease where access is difficult and associated with significant morbidity (i.e., mandibulotomies and lingual release) and the complexity of the functional anatomy of the upper aerodigestive tract makes it near impossible to meaningfully reconstruct. “Organ preserving” chemoradiation therefore is recommended. The modality used to treat the primary is generally also used to manage the neck, as discussed below.
When surgery is used, pathological staging offers the possibility of up- or down-staging a patient’s disease burden allowing treatment to be tailored. Adjuvant treatment is necessary to improve locoregional control in those with high(*)/intermediate risk clinicopathologic features, namely:
*Incomplete, or close (<5 mm) pathological margins
T3–4 primary tumor stage
Perineural invasion
Lymphovascular invasion
*Extranodal extension (ENE)
Two or more involved lymph nodes (>N2).
For those with high-risk (*) features, postoperative chemoradiation significantly improves locoregional control and disease-free survival. For those with intermediate risk features, retrospective studies support the role of postoperative radiotherapy alone to improve disease-specific survival. Adjuvant treatments are, however, not without significant morbidity and careful patient selection is necessary to avoid non-compliance and treatment failure. For instance, mucositis is nearly universal following adjuvant radiation and chemotherapy, and in a number of people will be severe enough to require nasogastric or gastrostomy feeding or cause failure to complete treatment. Most studies suggest long-term grade 3 and 4 toxicities (e.g., soft-tissue ulceration/necrosis/fibrosis, dysphagia, fistula/osteoradionecrosis) were similar between chemoradiation and radiotherapy, with an incidence of 17–38%. It follows too that while pathological staging with surgery may be intuitively attractive, unnecessarily exposing a patient to triple modality treatment may be negligent.
Regular post-treatment follow-up is essential to identify treatment failure and recurrent and metachronous tumors. More rigorous review is required in the initial 2-4 years post-treatment to capture the 80–90% of recurrences, but follow-up should be lifelong. Complications from treatment can also worsen over time and the patient’s resolve to avoid risk factors such as smoking may require reinforcement. Typically, a post-treatment CT or MRI is performed at 6 weeks to evaluate the outcome of treatment and provide baseline imaging. Routine ongoing follow-up scans is at the clinician’s discretion. Combined multidisciplinary clinics with established survivorship programs specific to head and neck cancer are an important for coordination of care.
Anatomically, the boundaries of the oral cavity extend anterior to posterior from the lip vermilion to the hard–soft palate junction above, the line of circumvallate papillae below, and the anterior tonsillar pillars and glossotonsillar folds laterally. For prognostication purposes the oral cavity is further subdivided into seven subsites under AJCC staging – lip, floor of mouth (FOM), oral tongue, buccal space, hard palate, gingiva, and retromolar trigone (see Fig. 8.1 ). Critical functions of these oral cavity structures include oral continence, speech, mastication, deglutination, and oral hygiene.
The most common cancer of the oral cavity is SCC (>90%), less commonly salivary gland tumors and sarcoma are encountered. The lower lip followed by the lateral oral tongue are the most common subsites involved, while the lip (88%) and FOM (54%) are associated with the best and worst overall prognoses, respectively. Uniquely, buccal SCC is the most common subsite of oral cavity SCC in Southeast Asia owing to widespread Areca nut chewing but rare in Western populations. Although oral cavity SCC is relatively more likely to present early than other head and neck cancers, presentation is still more commonly with locally invasive T3–4 disease (involving buccinator, parotid duct, VII, cheek skin, mandibular ramus, pterygoids, maxillary alveolus) or lymphatic metastasis (40%).
Staging is the most important determinant of prognosis, with overall 5-year survival dependent on the presence of small volume, localized disease (84%), lymph node metastasis (65%), and distant metastasis (39%). (Refer to T-staging of oral cavity SCC per AJCC Staging Manual, 8th edition).
Surgery is the preferred primary treatment modality for tumors of the lip and oral cavity as it provides comparable oncological outcomes with the least morbidity compared to the alternatives ( Figs 8.6 & 8.7 and Algorithm 8.1 ). For early stage (I–II) disease, primary radiotherapy may provide equivalent oncological outcomes but is generally reserved for those unfit for surgery due to the risk of early and late toxicities (e.g., mucositis, xerostoma radionecrosis). More commonly, radiotherapy is used adjunctly in instances where either the primary tumor (T3–4, perineural invasion, lymphovascular invasion) or neck disease (>N1) is considered at risk of locoregional failure. For those at particularly high risk of locoregional failure (i.e., incomplete/close [<5 mm] resection margins or ENE) adjuvant chemoradiation is recommended, provided the patient is fit enough to tolerate the increased toxicity of combined therapy.


Unlike the oropharynx, hypopharynx, and larynx, “organ preserving” treatment for oral cavity SCC with primary chemoradiation has been shown to be inferior in terms of overall survival and morbidity compared to surgery. Whether novel treatment regimens using neoadjuvant chemotherapy, or immunotherapy, prior to surgical resection can be used to reduce morbidity without compromising oncological outcomes are currently under investigation.
While historically debated, today elective neck dissection for the clinically N0 (cN0) oral cavity SCC is supported by level 1 evidence, demonstrating improved pathological staging of disease and a 12.5% improvement in overall survival compared to observation at 3 years follow-up. Subgroup analysis showed that this benefit was restricted to primary tumors with DOI >3 mm. T1 tumors may therefore be alternatively kept under close observation, which puts the emphasis on the quality of preoperative assessment and in particular the clinical examination (to distinguish between exophytic, ulcerative, infiltrative lesions) and baseline radiology of the cervical nodal field. American Society of Clinical Oncology (ASCO) guidelines suggest that an adequate elective neck dissection should include ipsilateral levels I–III, including at least 18 lymph nodes, and should be bilateral if the lesion is midline or a T3/4 oral tongue or FOM SCC. The perifacial lymph nodes should be carefully included in the 1b dissection as their involvement is estimated to be between 7% and 35% in oral cavity primaries. Notably, D’Cruz et al . documented 6.5% adverse events complicating elective neck dissection. Whether SLNB can offer a less morbid alternative in cN0 disease awaits the results of randomized control trials.
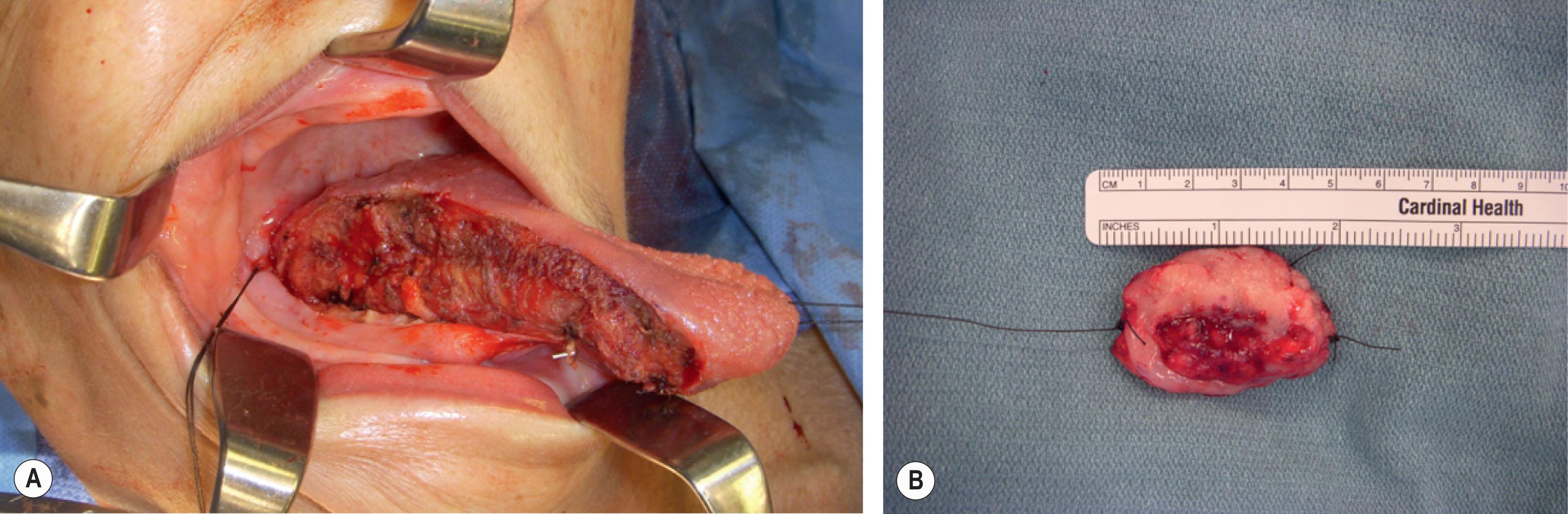
Technically, resection of oral cancers can be challenging. Because the resection is performed with restricted vision through limited access, in three planes and in an anatomically dense and complex region, there can be a delicate balance between acquiring inadequate margins and causing additional morbidity through unnecessarily wide surgical margins. Practically a 1 cm clinical margin is planned with the aim being to avoid a close (<5 mm) pathological margin. A partial glossectomy is illustrative. There are limited planes within the substance of the muscular tongue to use as anatomical guides, with the exception of the midline raphe which facilitates a compartmented hemiglossectomy resection. As a result, the resection technique involves marking a 1 cm margin around the tumor with loupe magnification and optimal lighting, a fine-tip diathermy is then used on the outer side of a palpating fingertip which always remains in contact with the margins of the cancer ( Fig. 8.8 ). Most oral cavity cancers can be accessed transorally. More invasive incisions such as lower and upper (Weber–Ferguson) lip-splitting incisions or degloving visor or facial maneuvers, which are associated with increasing morbidity, should be carefully considered, and adequately justified.
The FOM, gingival, and retromolar trigone SCCs are uncommon but SCCs of these subsites are aggressive. Uniquely in these locations the mucosa is thin and tightly adherent to the underlying periosteum which provides a limited barrier against bone invasion and T4 (stage IV) disease. From an oncologic perspective the periosteum is considered a barrier to invasion, but in the elderly and edentulous atrophic mandible this physiological barrier is impaired. Careful preoperative clinical assessment and imaging determines the extent of bony involvement and the resection required. Thin slice/high resolution CT can identify cortical erosion of the mandible with a sensitivity and specificity of 97–100% and 88%, respectively. In equivocal cases a complementary SPECT scan may be used to exclude bone involvement as it has a specificity of 100%. In general, SCC that is close to, but does not abut bone, may be removed with a 1–2 cm radial margin using the periosteum alone as the deep margin. For SCCs of the mandible that abut but do not invade the bone, or only superficially invade bone that is thick enough to permit a “scalloped” cortical resection leaving an intact mandible with a minimum height of 1 cm for stability, a marginal resection is permissible. This is contraindicated in a previously irradiated mandible which is prone to pathological fracture and osteoradionecrosis. Otherwise, a segmental resection is indicated. Planning for the resection should consider the potential local spread of disease into the adjacent masticator space from the retromolar trigone (to involve the pterygoid muscles, mandibular nerve [V3], soft palate musculature) or into the sublingual space from the FOM (to invade genioglossus, geniohyoid) ( Fig. 8.9 ). Extended access incisions are generally required when bone is resected. Composite resections including segments of maxilla or mandible create complex defects with connection between the oral cavity and the nose or neck. Bone and alveolar defects limit the restoration of speech, swallow, and dental rehabilitation (i.e., prosthesis, implants) as well as disrupting the height and width of the middle and lower thirds of the face. Such defects are best reconstructed with free tissue transfer.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here