Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Because of its prominent position, the zygoma is one of the more frequently injured facial bones. The zygomatic bone is an essential structure of the midface and serves as a foundation, contributing greatly to both form and function. Fractures of the zygoma occur independently and in association with fractures to adjacent bones, such as Le Fort fractures. Since the zygoma constitutes most of the lateral orbital wall and part of the orbital floor, these fractures are sometimes referred to as orbital (orbito-) zygomaticomaxillary complex fractures (OZMC fractures).
In a study of 362 patients, the age group presenting with zygomatic fractures most heavily represented was between 20 and 29 years of age, at 41% of the patient population, followed by the group between 30 and 39 years of age, at 18% of the patient population. In a separate study conducted by Ozyazgan et al., 689 patients with midface fractures were evaluated. Males constituted 81% and females 19% of these patients. Throughout the majority of the literature most of the patients presented between 20 and 40 years old. The most common causes leading to OZMC fractures are motor vehicle collisions, assaults, falls and sporting injuries. Some variations in incidence and pattern occur with age and geographic location.
The zygoma or cheek bone is an important foundation structure of the craniofacial skeleton; it is the most anterolateral projection of the midface. This lateral structural pillar helps dissipate forces along the cranial base. In doing so, it provides significant strength and stability to the midface. The zygoma presents as a thick quadrangular bone and constitutes most of the lateral and inferior orbital walls. Its strength comes from its five projections. These projections articulate with the frontal, sphenoid, temporal, maxillary bones, and inferior orbital rim ( Fig. 1.12.1 ) forming the zygomaticofrontal, zygomaticosphenoid, zygomaticotemporal, and zygomaticomaxillary sutures, and inferior orbital rim respectively. Fractures usually occur at or near these five articulations. The articulation at the frontal bone is strongest, often fracturing incompletely, or greensticking. The frontal process of the zygoma may also be displaced behind the zygomatic process of the frontal bone, and thus, impacted.
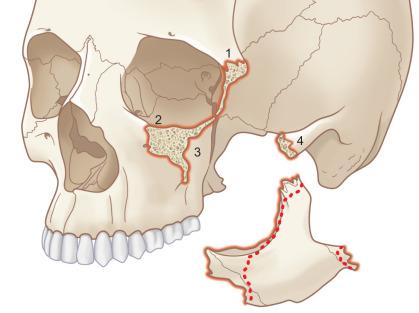
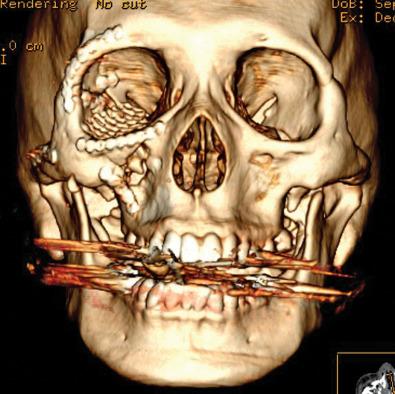
A comprehensive knowledge and understanding of the surgical anatomy of the orbit is necessary when treating OZMC fractures, as the orbit is frequently involved ( Figs. 1.12.2–1.12.4 ). The lateral orbital wall is formed by both the orbital process of the zygoma and the greater wing of the sphenoid bone. The zygomaticosphenoid suture, the greater wing of the sphenoid, and the zygomatic arch serve as key anatomical landmarks to ensure proper reduction and are especially helpful in treating comminuted fractures.


Another key anatomical landmark is the zygomaticofrontal suture – the site where the frontal bone and the lateral orbital wall meet. This area is usually at least 4 mm thick. The zygomatic arch, which lies lateral to the zygoma, includes the temporal process of the zygoma and the zygomatic process of the temporal bone. In the area where it inserts to the body of the zygoma it is commonly 4 mm or more in thickness. The area of the zygoma that extends medially towards the infraorbital foramen can be as thin as 2 mm. These thicknesses are pertinent as thinner areas correlate with a higher likelihood of fracture and comminution.
The second division of the trigeminal nerve also branches to the zygomatic-facial and temporal branches that exit the foramina in the body and frontal process of the zygoma, and provide sensory innervation in the area adjacent to the zygoma, including a segment of the lateral cheek and anterior temporal region, respectively. Another branch of the maxillary nerve, the infraorbital nerve, exits via the infraorbital foramen after coursing the orbital floor. This nerve provides sensation to the anterior cheek, bilateral nose, upper lip, and through a separate branch in the bone, the anterior maxillary teeth.
Pertinent facial and mimetic muscles in this area include the temporalis, zygomaticus major and minor, the levator labii superioris, and the masseter. The zygomaticus major, minor, and labii superioris are all innervated by cranial nerve VII and are all muscles of facial expression. The temporalis muscle attaches to the zygomatic arch and posterior portion of the body of the zygoma. These muscles and fascia are displaced inferiorly with fractured fragments due to their attachments. The masseter attaches along the inferior zygomatic arch around the temporal surface of the zygoma and plays a role in the inferior displacement of the zygoma following fracture.
Other anatomic landmarks of relevance include Lockwood's suspensory ligament, Whitnall's tubercle, and the lateral canthal tendon. The vertical position of the globe is largely determined by the attachment of Lockwood's suspensory ligament and the lateral canthal tendon to the lateral orbital wall. The lateral canthal tendon is attached to Whitnall's tubercle, which is located below the zygomaticofrontal articulation and is positioned on the inner medial portion of the frontal process of the zygoma. Inferiorly displaced fractures of the OZMC may result in inferior displacement of the lateral canthus.
OZMC fractures are most commonly attributed to motor vehicle collisions, assaults, falls, and sports injuries. Patients presenting from such trauma should be first evaluated for life-threatening injuries and stabilized. Careful evaluation must be taken of both bony and soft tissue components of the injury. It is critical to evaluate the status of cranial nerves II to VI, eyelids, lacrimal apparatus, canthal tendons, globe, visual function and acuity, diplopia, and retina. An ophthalmology consultation should be considered whenever injury to any part of the ophthalmic apparatus is present. It is also important to record the history: the nature, force, and direction of the causative trauma. The direction of trauma is important as differing directions of impacts create different presentations. Assault usually results in direct lateral blows that typically present with inferomedial fracture and posterior displacement. A direct blow to the side of the head may result in an isolated zygomatic arch fracture. Trauma from a frontal direction often leads to a fracture with posterior and inferior displacement. More severe impact forces cause disruption of muscle attachments and ligaments, creating lateral displacement and more comminution. Displaced fractures may lead to facial flattening on the affected site which is often best appreciated from a superior “bird's eye” view. This is due to a depression of both the malar eminence and infraorbital rim. Enophthalmos may also be evident especially from an inferior or “worm's eye” view with the globe positioned inferiorly, posteriorly, and medially. The palpebral fissure may be altered due to the inferior position of the zygoma with its attachment of the lateral canthus. In higher energy fractures, the displacement of the zygomatic body is lateral, and the midface is widened on that side.
Patients with OZMC fractures often present with pain, epistaxis, diplopia, subconjunctival hemorrhage, and periorbital edema and ecchymosis. OZMC fractures typically involve the orbital floor and normally travel through the infraorbital foramen and groove of the infraorbital nerve. Because of this, many patients present with decreased or absent sensation in the areas of distribution of both the zygomaticotemporal and infraorbital nerve. These areas include the cheek, lateral nose, maxillary anterior teeth, and ipsilateral upper lips. Trismus may be present whenever medial displacement causes impingement of the body on the coronoid process of the mandible or may be due to contusion of the masseter muscle. This manifests as limited opening and range of motion of the mandible. Downward displacement of the zygoma of that side can present with an antimongoloid slant of the palpebral fissure because of displacement of the lateral canthus, enophthalmos because of orbital enlargement, and a more pronounced supratarsal fold of the upper eyelid. On clinical examination, physical palpation should be completed and must include the orbital rim, zygomaticofrontal suture, zygoma, zygomaticomaxillary interface, and zygomatic arch. These areas should be assessed for any bone separation, step-offs or tenderness, as these would suggest further radiographical evaluation and indicate the presence of a fracture.
Patients with isolated arch fractures usually have trismus and limited mouth opening. These patients normally present with pain and decreased mandibular motion, but no orbital signs. A depression is often observed over the fracture; however, this may be masked if there is significant edema in the area.
Patients should have a thorough orbital examination, including evaluation of extraocular muscle movements noting incomplete excursion as possible entrapment of the globe. An ophthalmology examination prior to surgery may be necessary based on initial examination and suspected visual loss or globe injury. | A study by Barry et al. found 23 patients out of 138 to have ocular injuries. The most common include diplopia, enophthalmos, retina and pupil injuries (traumatic mydriasis). Jamal et al. evaluated 98 patients and found that 66.6% sustained minor ocular injuries. Studies have shown major ocular injuries such as ruptured globe, retinal hemorrhage or detachment and hyphema occur in approximately 10% of these patients, whereas the incidence of traumatic optic neuropathy is approximately 6%.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here