Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Surgical procedures of the head and neck present unique anesthetic challenges. Operative field isolation places the anesthesia provider at a distance from the airway and hampers access to the patient. The region's extensive parasympathetic innervations predispose patients to intraoperative bradycardia and asystole. Ophthalmic and otolaryngologic procedures require smooth induction and emergence from anesthesia. Coughing and bucking increase venous and intraocular pressure (IOP), which may negatively affect surgical outcome.
More than 2 million cataract operations are completed nationally each year. Most eye procedures are considered low risk for perioperative complications; however, ophthalmic patients are often at greater risk during surgery because typically they include the elderly (also see Chapter 35 ), who frequently have multiple concomitant medical issues, or pediatric patients (also see Chapter 34 ), who may be premature or have associated syndromes. Additionally, most operations are conducted on an ambulatory basis (also see Chapter 37 ), emphasizing the importance of preoperative evaluation (also see Chapter 13 ).
Most ophthalmologic procedures are performed via monitored anesthesia care (MAC) and some form of regional or topical eye anesthetic. Aside from intraoperative analgesia and akinesia, advantages of ophthalmic regional blocks include suppression of the oculocardiac reflex (OCR) and provision of postoperative pain management. An understanding of regional block techniques and management of their complications is requisite. General anesthesia is reserved for operations of prolonged duration; more invasive orbital procedures; and patients unable to remain relatively still such as neonates, infants, and children.
Anesthetic drugs and maneuvers may affect ocular dynamics and surgical outcomes, and ophthalmic medications can cause adverse anesthesia reactions or may significantly affect systemic physiology. Appreciation of factors affecting IOP and vigilance vis-à-vis the OCR are critical.
Adequate pressure within the eye serves to maintain refracting surfaces, corneal contour, and functionally correct vision. IOP is primarily derived from a balance between aqueous humor production and drainage. Aqueous humor is actively secreted from the posterior chamber's ciliary body and flows through the pupil into the anterior chamber, where it is admixed with aqueous humor passively produced by blood vessels on the iris's forward surface. After washing over the avascular lens and corneal endothelium, aqueous humor filters through the spongy trabecular meshwork into the canal of Schlemm tubules at the base of the cornea. From there, it exits the eye into episcleral veins and ultimately to the superior vena cava and right atrium. Therefore any obstruction of venous return from the eye to the right side of the heart can increase IOP. Lesser factors that influence IOP include force transmitted to the globe by contraction of the orbicularis oculi or extraocular muscles in addition to hardening of the lens, vitreous, and sclera that can occur with aging.
IOP ranges between 10 and 22 mm Hg in the intact normal eye. Typically, there is a 2 to 5 mm Hg diurnal variation. Small transient changes occur with each cardiac contraction and with eyelid closure, mydriasis, and postural changes. These changes are normal and have no bearing on the intact eye. A sustained increase in IOP during anesthesia, however, has the potential to produce acute glaucoma, retinal ischemia, hemorrhage, and permanent visual loss.
Venous congestion resulting from obstruction at any point from the episcleral veins to the right atrium may cause a substantive increase of IOP. Before induction of anesthesia, Trendelenburg positioning or presence of a tight cervical collar can increase intraocular blood volume, dilate orbital vessels, and inhibit aqueous drainage. Straining, retching, or coughing during induction of anesthesia will markedly increase venous pressure and can readily precipitate an increase in IOP of 40 mm Hg or more. Should this occur while the globe is open during surgery, such as during corneal transplant, loss of vitreous, hemorrhage, and expulsion of eye contents may lead to permanent damage to the eye or even blindness. Arterial hypertension can transiently increase IOP but has much less impact than perturbations of venous drainage. External compression on the globe by a tightly applied facemask, laryngoscopy, and tracheal intubation also elevate IOP, but placement of a supraglottic airway has minimal impact. Hypoxemia and hypoventilation can increase IOP. Hyperventilation and hypothermia have the opposite effect.
Inhaled and most intravenous anesthetics produce dose-related reductions in IOP. Although the exact mechanisms are not known, IOP is probably reduced by a combination of central nervous system depression, diminished aqueous humor production, enhanced aqueous outflow, and relaxation of extraocular muscles. There is controversy surrounding the effect of ketamine on IOP. Although ketamine may not increase IOP, it does cause rotatory nystagmus and blepharospasm, making it a less-than-ideal anesthetic for eye surgery.
In the absence of alveolar hypoventilation, nondepolarizing neuromuscular blocking drugs decrease IOP via relaxation of the extraocular muscles. In contrast, succinylcholine produces an increase of about 9 mm Hg in 1 to 4 minutes after intravenous administration, with a subsequent diminution to baseline within 7 minutes. The increase in IOP is probably the result of several mechanisms, including tonic contraction of extraocular muscles, relaxation of orbital smooth muscle, choroidal vascular dilation, and aqueous outflow-impeding cycloplegia. Many clinicians avoid using succinylcholine with eye surgery patients; however, pretreatment with a small dose of a nondepolarizing neuromuscular blocking drug, lidocaine, β-blocker, or acetazolamide may attenuate the increase in IOP associated with induction of anesthesia with succinylcholine, direct laryngoscopy, and endotracheal intubation.
Systemic absorption of topical ophthalmic drugs from either the conjunctiva or via drainage through the nasolacrimal duct onto the nasal mucosa can produce untoward side effects. These drops include acetylcholine, anticholinesterases, cyclopentolate, epinephrine, phenylephrine, and timolol ( Table 31.1 ). Phospholine iodide (echothiophate) is a miosis-inducing anticholinesterase that profoundly interferes with metabolism of succinylcholine. Prolonged paralysis after a single dose of succinylcholine may ensue. Phenylephrine drops are available in concentrations of 2.5% and 10%. Systemic absorption via the nasolacrimal duct of 10% phenylephrine drops can induce transient malignant hypertension. Parenteral administration of a long-acting antihypertensive drug may result in untoward hypotension after resolution of the short-acting phenylephrine. Some systemic ophthalmic drugs, such as glycerol, mannitol, and acetazolamide, may also produce untoward side effects.
| Ophthalmic Indication | Drug | Mechanism of Action | Systemic Effect |
|---|---|---|---|
| Miosis | Acetylcholine | Cholinergic agonist | Bronchospasm, bradycardia, hypotension |
| Glaucoma (increased intraocular pressure) | Acetazolamide | Carbonic anhydrase inhibitor | Diuresis, hypokalemic metabolic acidosis |
| Echothiophate | Irreversible cholinesterase inhibitor | Prolongation of succinylcholine's effects Reduction in plasma cholinesterase activity up to 3–7 weeks after discontinuation Bradycardia, bronchospasm |
|
| Timolol | β-Adrenergic antagonist | Atropine-resistant bradycardia, bronchospasm, exacerbation of congestive heart failure; possible exacerbation of myasthenia gravis | |
| Mydriasis, ophthalmic capillary decongestion | Atropine | Anticholinergic | Central anticholinergic syndrome ( mad as a hatter , delirium, agitation; hot as a hare , fever; red as a beet , flushing; dry as a bone , xerostomia, anhidrosis) Blurred vision (cycloplegia, photophobia) |
| Cyclopentolate | Anticholinergic | Disorientation, psychosis, convulsions, dysarthria | |
| Epinephrine | α-, β-Adrenergic agonist | Hypertension, tachycardia, cardiac dysrhythmias; epinephrine paradoxically leads to decreased intraocular pressure and can also be used for glaucoma | |
| Phenylephrine | α-Adrenergic agonist, direct-acting vasopressor | Hypertension (1 drop, or 0.05 mL, of a 10% solution contains 5 mg of phenylephrine) | |
| Scopolamine | Anticholinergic | Central anticholinergic syndrome (see atropine earlier) |
The OCR is a sudden profound decrease in heart rate in response to traction on the extraocular muscles or external pressure on the globe. There is a wide range of reported incidence, varying from approximately 15% to 80%. This reflex occurs more commonly in young patients. The reflex arc has a trigeminal nerve afferent limb that generates an efferent vagal response that may precipitate a variety of dysrhythmias, including junctional or sinus bradycardia, atrioventricular block, ventricular bigeminy, multifocal premature ventricular contractions, ventricular tachycardia, and asystole.
The OCR is most often encountered during strabismus surgery but can occur during any type of ophthalmic surgery. OCR may also occur while performing an ophthalmic regional anesthetic nerve block. Hypercarbia, hypoxemia, and light planes of anesthetic depth augment the incidence and severity of OCR.
Prompt removal of the instigating surgical stimulus frequently results in rapid recovery. Unrelenting tension may induce cardiac arrest, so heart rate must be continuously monitored during eye regional block and surgery. At the first sign of dysrhythmia, surgery must stop and all pressure on the eye or traction on eye muscles discontinued. The ventilatory status and depth of anesthesia should be reassessed. The reflex may extinguish itself after a few minutes; it also can be abated by administration of a parasympatholytic drug such as atropine or glycopyrrolate. The OCR can also be eradicated by an anesthetic eye block, thereby abolishing its afferent arc. Paradoxically, initial placement of a regional block can induce the OCR.
The prophylactic use of intramuscular anticholinergics for adult ophthalmic surgery patients is not recommended, as the tachycardia after atropine or glycopyrrolate may have significant consequences for geriatric patients with coexisting cardiac disease (also see Chapter 26 ). In children (also see Chapter 34 ) who are more dependent on heart rate to maintain cardiac output, prophylactic intravenous administration of atropine (0.01 to 0.02 mg/kg) or glycopyrrolate may be prudent just before commencing eye surgery.
Patients having eye surgery are often at the extremes of age, —ranging from premature babies with retinopathy to the elderly. Hence, special age-related considerations such as altered pharmacokinetics and pharmacodynamics apply (also see Chapter 35 ). The elderly, pediatric patients with various syndromes, and premature infants frequently have multiple comorbid conditions. Preoperative evaluation is vital, but routine laboratory testing is not appropriate. For cataract surgery, in particular, routine testing is associated with a significant increase in health care spending. Physician assessment and judgment determine the need for indicated laboratory testing. Cessation of antiplatelet/anticoagulant drugs before eye surgery is controversial. The risk of intraocular bleeding versus the risk of perioperative stroke, myocardial ischemia, and deep venous thrombosis must be assessed.
One of the most important preoperative assessments is the likelihood of patient movement during surgery. Inability to remain supine and relatively still during intraocular surgery with MAC may result in eye injury and have devastating long-term visual consequences.
Anesthetic options for most ophthalmic procedures include general anesthesia, retrobulbar (intraconal) block, peribulbar (extraconal) anesthesia, sub-Tenon block, and topical analgesia ( Box 31.1 ). Often, there is minimal exposure to regional anesthetic eye block techniques during anesthesia training, creating a reluctance to perform such blocks. Professional societies dedicated to teaching safe ophthalmic regional anesthesia can provide valuable instruction. Site of surgery errors is more common for eye procedures than all other surgeries (except dental and digital). Of prime importance is confirmation of the correct side of surgery (i.e., right eye versus left eye) immediately before anesthesia and surgery.
Safety
Analgesia
Akinesia (when indicated)
Control of intraocular pressure
Avoidance of the oculocardiac reflex
Awareness of possible drug interactions
Awakening without coughing, nausea, or vomiting
The anatomic foundation of needle-based eye blocks rests upon the concept of the orbital cone. This structure consists of the four ocular rectus muscles extending from their origin at the apex of the orbit to the globe anteriorly. These muscles and their surrounding connective tissue form a compartment behind the globe akin to the brachial plexus sheath in the axilla.
A retrobulbar block is performed by inserting a steeply angled needle from the inferotemporal orbital rim into this muscle cone such that the tip of the needle is behind (retro) the globe (bulbar). A more descriptive term is intraconal block ( Fig. 31.1 ). Injection of a small volume of local anesthetic into this compartment will produce rapid onset of akinesia and analgesia.
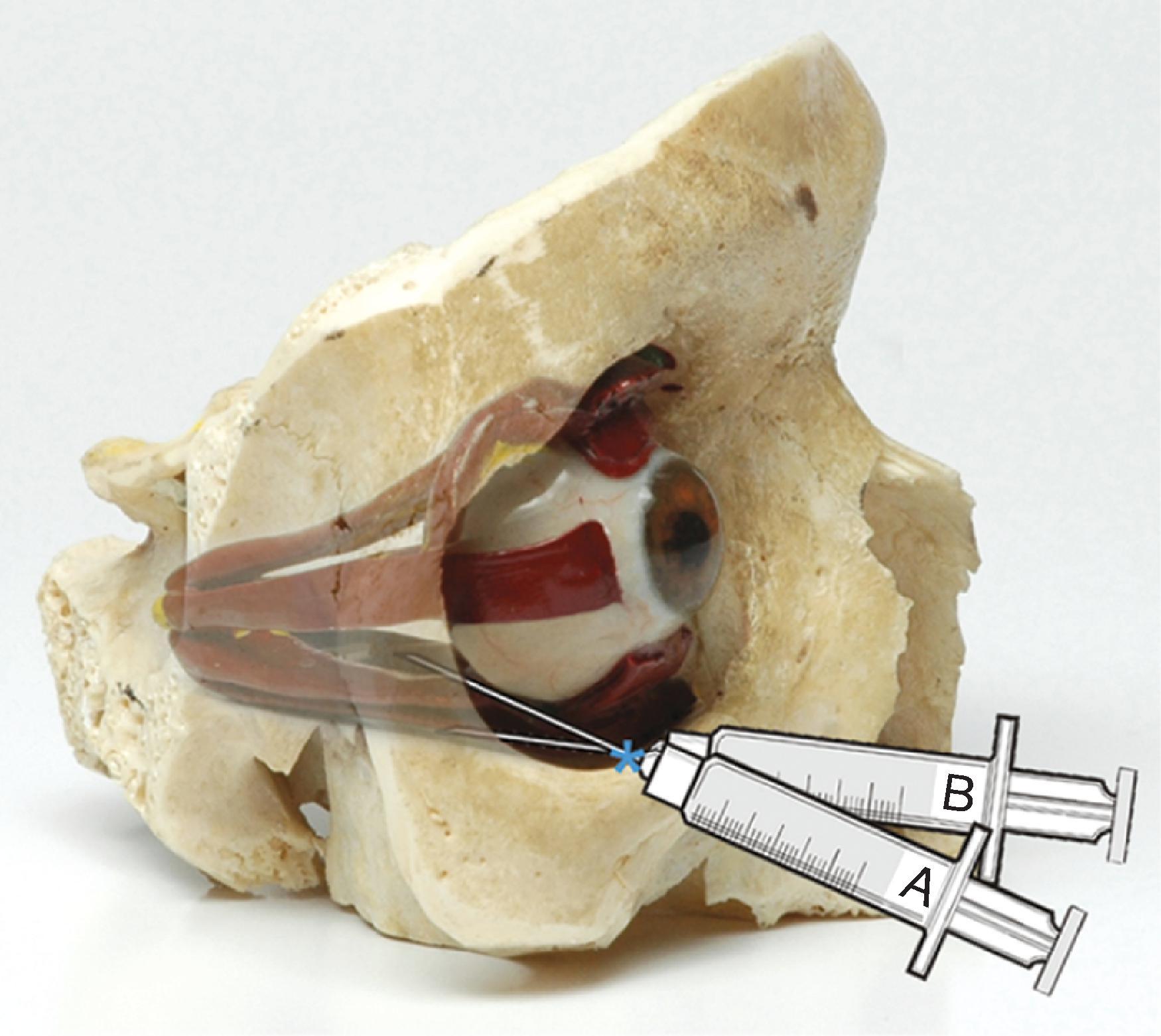
The boundary separating the intraconal from extraconal space is porous, and thus local anesthetics injected outside the muscle cone diffuse inward. A peribulbar block can be achieved by directing a minimally angled needle to a shallow depth such that the tip remains outside the cone (see Fig. 31.1 ). This extraconal block is theoretically safer because the needle is not directed toward the apex of the orbit; hence, the needle tip is ultimately situated farther from key intraorbital structures. This distance minimizes the potential for optic nerve trauma, optic nerve sheath injection, orbital epidural, and brainstem anesthesia. Complications of needle-based eye blocks are listed in Box 31.2 . Because extraconal block local anesthetics are injected at a farther distance from the nerves, larger volumes and more time for diffusion of the local anesthetic are needed. Thus intraconal versus extraconal anesthesia is somewhat analogous to subarachnoid versus epidural anesthesia in terms of volume, onset, and density of block.
Superficial or retrobulbar hemorrhage
Elicitation of the oculocardiac reflex
Puncture of the globe
Intraocular injection
Optic nerve trauma
Seizures (intravenous injection of local anesthetic solution)
Brainstem anesthesia (spread of local anesthetic to the brainstem causing delayed-onset loss of consciousness, respiratory depression, paralysis of the contralateral extraocular muscles)
Central retinal artery occlusion
Blindness
Altered physiologic status after an ophthalmic anesthetic block has important implications. Differential diagnosis includes oversedation, brainstem anesthesia, and intravascular injection of local anesthetic ( Table 31.2 ). Abrupt onset of seizure activity is characteristic of intravascular injection. Convulsions are typically of brief and limited duration. A small dose of induction agent (e.g., propofol) or benzodiazepine may be beneficial. Brainstem anesthesia may have a gradual latency of onset and persist for 10 to 40 minutes or longer. Patients must be continuously monitored after anesthetic eye blocks for signs of oversedation, brainstem anesthesia, and intravascular absorption of local anesthetics.
| Alteration | Oversedation | Brainstem Anesthesia | Intravascular Injection |
|---|---|---|---|
| Loss of consciousness | ± | + | + |
| Apnea | ± | + | ± |
| Cardiac instability | ± | + | ± |
| Seizure activity | Ø | Ø | + |
| Contralateral mydriasis | Ø | ± | Ø |
| Contralateral eye block | Ø | ± | Ø |
Branches of the facial nerve that innervate the eyelid's orbicularis oculi muscle are blocked by the larger volume of local anesthetic used with extraconal injection. This prevents eyelid squeezing and is a distinct advantage during corneal transplantation. An intraconal block requires a separate facial nerve injection to limit blepharospasm.
Ophthalmic anesthesia can also be achieved by instilling local anesthetics through a cannula into the space between the globe's rigid sclera and sub-Tenon capsule ( Fig. 31.2 ). The capsule consists of fascia that envelops the eye, providing a smooth friction-free interface in which to rotate. Anteriorly, it originates near the limbal margin, where it is fused to the conjunctiva. As the capsule extends posteriorly, it surrounds the eye, with portions reflected onto the extraocular muscles. Local anesthetics injected into the sub-Tenon space block ciliary nerves that penetrate the capsule and the optic nerve posteriorly.
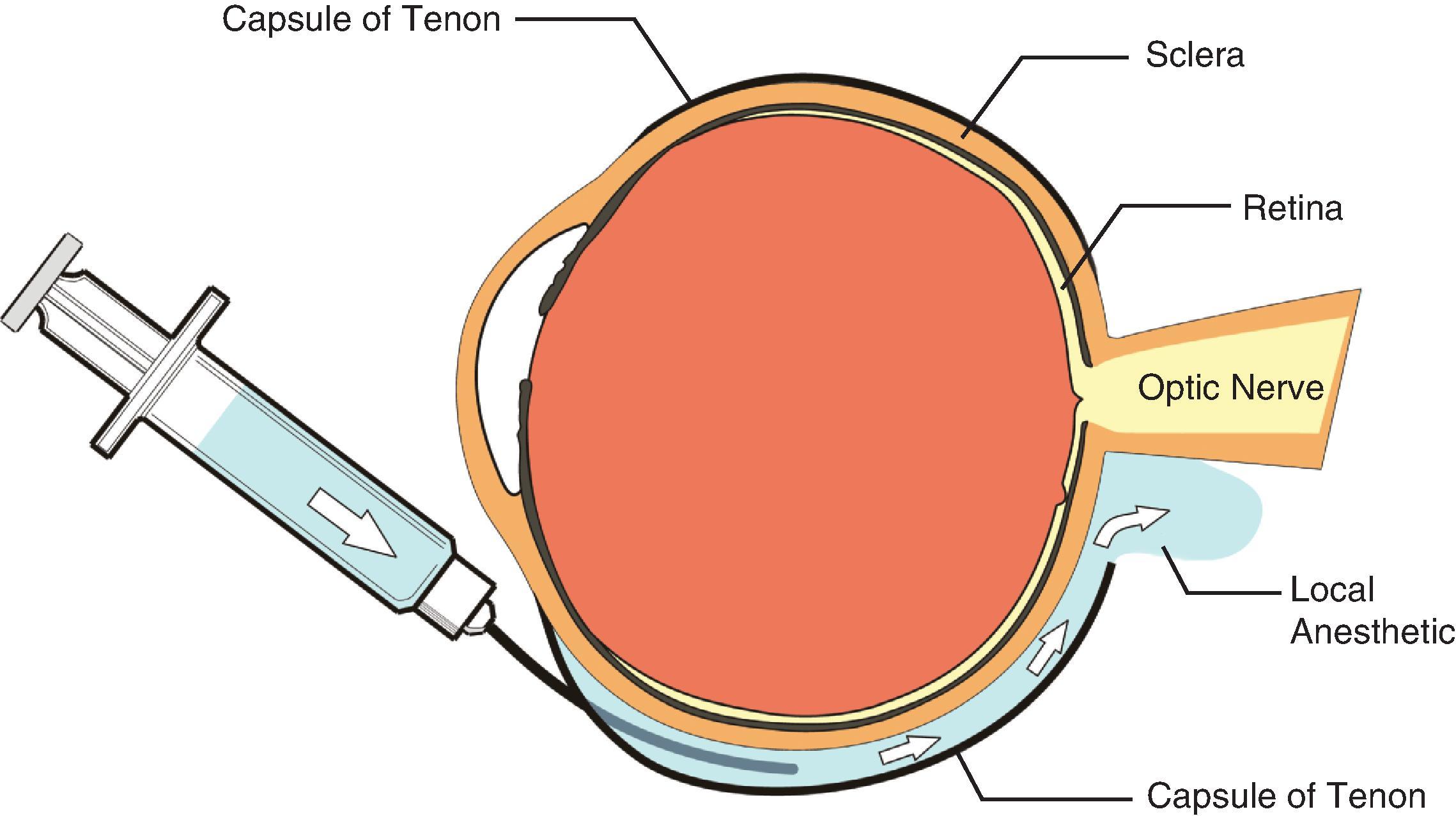
A cannula is introduced into the episcleral (or sub-Tenon) space through a dissection accomplished with blunt scissors. Alternatively, the dissection can be created with a blunt conjunctival probe or by using a blunt-tipped, side-ported rigid cannula.
Topical anesthesia is typically achieved using local anesthetic lidocaine gel. The gel acts as a barrier to antiseptic, so 5% betadine drops are instilled before application of gel. Local anesthetic drops are placed to minimize the astringency of the betadine. Intraoperatively, the surgeon can inject preservative-free local anesthetic into the anterior chamber to supplement anesthesia.
The globe's posterior inner wall is lined by the retina, sensory tissue that converts incoming light into neural output and, ultimately, vision. The densely packed macula near its center provides fine detailed vision. Perfusion comes from the choroid layer situated between the sclera and the retina. The retina may break or detach from the choroid, leading to ischemia and compromised vision. Patients with diabetic retinopathy or extreme myopia are at particular risk. Surgical options include combinations of scleral buckle, vitrectomy, laser, cryotherapy, and injection of intravitreal gas.
Preoperative evaluation of patients with diabetes and coexisting comorbid conditions (also see Chapter 13 ) is important, and appropriate changes should be made to ensure that these patients are in optimal medical condition for surgery. Sudden death during retina surgery can occur because of venous air embolism introduced into the choroid blood flow during the air/fluid exchange portion of vitrectomy. Retina surgery is often prolonged and associated with more extensive manipulation of the eye, therefore requiring general anesthesia or dense regional anesthetic block with MAC. Perfluorocarbons such as sulfur hexafluoride (SF6) and C3F8 are inert, relatively insoluble gases that are injected to internally tamponade the retina onto the choroid. Resorption can take 10 to 28 days depending on which drug is selected. As nitrous oxide is over 100-fold more diffusible than SF6, it can expand the size of the gas bubble, increase IOP, and potentially cause retinal ischemia and permanent loss of vision. Nitrous oxide should be discontinued 20 minutes before gas injection or omitted altogether.
Glaucoma is commonly characterized as a sustained increase in IOP that leads to diminished perfusion of the optic nerve and eventual loss of vision. Various forms of glaucoma exist, each presenting with differing degrees of IOP variation. Terminology can be confusing, resulting in several classifications: acquired versus congenital, high IOP versus normal pressure, acute versus chronic, and open versus narrow or closed angle. Angle-closure (acute) glaucoma occurs when the angle between the iris and cornea narrows and obstructs outflow. Open-angle (chronic) glaucoma results from sclerosis of the trabecular meshwork and impaired aqueous drainage. Outflow is improved with constriction of the pupil by miotic drugs. Administration of atropine drops into the eye produce mydriasis and are contraindicated. Intravenous atropine, on the other hand, is minimally absorbed by the eye and should be used when indicated during anesthesia. Infantile glaucoma may readily progress to blindness, making early surgery more urgent. Congenital glaucoma is often a component of many syndromes, several of which have important anesthesia implications.
Many adult glaucoma procedures can be managed with regional anesthesia and MAC. General anesthesia is requisite for pediatric glaucoma cases. Anesthesia implications include (1) avoiding mydriasis by continuing all miotic drops; (2) understanding the interactions of antiglaucoma medications and anesthetics (see Table 31.1 ); and (3) preventing increases in IOP associated with induction, maintenance, and emergence from anesthesia.
Strabismus surgery is performed to correct misalignment of extraocular muscles and realign the visual axis. Most patients are pediatric (also see Chapter 34 ). Special considerations include (1) frequent incidence of intraoperative OCR, (2) potential increased risk for malignant hyperthermia, and (3) marked prevalence of postoperative nausea and vomiting (PONV).
The incidence of PONV after strabismus surgery varies widely but has been quoted as high as 85%. PONV is the most common reason for pediatric inpatient admission after outpatient surgery and is probably a vagal-mediated response to surgical manipulation of extraocular muscles. Multimodal antiemetics with differing mechanisms of action may be more effective than individual medications for those patients at most risk of PONV after eye surgery.
Strabismus is a neuromuscular disorder that can be associated with other myopathies. The frequency of masseter muscle spasm after succinylcholine is fourfold greater than baseline. Suspect malignant hyperthermia if hypertension, tachycardia, hypercarbia, and increasing temperature occur (also see Chapter 7 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here