Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Good outcome measures are a critical component of any successful therapeutics evaluation program. Although some pediatric neuromuscular diseases are now seeing discoveries translated into early-phase clinical trials, there remains a great need for better therapeutics. Bringing these therapeutics to patients requires clinical trials using outcome measures that ideally are easy to implement, are sensitive to change, and reflect an important aspect of the disease.
Outcome measures can be biomarkers, meaning that they measure a biological characteristic of the disease in question. Biomarkers can be metabolites measured in blood or cerebrospinal fluid, electrophysiological measures, or imaging markers. Outcome measures can also be clinical measures, meaning that they measure something that can be reported by observers such as clinicians or caregivers, or by the patient directly.
The goal of using these biomarkers or clinical outcome measures is to assess changes that occur over the course of a clinical trial. Biomarkers or clinical measures can also be used in different contexts, such as when diagnostic or prognostic markers are sought. However, the overview in this chapter will focus only on measures of disease activity or progression, and will discuss them in the context of their potential usefulness in clinical research.
To set the stage for successful clinical trials, researchers need not only patients who are ready to participate, but also high-quality datasets on the natural history of the disease using outcome measures suitable for clinical trials. Collecting natural history data requires significant resources, and an uncommon degree of altruism on the part of patients and their families, because there is no potential for direct benefit to the participant. To lessen the burden added by the study visits, it can be helpful if outcome measures can be collected at the same time that clinical care is provided. Conversely, collecting a small set of outcome measures during clinical visits can also help patients and their care team with charting disease progression. The outcome measures information can help guide care, and can help better understand how the patient’s disability affects function.
Developing and validating outcome measures requires time and resources, and is associated with burden to patients and research teams. Therefore, progress in a given field can be accelerated when research teams can agree on the use of a common set of outcome measures. Using a common set of measures across sites leads to larger datasets being available in a shorter timeframe, so that outcome measures can be developed and tested more efficiently. Avoiding the development and use of multiple outcome measures focused on the same concept and indication can save time and money. In situations when no good outcome measure is available to help address a question, it is preferable if researchers turn to existing outcome measures rather than starting anew in developing one. For example, using an existing scale, or part thereof, can lead to more rapid validation of a potential outcome measure, and can also create opportunities to address important questions across diseases, for example by comparing datasets for two different neuromuscular diseases.
Outcome measures are better delineated for some neuromuscular diseases than others; to a degree, this reflects how far along the respective fields are in terms of therapeutics development. This overview will focus on spinal muscular atrophy (SMA) and Duchenne muscular dystrophy (DMD), but several of the principles and in some cases even the outcome measures discussed may be applicable to a wider range of pediatric neuromuscular disorders.
The hallmark of pediatric neuromuscular disorders is muscle weakness. Muscle weakness can be directly measured using manual or quantitative muscle testing. It can also be measured more indirectly in terms of its effect on motor function. For pivotal clinical trials, an outcome measure that is inherently related to how a patient functions or feels in their everyday life is more meaningful than a measure that quantitates strength but cannot be interpreted in terms of its functional consequences. Weakness can affect muscles other than skeletal muscles; respiratory muscle weakness, for example, is of interest as an outcome in most neuromuscular diseases. Similarly, involvement of bulbar muscles may prompt use of outcome measures assessing bulbar function. In a subset of pediatric neuromuscular disorders, cardiac muscle can be affected as well.
When muscle function or strength cannot be easily measured, or when it is not clear if clinical measures of muscle function would change within the observation period of a trial, then biomarkers may be useful. This is particularly relevant in early phase (Ib or II) trials. In this scenario, it is hoped that biomarkers may be more sensitive to early treatment effect than are clinical measures.
In rare instances in medicine, biomarkers can be surrogates of downstream clinical outcomes. Hypertension, for example, is thought to predict the downstream risk of cardiovascular events. In most instances, this kind of strong association cannot be established. The expectation for pediatric neuromuscular disorders at this time is not to establish a surrogate marker in the foreseeable future, but rather to use biomarkers in a therapeutics development program as an early signal of activity, to be followed by later stage trials with observations using clinical markers.
Another type of biomarker is not specific to the disease and its hallmark features, but is specific to the presumed mechanism of action of the intervention. These kinds of markers of biological activity can be very useful in early proof of mechanism trials when it is important to establish that the intervention has the desired biological effect in patients.
Clinical outcome measures ideally reflect an aspect of the disease that matters to patients. In other words, clinical outcome measures should reflect how a patient feels or functions. This information is best obtained from the patient directly. When assessments of functional status are obtained from an observer, such as a relative, caregiver, or clinician, then the outcome measure captures not only the actual function of the patient, but also the subjective perception and opinion of the observer. Therefore, any measure that captures information from the patient as a source is preferable to one that captures information indirectly.
Clinical outcome measures are, ideally, easily interpretable and clinically meaningful. When an outcome measure focuses on a function relevant to the patient’s daily living activities, the clinical meaning and relevance of any change can be easily understood and communicated. To ensure the meaningfulness of an outcome, experts in outcomes development often start with focus groups to determine which domains are most important to patients, rather than starting with what clinicians think is most important. When outcome measures contain a large number of disparate items, or when they mix functional information with clinical observation and physical examination, then the interpretation of any change is often unclear.
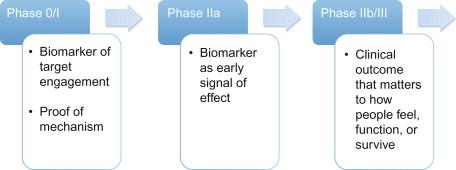
Different outcome measures have variable places in the spectrum of drug development. In early human trials (phase 0 and Ib), biomarkers of mechanism, to demonstrate that the intervention hits its target, are useful. In early exploratory efficacy trials (phase IIa), biomarkers that can signal an early effect of the intervention can be useful. Clinical efficacy trials (phase IIb or phase III) mandate clinical outcomes that ideally indicate how a patient feels, functions, or survives. Figure 54.1 summarizes the drug development process.
The ideal clinical outcome measure is age appropriate, easily administered, functionally meaningful, and imposes minimal patient burden. In rare neuromuscular conditions where enrollment in clinical trials requires multiple international sites, ideal outcome measures are those which require minimal training and equipment to allow participation of investigators with limited clinical resources.
It is best to build on existing tools when choosing an outcome measure because one can take advantage of any data available for the existing tools, compare data to published cohorts in the same or another condition, and take advantage of any regulatory pathway already established for the outcome measure. Outcome measures designed specifically for a particular condition are ideal but not mandatory since children with weakness have similar functional limitations.
There is a broad clinical phenotype both across different pediatric neuromuscular conditions as well as within individual disorders. For example, in SMA, there is a spectrum of disease severity and functional ability, ranging from infants and children never achieving the ability to sit unsupported, to those only able to sit but unable to stand and walk, and to those who can walk but have weakness limiting their ability to rise from the floor, run, and jump. It is difficult to envision a single motor performance-based measure assessing functionally meaningful abilities for all SMA types. Similarly, boys with DMD transition from an ambulatory stage to a nonambulatory stage in which gross motor function is significantly reduced, and upper limb function is a more relevant potential outcome measure. One must consider if the population of patients enrolled in a clinical trial will lose function during their participation that would not be captured on the outcome measure they choose because of a floor effect. For example, if a boy with DMD loses ambulation during a clinical trial where a walking test is the primary outcome measure, without a nonambulatory assessment any further changes in the participant’s clinical function would not be identified.
We have categorized the different motor function outcome measures below into those for ambulatory and nonambulatory children. Careful consideration with regards to the best clinical outcome measure based on age, disease severity, functional level, and rate of progression must be made when designing a clinical trial.
Gait assessments are desirable clinical outcome measures because they reflect weakness, the primary feature in neuromuscular diseases, and are functionally relevant. How a person or child is able to navigate their environment is meaningful and noticeable to both the patient and clinician. As a result of weakness, balance and endurance can be affected and should be quantified in the outcome measure ( Table 54.1 ).
| Outcome Measure | Age | Disease Specific | Assessment Characteristics | Published Clinical Trials |
|---|---|---|---|---|
| Time to rise from floor | > 5 years | No | Measures time to rise from supine; evaluate for Gowers’ maneuver |
|
| Time to walk/run 10 or 30 meters | > 5 years | No | From standing, time to walk/run on a straight path |
|
| Time to climb steps | > 5 years | No | Measures time to ascend and descend stairs |
|
| Six Minute Walk Test | > 4 years | No | Measures distance walked on a 25-meter course. Evaluates functional exercise capacity and fatigue |
|
| Timed up and go test | No | Measures time to rise from a chair, walk 3 meters, turn around, and sit down | ||
| North Star Ambulatory Assessment | > 5 years | DMD | Includes 17 items such as standing, running, jumping, hopping, and stair climbing scored on a 3-point qualitative scale. Some items are timed |
The Six Minute Walk Test (6MWT) is a commonly used assessment in childhood neuromuscular disease that has been used as the primary outcome measure in clinical trials involving conditions with ambulatory participants. While the 6MWT was originally designed to measure exercise capacity in cardiopulmonary disease, it has been widely adopted as an assessment of functional walking ability in both adult and pediatric neurological and neuromuscular conditions. The test is simply the distance walked in 6 minutes on a fixed linear course. It is easily administered and requires no special equipment and little training. Standardization is important and includes prespecifying the level of encouragement given to the patient so that any potentially confounding evaluator influences on performance are minimized. In disorders like DMD, protocols have been established to make testing feasible in children where attentional difficulties may complicate the assessment. Because there is a large body of normative data including children as young as 3 years old on the 6MWT, comparisons across age groups, gender, and body size can be made. This is important because the performance in normal volunteers changes over the course of life due to development and aging, so that comparison to normative data may be needed in some circumstances, rather than just the measurement of absolute change over time. The 6MWT is currently the preferred measure of functional walking ability, endurance, and fatigue.
The 10-meter walk/run test is typically included with the 6MWT in clinical trials. Unlike the 6MWT, children are permitted to walk or run, if possible, as fast as they can. The 10-meter walk/run is easy to administer and is a good complement to the 6MWT because it is more reflective of strength rather than endurance.
Other timed functional assessments for ambulatory participants include time to rise from the floor and time to ascend and descend stairs. These tests typically include a qualitative score in addition to the timed evaluation, to best capture changes in strength and function. For example, time to rise from the floor will elicit a Gowers’ maneuver in conditions like DMD and SMA, in which proximal weakness is the primary problem. If strength improves with a therapeutic intervention, understanding how subjects negotiate the transfer from floor to stand is as meaningful as how quickly they do this. Similarly, the pattern by which a child navigates stairs, such as the use of the railing and their step pattern, is important to evaluate, as it impacts how they function in their environment.
The timed up and go test (TUG) measures the time it takes a patient to stand up from an armchair, walk a distance of 3 meters, turn, walk back to the chair, and sit down. It is a quick, meaningful, and applied objective measure of balance, gait speed, and functional mobility. While TUG was originally designed to identify the community-dwelling elderly at risk for falls, it has been widely adopted as a clinical outcome measure in both pediatric and adult neurological and neuromuscular conditions. Unlike the 6MWT or 10-meter walk/run, TUG incorporates rising from and sitting in a chair, adding another functionally relevant aspect of mobility to the assessment.
So far, the tests described here are not specific to any one neuromuscular condition and are widely applied across clinical trials. Disease-specific measures, when available, may have some advantage as they focus on the unique characteristics and functional deficits of the disorder. The North Star Ambulatory Assessment (NSAA) is designed specifically for boys with DMD. This 17-item assessment includes evaluations of standing, running, jumping, hopping, and stair climbing, scored on a 3-point qualitative scale. Some items on the NSAA are timed and include time to rise from the floor, time to climb stairs, and 10-meter walk/run.
Standardized gross motor function assessments are typically used as primary outcome measures in clinical trials where nonambulatory participants are included ( Table 54.2 ). While ambulatory function is assessed in most of these exams, it is not required. This allows for inclusion and comparisons across a broad phenotypic spectrum of a disorder. Typically these assessments arrange items hierarchically so the child moves through activities from lower to higher functioning items. Gait assessments are typically included but seldom include an evaluation of endurance, making the 6MWT a good complement in ambulatory children. There are many motor function assessments available but those tailored specifically to a single disorder are sometimes considered preferable as they focus on disease-specific problems. In infants, toddlers and young children, developmentally appropriate scales are necessary.
| Outcome Measure | Age | Disease Specific | Assessment Characteristics | Published Clinical Trials |
|---|---|---|---|---|
| Gross Motor Functional Measure (GMFM) | 2–18 years | No | 66- or 88-item motor function assessment | hydroxyurea (SMA) |
| Hammersmith Functional Motor Scale—Expanded (HFMSE) | 2–45 years | SMA | 33-item gross motor function assessment |
|
| Motor Function Measure | 1 – adults>25 years | No | 32 items in 3 domains of motor function | prednisone (DMD) |
| Egen Klassifikation Scale (EK Scale) | teens – adults | No | evaluator administered, self-rated questionnaire of function | |
| Vignos Lower Extremity Scale | DMD | 10-point scale of leg function and ambulation | prednisone (DMD) | |
| Wee Functional Independence Measure (Wee FIM) | 6 months – 6 years | No | functional, evaluator administered questionnaire | |
| Test of Infant Motor Performance (TIMP) and Screening Items (TIMPSI) | infants to 4 months | No | observed and elicited behaviors and motor function | |
| Children’s Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND) | infants and weak children | No | observed and elicited behaviors and motor function |
The Gross Motor Function Measure™ (GMFM) is a well-established assessment that was originally designed to assess children with cerebral palsy. It has been adopted and used in many different neurological conditions, including SMA. The GMFM takes approximately 45 to 60 minutes to complete in stronger, higher functioning children and contains 88 items in 5 dimensions: (A) lying and rolling, (B) sitting, (C) crawling and kneeling, (D) standing, and (E) walking, running, and jumping. This hierarchical organization permits patients to progress through each dimension, according to their ability, without a ceiling effect. A detailed manual for the GMFM is available including video instruction.
The Motor Function Measure (MFM) was developed specifically for people with neuromuscular disease to assess motor function. Similarly to the GMFM, it is organized in 3 domains: (A) standing position and transfers, (B) axial and proximal motor function, and (C) distal motor function. Test items include a continuum of functional ability, organized in a hierarchical fashion, ranging from simple motor skills in supine to a 10-meter run. Also included in the MFM is a fine motor assessment of hand function. The MFM was designed specifically for neuromuscular conditions, and has been widely applied in SMA, DMD, and other dystrophinopathies, and other neuromuscular conditions.
The Hammersmith Functional Motor Scale (HFMS) was originally designed to assess motor function in patients with SMA type 2, and was later revised to include higher functioning and ambulatory SMA patients in an expanded version (HFMSE). This 33-item scale covers a continuum of functional assessments designed to delineate the patterns of weakness present in SMA patients. The test requires only standard equipment and takes less than 15 minutes on average to complete. The HFMSE is highly correlated with other motor function assessments, including the GMFM, and can discriminate between walkers and nonwalkers as well as respiratory function. The scale is well-suited as a clinical outcome measure in SMA clinical trials because of its specificity and minimal patient burden.
While most functional assessments require the patient to perform each motor task, some scales are evaluator-administered questionnaires for which the examiner queries the child or parent on their abilities. The Wee Functional Independence Measure was designed to assess disability in children with developmental delay, based on the framework proposed by the World Health Organization in children between 6 months and 6 years. It is organized in three main domains: (A) self-care, (B) mobility, and (C) cognition, and is scored on a 7-point scale ranging from total assistance to complete independence. While this assessment has been applied to some neuromuscular conditions, it is best suited for those in which cognition may also be affected, which is not the case in SMA.
The Egen Klassifikation Scale is also an evaluator-administered questionnaire that was developed to assess motor function in older, nonambulatory children and teens, as well as adults, in disorders such as DMD and SMA. It includes assessments of activities of daily living such as wheelchair use, ability to transfer, arm function and feeding, turning in bed, coughing, and speaking.
Scales incorporating developmentally appropriate motor function items should be included as outcome measures in clinical trials for infants and young children. The Test of Infant Motor Performance (TIMP) is a functional scale validated in preterm infants under 4 months of age. The TIMP includes both observed and elicited motor assessments, is sensitive to age-related development, discriminates between those at low and high risk for motor problems, and predicts delayed motor development in preterm infants. In neuromuscular disease, specifically SMA, a shorter version of the TIMP that includes only the screening items has been applied, since these patients suffer such profound weakness and motor delay.
Similarly, the Children’s Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND) was developed specifically for weak infants. It includes both active and elicited reflexive movement of the head, neck, and trunk, as well as proximal and distal limb strength. The CHOP INTEND is structured to move from easiest to most difficult, and includes gravity eliminated (lower scores) to antigravity movements (higher scores). Typically, motor function assessments are included as secondary outcome measures in clinical trials in SMA type 1 to measure change over time, but survival or time to respiratory failure are the ideal primary endpoints in this life-threatening form of the disorder.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here