Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pathologic processes in the pediatric esophagus can result in a variety of symptoms. These range from the classic esophageal symptoms of heartburn, odynophagia, dysphagia, chest pain, and regurgitation to nonspecific symptoms such as feeding difficulties, recurrent abdominal pain, or increased fussiness in infants. Dysphagia is defined as difficulty swallowing, whereas odynophagia is defined as painful swallowing. Esophagitis encapsulates more than just chemical damage to the lumen: the term “esophagitis” can be used to describe immunologic, inflammatory, degenerative, chemical, ischemic, and infectious processes. Gastroesophageal reflux disease, eosinophilic esophagitis, structural abnormalities of the esophagus and chest, esophageal foreign body, caustic ingestion, and esophageal motility disorders are discussed in other chapters in this volume. This chapter addresses esophageal infections, chemotherapy/neutropenia-induced esophagitis, graft-versus-host disease (GVHD), radiation esophagitis, medication-induced esophagitis, esophageal involvement by systemic immune-mediated disorders, and esophageal tumors.
When potentially caustic medications fail to rapidly transit into the stomach and remain in the esophagus, thereby dissolving and releasing their noxious contents to damage the esophageal wall, the resulting injury is called medication-induced esophagitis. Most patients experience only self-limited pain, but esophageal hemorrhage, stricture, and perforation may occur, and, in some cases, death has been reported. “Pill-induced” esophagitis is associated with the ingestion of certain drugs ( Box 23.1 ) and accounts for many cases of erosive esophagitis. To date, close to 100 different medications have been reported to induce esophageal disorders. Antibacterials such as doxycycline, tetracycline, and clindamycin are the offending agents in more than 50% of cases. Other commonly prescribed drugs that cause esophageal injury include naproxen, aspirin (acetylsalicylic acid), potassium chloride, ferrous sulfate, quinidine, alprenolol, alendronate, and various steroidal and nonsteroidal antiinflammatory agents. Pill esophagitis has been reported in all age groups and in both male and female patients. However, patients with pathologic disorders such as esophageal rings, webs, compression from an enlarged left atrium, motility disorders, hiatal hernia, gastroesophageal reflux, or prolonged supine position are more susceptible.
Doxycycline
Tetracycline HCL
Oxytetracycline
Minocycline
Pivmecillinam
Penicillin
Amoxicillin
Clindamycin
Naproxen
Aspirin
Ibuprofen
Indomethacin
Piroxicam
Potassium chloride
Alendronate
Ferrous sulphate or succinate
Quinidine
Theophylline/aminophylline
Corticosteroids
Ascorbic acid
Pamidronate
Oral contraceptives
Symptoms are usually acute and can occur immediately after ingestion of medication to as long as several hours later. Most patients present with retrosternal chest pain, odynophagia, and dysphagia, although hematemesis and melena have been reported from drug-induced esophageal damage. , The sudden onset of severe retrosternal pain clearly exacerbated by swallowing should raise the possibility of pill esophagitis, even if medication has been taken correctly. In uncomplicated cases with typical symptoms, diagnostic testing may be avoided if the history includes ingestion of a potentially caustic medication. A careful history and physical examination are required to rule out complications and to determine if removal of the offending medication is feasible. Hemorrhage can be the presenting symptom, particularly with use of nonsteroidal antiinflammatory medications. Deep esophageal ulcers may lead to esophageal perforation and penetration into the adjacent major vessels or the left atrium, resulting in life-threatening or fatal hemorrhage.
Further evaluation with endoscopy is necessary when there is no clear offending medication, when symptoms are unremitting or progressive, or when patients present with hemorrhage. Endoscopy is superior to barium esophagography in identifying subtle mucosal lesions and in establishing alternative diagnoses such as gastroesophageal reflux disease and infectious esophagitis; findings are usually abnormal in drug-induced esophagitis. The higher yield and accuracy make endoscopy the diagnostic procedure of choice.
The junction of the proximal and middle thirds of the esophagus is a common site of injury, presumably because of lower peristaltic amplitude in this region, but any area of the esophagus may be affected. Discrete ulcers with normal surrounding mucosa are the most common endoscopic findings and can vary from a few millimeters to several centimeters in diameter. In one case series, 43% of patients were observed to have kissing esophageal ulcers, which can be a useful diagnostic clue. If diffuse inflammation surrounds the ulcers or is the only finding on endoscopy, biopsies help to exclude other pathology such as infection. Larger and more diffuse areas of injury, deep ulcerations, circumferential lesions, or repetitive injury may lead to fibrotic strictures requiring future dilation or even surgery.
In most cases, withdrawal of the offending agent is sufficient to allow for healing and resolution of symptoms within several days to a few weeks. No treatment has been proven to speed up recovery; however, acid suppression, sucralfate, and topical anesthetics are often used to lessen symptoms and improve oral intake. On rare occasions, prolonged severe odynophagia can lead to anorexia and the need for temporary parenteral nutrition. Complications such as strictures, perforation, mediastinitis, or hemorrhage require specific therapy.
Although fungal species may cause life-threatening infections in some people, most individuals carry them asymptomatically. In fact, in the case of Candida albicans , such fungi are considered to be part of the benign commensal microflora that inhabits the skin, the mucosal surfaces, and the gastrointestinal tract of many healthy individuals. , In the immunocompetent host, the frequency of oral yeast carriage varies from approximately 40% in children to 48% in adults over age 18. , The maintenance of a healthy host-fungal interaction is sustained by a complex equilibrium of several interconnected factors. Theses interactions between fungi and their hosts begin at the cell-cell interface. Fungal cells differ from animal cells primarily in the cell wall that includes numerous molecules that act in pathogen-associated molecular patterns (PAMPs). These PAMPs are recognized by the host through an array of pattern-recognition receptors (PRRs), including Toll-like receptors (TLRs) and C-type lectin receptors (CLRs), which are able to sense the different molecular moieties that comprise the fungal cell wall. Instead of a simple one-to-one interaction between each PRR and its cognate PAMP the host-fungal interaction is a complex system with many dynamic features allowing the host to discriminate between pathogenic and nonpathogenic fungi.
At least five different forms of C. albicans can be identified (i.e., white and opaque yeast cells, pseudo-hyphae, hyphae, and chlamydospore). Although yeast forms ensure the dissemination of C. albicans , hyphae facilitate tissue invasion or biofilm formation and chlamydospores are predicted to allow survival in hostile environments. Furthermore, C. albicans can induce these different morphologic switches, such as the yeast-to-hyphae transition, in response to several stimuli encountered in the host (such as CO 2 ), masking certain cell-wall components and unmasking others, thereby qualitatively changing the PAMPs that it exposes to the host.
The control of the fungal population by the human host is not limited to the interaction between the fungi and the immune system; it also involves the estimated 1000 microbial species in the human microbiome. Several specific synergistic and antagonistic interactions have been identified that take place between bacteria and fungi in the gastrointestinal tract. For example, fluconazole resistance and virulence of C. albicans are enhanced by Pseudomonas aeruginosa, Escherichia coli , and Staphylococcus epidermis, , - whereas Lactobacilli species produce reactive oxygen, organic acids, and biosurfactants, all of which can inhibit C. albicans growth. Disruption of this equilibrium of the host-bacterial-fungal interaction through primary or acquired immunodeficiency can lead to severe fungal infections.
Oropharyngeal candidiasis (OPC) and esophageal candidiasis (EC) are the most common fungal infections of the gastrointestinal tract and have been well described in adults and children with underlying HIV infection. In a large pediatric study of HIV-positive patients, low CD4 counts (fewer than 200 cells/μL) and antibiotic exposure were the most prominent risk factors for development of EC. Indwelling catheters, chemotherapy, use of broad-spectrum antibiotics, and organ transplantation are additional risk factors. However, even in the immune-competent host change of the mucosal balance due to inhaled steroids for asthma therapy, swallowed steroids for treatment of eosinophilic esophagitis, or acid suppression can predispose to candidal esophagitis. Oral thrush may be an indicator of an underlying pathologic esophageal process. In a large pediatric study of EC, oral thrush was the single most common presentation (94%), followed by odynophagia (80%), retrosternal chest pain (57%), fever (29%), nausea/vomiting (24%), dehydration (12%), and gastrointestinal bleeding (6%). In adults, however, oral thrush was absent in 25% of Candida esophagitis cases.
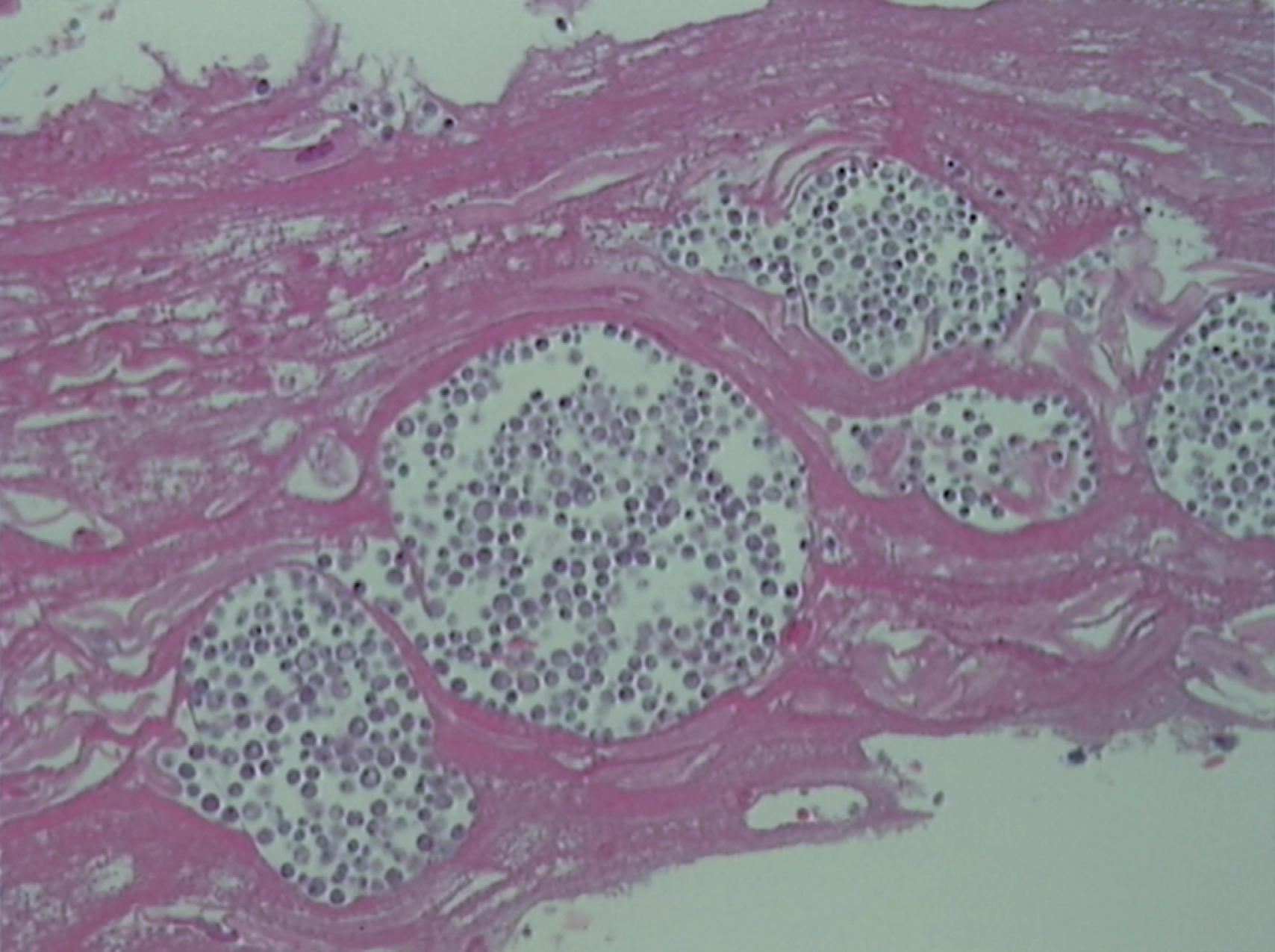
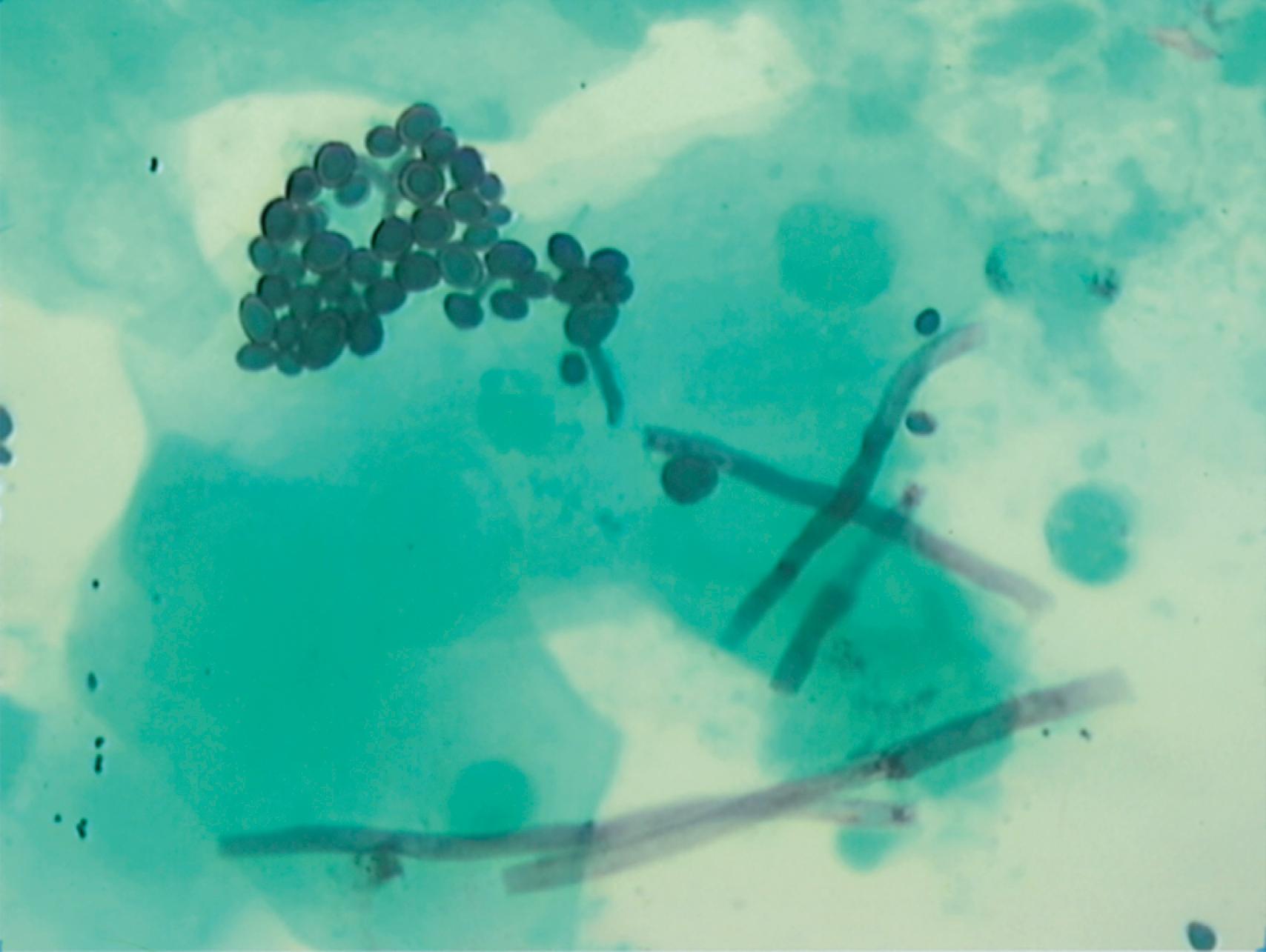
Endoscopic findings in candidal esophagitis are raised, white candidal plaques in the esophagus that cannot be washed away with water. Brushing of the plaques usually leads to bleeding at the site of attachment. The plaque represents desquamated epithelial cells with debris of fungal organisms, inflammatory cells, and bacteria. Endoscopic appearance alone is insufficient for diagnosis of Candida esophagitis. Plaque-like material mimicking Candida may be found in severe reflux esophagitis, herpes simplex infection, cytomegalovirus (CMV) infection, pill esophagitis, eosinophilic esophagitis, and swallowed oropharyngeal debris. Cytologic examination of brushings is more sensitive than histologic examination of biopsy specimens to confirm diagnosis of esophagitis. Budding yeast cells, hyphae, and pseudo-hyphae are best seen by silver stain, periodic acid–Schiff (PAS) stain, or Gram stain. Brushings showing mycelial forms and budding yeast should be interpreted as confirming invasive Candida infection ( Figs. 23.1 and 23.2 ). Culture of the mucosa is usually not indicated, but should be undertaken if azole-resistant Candida species are suspected or if unusual pathogens (e.g., bacterial, Mycobacterium tuberculosis , or viral esophagitis) are being entertained in the differential diagnosis of the clinical presentation. Rarely, adherent plaques may not be present. An inflammatory stricture with no gross hint of a fungal cause may prove to have invasive fungal elements on biopsy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here