Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Neonatal intensive care units (NICUs) are organized for the clinical care of premature and critically ill newborn infants.
Healthcare centers require a well-considered structure to enable collaborative decision-making to provide family-centered, high-value care to the mother-infant dyad.
In most parts of the world, NICUs are designated per the infrastructural levels and the severity of illness of infants receiving care in the units.
With increasing information on the determinants of outcomes, specialized, disease-focused level IV NICUs are in development, such as small-baby units, neuroneonatal intensive care units (ICUs), congenital diaphragmatic ICUs, esophageal airway and trachea programs, and neonatal surgical units.
NICUs care for the most vulnerable patients receiving multisystem support, multiple medications, indwelling central catheters, parenteral nutrition, and various other clinical interventions. In this complex paradigm, a central philosophy of “zero harm” has been emphasized.
Care coordination and communication are key for a safe discharge process and optimal outcomes.
Neonatal intensive care units (NICUs) care for vulnerable patient populations, and there is a need to staff these in-patient hospital sections with an appropriate complement of medical, nursing, and support staff (healthcare professionals). Medical and hospital leaders both need to work together to ensure efficient, seamless operations to provide the highest-value care to infants admitted to the NICUs and to their families. In most parts of the world, the NICUs are designated per the recommendations of the American Academy of Pediatrics in the United States and those of comparable national organizations, which closely resemble each other. This need to designate NICUs is indeed important, and these decisions have to be based on the complexity of medical conditions treated, the risk of mortality, and the average daily patient census in these units.
In the United States, there has been considerable discussion about the best strategies to improve neonatal care. The nurse-to-patient ratio, when analyzed in the context of illness acuity tools, is an important marker. There is also a need for continuous improvement in the utilization and education of the trainee workforce (physician residents, fellows, trainee nurses, and students in various auxiliary services). There are important recommendations from the Accreditation Council for Graduate Medical Education ( https://www.acgme.org/ ) and comparable global organizations. These recommendations combine our current understanding of the impact of the skill sets of trainees and the staffing priorities in the newborn nurseries/NICUs. The goal of developing these collaborative healthcare teams is to provide safe, efficient, timely, and effective care based on current evidence. All these considerations require effective leadership, optimal communication, understanding of our goals, and coordinated care.
Healthcare centers require a well-considered structure to enable collaborative decision-making to provide family-centered, high-value care to the mother-infant dyad. This is a priority, and this change in focus contrasts with traditional leadership models that drew primarily on industrial structures that were recognized as financially efficient. It is now recognized that the medical director and the nurse manager need to work with all the other key leaders in the newborn nursery and the hospital to oversee policies and procedures and ensure constant availability of behavioral competencies, cognitive abilities, and technical skills in order to provide safe, effective, and evidence-based care. Obviously, they need to track clinical, quality, and revenue outcomes, but these goals need to be expanded. In this regard, the designation of NICUs by expert groups such as the American Academy of Pediatrics Committee on the Fetus and Newborn provides a framework with appropriate leadership structures to provide high-value patient care. Indeed, these designations are gradually being adopted worldwide. For level I newborn nurseries, a designated pediatrician can serve as the medical director and collaborate with the nurse manager to provide care to healthy late preterm and term infants. This team can also treat a selected population of newborn infants with medical issues of relatively lower complexity seen in the first few days after delivery, such as establishing maternal feeding, preventing hypoglycemia, ensuring that infants with known high-risk factors do not have actual neonatal sepsis, observation of transient heart murmurs, and monitoring of physiologic hyperbilirubinemia. In this period, close medial-nursing teamwork will ensure appropriate transitional care, and if needed, a smooth transition to higher-intensity clinical management in level II–IV NICUs. All stakeholders will need to work together as a team to meet the needs of patients/families and also to ensure work-life balance for all care providers.
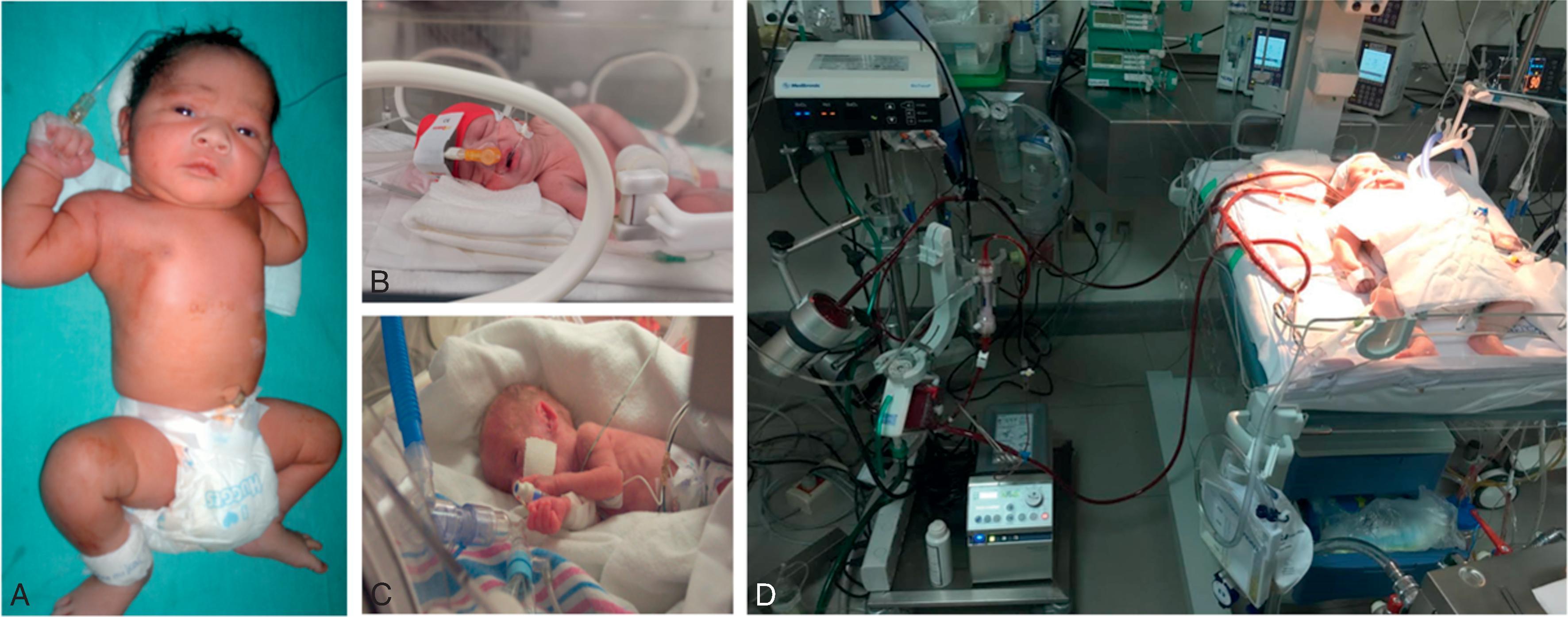
The composition of the care-provider workforce is usually based on the intensity- and complexity-based designation of the NICUs ( Table 100.1 , Fig. 100.1 ).
| Level of Newborn Care | Scope |
|---|---|
| Level I | Care for healthy, full-term babies. The focus is to stabilize babies born at or near full term for discharge or ensure timely, safe transfer to facilities that provide advanced care. |
| Level II | Provide advanced newborn care to infants born at greater than 32 weeks’ gestation or who are recovering from more serious conditions. |
| Level III | Provide subspecialty newborn care to infants born at less than 32 weeks’ gestation and to those born with critical illness at all gestational ages. These facilities offer a full range of respiratory support and advanced imaging and can provide prompt and readily available access to a full range of pediatric medical subspecialties, pediatric surgeons, and pediatric anesthesiologists. There is a need to transfer infants with critical congenital heart defects or those who may need extracorporeal membrane oxygenation. |
| Level IV | Provide the highest-level, most acute care. These nurseries are located in hospitals that can provide surgical repair of complex congenital or acquired conditions and have a full range of pediatric medical and surgical subspecialties and pediatric anesthesiologists on site. Level IV neonatal intensive care units also facilitate transport and provide education outreach. |
Most level I nurseries are managed by pediatricians and experienced nurses. Other medical providers, such as pediatric and/or family practice nurse practitioners, physician assistants, and pediatric resident trainees may be involved. However, the numerical adequacy of care providers often varies between nurseries and may depend on the geographic location, the relative size of the medical center, the availability of resources, the number of births, and various other responsibilities entrusted to the providers. Ideally, a consistent, dedicated group of medical providers in the newborn nursery would facilitate seamless, high-value care, effective collaboration among staff, and overall satisfaction of mothers and families. In many countries, these neonatal units have been provided the basic infrastructure to treat mild illnesses and avoid the need for long-distance transfers. One such example is the creation of sick newborn care units in India, which has helped lower the mortality rates in many parts of the country.
Level II nurseries have been successful in lowering infant mortality, but the levels of staffing remain variable. Studies show that the size of these nurseries is often dependent on operational revenues, requests by obstetricians, and the availability of experienced staff in the specific geographic location. Many level II NICUs are still managed by only a minimal number of neonatologist(s) available in the region, who work with advanced-practice providers (such as experienced midwives, advanced nurse practitioners, or physician assistants who have some experience in newborn care). The accreditation committees have emphasized that these level II nurseries need to have a skilled neonatal provider in house 24/7 to attend high-risk deliveries in a timely manner, and these recommendations have facilitated the development of an appropriate provider workforce. There is still a considerable shortage of adequately trained neonatal nurse practitioners across the world. Consequently, there is a desperate need for pediatricians with interest and expertise in neonatology (neonatal hospitalists) to maintain the workflow.
In level III and level IV NICUs, the staffing situation is slightly better. The medical provider workforce has evolved during the past 2 decades based on cohort-based care models and other specific areas of expertise. The medical provider groups in most level III and level IV NICUs are composed of neonatologists, neonatology fellows, pediatric residents, and advanced-practice providers (neonatal nurse practitioners and/or physician assistants). The staffing models in level III NICUs depend on whether there is a requirement for the neonatologists to be in house to render timely and in-person supervision of the trainee and/or auxiliary staff. The organizations make these operational decisions based on the need to hire neonatologists to provide in-house coverage and its financial implications. There is an ongoing debate on whether level III NICUs need 24/7 neonatologist coverage, because the impact on clinical outcomes remains unclear.
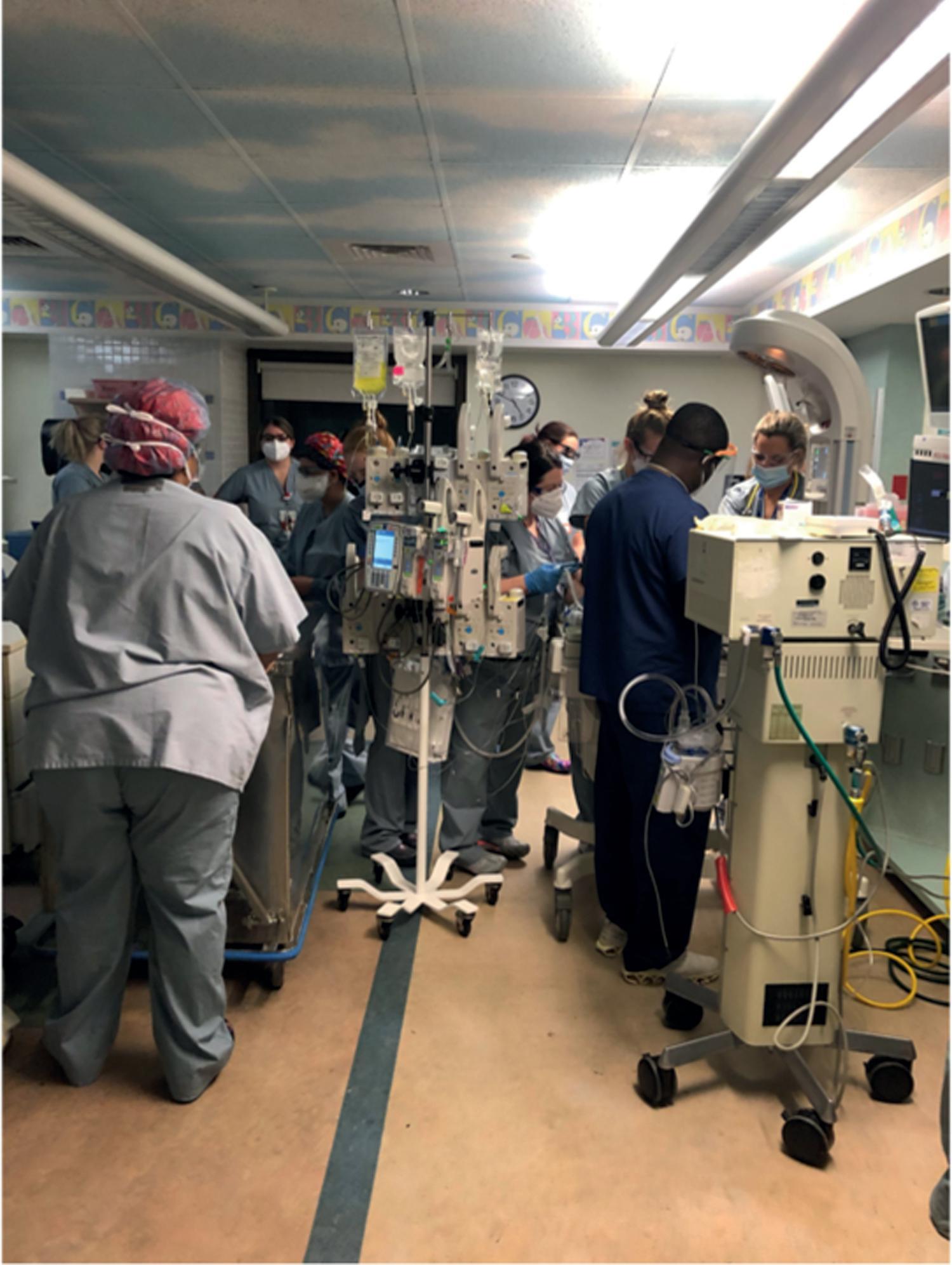
We do not anticipate major changes in the immediate future in the medical provider workforce in level III NICUs, but there is a possibility of a significant shift in care models in level IV NICUs. Children's hospitals, where most of the best-equipped level IV NICUs are located, are developing specialized, disease-focused units within the NICUs; these facilities include small-baby units, neuroneonatal intensive care units (ICUs), congenital diaphragmatic ICUs ( Fig. 100.2 ), esophageal airway and trachea programs, and neonatal surgical units. , These specialized programs add to the complexities in the development of leadership, operations, medical provider staffing, and challenges in allocations of revenue and personnel. To find some solutions, many units are training the most-motivated personnel for collaborative functioning and leadership. There is a major need for committed medical providers, who can/will help plan and develop condition-specific clinical programs. These consolidated cohorts are already beginning to show improved expertise and clinical outcomes, timely referrals, allocation of resources, and the development of focused translational and clinical research. All these developments show exciting feed-forward loops with support from all constituents, be it physicians, hospitals, or the local administration. This may potentially bring a true change in the outlook for infants with problems that were hitherto considered to be lethal in most patients.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here