Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Subperiosteal orbital abscess (SPOA) is a well-defined complication of bacterial ethmoid sinusitis with potential vision and life-threatening sequelae. In fact, the most common cause of orbital cellulitis is sinusitis, especially of the ethmoid sinuses. The severity of these potential outcomes emphasizes the importance of rapid clinical identification, risk stratification, and treatment. During the second half of the 20th century, these sequelae prompted surgical drainage of the orbit and sinuses in nearly all patients with this diagnosis. There have since been retrospective analyses showing bacteriology and response to antibiotic treatment correlating with the patient’s age. It has been speculated that age-related anatomic and physiologic differences in the sinuses may account for this correlation. The sinus cavities markedly enlarge from the neonate to the adult, but the ostia remain constant. The rapid growth of the sinuses leads to a relative overwhelming volume to be drained by the unchanged size of the ostia. Bacteria can easily access the subperiosteal space through foramina and direct extension through thin bones such as the lamina papyracea.
After the patient is under general anesthesia, forced ductions are always performed in all directions of all SPOA patients before and after drainage of the abscess. This helps differentiate a paretic from a restrictive ophthalmoplegia, thereby allowing for clinical correlation when there is suspected cavernous sinus involvement. The contralateral eye can be used for comparison if uncertain.
Ensure that the cornea is protected at all times.
When using a sub-eyebrow approach, bevel the scalpel blade in the direction of cilia growth to help prevent the destruction of the hair follicles.
When using an inferior approach:
Take care to follow the curvature of the apex of the orbital rim to help prevent premature entry into the orbit and thusly unwanted presentation of orbital adipose tissue.
Use a circumspect approach to the periosteum to help prevent dissection into the eyelid or even transection of the origin of the inferior oblique muscle (IOM).
When using a medial approach:
Be cognizant of the origin of the IOM.
The caruncle is an easily identifiable and reliable external landmark for prediction of the IOM origin. The origin of the IOM is just anterior to a small depression just below and lateral to the lacrimal sac fossa.
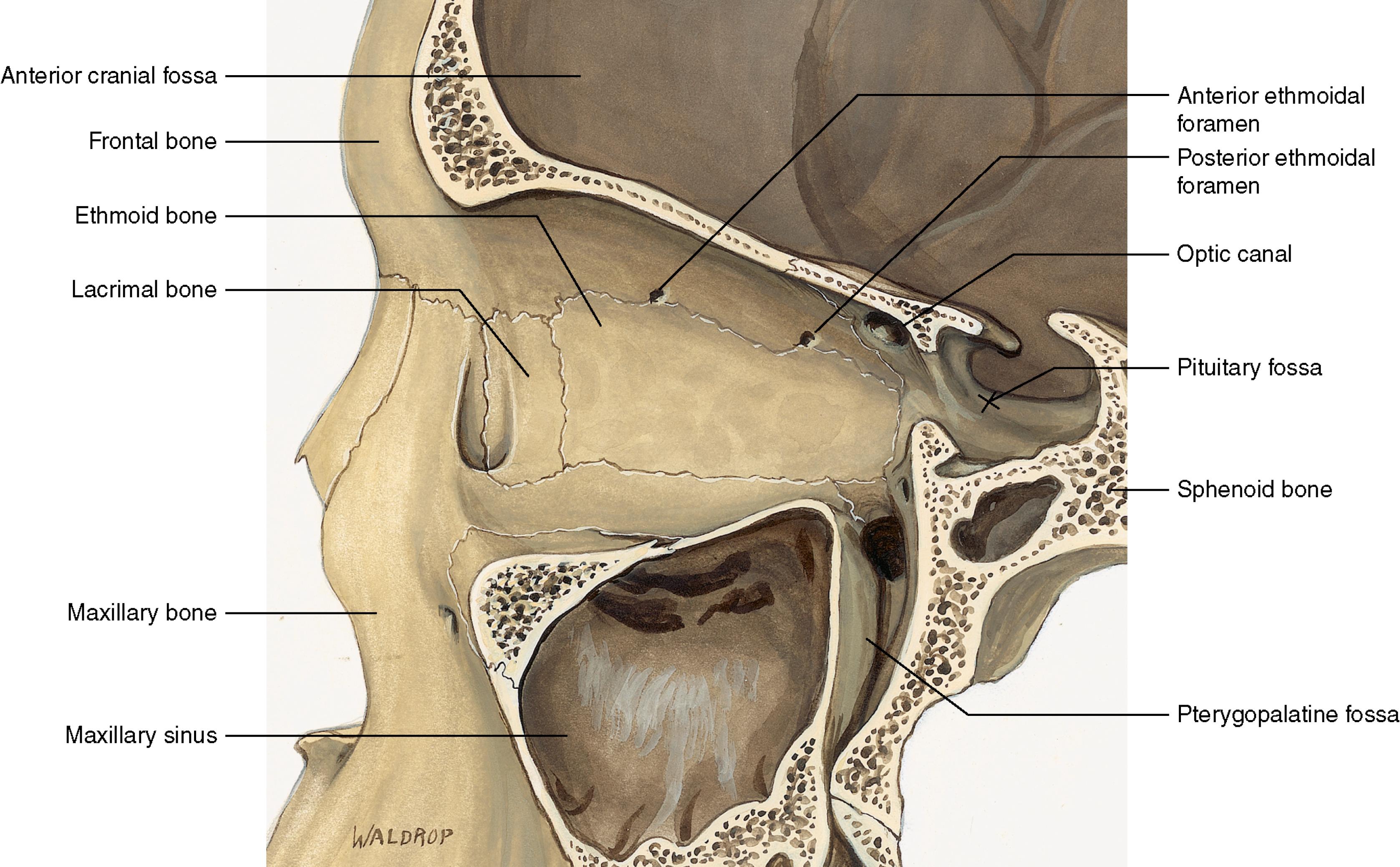
“The rule of twelves”—The anterior-to-posterior length from the anterior lacrimal crest to the anterior ethmoidal foramen is approximately 24 millimeters. From the anterior ethmoidal foramen to the posterior ethmoidal foramen is approximately 12 millimeters, and from the posterior ethmoidal foramen to the optic canal is about six millimeters ( Fig. 152.1 ).
Being cavalier in the approach to the medial periosteum can result in fracture of the ethmoid bone or even transection of the origin of the IOM.
Take care not to use the globe as a fulcrum.
Always obtain cultures/Gram stain of the abscess contents.
History of present illness
Potential source of the abscess can be elicited by asking about recent sinus infections, preceding trauma compromising the integrity of the skin, or recent insect bites
Onset of eye pain, headache, decreased vision, pain with movement of the eye
Antibiotic or other treatment prior to presentation
Past medical history
Previous episodes of orbital cellulitis or orbital abscess. How were they treated?
Existing renal disease, integumentary or hematologic methicillin-resistant Staphylococcus aureus (MRSA) infection, chronic sinus infection
Surgery including organ transplantation and previous sinus surgery
Otherwise immunocompromised state
Medications
Anticoagulants
Allergies to antibiotics
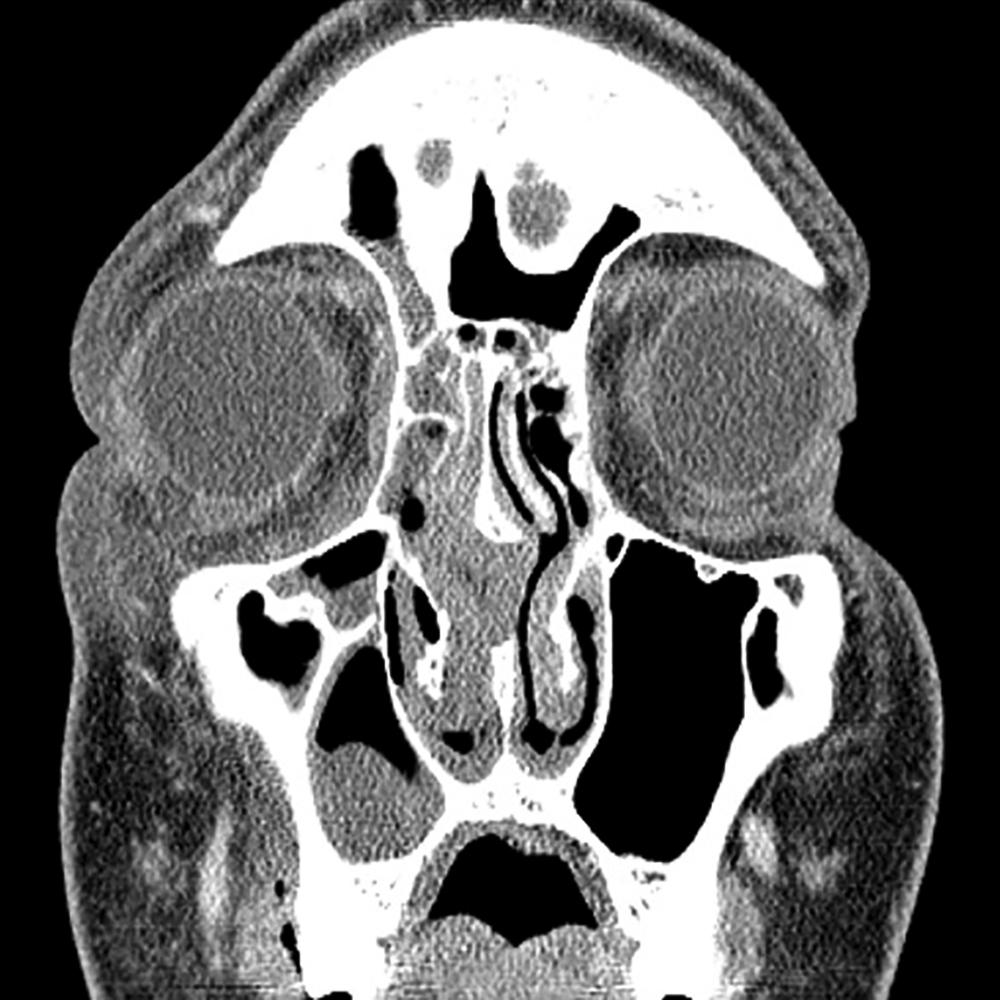
Every patient with orbital cellulitis, irrespective of the presence of a SPOA ( Fig. 152.2 ), should have an ophthalmologic examination at least twice daily to include the following:
Assessment of periorbital/eyelid edema and erythema
Visual acuity
Color vision
Measurement of intraocular pressure
Evaluation of pupils for the presence of an afferent pupillary defect
Assessment of chemosis
An undilated evaluation of the posterior pole
Exophthalmometry
Extraocular motility
Associated pain with extraocular motility

Computer tomography (CT) scan of the orbits with and without contrast or CT maxillofacial with and without contrast ( Figs. 152.3 to 152.5 )


The following patients should undergo immediate surgical intervention:
Those less than 9 years of age with any of the following age-superseding criteria:
Decreased vision
Signs of optic neuropathy
Large SPOAs
An SPOA that is located anywhere except medially
Frontal sinusitis
Intracranial involvement
Risk factors for anaerobic involvement
The following patients should undergo surgical intervention within 8 to 24 hours:
All patients ≥9 years of age
Always consider:
Decrease in visual function (acuity and color vision)
SPOA size
SPOA location
Frontal sinus involvement
Intracranial extension
Factors predicting anaerobic infection such as:
Age ≥9 years
Chronic sinusitis
Odontogenic origin
Patients failing prompt response to intravenous antibiotics proceed to surgical drainage
No clinical improvement after 72 hours
Clinical deterioration despite 48 hours of treatment
Lack of fever abatement after 36 hours of appropriate antibiotic treatment
Surgical factors
Inadequate expertise of the surgeon
Evaluations by:
Ophthalmologist
Otolaryngologist well versed in endoscopic sinus surgery
Internist/pediatrician
Anesthesiologist
Keep patients on nothing by mouth (NPO).
Broad-spectrum intravenous antibiotics (e.g., third-generation cephalosporin or ampicillin/sulbactam + vancomycin or clindamycin) to include anaerobic coverage especially in those with signs of or suspected chronic sinusitis or an SPOA of odontogenic origin
A lateral canthotomy and cantholysis may be indicated to help relieve an orbital compartment syndrome.
General
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here