Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The pediatrician may be faced with a child who is systemically well or systemically unwell and has a common eye or visual problem, OR a child who is systemically well or unwell with an uncommon eye or visual problem. In the systemically unwell child, the eye findings may well help towards a unifying diagnosis. Assessing the child from an anatomical or structural attitude as well as the child’s neurophysiological and psychophysical visual status is key. While common ocular conditions are important to recognize, the pediatrician must also be aware of certain uncommon ocular conditions that may form part of a syndrome affecting the child.
In this chapter a diagnostic approach to eye conditions is described with the most common conditions discussed first followed by important to know uncommon conditions.
The visual system is conveniently separated into three principal parts: the globe and surrounding structures ( Fig. 20.1 ), the visual pathways, and the visual or calcarine cortex.
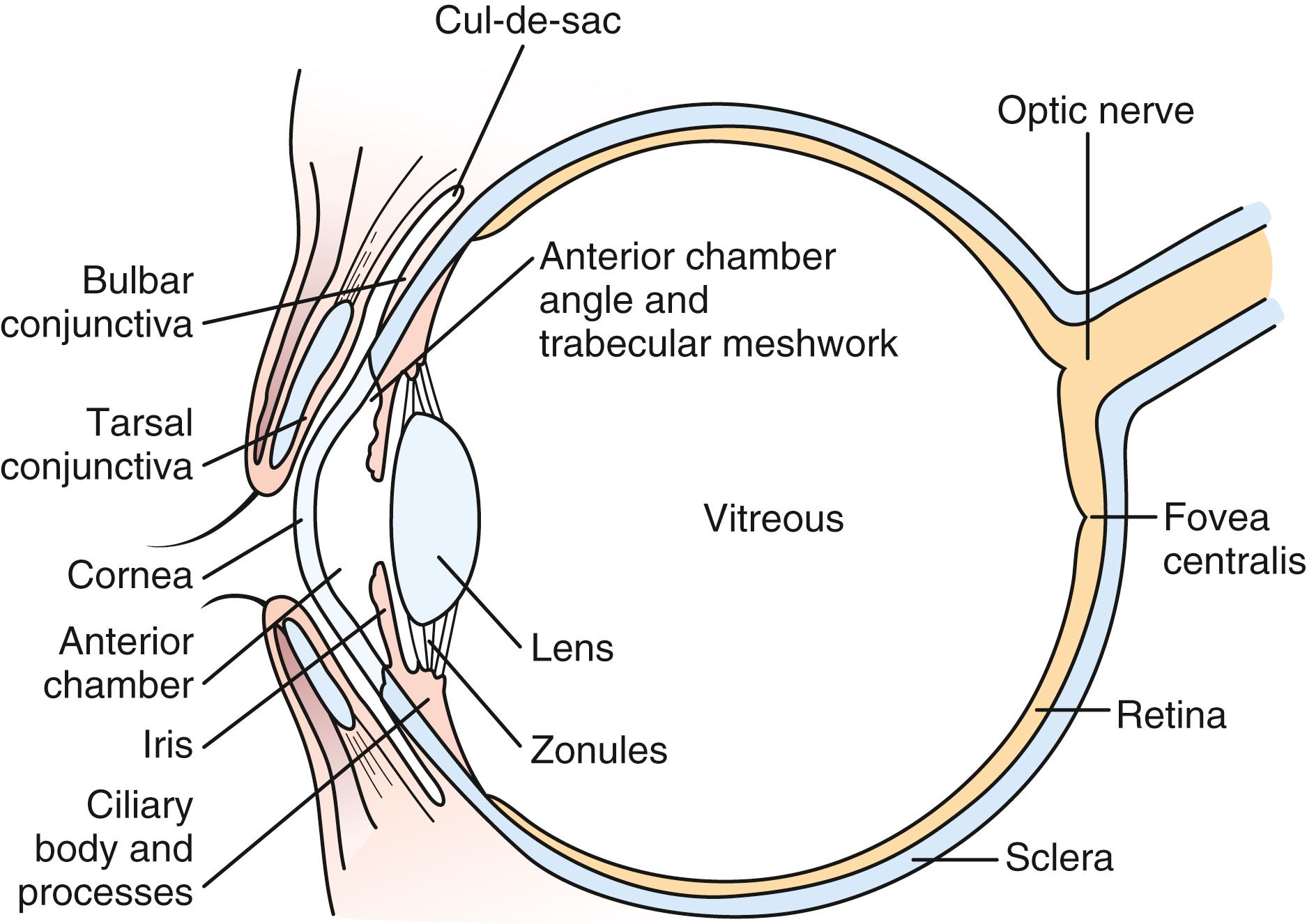
The eyelids provide protection for the globe and assist in even distribution of the tear film over the cornea to provide a clear, undistorted optical surface. The crystalline lens complements the cornea’s refracting power with its ability to adjust the focal length of the optical system so that incoming light from objects at any distance may be clearly imaged on the retina. The process of changing the focal length of the lens is called accommodation. During the first 2 to 3 months of life, children develop the ability to focus on images at any range. Light is focused on the macula, the portion of the retina responsible for the central field of vision ( Fig. 20.2 ).

Accommodation is the ability to rapidly focus from near to distance and vice versa. The retina contains the photoreceptors, rods, and cones, which convert light energy into a nerve response. The fovea centralis is the center of the macula; it has the greatest concentration of cones and is responsible for detailed, color central visual acuity. While central visual acuity is the parameter most commonly measured, visual function includes visual fields, color vision, contrast sensitivity, and visuospatial discrimination.
Nerve fibers emanate from the ganglion cell layer of the retina and coalesce to form the optic nerve. The right and left optic nerves pass from the orbits and decussate at the optic chiasm. Nerve fibers from the nasal retina cross at the chiasm and are directed toward the contralateral side of the brain. Fibers from the temporal retina travel without crossing at the chiasm to the ipsilateral visual cortex ( Fig. 20.3 ). From the optic chiasm, the fibers form the optic tracts and synapse in the lateral geniculate nucleus in the midbrain. From there, the optic radiations, one on each side of the brain, travel posteriorly to the visual cortex above the cerebellum. If an object is seen in the patient’s left half field, the image is received by the nasal retina of the left eye and the temporal retina of the right eye. If the object is seen in the patient’s right half field the image falls on the nasal retina of the right eye and the temporal retina of the left eye. As a result of the decussation of nasal retinal fibers, the right visual cortex receives images from the left half of the visual field and the left visual cortex receives images from the right half.
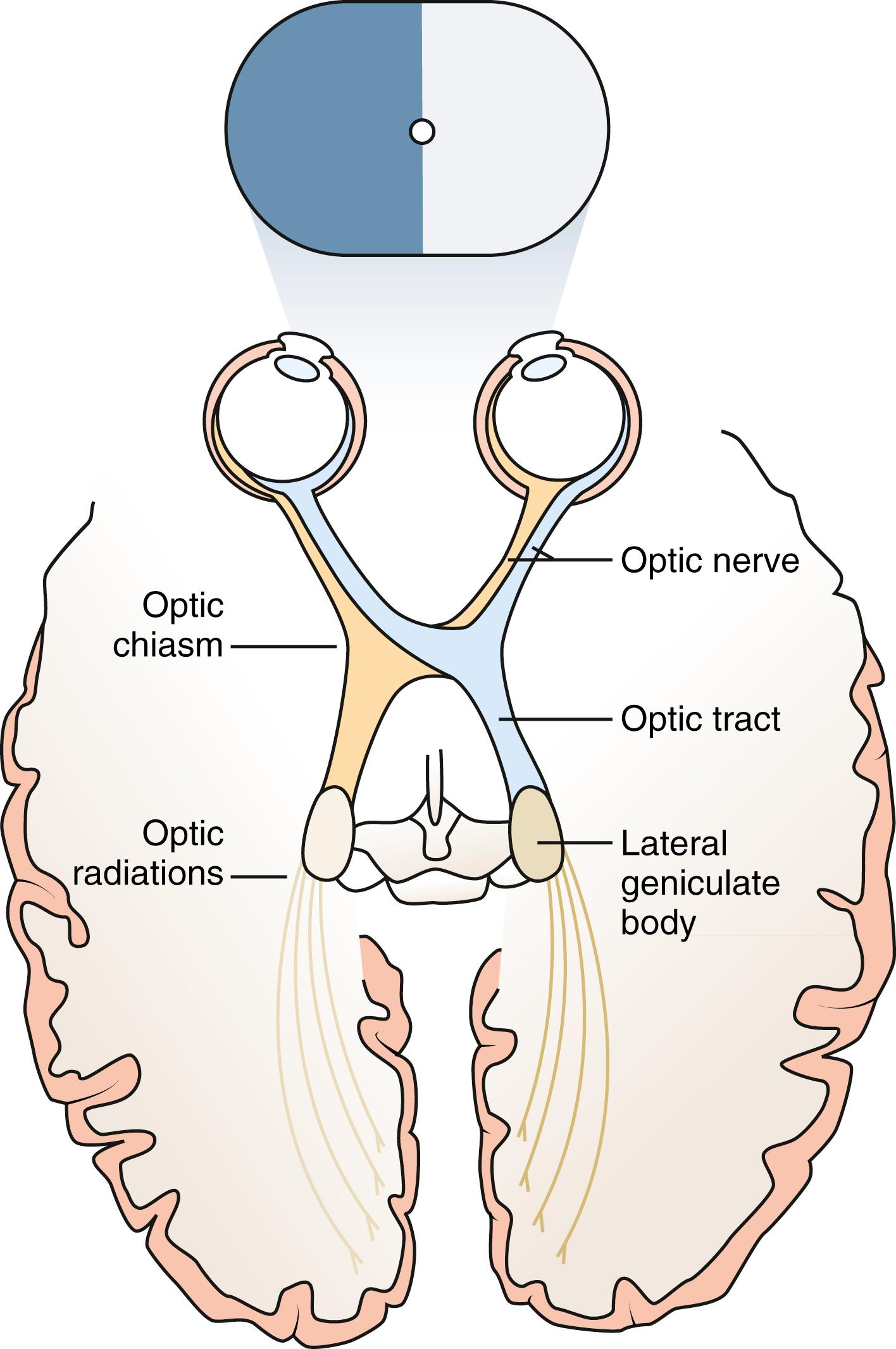
Lesions of the visual pathways can be localized by the pattern of visual field loss (see Fig. 20.3 ).
The visual field can be arbitrarily divided into the central field of vision and the peripheral field. The macula is responsible for the central field and the posterior anterior intraparietal area sub serves the receptive filed from the fovea while the anterior lateral intraparietal area sub serves the receptive filed from the parafoveal areas. A physiologic blind spot is found about 10 to 15 degrees temporal to central fixation and represents the area of the visual field that corresponds to the optic disc. Visual fields may be grossly assessed by a confrontation method, in which the child fixates on the examiner’s nose and is asked to identify the examiner’s fingers held static in the child’s peripheral field; it is better to display fingers in both halves of the field simultaneously so that sensory inattention can also be picked up. An infant or young child’s visual field may also be evaluated by looking for fixation on fingers or objects brought into the peripheral visual field but this phenomenon of fixation shift relies on a complicated and incompletely understood neural network involving the area prostriata, intraparietal sulci, and the temporal occipital cortical areas. Confrontation visual fields are especially valuable in the detection of visual field defects that respect the vertical midline, which are typically caused by neurologic conditions. The visual field can also be formally plotted for each eye in a cooperative child or adult, manually or with an automated visual field device. This test requires steady fixation and concentration. In young children, it is impractical to attempt this tedious measurement; instead, hemifield stimulation using visual evoked potential can be used to detect hemifield problems.
Please refer to Table 20.1 , which shows the development of visual behavior in the first 12 months of life in a term baby. It is important to note that the defensive blink reflex, on average, is not observed until 6 to 8 weeks of age, but the pupil light reaction should be intact by 4 weeks of age.
| Age | 1 Week | 2 Weeks | 3 Weeks | 4 Weeks | 4–6 Weeks | 6–8 Weeks | 3 Months | 6 Months | 9 Months | 12 Months |
|---|---|---|---|---|---|---|---|---|---|---|
| Pupils react to light | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Defensive blink present | N | N | N | N | N | Y | Y | Y | Y | Y |
| Watches familiar face when being fed | N | N | Y | Y | Y | Y | Y | Y | Y | Y |
| Gaze caught and held by dangling bright toy moved in line of vision at 15–25 cm | N | N | N | Y | Y | Y | Y | Y | Y | Y |
| Converges | N | N | N | N | N | N | Y | Y | Y | Y |
| Fix and follows toys at 15–25 cm | N | N | N | N | N | N | Y | Y | Y | Y |
| Reaches out for objects | N | N | N | N | N | N | N | Y | Y | Y |
| Searches for objects that leave visual regard | N | N | N | N | N | N | N | Y | Y | Y |
| Immediately grasps for toys | N | N | N | N | N | N | N | N | Y | Y |
| Watches activity of people/animals at 3–4 m | N | N | N | N | N | N | N | N | Y | Y |
| Interest in pictures | N | N | N | N | N | N | N | N | N | Y |
| Points to objects of interest | N | N | N | N | N | N | N | N | N | Y |
Selection of a test to measure a patient’s visual acuity depends on the patient’s cooperation and level of development. Discussion of visual acuity measurements should include whether the visual acuity has been measured without correction of refractive errors or whether any refractive error present has been corrected with glasses or contact lenses to best visual acuity. To differentiate an organic problem of the visual system from simple refractive error, the best corrected visual acuity provides the most useful information. If correction of the patient’s refractive error with glasses is not available, an approximation of corrected visual acuity can be made by having the patient look through a pinhole. The pinhole prevents indirect rays of light, which need to be refracted by the optics of the eye, from entering the eye, so that the effects of refractive errors in the eye are minimized. Patients demonstrate the pinhole effect when they squint in order to see better. If the patient’s visual acuity improves when looking through the pinhole, a refractive error is present. If it does not improve then there is likely another cause for the decrease in vision.
Visual acuity tests are comprised of both qualitative and quantitative measures.
Qualitative tests include:
Fixation reflex test as mentioned above. This test is used to assess vision in young infants or uncooperative patients. This reflex develops during the first month or two of life. Although almost all 2- to 3-month-old infants can fixate and follow a face or bright object quite well into all fields of gaze, some infants who eventually display normal vision will not display this ability until even 4 to 6 months of age; this occurs because of the complex nature of the underlying neurophysiology of this fixation shift.
Central fixation behavior. If vision is grossly normal, fixation is central, steady, and maintained on objects. If visual acuity is profoundly decreased, the quality of fixation may be wandering in nature, poorly maintained, or eccentric. Central, steady, maintained fixation equates to visual acuity of 20/200 or better. Eyes with unsteady or wandering fixation usually have visual acuity decreased to the 20/800 level ( Fig. 20.4 ).

Quantitative tests
Forced preferential looking: nonverbal infants or children may have their grating visual acuity measured with Teller Acuity Cards (Stereo Optical, Chicago, IL). This test is based on a child’s reflex to move the eyes or head toward a pattern of alternating black-and-white stripes of increasing frequency rather than neutral gray of the same brightness (forced preferential looking).
Vanishing optotypes. The vision testing optotypes (shapes) are constructed with a white band bordered by two black bands, each of half the width of the white band, all on a neutral grey background. The idea is that the average target luminance is equal to that of the grey background. If the target lies beyond the child’s acuity limit, it merges with the grey background, and becomes invisible. The shapes used are all of the same overall size but decreasing in width of white and black bands. The acuity is given by the narrowest white band for which the shape is visible. The principle of the test is that of Preferential Looking—a young child will choose to look towards a target rather than towards a plain stimulus. The test is designed for children 1 to 3 years old but can also be used for older children and adults with developmental delay.
Object recognition cards
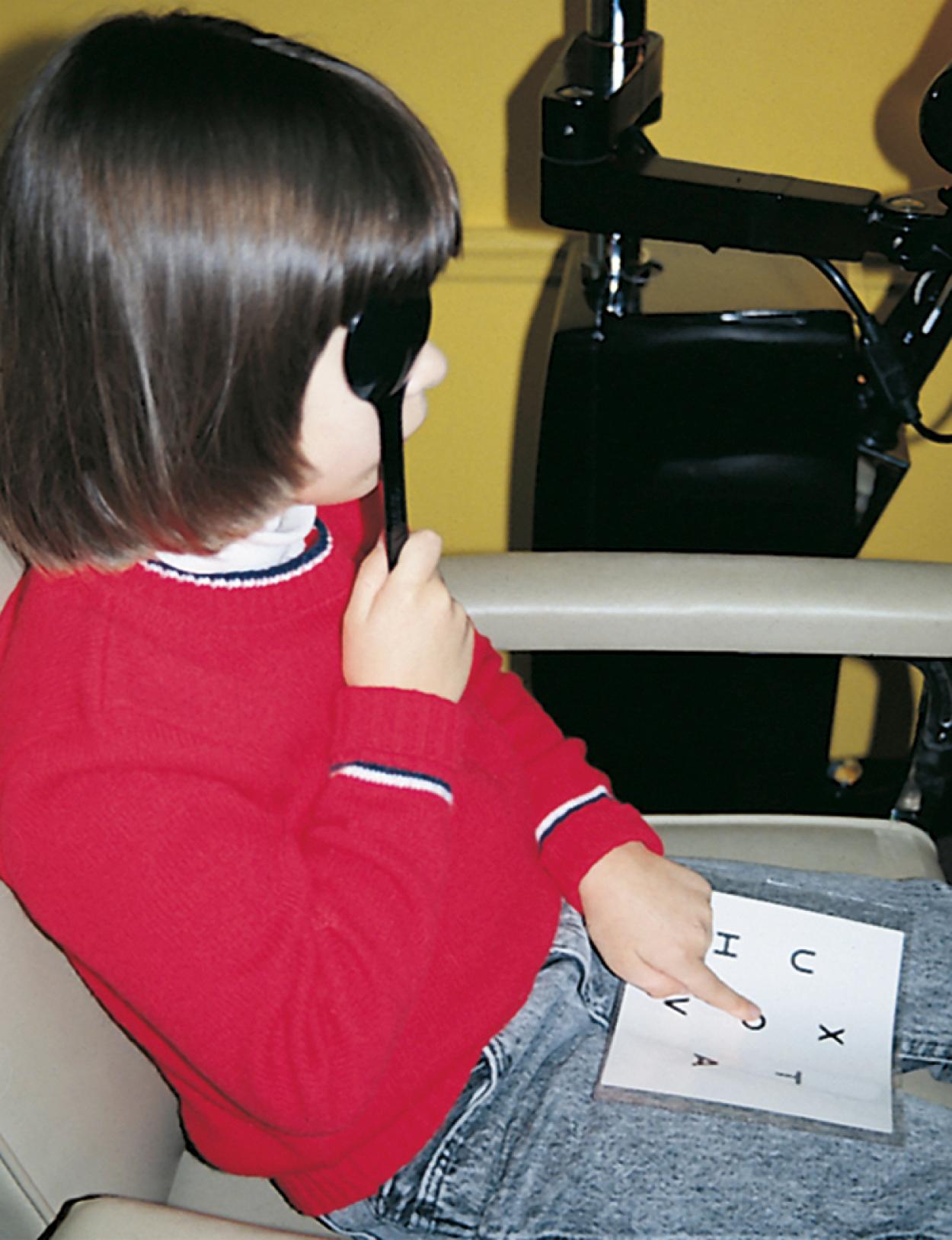
Allen Cards and LEA symbols (Good Lite Company, Elgin, IL), which are simple pictures of common objects, are useful for assessing visual acuity in a 2- to 5-year-old child who cannot comprehend more complicated vision tests, such as the illiterate or tumbling E game, Landolt Cs, or recognize Snellen letters. To measure vision with the Allen cards, the child is taught what the pictures are, and then one eye is occluded and picture cards are individually presented at increasing distances until the patient recognizes the cards at 20 feet or fails to recognize the cards ( Fig. 20.5 ). Recognition of the cards at a distance of 20 feet equates to a visual acuity of 20/30. The farthest distance at which the cards can be recognized is noted, and the visual acuity is quantitated as that distance over the denominator of 30 (e.g., 5/30, 15/30, 20/30). This is a measurement of recognition visual acuity. Although use of isolated targets is not ideal for detection of amblyopia, the test can be quickly and easily taught to apprehensive or shy young children and comparison of vision between the eyes detects most cases of amblyopia and other defects in visual acuity.

The LEA symbols have the advantage of having five symbols on each card, and the child identifies the symbol in the middle of the card. Presentation of several symbols or letters at a time is a more accurate measurement of visual acuity, due to a phenomenon termed crowding. Amblyopic eyes recognize letters or symbols better if they are presented in isolation or one at a time rather than if four or more are presented together on lines above and below one another. The difference may be as much as one or two lines of visual acuity (e.g., 20/30 isolated symbol visual acuity reducing to 20/40 or 20/50 when measured with a Snellen letter chart). Many different visual acuity tests are calibrated using different letters and symbols or groups of symbols ( Fig. 20.6 ).
KAY pictures use different shapes/symbols from LEA symbols and achieve the crowding phenomenon by putting a box around the shape/symbol. They are again designed for the preliterate child. It is easier to use Cardiff cards for intellectually impaired older children or adults rather than either LEA symbols or KAY pictures.
Landolt C and Illiterate E. Other commonly used tests to measure the visual acuity of 3- or 4-year-old children are the tumbling E and Landolt C tests. The child is presented with the letter E or C in decreasing sizes and rotated in an up, down, right, or left orientation, and the child indicates the direction of the crossbars of the E or the open end of the C by pointing.
Visual evoked potentials
The visual pathways coalesce in the visual cortex. Electrical impulses in the visual cortex produced by light stimulation of the retina can be measured by placement of sensitive electrodes on the overlying scalp. This is termed the visual evoked potential or response. The pattern visual evoked potential uses an alternating checkerboard stimulus, which can be controlled to produce a pattern of checks that may be increased or decreased in size. This test can be used to estimate visual acuity in young or nonverbal children. However, caution must be used in interpreting this test, because children and adults with known 20/20 vision can voluntarily suppress the visual evoked response. In addition, children who have significant decreases in their visual acuity may have a visual evoked response that overestimates the visual acuity.
The gold standard for measurement of visual acuity is the presentation of a full line of letter optotypes. This presentation is best achieved with a wall chart or by projection of the letters onto a standardized reflective surface. Other components of vision such as contrast sensitivity, color vision, and color and brightness desaturation can also be assessed to quantify visual function.
Normal values for best corrected visual acuity depend on the patient’s age. A child at 6 months of age should have a visual acuity of 20/60 to 20/100. A child who is 3 years old can be expected to have acuity in the range of 20/25 or 20/30, using the E game or a recognition target test. With further maturation, a 5 to 7-year-old child should have visual acuity of 20/20 to 20/25 as tested with a full-line presentation of Snellen letters. If the best corrected visual acuity is less than 20/20 in a developmentally normal child older than 8 years old, investigation for the cause of the decrease in visual acuity should be made.
In infancy, the fixation and following response of each eye to a fixation target should be recorded. Beginning at age 3, measurement of visual acuity should be completed. Later, a Snellen or letter chart visual acuity test should be performed by the office staff or physician, and the results should be recorded as part of the patient’s medical record. Most importantly, the visual acuity should be equal in both eyes. Further evaluation of a young child is prompted if the patient is cooperating well and the visual acuity is less than 20/40 with letters, or less than 15/30 measured with Allen visual acuity cards, in either or both eyes.
When testing vision in children with nystagmus there are three important points to keep in mind. If the child has a null position, he or she will adopt that position to read the distance and/or the near vison test. You should allow them to do so but also note the head position adopted.
Validated instrument-based vision screening is becoming more widely used in the offices of pediatricians and in the preschool setting. These devices can detect amblyopia, strabismus, and refractive errors and may be used even in infants and nonverbal children but some level of cooperation is necessary and results are generally better after 18 months old. The use of this technology in children before they can have visual acuity measured allows for earlier detection of risk factors for the development of strabismus and amblyopia. There are a number of devices available and also digital apps that can perform the above tasks.
It is recommended that vision screening be conducted as part of well-child care at regularly scheduled intervals in the pediatrician’s or family practitioner’s office. Routine comprehensive eye examinations with an ophthalmologist or optometrist are not cost effective, necessary, or indicated. Low-birth-weight preterm infants, newborn infants with family histories of infantile cataracts or glaucoma, metabolic disease, or children with systemic disease with potential associated ocular disease should be referred to an ophthalmologist for evaluation. Children with immediate family histories of strabismus or amblyopia should be watched carefully for strabismus and referred promptly. Because of the increased risk in these children, referral for comprehensive examination should be considered between 18 and 30 months old. Children suspected by their parents or teachers of having reading or learning problems should have eye examinations performed with an emphasis on an evaluation of the amplitude of accommodation and the facility of accommodation. While we are aware that by the time we reach approximately 45 years, it becomes harder to read things close (presbyopia), this can sometimes happen in children between 5 to 15 years. Recognizing this means that often a temporary use of bifocal glasses or reading glasses corrects the issue. Classically these children jump lines when they are reading, lose concentration very easily, and their handwriting becomes untidy, as does their ability to color in within the lines. A dynamic retinoscopy done by a pediatric ophthalmologist or optometrist will pick this condition up.
Some states have legislation in place that requires vision screenings be performed prior to entry into school or in school at 1- to 2-year intervals. In a child 6 years old or older, referral to an ophthalmologist is indicated if the vision is less than 20/30 in either eye. If appropriate vision screenings are passed in the primary care physician’s office, preschool, or school and no family history of hereditary eye disease or other suspicion or risk factor for eye disease are present, comprehensive examination of the child’s eyes by an optometrist or ophthalmologist is not cost effective and not recommended.
Decreased visual acuity is most commonly the result of a refractive error in the eye. This may be due to variation in the curvature of the cornea, shape of the lens, or variation in the axial length of the eye. Determination of the refractive state of the eye is part of a comprehensive ophthalmic evaluation. In children, an objective measurement of the refractive error is best obtained by using eye drops that temporarily inhibit accommodation (cycloplegia) and cause pupillary dilation (mydriasis). Cycloplegic/mydriatic agents such as cyclopentolate or tropicamide are instilled, and 30 minutes later the pupil is dilated and accommodation is temporarily paralyzed. Retinoscopy is performed by using a retinoscope to project a beam of light into the eye and illuminate the retina. The light is then reflected back to the examiner through the optical system of the eye. The focus of the reflected light is neutralized by placement of appropriate lenses in front of the eye, and the refractive error of the eye is accurately and objectively measured ( Fig. 20.7 ). Refraction can also be measured by devices called auto-refractors, and some vision screening devices are based upon refraction technology and will give refraction measurements.

Low levels of hyperopia (farsightedness) in the range of +1.50 to +2.00 diopters (D) are normal during childhood and are easily compensated for by the focusing mechanism of the lens (accommodation), so glasses are not necessary. The amount of hyperopia normally increases until 5 years old and then decreases. Under normal circumstances, emmetropia, or no refractive error, is achieved around adolescence. If excessive axial growth, elongation, of the eye occurs, myopia (nearsightedness) develops. A patient’s refractive error is for the most part genetically predetermined. The effect that environment has on refractive error is not completely understood.
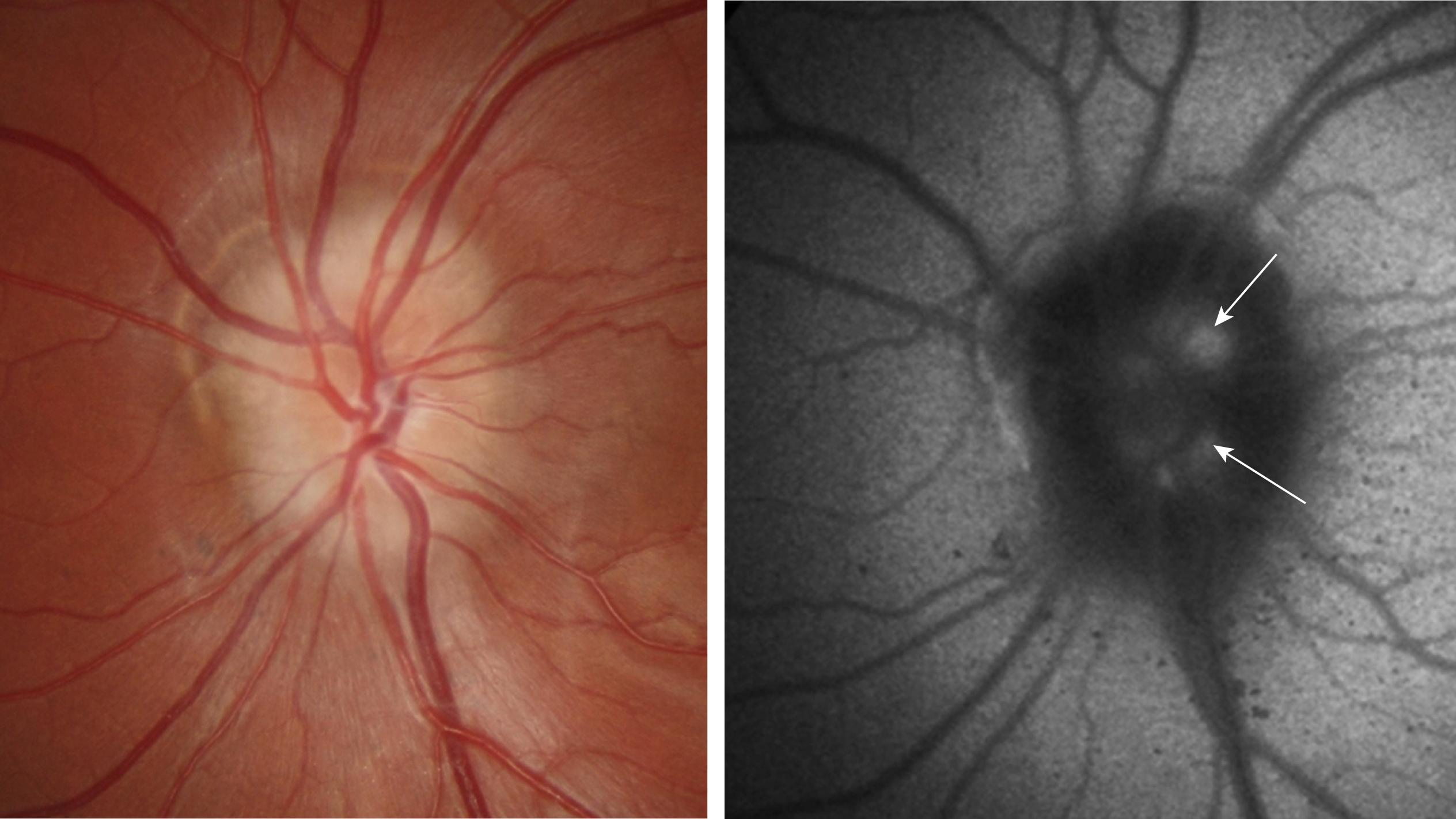
The optical image formed by a hyperopic eye is in focus behind the retina ( Fig. 20.8C ). By changing the shape of the lens with accommodation, the image can be brought into focus on the retina and glasses may not be required. If a large amount of hyperopia is present (+4.00 D or more), fatigue; headaches; asthenopia; and blurring of vision, especially at near, may occur. Hyperopia more than +5.00, or +6.00 D may cause ametropic or refractive amblyopia. When this occurs, glasses are prescribed to correct the child’s refractive error so that focused images stimulate the development of normal vision. If large hyperopic refractive errors are not treated by 6 to 8 years old, the resultant amblyopia may be irreversible. There is also some evidence to suggest that uncorrected high hyperopia may be associated with delays in the development of reading comprehension. The optic discs in eyes with large degrees of hyperopia may have an appearance simulating papilledema (pseudopapilledema) ( Fig. 20.9 ).
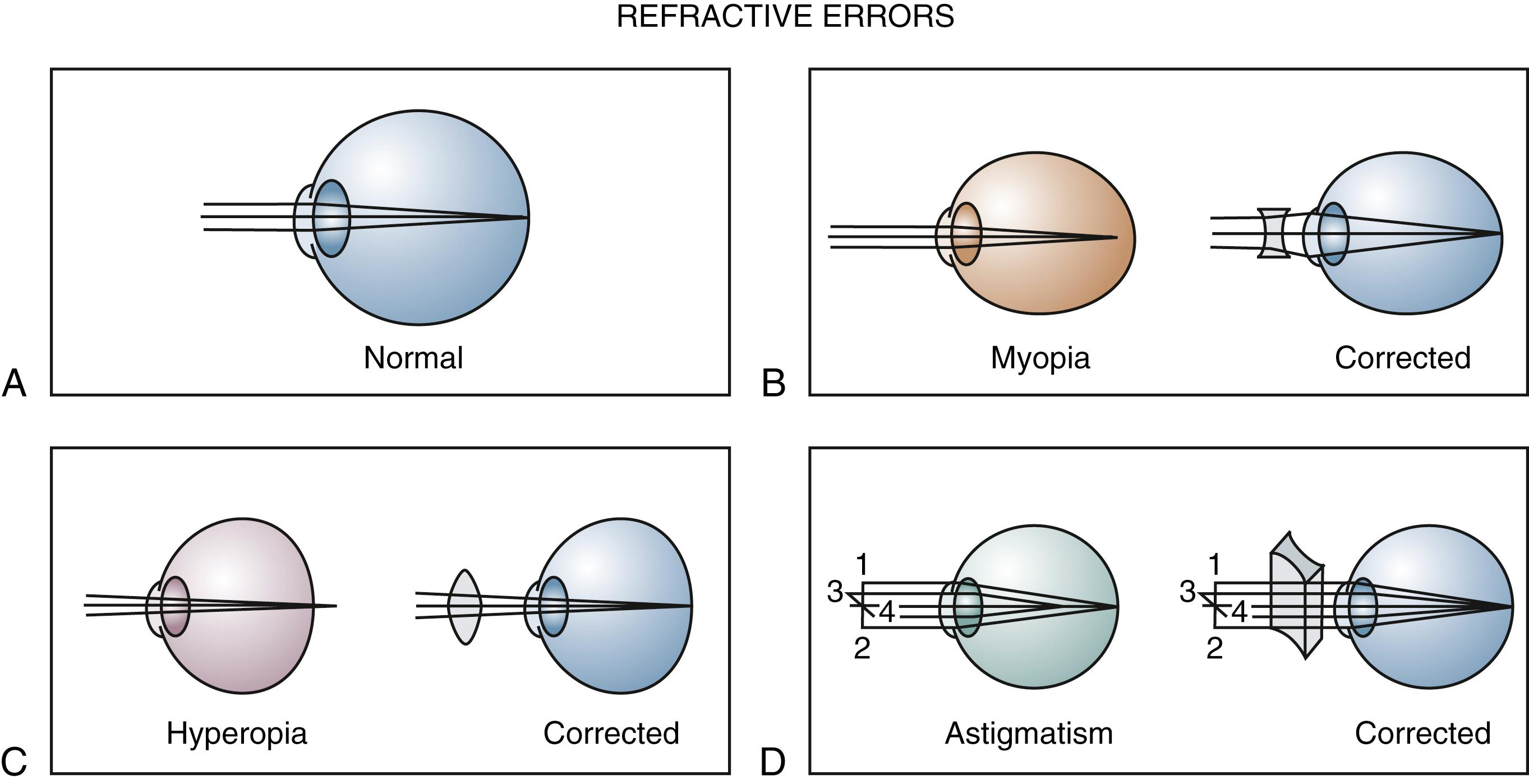
Myopia is most commonly caused by an increase in axial length of the eye with respect to the optical power of the eye ( Fig. 20.8B ). Children who are myopic can see near objects clearly; objects at distance are blurred and cannot be brought into focus without the aid of glasses or a contact lens. Wearing glasses for myopia does not change the growth of the eye and, contrary to popular belief, does not promote the resolution or progression of the myopia.
Myopia may be present at birth but usually develops with growth spurts that occur between 8 and 10 years old. The amount of myopia present usually increases until growth is completed after adolescence. Myopia is inherited as a multifactorial trait.
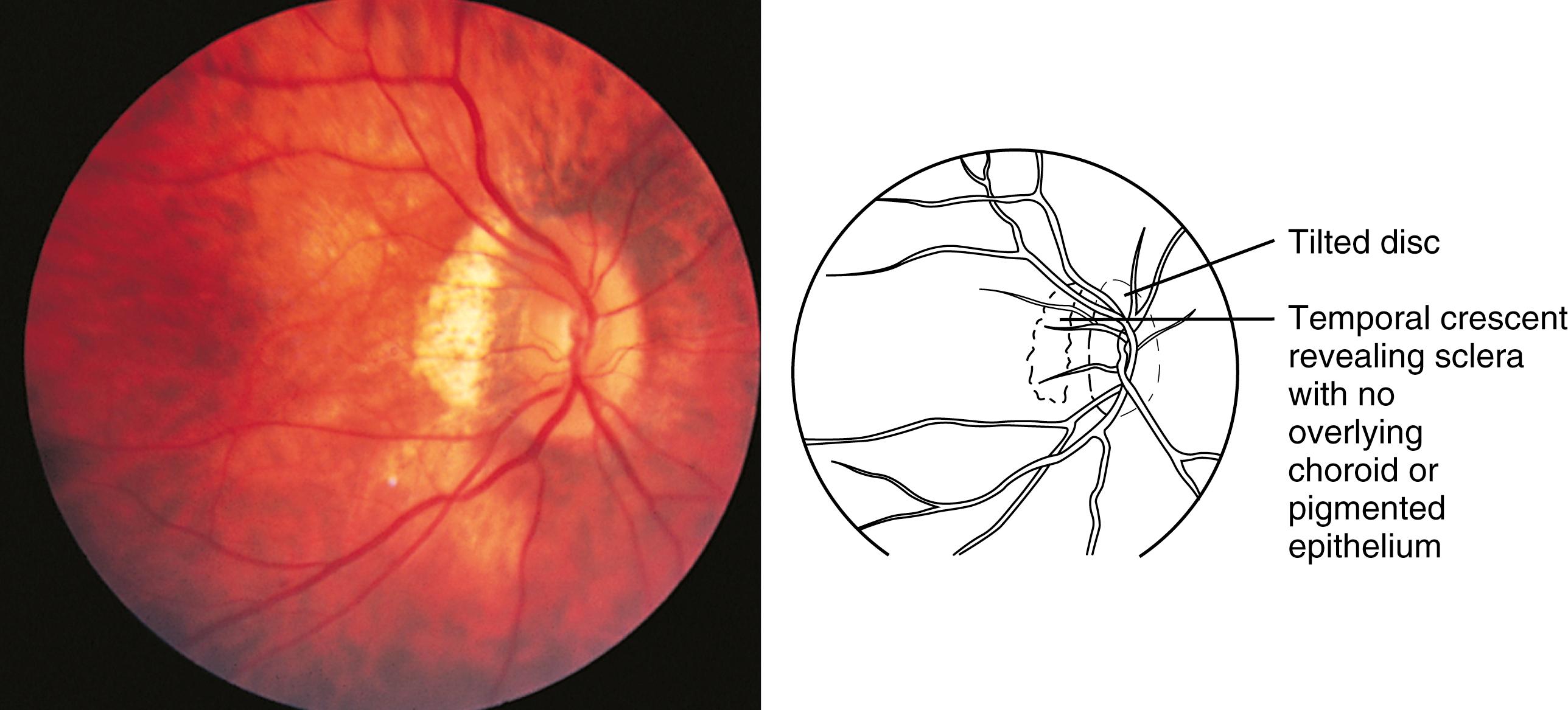
High degrees of myopia, with increased axial length of the eye, ranging from −8.00 to −20.00 D may occur in isolation or be associated with systemic conditions. Causes of high or early onset moderate myopia include connective tissue disorders such as Marfan, Ehlers Danlos, and Stickler syndromes. Children with high myopia should be referred to a pediatric ophthalmologist to rule out pathology to explain the high myopia. Retinal disorders such as sequelae of retinopathy of prematurity (ROP), familial exudative vitreoretinopathy (FEVR) and retinal dystrophies most commonly congenital stationary night blindness (CSNB) can cause high myopia; however, these are usually associated with nystagmus. Rarely, juvenile glaucoma may present as early onset myopia. Retinal thinning, peripapillary pigment crescents, staphylomas (a focal area of bulging of the posterior globe wall), and decreased macular function with poor visual acuity may all be present in patients with high myopia. The optic nerve may appear to enter the eye at an angle ( Fig. 20.10 ). Patients with high myopia have an increased risk for retinal detachment, especially after direct trauma to the eye or concussive head trauma.
In astigmatism, the refractive power of the eye is different in different meridians (see Fig. 20.8D ). This produces a blurred retinal image for objects at both distance and near. Astigmatism occurs when the cornea, lens, or shape of the globe has a toric shape, like the surface of a football, rather than a spherical one. Bulky masses in the lids (such as chalazions or hemangiomas) may compress the cornea and induce astigmatic refractive errors.
Myopia affects 85% to 90% of young adults in some Asian countries such as Singapore and Taiwan, and between 25% and 50% of older adults in the United States and Europe. Unlike Western populations where the prevalence of myopia is low (<5%) in children aged 8 years or younger, in Asian children there is a significantly higher prevalence of myopia, affecting 9% to 15% of preschool children, 24.7% of 7-year-olds, 31.3% of 8-year-olds, and 49.7% of 9-year-old primary school children in Singapore. In 12-year-old children, the prevalence of myopia is 62.0% in Singapore and 49.7% in Guangzhou, China compared with 20.0% in the United States, 11.9% in Australia, 9.7% in urban India and 16.5% in Nepal. With increasing myopia, there is a significantly increased odds ratios for myopic maculopathy, retinal detachment, cataracts, and glaucoma, even for low and moderate levels of myopia. These odds ratios increase further with higher levels of myopia.
Evidence supports heritability of the nonsyndromic forms of myopia, especially for high-grade myopia (−5 D or higher), and genome-wide association studies (GWAS) have identified greater than 20 associated loci for myopia. There has been much interest recently to try and retard myopic progression of childhood.
In overnight orthokeratology, the patient wears reverse geometry contact lenses overnight to temporarily flatten the cornea and provide clear vision during the day without any glasses or contact lenses. Reduction in myopia (up to −6 D) is achieved by central corneal epithelial thinning, midperipheral epithelial, and stromal thickening. Unfortunately, more than one hundred cases of severe microbial keratitis related to orthokeratology have been reported since 2001. There is no good controlled long-term study demonstrating sustained myopia control effect and there is no washout data.
While accumulating evidence for the role of the peripheral retina in the development of refractive errors with initial human studies involving mainly Caucasians suggests an association between relative peripheral hyperopia and axial myopia, the Peripheral Refraction in Preschool Children (PREP) Study of Singaporean Chinese children and Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study showed that relative peripheral hyperopia had little consistent influence on the risk of myopia onset, myopia progression, or axial elongation.
There has been great interest in the use of topical atropine. Atropine blocks muscarinic receptors nonselectively. Muscarinic receptors are found in human ciliary muscle, retina, and sclera. Although the exact mechanism of atropine in myopia control is not known, it is believed that atropine acts directly or indirectly on the retina or sclera, inhibiting thinning or stretching of the sclera, and thereby eye growth. Studies have shown some clinical effect on slowing the progression of myopia in children. The Atropine for the Treatment of Myopia studies (ATOM 1 and 2) were randomized, double-masked, placebo-controlled trials involving 400 Singapore children in each study. The ATOM 1 study suggested 1% atropine eyedrops nightly in one eye over a 2-year period slowed myopic progression by 77% and reduced the axial length elongation (mean axial length increase of 0.39 mm in controls versus no growth in the atropine group). The ATOM 2 study demonstrated a dose-related response with 0.5%, 0.1%, and 0.01% atropine slowing myopia progression by an estimated 75%, 70%, and 60% with spherical equivalent (SE) changes of 0.30 D, 0.38 D, and 0.48 D, respectively over 2 years. However, when atropine was stopped, there was an inverse increase in myopia, with rebound being greater in the children previously on higher doses. This resulted in myopia progression being significantly lower in children previously assigned to the 0.01% group at 36 months compared with that in the 0.1% and 0.5% groups. Younger children and those with greater myopic progression in year 1 were more likely to require retreatment. By the end of 5 years, myopia progression remained lowest in the 0.01% group. It was estimated that, overall, atropine 0.01% slowed myopia progression by at least 50%. The efficacy of lower dose atropine is corroborated by Taiwanese cohort studies. However, there may be children who are poor responders to atropine. In ATOM 1, 12.1% of children (younger, with higher myopia, and greater tendency of myopic progression) had myopia progression of more than 0.5 D after 1 year of treatment with atropine 1%. Atropine 0.01% caused minimal pupil dilation (0.8 mm), minimal loss of accommodation (2 to 3 D), and no near visual loss compared with higher doses. Children on atropine 0.01% did not need progressive additional lenses.
The notion that at least 2 hours daylight exposure can be preventive against myopic progression of childhood has gained favor and in some countries is influencing the design of classrooms to increase daylight exposure while indoors.
Anisometropia refers to the condition in which one eye has a different refractive error than the other. Usually the eye with the least amount of hyperopia or refractive error is the dominant or preferred eye. The fellow eye may be suppressed and develop amblyopia because the development of the visual system is being stimulated by a sharp focused image from one eye and a less focused image from the other eye. The magnitude of the amblyopia depends on the magnitude of the anisometropia and the age at which it developed. Anisometropia may occur with hyperopia, myopia, astigmatism, or a combination of these refractive errors. If the degree of anisometropia is large, the optical properties of the required correcting lenses produce a difference in image size between the two eyes, aniseikonia, which may be difficult for the patient to tolerate. The risk of amblyopia exists in children up to the age of 8 years; the younger the amblyogenic insult starts, the greater the amblyopia if left untreated.
Misalignment of the visual axes is referred to as strabismus. Strabismus occurs in 1% to 4% of the population and may be congenital or acquired. It may occur on a hereditary basis, most commonly without a clearly defined inheritance pattern. In the majority of childhood strabismus, the misalignment of the eyes is not caused by a specific cranial nerve or extraocular muscle dysfunction; however, cranial nerve paralysis and neuromuscular disorders (myasthenia gravis) may be the cause in some cases.
Voluntary and reflex movements of the eyes occur via the action of the extraocular muscles. These muscles are coordinated in their saccadic and pursuit movements by centers in the frontal and occipital areas of the cerebral cortex with modification by the cerebellum. Saccades are voluntary movements used to move the eyes to the object of regard. These are rapid eye movements. Pursuit or following movements are used to track or follow moving objects. These are slow eye movements.
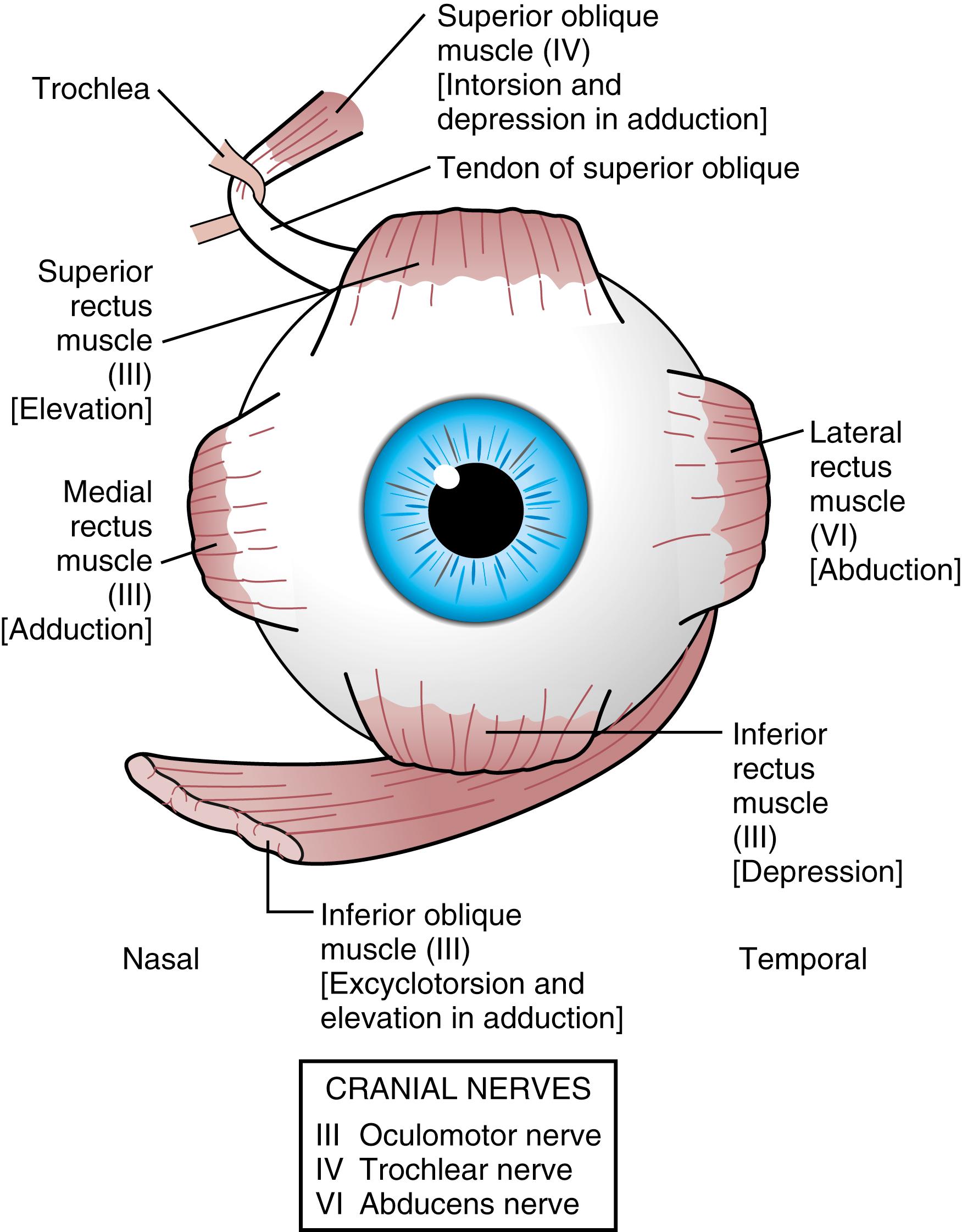
The third, fourth, and sixth cranial nerve nuclei, located in the brainstem, are the centers responsible for innervating the extraocular muscles. In addition to innervation of the inferior oblique, medial, inferior, and superior recti, the third cranial nerve is responsible for innervation of the levator muscle, pupillary constrictor, and ciliary muscle, which is responsible for changing the shape of the lens that produces accommodation. The fourth cranial nerve provides innervation to the superior oblique muscle, and the sixth cranial nerve supplies the lateral rectus muscle ( Fig. 20.11 ). When one or more of the cranial nerves are paretic, the action of the innervated muscle is decreased, leading to a deficit in the duction or movement of the eye into the field of action of the muscle. The muscle having a function of movement in the opposite direction is no longer balanced, producing misalignment of the eye or strabismus.
Eye movements are tested by moving the eyes right, left, up, down, up and right, down and right, up and left, and down and left. These test the function of each extraocular muscle and its counterpart or yoke muscle in the fellow eye. Versions refer to movement of both eyes together in conjugate gaze. A duction is the movement of a single eye. Normal version movements should be present by 4 months of age.
Vergence movements consist of convergence or divergence of the eyes. Vergences are well established by 6 months of age. Convergence of the eyes, coupled with accommodation and miosis of the pupil, is referred to as the near response. Convergence assists alignment of the eyes at near.
A strabismus deviation that changes in size or magnitude in different gaze positions is termed incomitant. Strabismus deviations that remain the same in all gaze positions are termed comitant. An important distinction is that incomitant deviations may be, but are not always, an indication of cranial nerve paralysis.
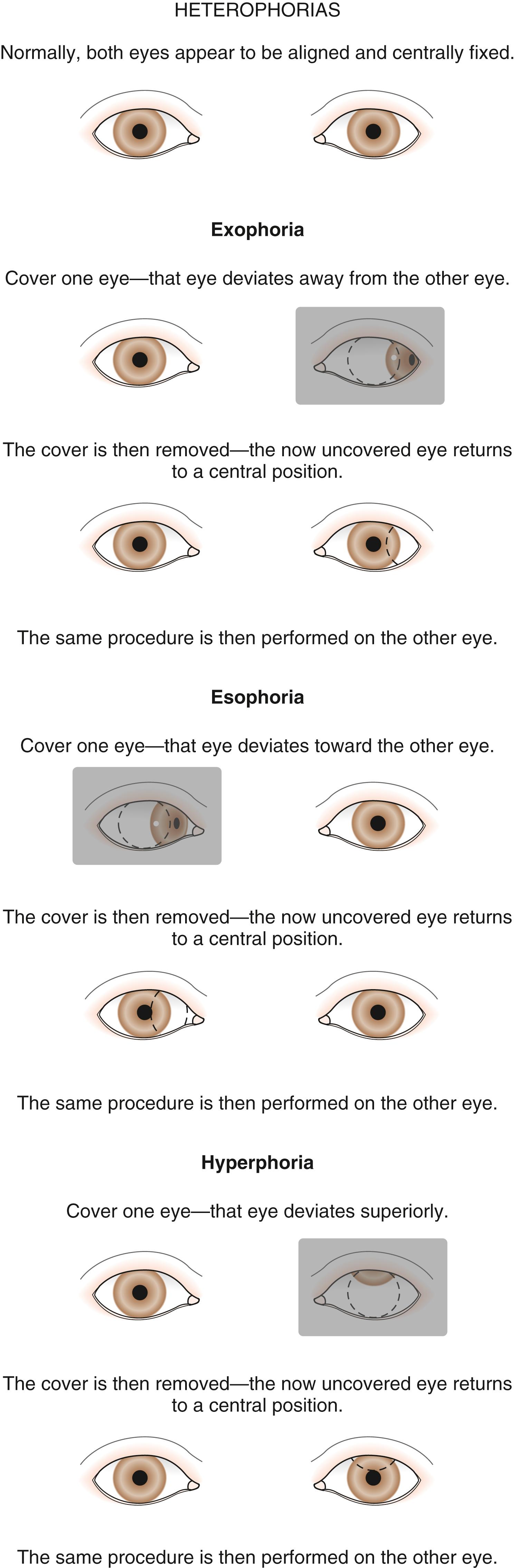
If strabismus is present, it may be manifest (i.e., a tropia) or held latent by sensory fusion (i.e., a phoria). Fusion is the patient’s unconscious desire to use both eyes together for binocular vision. When the fusion of a patient with a phoria is interrupted by placing an occluder in front of one eye, the eye seeks its position of rest and deviates so that the visual axes of the two eyes are no longer both aligned on the point of fixation. When the eye is uncovered and binocular vision is reestablished, the fusion response assists in the realignment of the eyes on the object of regard. A phoria may produce symptoms of fatigue, blurring, or straining to see. When a phoria breaks down into an intermittent tropia, there may be a symptom of intermittent double vision or diplopia. Phorias, especially if large, may become symptomatic at times of fatigue, stress, or illness.
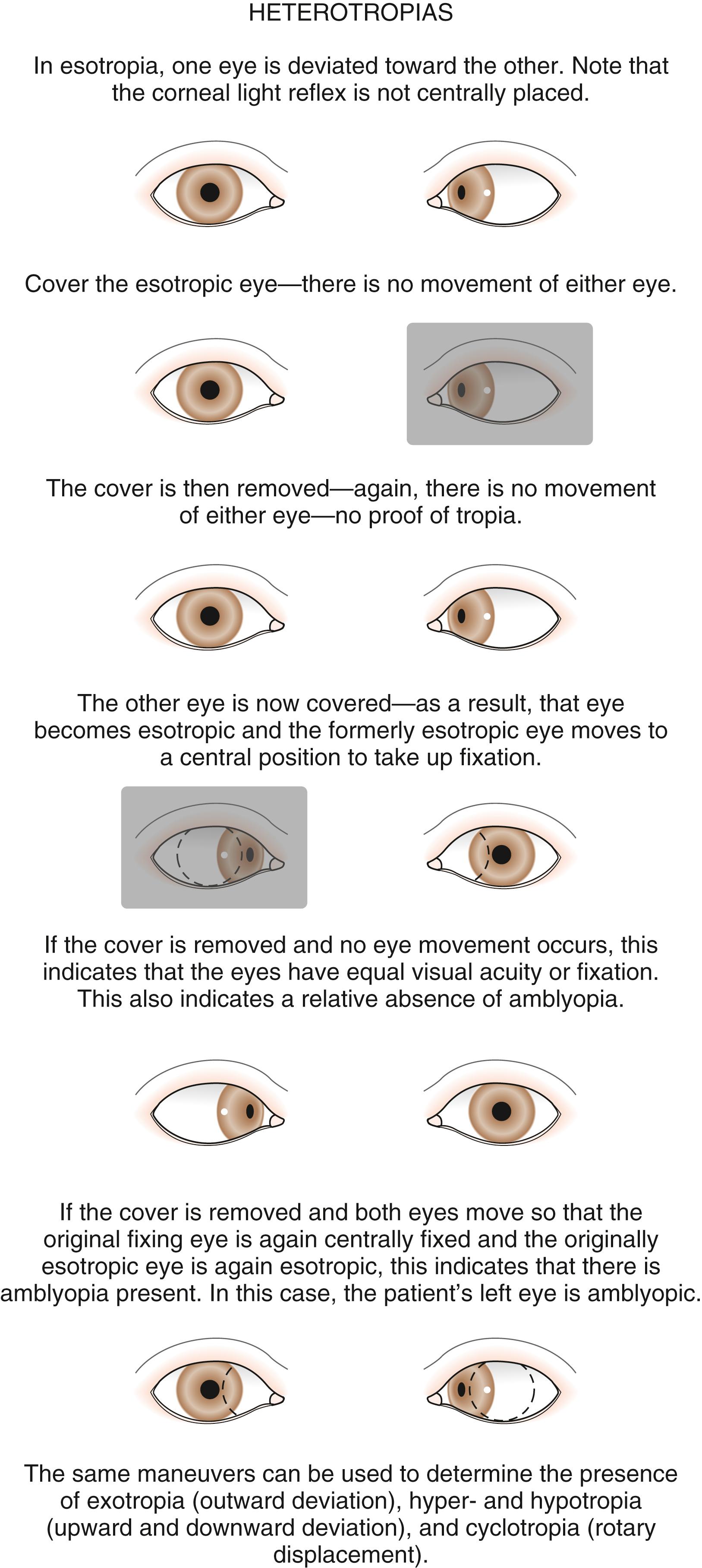
A tropia is a constant or intermittently present ocular deviation. The fusion mechanism is unable to maintain alignment of the eyes. Young children with tropias develop suppression of the tropic eye as an innate response to avoid diplopia. Older children or adults who acquire a tropia (e.g., from an acquired cranial nerve palsy) have diplopia as a symptom of the misalignment of their eyes. The deviation present in a tropia may occur in one or all positions of gaze, depending on the cause of the tropia.
Phorias and tropias are classified according to the pattern of the eye deviation. The prefixes eso- and exo- classify horizontal strabismus. Hyper- and hypo- are used for vertical deviations, and incyclo- and excyclo- are used for torsional deviations.
An esodeviation is a convergent or crossing deviation of the eyes. The deviation may be latent, a phoria (esophoria), or it may occur as a manifest deviation, a tropia (esotropia). Common esodeviations seen in children are infantile esotropia, accommodative esotropia, esotropia resulting from sixth cranial nerve palsy, and Duane syndrome.
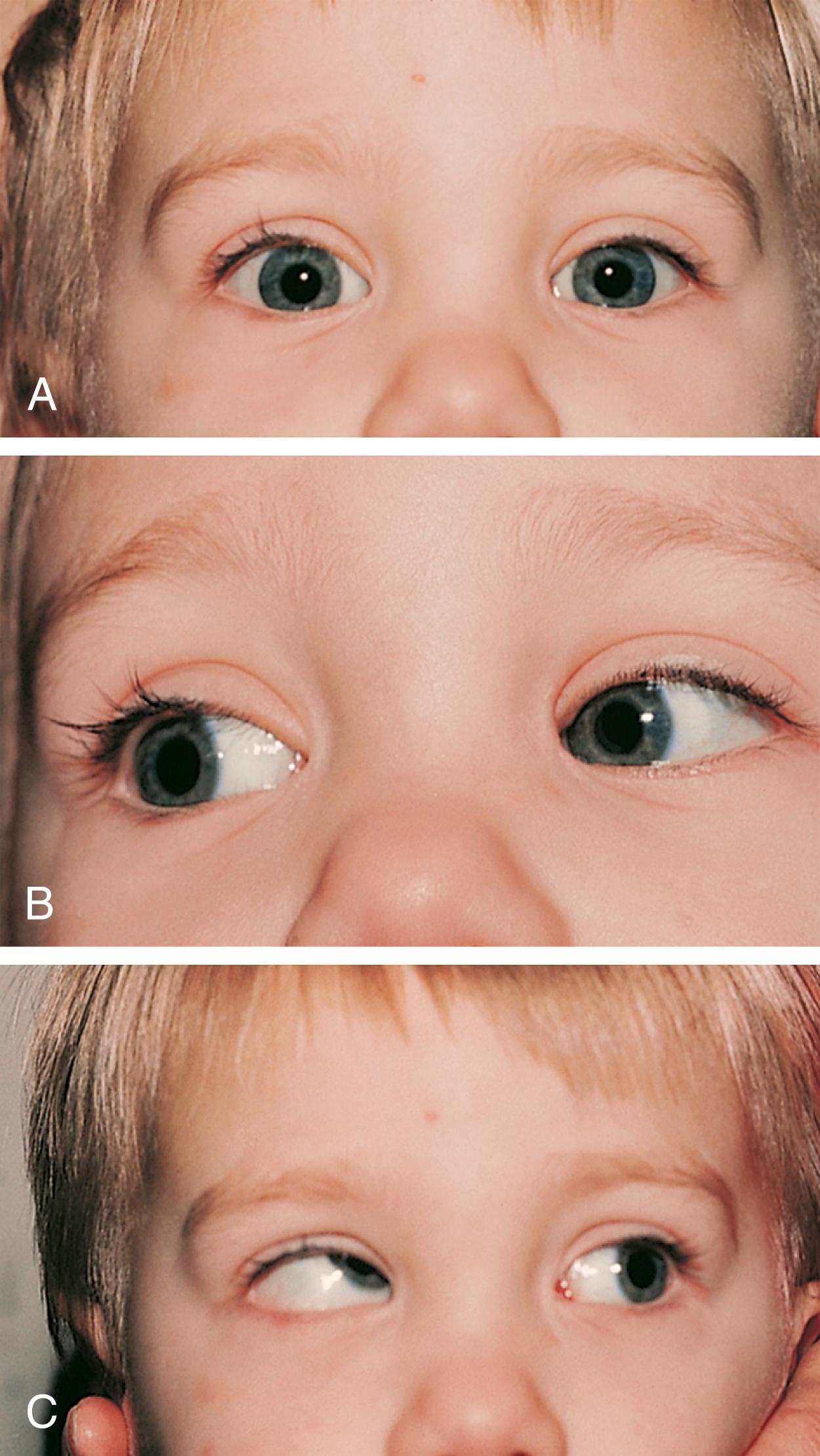
The most common cause for an esodeviation presenting in infancy is infantile, or congenital, esotropia ( Fig. 20.12 ). In this condition, the esotropia is seen at birth or very early in infancy. On occasion, a family history of infantile esotropia exists. The angle of esodeviation is large and constant. Abduction may be deficient due to contraction of the medial rectus muscles, and differentiation from sixth nerve palsy may be difficult. Cross-fixation is usually present, with the adducted right eye used for vision to the left and the adducted left eye used for vision to the right. Abduction of an eye is checked by holding the head, occluding the contralateral eye, and quickly encouraging fixation movements. Doll’s head maneuvers may also be used to test abduction of the eyes. Children with this condition usually do not develop much amblyopia and maintain good visual acuity in both eyes, due to their use of cross-fixation, whether they are treated or not. There are no associated neurologic or systemic abnormalities.

The esodeviation present in infantile esotropia requires surgical correction. After correction, the ocular alignment is frequently unstable, with further surgery not infrequently required later in life, regardless of how early surgery is performed or how well aligned the eyes are after surgery. Inferior oblique overaction and dissociated vertical deviations (DVDs) frequently develop later in childhood or adolescence. Inferior oblique overaction is seen as an elevation of one or both eyes in adduction. A DVD ( Fig. 20.13 ) is an upward and outward “floating” movement of one or both eyes that becomes more prominent with fatigue or inattention. A DVD may be elicited on examination by covering one eye and watching its position as the eye is covered. These patients do not experience diplopia. Patients with infantile esotropia also commonly develop accommodative esotropia, with a need for glasses later in childhood. Excellent visual acuity in both eyes and alignment of the eyes are typically achieved with treatment. Although early surgery is associated with better development of binocular function than later surgery, the development of very high levels of binocular function (stereopsis) is usually not obtained.

Accommodative esotropia most commonly presents as an acquired strabismus at 2 ½ to 5 years of age. Family histories of hypertropia, anisometropia, esotropia, and amblyopia are very common. The inheritance pattern is unknown and inconsistent with parents, siblings, or more distant relatives being affected in different families. The presence of uncorrected hyperopia causes the patient to accommodate or focus to obtain clear visual acuity. With accommodation, the synkinetic near response produces convergence of the eyes. If the fusion mechanism is unable to diverge the eyes to compensate for the excessive convergence accompanying the need to accommodate to correct for the patient’s hyperopia, esotropia results.
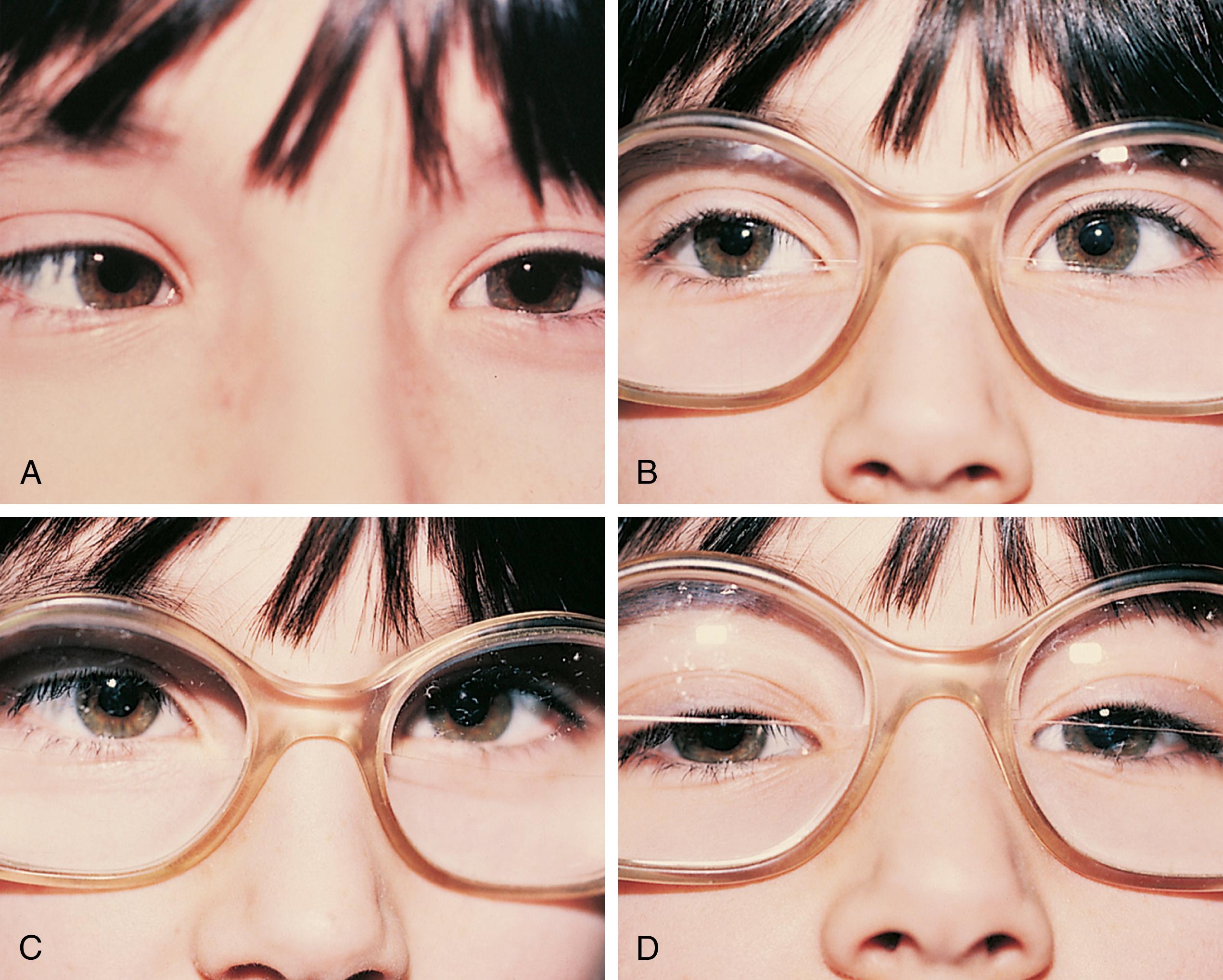
If an esodeviation is associated with a modest degree of farsightedness, treatment of the hyperopia optically with glasses is indicated. In patients with purely accommodative esotropia, this measure alone may completely correct the deviation ( Fig. 20.14 ). Frequently, especially if the esodeviation has been left untreated for a long period of time, a residual esodeviation will remain. This is a partially accommodative esotropia. Surgical correction may be recommended for these patients. Some patients have straight eyes for some time with their glasses in place and decompensate to partially accommodative or non-accommodative esodeviations later.
In patients with accommodative esotropia, the eyes are straight with their glasses on and esotropic when they are removed. Frequently, if the patient is only moderately hyperopic in the preferred fixating eye, they will say that they can see just as well or perhaps better without their glasses. The glasses are not being prescribed necessarily to improve visual acuity; they are to improve the esotropia.
In another form of accommodative esotropia, the ratio between accommodative convergence and accommodation (AC/A) ratio may be abnormally high, producing excessive convergence when focusing on near objects. In high AC/A ratio accommodative esotropia, the esodeviation with near vision is greater in magnitude than it is with distance vision ( Fig. 20.15 ). These patients may be treated with a bifocal. The bifocal gives them additional hyperopic correction for near, decreasing the accommodative effort needed at near and decreasing the near esodeviation.
Children may develop an esodeviation that is present without any relationship to the patient’s refractive error ( Fig. 20.16 ). Correction of the hyperopia with glasses does not improve the esotropia in these patients. These non-accommodative esodeviations may be associated with poor vision, trauma, prematurity, aphakia, or high myopia. Non-accommodative esotropia may develop when accommodative esotropias are left untreated; however, they also occur without the presence of any other ocular abnormalities.

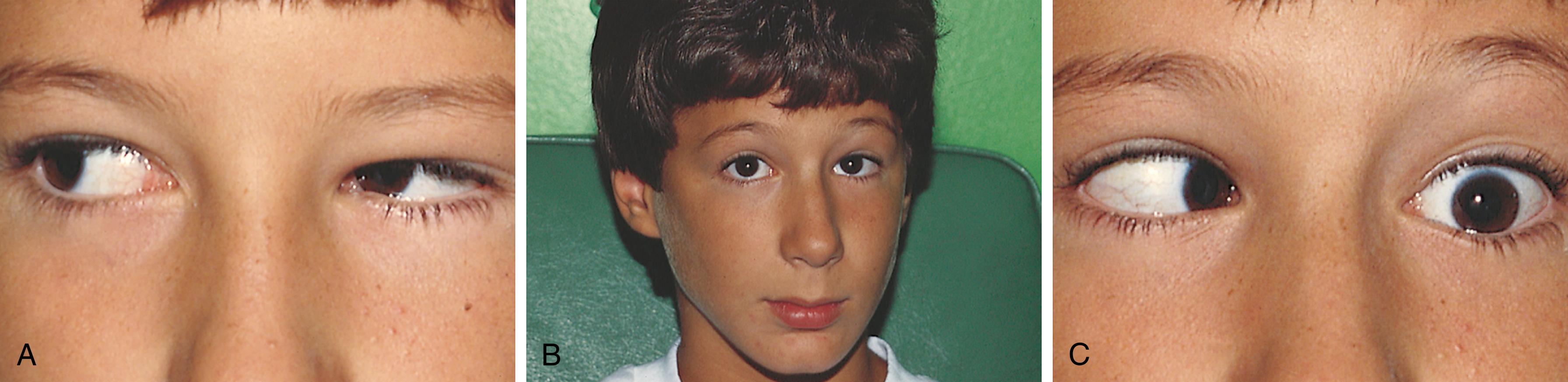
Unilateral or bilateral sixth cranial nerve palsy causes deficient abduction and an esodeviation. In sixth nerve palsy, the esotropia increases with gaze directed toward the side of the palsy (gaze incomitance). Patients may display a head turn toward the side of the palsy to hold the involved eye in adduction, away from the side of the palsy, to maintain binocular vision. Other signs of the nerve paralysis that may be subtle and more difficult to detect include the extent and speed of abduction of the eye. Sixth cranial nerve palsies in children may be associated with increased intracranial pressure, trauma, tumor, or antecedent viral illness. In benign or “post-viral” and traumatic cases, the lateral rectus function may return gradually and fully over a 6-month period. In idiopathic cases, if improvement does not occur, if the deviation increases, or if gaze palsy develops, suspicion should be raised that a tumor, most commonly pontine glioma, may be the cause for the sixth nerve paralysis.
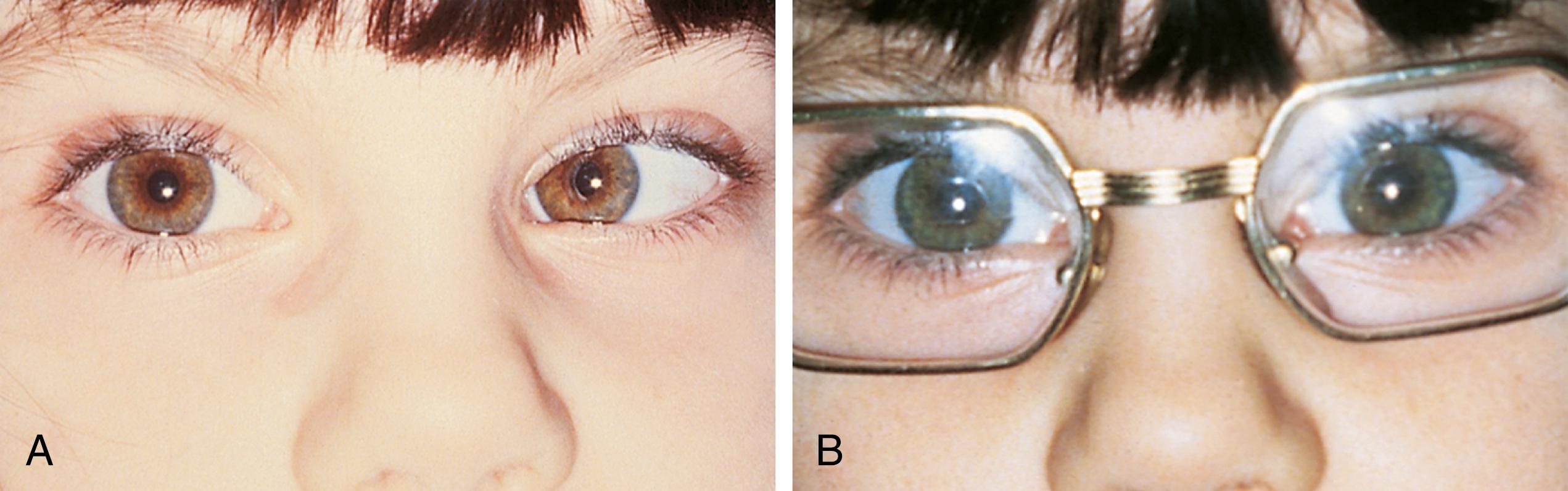
Duane syndrome is a congenital unilateral or bilateral defect characterized by inability to abduct an eye. This may be accompanied by an up or down shoot of the eye and narrowing of the lid fissure on attempted adduction. In attempted abduction, the palpebral fissure widens. Duane syndrome is caused by a malformation of the cranial nerve nuclei producing co-innervation of the medial and lateral rectus muscles. The lateral rectus muscle does not contract with abduction and paradoxically co-contracts along with the medial rectus on adduction. The co-contraction with adduction causes a retraction of the globe and the lid fissure narrowing. Patients with Duane syndrome may be esotropic and have a head turn toward the involved side analogous to those seen with a sixth cranial nerve palsy. The changes in lid position and presence of vertical deviations help to differentiate the two conditions ( Fig. 20.17 ). It is important to remember that children with Duane syndrome have a high incidence of hearing deficit.
Pseudostrabismus is seen in infants with prominent epicanthal folds, closely placed eyes, and flat nasal bridges. Asymmetry of the orbits, lids, or nasal bridge may also produce pseudostrabismus. When these facial features are present, the white of the sclera between the cornea and inner canthus frequently may be obscured or asymmetrical between the two eyes, giving the optical illusion that the eyes are esotropic ( Figs. 20.18 and 20.19 ). Parents and caretakers frequently report subtle esodeviations that worsen with gaze to the right or left. This is frequently pointed out in photographs in which careful examination shows the eyes to be in slight right or left gaze. Observation of symmetrical corneal light reflexes or cover testing confirms or excludes the presence of a true deviation. Pointing out the symmetry in the corneal light reflexes seen in photographs that the family is concerned about is frequently helpful.


When the visual axes are divergent, an exodeviation is present ( Fig. 20.20 ). Many children with exodeviations have family histories of strabismus. Exodeviations may also occur with vision loss in one eye (sensory exotropia) and cranial nerve paralysis (third nerve palsy). An exodeviation may be controlled by fusion (exophoria), be manifest intermittently (intermittent exotropia), or be constant (exotropia).

Intermittent exodeviations may become manifest with fatigue, daydreaming, or illness. Patients with exodeviations frequently squint one eye in bright light, but they typically do not experience diplopia. They may complain of images jumping as they switch fixation or of discomfort at night or when tired. Patients with intermittent exotropia usually do not have amblyopia, or it may only be mild. One-third of cases improve spontaneously. Treatment of intermittent exotropia may not be necessary if the deviation is not present frequently. Treatment consists of glasses to correct refractive errors, patching, and surgery.
If one eye has poor vision, the decreased visual stimulation may produce a sensory deviation. Generally speaking, if the onset of decreased vision occurs after 4 years old, an exodeviation will occur; however, if sensory input to the eye is decreased before 2 years old, an esodeviation usually occurs. Because young children do not complain of monocular vision loss, especially if congenital or with onset during infancy, sensory strabismus is frequently the presenting sign of vision loss caused by pathology of the retina or optic nerve.
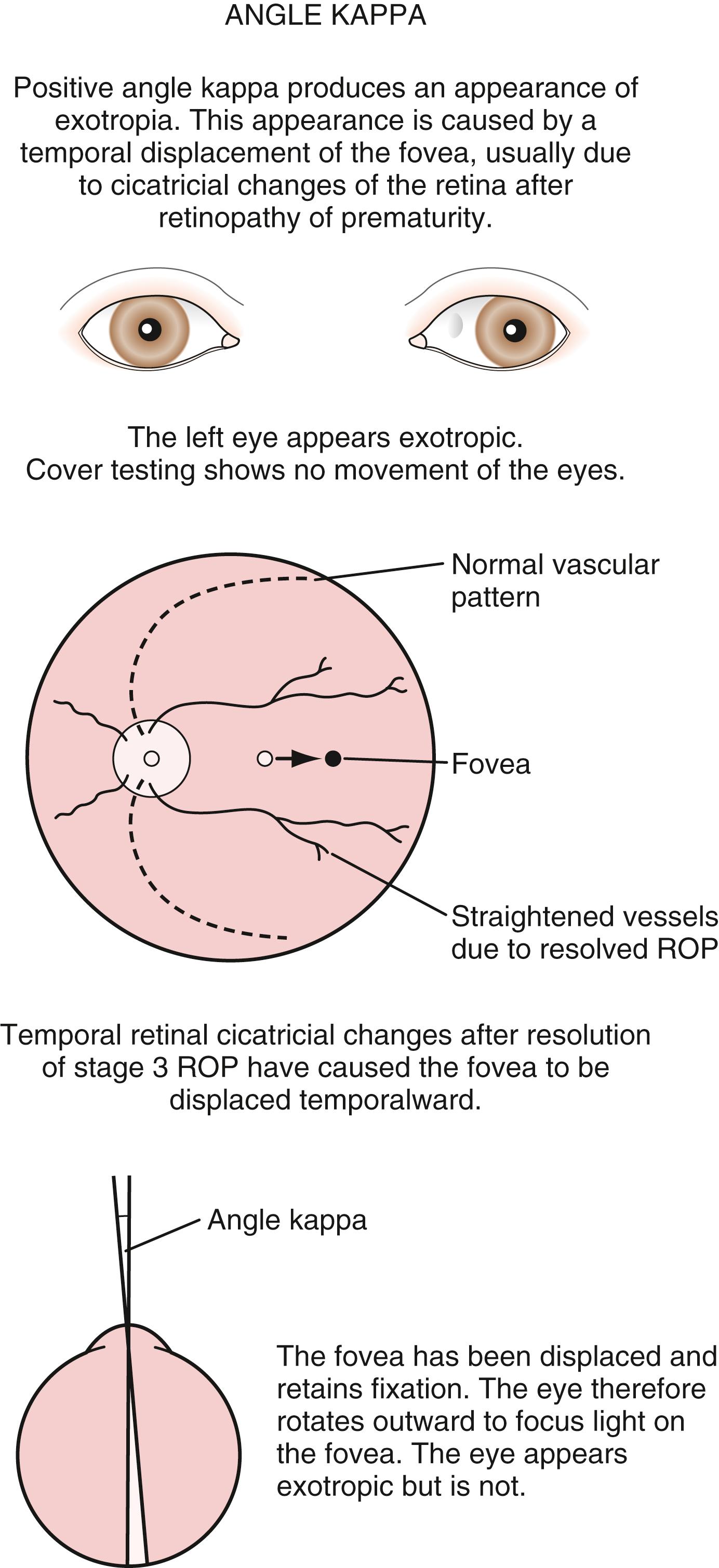
Exodeviations may be simulated in patients with widely spaced eyes (hypertelorism) or in those whose maculae are temporally displaced, as may occur in advanced ROP. When the macula is displaced temporally, the eye rotates outward to align its visual axis on the fixation target. The term positive angle kappa is used to describe this condition ( Fig. 20.21 ).
Convergence insufficiency describes an exodeviation in which the size of the deviation is greater in the near range than at distance. Most frequently, there is an exodeviation at near only and no distance deviation. This may cause symptoms of discomfort while reading, complaints of images jumping or moving, or intermittent diplopia at near range. To test for convergence insufficiency, the child is asked to fixate on a target with detail as it is brought progressively closer. Normally the child should be able to converge to a point 10 cm from the nose. If the eyes converge, and then break their alignment and diverge at a distance greater than 10 cm from the eyes, the patient should be evaluated for convergence insufficiency. With cover and uncover testing, an exodeviation will be seen at near fixation, and it will be smaller or not seen at distance fixation. Treatments include glasses and in some cases convergence exercises and therapy. Children who have postconcussion symptoms will often develop or have convergence insufficiency. This may or may not be accompanied by an accommodation deficit.
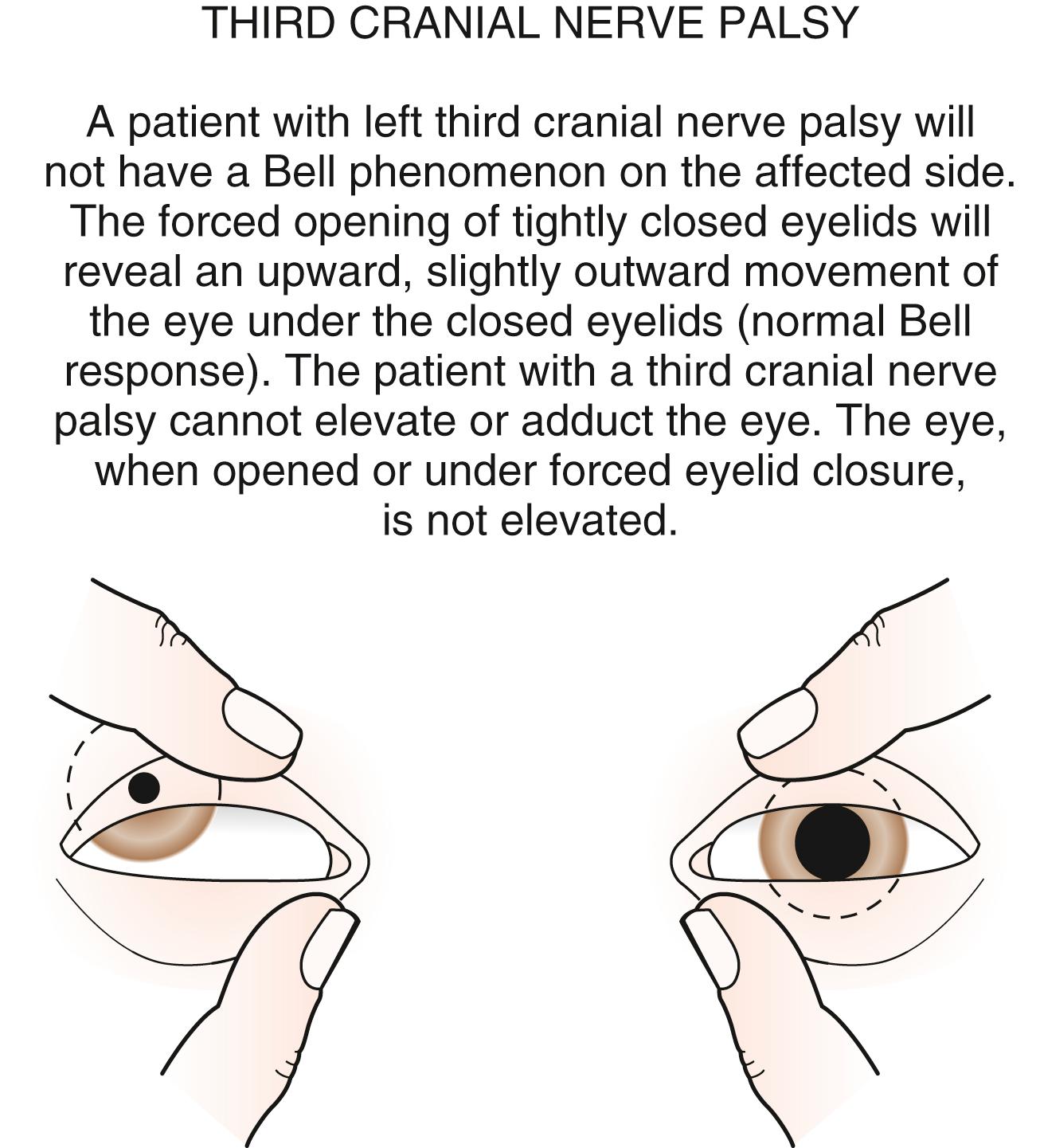
The third cranial nerve innervates the medial rectus muscle. In third nerve paralysis, the action of the lateral rectus muscle, innervated by the sixth cranial nerve, is unopposed and produces an exodeviation. The third nerve has two branches: a larger inferior branch or division, which innervates the inferior rectus, medial rectus, inferior oblique muscles and the ciliary muscle, which is responsible for accommodation of the lens and the iris sphincter muscle that produces miosis of the pupil; and a smaller superior branch or division that innervates the superior rectus and the levator palpebrae superioris, which elevates the lid. In the presence of a complete third cranial nerve palsy, the eye assumes a down and outward position, the eyelid is ptotic, and the pupil is enlarged. A palsy of the inferior division can present with intact elevation and no ptosis but adduction, and depression deficit with an enlarged pupil ( Fig. 20.22 ). Elevation of the eye with forced eyelid closure (Bell phenomenon) is typically absent in patients with third cranial nerve palsy ( Fig. 20.23 ). The most common causes for acquired third nerve paralysis in children are trauma and tumor. A third nerve palsy may also occur as a congenital defect.

Vertical deviations may occur in only one field of gaze, or they may be comitant, the same, in all fields of gaze. Vertical deviations may have a cyclotorsional component and be associated with a head tilt or head posture to eliminate double vision. All patients with torticollis should be evaluated for cyclovertical muscle palsies.
The most common cyclovertical deviation is due to a palsy of the fourth cranial (trochlear) nerve ( Fig. 20.24 ). Fourth nerve palsies in children occur congenitally or secondary to head trauma. The eye is excyclorotated, and the head is tilted to the shoulder opposite the side of the paretic nerve and superior oblique muscle to place the eyes in the position of best ocular alignment. Other features are elevation of the eye and difficulty depressing the eye in adduction ( Fig. 20.25 ). Children with congenital fourth nerve palsies usually do not have complaints of diplopia; but if they are asked about diplopia when their eyes are in the contralateral field of gaze, especially up and away from the paretic side, they can recognize the presence of diplopia. Later in life, patients with congenital fourth nerve palsy may decompensate in their control of the deviation and develop symptomatic diplopia. Some subtle facial asymmetry, especially of the cheek and jaw line, is almost always seen in congenital cases as the children age. Review of candid photos will frequently display consistently repeated head tilts that usually have not been noticed by the family.

Brown syndrome describes an isolated motility disorder in which there is an inability to elevate the eye when in adduction ( Fig. 20.26 ). This may be caused by a congenital anomaly of the superior oblique tendon, or it may be acquired as an idiopathic inflammation or tenosynovitis of the superior oblique tendon. Acquired cases may be persistent, resolve spontaneously (sometimes over many years), or respond to nonsteroidal antiinflammatory drugs (NSAIDs).

Abnormalities of extraocular muscle innervation rarely cause vertical deviations. Double elevator palsy is an inherited unilateral or bilateral condition in which there is hypotropia and limitation of elevation of the involved eye. To achieve binocularity, patients tilt their chins up and position their heads back. Ptosis is frequently present.
Additional causes of vertical deviations include myasthenia gravis, thyroid ophthalmopathy, chronic progressive external ophthalmoplegia, orbital fractures with muscle entrapment (most commonly the inferior rectus entrapped within a blowout fracture of the orbital floor), and orbital disease with intraorbital masses.
There is overwhelming evidence that strabismus surgery in children with developmental delay is unpredictable. It is becoming more and more reliable to use botulinum toxin injections to reduce the number of surgical procedures. While a brief anesthesia is still needed for botulinum injections into one or more of the extraocular muscles (usually horizontal rectus muscles) it avoids scarring and the further unpredictability of surgical reoperations.
Although gross observation may detect the majority of cases of strabismus, pseudostrabismus will frequently lead to unnecessary referrals. More significantly, smaller angle deviations may be missed, leading to delays in treatment if more sensitive tests for strabismus are not employed by the primary care physician.
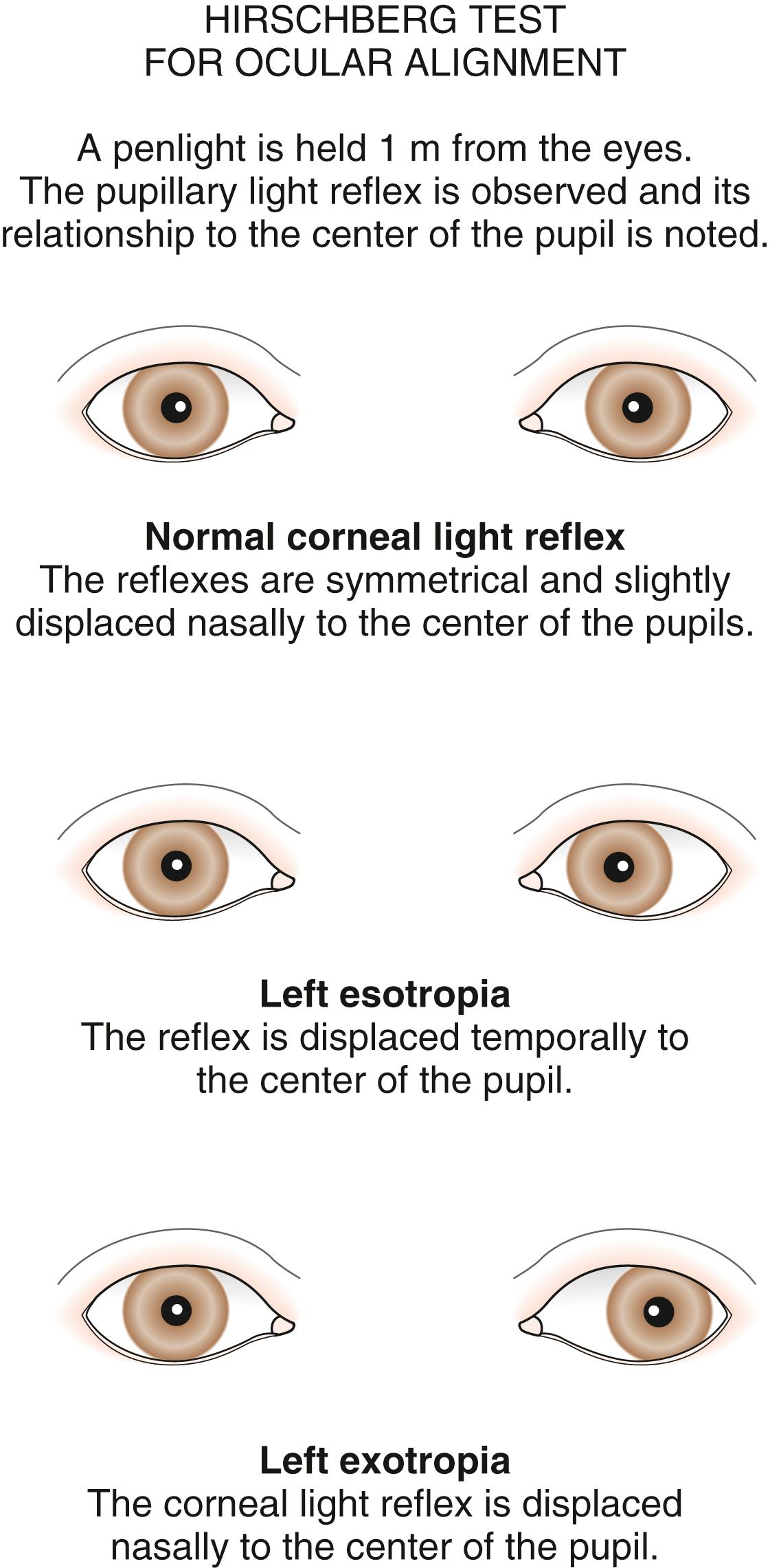
The type and degree of ocular misalignment may be estimated using the corneal light reflex test, or Hirschberg method. The patient fixates on a penlight held at 1 m. Using the pupil edge as a point of reference, the light reflections between the two eyes are compared for symmetry; if the light reflex is displaced temporally in one eye compared with the reflex seen in the other eye, an esotropia is present. If the light reflex is displaced nasally in comparison with the other eye, an exodeviation is present ( Fig. 20.27 ). Although observation of the corneal light reflexes is more sensitive and specific than gross observation alone, a more accurate method of detecting misalignment of the eyes is cover and uncover testing.
The cover test requires cooperation, vision in each eye and use of a target that stimulates accommodation. Cover testing is performed while the patient maintains fixation on targets at 6 m and at 1 m, because some types of strabismus produce misalignment of the eyes that is present only at either distance or near. The cover/uncover test is used to detect phorias. The test is performed by placing a cover over one eye to disrupt fusion or binocularity. The covered eye is observed as the cover is removed. If the eye deviates while covered and then moves to regain fusion and assumes fixation as the cover is removed, a phoria exists. The test is then repeated, covering and uncovering the other eye ( Fig. 20.28 ). If no movement is seen as each eye is covered and uncovered, both eyes are aligned on the object at that distance and there are no phorias present.
The second component of the cover test is performed by covering one eye and observing the movement of the other eye. If neither eye moves as the eyes are alternately covered, the eyes are both aligned on the fixation target, and the term orthophoria is used. No deviation is present in this case. If a tropia and a fixation preference are present, a fixation movement of the deviating uncovered eye occurs when the preferred fixating eye is covered; when the cover is transferred back, the previously deviating eye again deviates behind the cover ( Fig. 20.29 ). If a deviation is well controlled by fusion (a phoria) and is small in size, it may be safely observed if there are no symptoms and the fundus is normal. When a tropia is present, either constantly or intermittently, after 3 months old, the patient should be referred to an ophthalmologist. Ophthalmologists use prisms along with cover testing to measure the size of strabismic deviations. An online resource for visualization and practice of the cover test as well as the prism and cover test for measurement of strabismus can be found at the American Academy of Ophthalmology’s Pediatric Ophthalmology Education Center website at https://www.aao.org/pediatric-center-detail/strabismus-simulator .
Amblyopia is present when a decrease in vision in one or both eyes is present and all potential anatomic causes (refractive errors, media opacities, structural abnormalities) for the decrease in vision have been corrected or excluded. Amblyopia may be caused by the absence of stimulation of the immature visual system by a focused retinal image or by strabismus and the resultant suppression of one eye. Visual deprivation amblyopia may be caused by a corneal opacity, a dense cataract, vitreous opacity (hemorrhage or inflammation), or high refractive error ( Fig. 20.30 ).
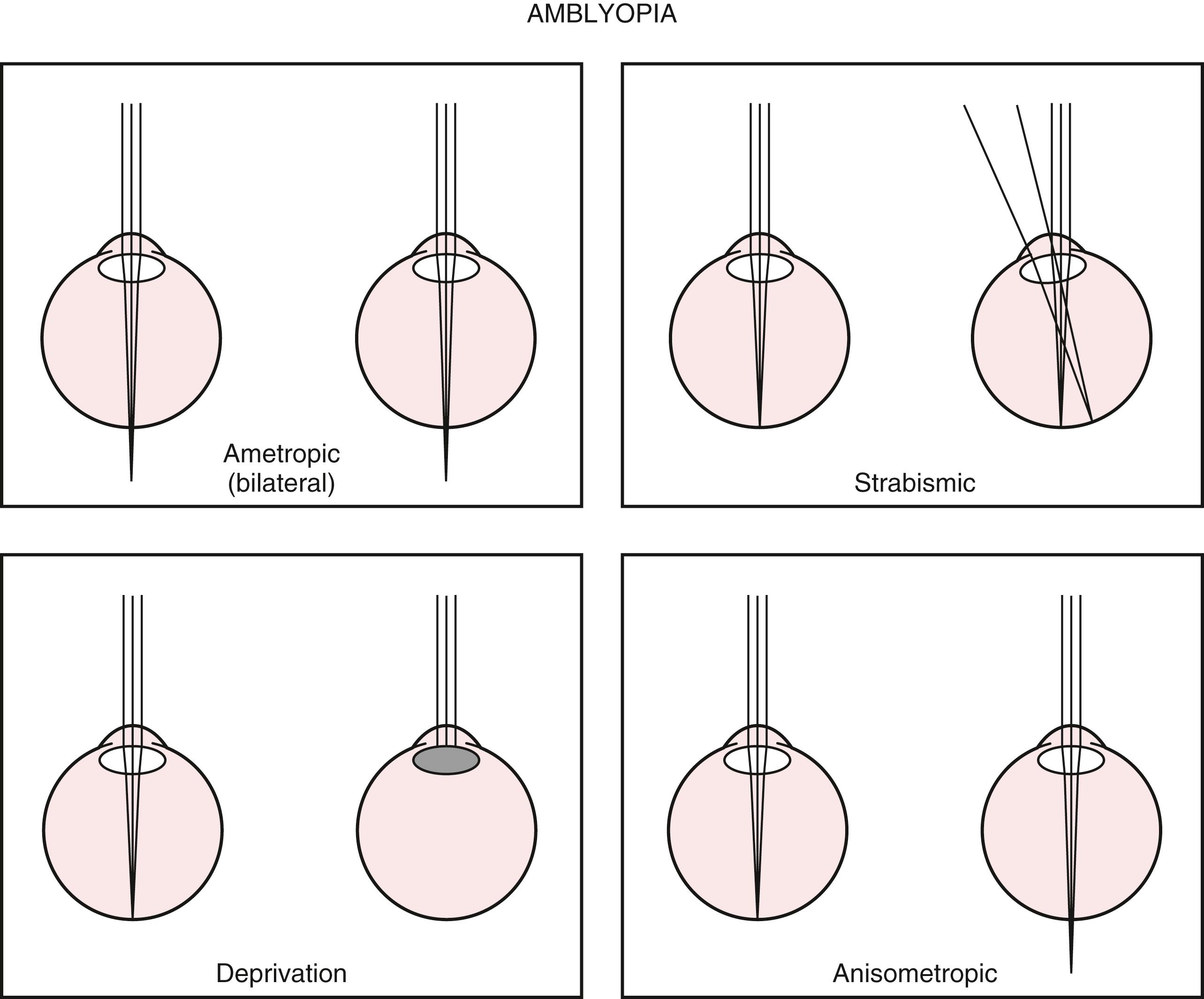
In anisometropic amblyopia, an image is clearly focused on the fovea of one eye; however, the image is out of focus in the other eye. The blurred retinal image is suppressed or ignored by the child’s immature visual system, and that eye develops amblyopia. In anisometropic amblyopia, most commonly one eye is more hyperopic than the other. Because both eyes must accommodate the same amount, the less hyperopic eye is preferred and the more hyperopic eye has the blurred image and develops the amblyopia. With high hyperopia or astigmatism affecting both eyes, bilateral refractive, or ametropic, amblyopia may occur if the child does not or cannot consistently accommodate to produce a focused retinal image to stimulate the visual system with either eye. These patients have decreased vision in both eyes. In children with strabismus, the image from the deviating eye is suppressed by the brain as an adaptation to avoid diplopia and the deviating eye develops strabismic amblyopia. Patients often have both strabismus and anisometropia simultaneously as causes for their amblyopia.
The severity of the visual loss produced by amblyopia is determined by the nature of the visual deprivation; the age at onset; and its consistency, severity, and duration. Amblyopia is treated by removing the cause of the amblyopia, if possible, and by forcing use of the affected eye to stimulate the development of the vision from that eye. In bilateral refractive amblyopia, the appropriate glasses are given as treatment. In strabismic or anisometropic amblyopia, appropriate glasses are given, and the preferred, nonamblyopic eye is penalized to force the use of the amblyopic eye.
An occlusion patch placed over the preferred fixating eye is commonly used as treatment. Other methods of treatment are optical via the eyeglass prescription and pharmacologic, with atropine drops placed in the nonamblyopic eye to prevent accommodation in that eye. This forces the use of the amblyopic eye for reading and near vision. New treatments for amblyopia based on encouraging binocular stimulation are promising new developments.
Amblyopia responds most rapidly and completely to treatment begun early in life. The visual system has developmental phases, and if certain levels of visual acuity are not reached early in life, the amblyopia present is unlikely to respond completely to treatment. Treatment is more difficult and less effective after 8 years old but remains possible in older children, especially if they have no history of previous treatment.
Children may present with an anomalous head posture. This may or may not be due to the eyes. An anomalous head posture may be a face turn, a head tilt, chin up or chin down or any combination of these. A combination of head positions for example, left face turn with right head tilt is most often seen in cases of nystagmus when the brain places the eyes in the position of least ocular oscillation (the null position). Otherwise, ocular causes of a face turn may be due to restriction of either abduction of one eye or adduction of one eye or a gaze paresis of both eyes. Ocular causes of a head tilt are as superior oblique palsy, or any extraocular muscle problem that causes one eye to sit higher than the other; the head tilts to the lower positioned eye (i.e., the eye with the hypotropia). Ocular causes of a chin-up head position include bilateral ptosis, or an esotropia that disappears in down gaze but is present in primary and up gaze (this is called an A pattern esotropia) or an exotropia that disappears in down gaze but is present in primary and up gaze (this is called a V pattern exotropia). If a child with vertical nystagmus has a null position with the eyes in downgaze, then this would also cause a chin-up head position. Similarly, ocular causes of a chin down head position are vertical nystagmus with null position in up gaze. An A pattern exotropia with little or no exotropia in up gaze is a possible cause of a chin down head position but is exceedingly rare but a V pattern esotropia with the eyes relatively straight in up gaze but esotropia in down gaze can be seen.
Nonocular causes of head tilt include torticollis, while a face turn may be seen in a child with a homonymous hemianopia with the turn of the head into the hemianopia field. A child who has hearing deficit on one side may also turn the face with the hearing side turned further forward so as to hear more clearly.
To differentiate between an ocular or nonocular cause of anomalous head position, the clinician should move the child’s head into the primary and neutral position and observe any restriction of eye movement, or any worsening of nystagmus. Moreover, if one eye is covered and the head position was being driven by the need of binocular vision the head will straighten ( Fig. 20.31 ).

Very occasionally, a child will develop a head tilt if they have astigmatism that is uncorrected.
Nanophthalmos: In this uncommon congenital condition, the eye is small but is not associated with other developmental defects. There is high hypermetropia, with short axial length (16 to 18.5 mm), and a crowded anterior chamber predisposing to glaucoma after the second decade of life. Choroidal effusions can occur because of the thickened inelastic sclera. It may be associated with the Kenny Caffey syndrome. Refractive correction is important, as is surveillance for glaucoma.
Microphthalmos: This rare developmental anomaly tends to be bilateral. The eye is small but abnormal either with coloboma (defective closure of the embryonic fissure) or coloboma with cyst or cataract ( Fig. 20.32 ). Vision may be normal or as poor as light perception. Microphthalmos may be seen in CHARGE syndrome, MICRO syndrome (microphakia, microphthalmos, characteristic lens opacity, and atonic pupils, cortical visual impairment, microcephaly, and developmental delay), and MIDAS (microphthalmia, dermal aplasia, and sclerocornea—also known as MLS) syndrome.

Anophthalmia: Very rare anomaly where the eye clinically is not present or is present as a vestigial nonfunctioning structure. The child may be otherwise healthy but intracranial and systemic anomalies are often seen. The absence of a normal eye affects normal orbital growth and for this reason orbital expanders may be needed and referral to an oculoplastic surgeon is needed. Systemic and genetic evaluation is needed.
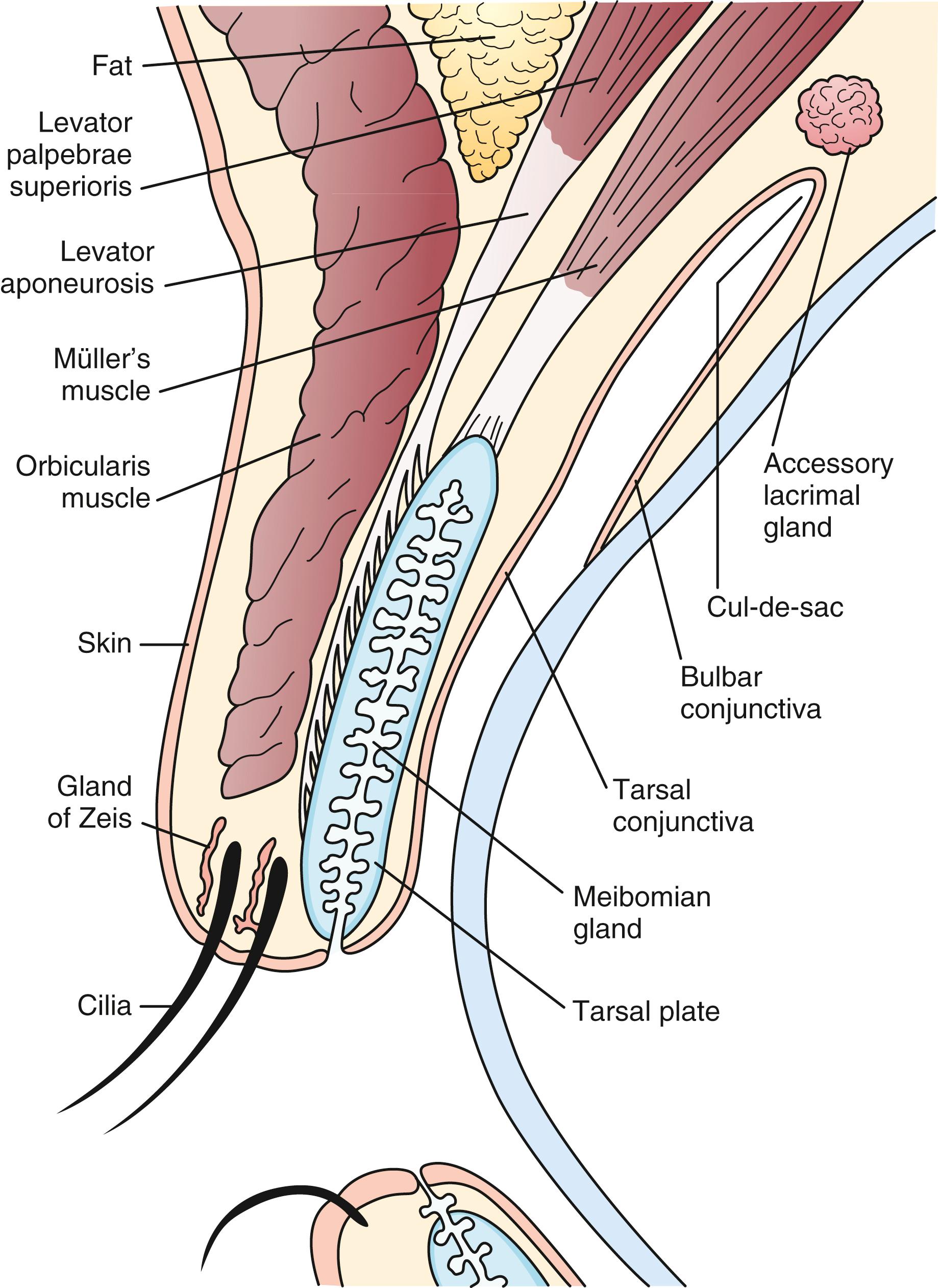
The eyelid is composed of skin and its related appendages, meibomian glands that contribute to the tear film, tendons that define the shape and position of the eyelid, and muscular structures permitting the eyelid to open and close ( Fig. 20.33 ). Conditions affecting the eyelid are related to these anatomic structures.
Conditions that affect the lids can be congenital or acquired. Congenital conditions may be rare or common. Common congenital conditions include the following.
Telecanthus is an increase in the distance between the inner canthus of each eye ( Fig. 20.34 ). Telecanthus can be due to the hereditary transmission of facial features or midline embryonic defects (congenital), or it may be related to a syndrome, such as blepharophimosis syndrome (BPES) ( Fig. 20.35 ). This inherited syndrome consists of telecanthus, epicanthus inversus (a skinfold projecting over the inner angle of the eye and covering part of the canthus, arising from the lower lid skin), blepharophimosis (horizontal shortening of the lid fissure), and ptosis. Telecanthus can be improved surgically.
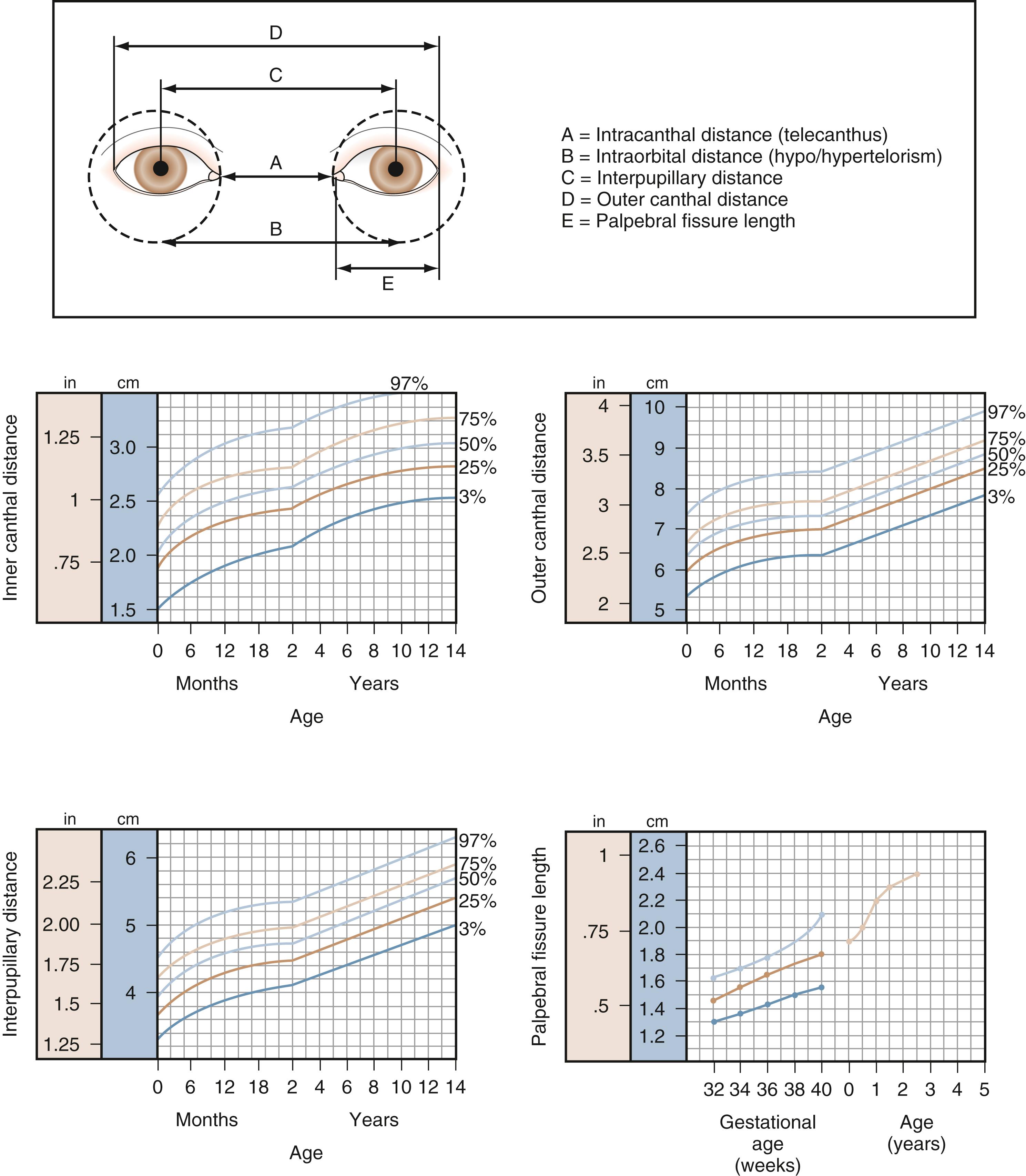
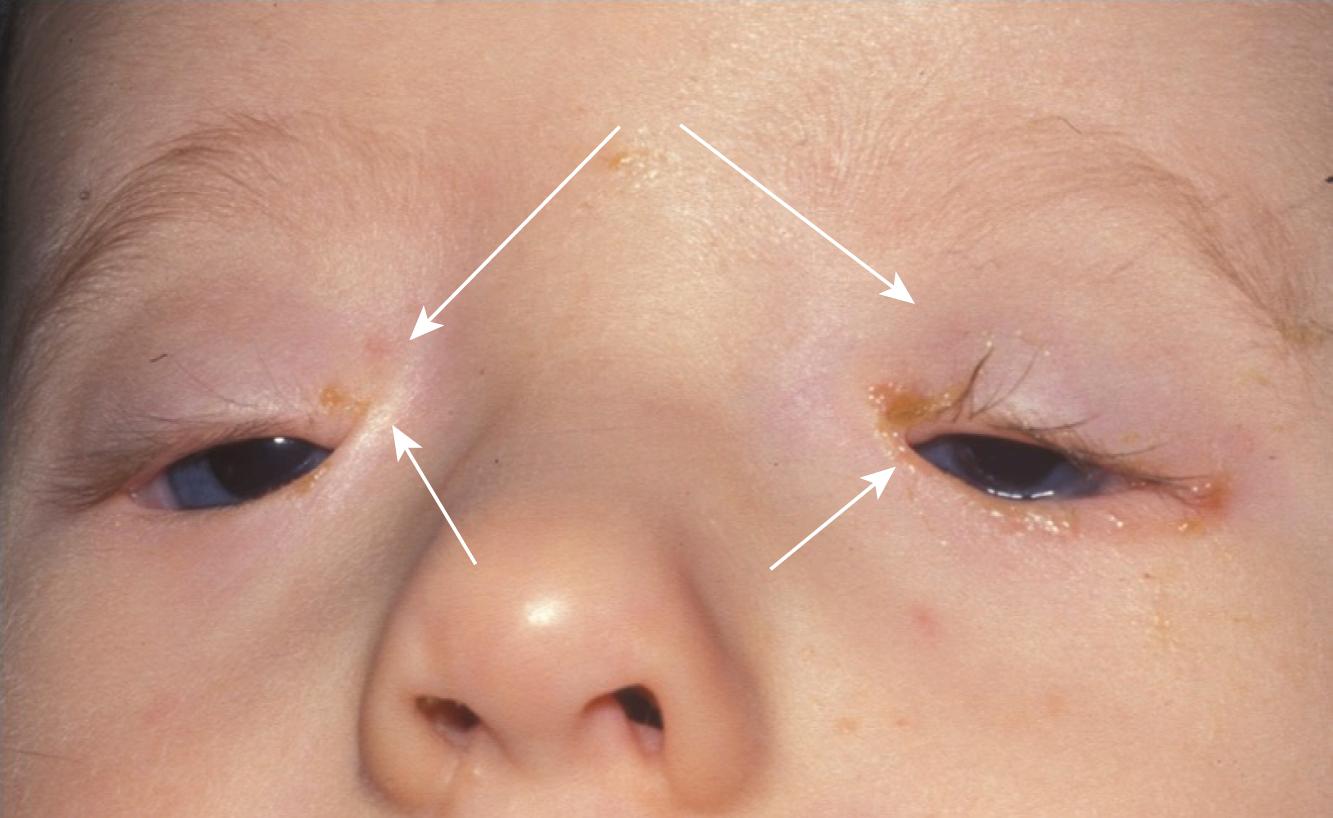
Epicanthus or epicanthic folds are vertical fold of skin on either side of the nose, sometimes covering the inner canthus—may be a normal ethnic variant. Can give the impression of a pseudostrabismus but resolves with age (see Fig. 20.18 ).
Ptosis is a drooping of the upper eyelid that is not uncommon and may be congenital ( Fig. 20.36 ) or acquired. It may either be myogenic, neurogenic, or mechanical. Lowered upper lid margin position may be measured in terms of palpebral aperture or marginal reflex distance (distance of the upper lid margin to the central corneal reflection when using a flashlight as a target for the patient to look at, normally 3.5 to 4.5 mm).

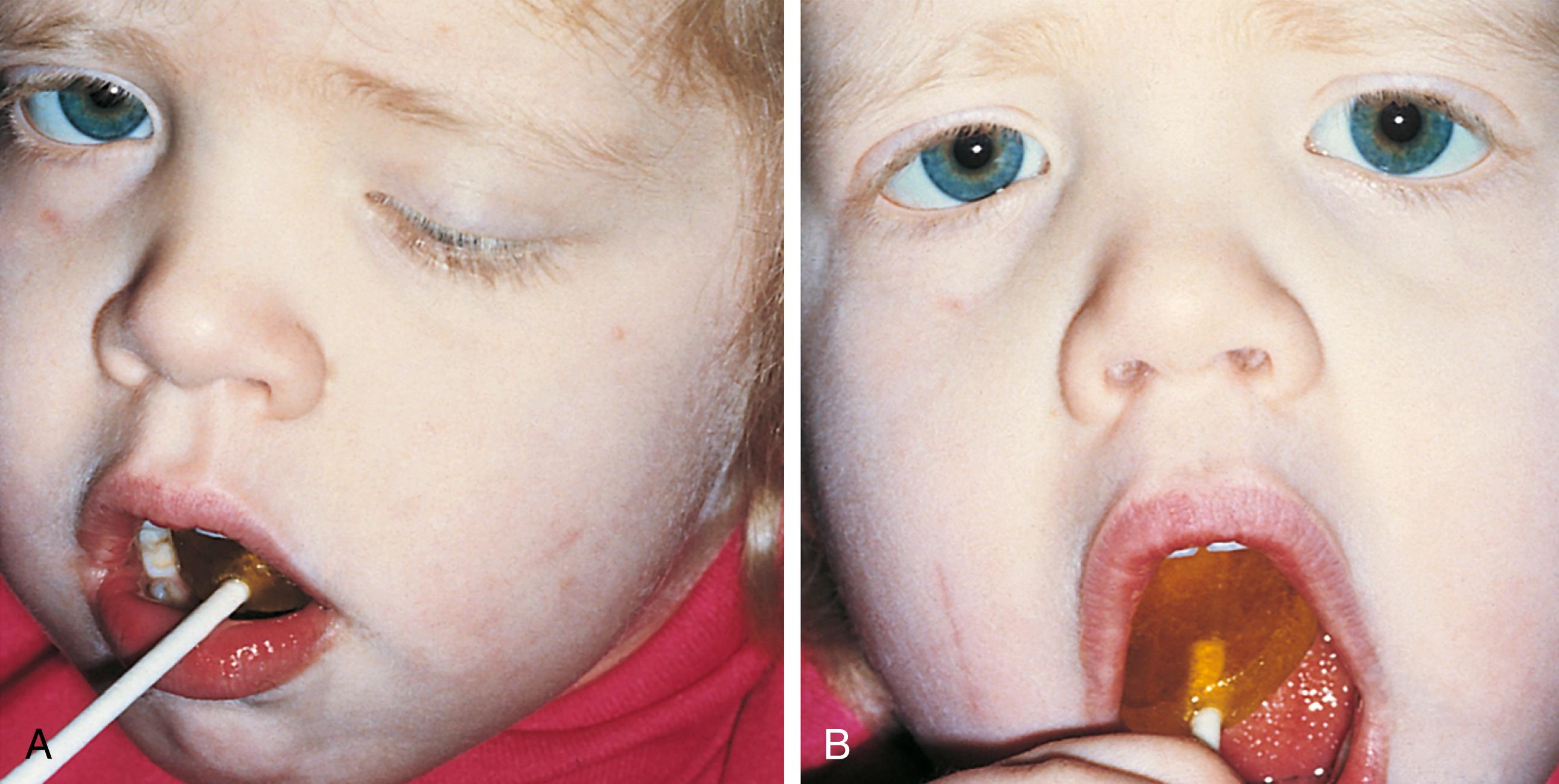
The treatment depends on the cause. Ptosis may be due to dysfunction or absence of the levator palpebrae superioris muscle. Dysfunction may allow strengthening of the muscle while absence requires a frontalis sling (i.e., attaching the lid to the frontalis muscle). Ptosis can cause amblyopia related to either stimulus deprivation (if severe ptosis) or astigmatism (mild to moderate ptosis). In any case, prompt ophthalmic referral is required. Care should be taken so as not to cause exposure keratopathy if ptosis repair is undertaken. If the etiology is mechanical, then the cause needs to be removed, e.g., large hemangioma. The prognosis is generally good. The Marcus Gunn jaw-winking phenomenon is caused by a misdirection of the motor division of the fifth cranial nerve to the ipsilateral levator muscle of the eyelid. Jaw movement causes the lid to “wink” ( Fig. 20.37 ). Systemic associations of congenital ptosis that are noteworthy are BPES (see above) and Rubinstein-Taybi syndrome (anomalous thumbs). Acquired associations include myasthenia gravis (fatiguability), myotonic dystrophy, and Kearns-Sayre syndrome (heart block and retinal dystrophy). Unilateral ptosis with ipsilateral miosis must have Horner syndrome excluded.
Epiblepharon: A skinfold extends over the lid margin and presses the lashes against the globe. It is commonly observed during the first year of life ( Fig. 20.38 ). The lower lid is more commonly affected in the European population, and both the upper and lower lids may be affected in Asian infants. This defect usually corrects itself spontaneously by 1 year old. In Asians, the problem may be persistent. Corneal abrasion usually does not occur because it is the shaft of the eyelash rather than the tip of the lash that touches the cornea. However, surgical correction may be required if it is persistent and causing corneal abrasion. Conjunctival injection, epiphora, and photosensitivity are symptoms in more significant cases.

Rare congenital conditions affecting the lids include the following.
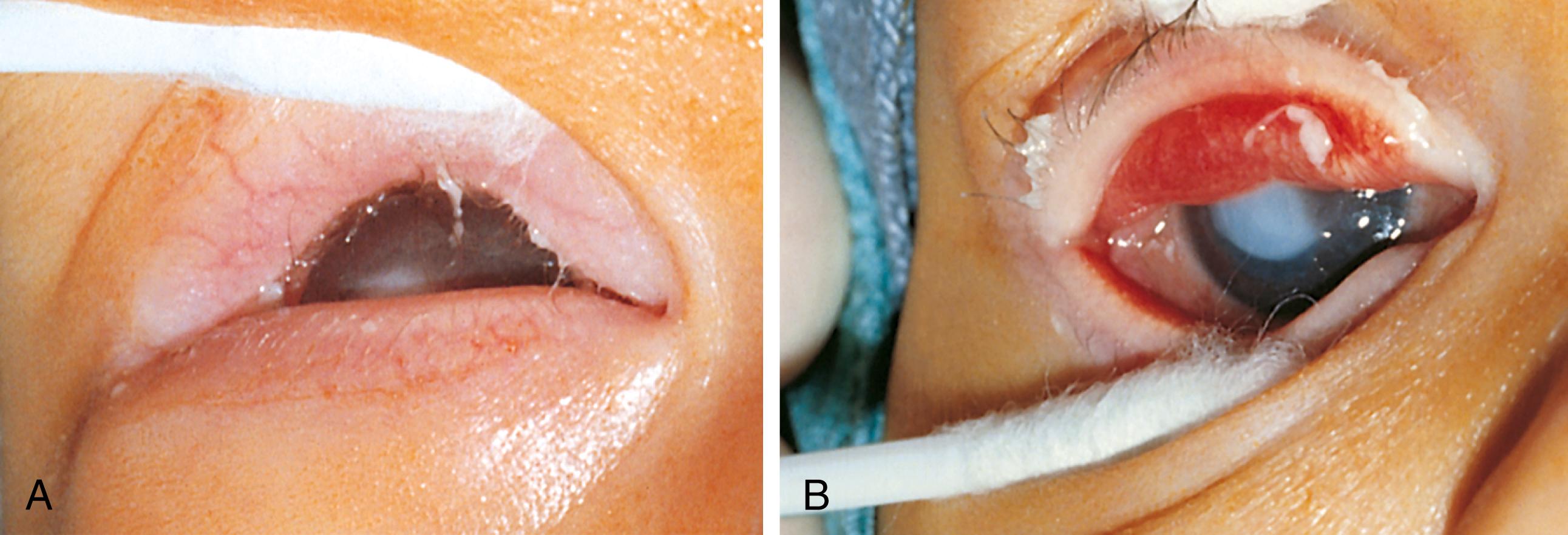
Ablepharon is a very rare condition of absent or hypoplastic lids. The child has exposed globes and may also have macrostomia. This condition can be confused with congenital everted upper lids but these can be flipped so as to allow the lids to close. Exposure keratopathy is a threat to vision ( Fig. 20.39 ).

Ankyloblepharon consists of fusion of the upper and lower eyelid margins but with a few thin strands of tissue. If only threadlike strands are present, treatment may be with lid separation with simple eyelid opening. Use of scissors occasionally may be necessary.
Cryptophthalmos describes complete fusion of the upper and lower lids so that the skin of the forehead passes onto the skin of the cheeks. This is most often associated with Fraser syndrome (Fryn 1 gene).
Coloboma is the incomplete formation of the upper/lower lid(s). It is most commonly seen in Goldenhar syndrome (upper lid, Fig. 20.40 ), amniotic band syndrome, and other clefting syndromes (usually lower lid, Fig. 20.41 ). Treatment is with lubrication in first instance to prevent exposure keratopathy. Early referral to an oculoplastic surgeon to allow reconstruction of lid(s) is needed.


Entropion defines an inverted eyelid with the lashes rubbing against the conjunctiva or cornea. This may be present at birth or occur with severe blepharospasm, inflammation, or trauma. If severe, abrasion of the cornea by the lashes can cause permanent corneal scarring ( Fig. 20.42 ). Its differential is an epiblepharon, which is due to an excess skin fold causing the lashes only to turn in. Surgical correction is straightforward.
Ectropion is an outward rotation of the eyelid margin. It usually is acquired due to shortening/cicatrization of lid skin, for example, scleroderma and epidermolysis bullosa. Congenitally, it can be seen in ichthyosis with ectropion of both upper and lower eyelids (Harlequin Baby) ( Fig. 20.43 ). It is clinically diagnosed by exposure of tarsal conjunctiva. Treatment depends on etiology but emollient use in cases of ichthyosis often leads to resolution. Rarely, surgical correction is needed.

If severe, ectropion can lead to problems of corneal exposure (see Fig. 20.43 ). Ectropion may also occur after seventh cranial nerve palsy with paralysis of the facial musculature, usually of the lower eyelid.
Distichiasis describes a condition in which there is an accessory row of eyelashes (cilia) along the posterior border of the eyelid. This condition is inherited as an autosomal dominant condition but may be associated with lymphedema of the limbs.
Madarosis is a lack or loss of eyelashes that can be seen in skin conditions such eczema, icthyosis, or ectodermal dysplasia. It can also be due to pulling eyelashes out.
Poliosis refers to white or depigmented eyelashes. It usually is seen in oculocutaneous albinism but may be acquired as part of Vogt-Koyanagi-Harada disease, an autoimmune disorder affecting the eyes (inflammation) and skin (vitiligo and poliosis).
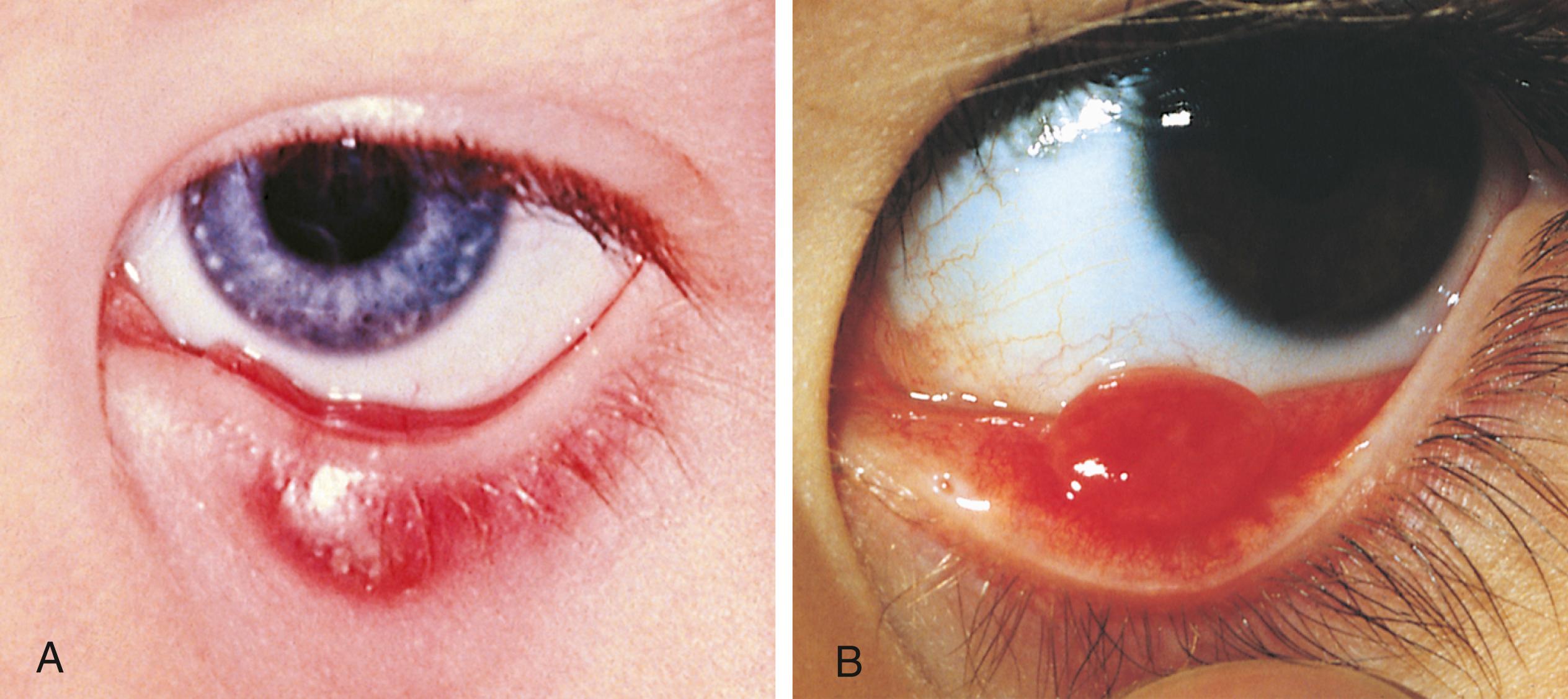
Symblepharon is a rare anomaly; it is usually acquired but may be congenital ( Figs. 20.44 and 20.41 ). Acquired types are seen in Stevens-Johnson syndrome, toxic epidermolysis syndrome, alkali injuries to the eyes, ocular cicatricial pemphigoid and rarely, epidermolysis bullosa (recessive types usually). It presents as shortened fornices due to an adhesion between the lid and conjunctiva ( Fig. 20.44 ). Prevention is the best approach in conditions where symblepharon may be acquired; topical lubrication and steroids may be needed but ophthalmic opinion must be sought early. Once formed, amniotic membrane may be used to treat after resection of the symblepharon. Acquired conditions of the lids include:

Trichiasis describes misdirected eyelashes that irritate the cornea or conjunctiva. It can be caused by chronic inflammation of the eyelids, entropion (inturning of the eyelid), eyelid trauma, or inflammatory conditions with scarring of the conjunctiva, such as Stevens-Johnson syndrome.
Blepharitis is inflammation of the eyelid margins ( Fig. 20.45 ), with or without chalazion (blocked meibomian gland) (see chalazion below). The anterior type usually affects lashes while the posterior type is caused by meibomian gland dysfunction. It is often mistaken for pink eye but the clue is its chronicity and often asymmetry. It may present with recurrent chalazia, chronic red eyes or chronically crusted lids. While usually isolated, chalazia may be associated with acne rosacea. Treatment includes lid hygiene, topical antibiotics. Mild steroids may be needed and occasionally systemic antibiotics may be needed. Treatment is necessary to prevent corneal complications (vascularization/keratitis).

Prognosis is moderate since the condition may never totally resolve, although the signs and symptoms can be controlled to prevent ocular damage. Blepharitis may be associated with chronic environmental allergies and occurs commonly in children with Down syndrome.
A hordeolum, commonly referred to as a stye, is an inflamed gland of Zeis along the eyelid margin ( Fig. 20.46 ). It may be painful and produce swelling and erythema of the eyelid. Infection may occur frequently with Staphylococcus . Some discharge may be seen. Rarely, preseptal cellulitis may occur as a complication. Removal of eyelash accelerates resolution. Occasionally, topical antibiotics may be needed.
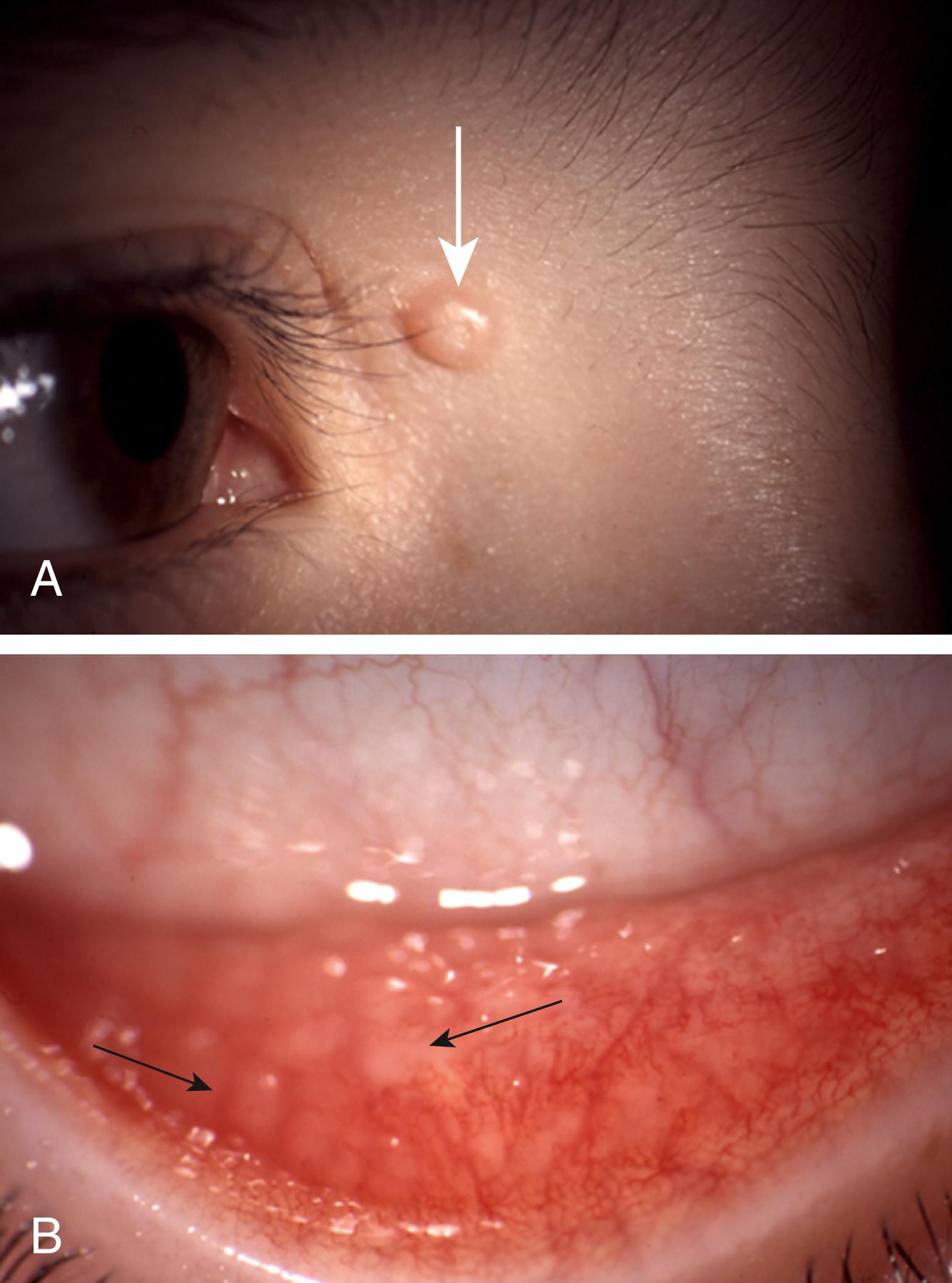
A chalazion is a chronic granulomatous inflammation of the meibomian glands within the tarsal plate (higher on the lid than a hordeolum). Painless swelling and redness of the eyelid result from distention of the gland and the inflammatory response caused by the retained glandular secretions. The gland may spontaneously rupture either to the conjunctival surface or externally to the skin ( Fig. 20.47A and B). Spontaneous resolution may occur; however, tissue reaction may persist and leave a firm mass within the lid. Surgical excision of the lesions may be required if chronic or inflamed in order to prevent drainage through the skin surface with scarring of the skin or possible permanent loss of lashes if the lid margin is severely affected. Small lesions that are not significantly inflamed or threatening drainage on the skin surface may be conservatively treated for weeks or months to avoid surgery.
Molluscum contagiosum is a common eyelid infectious tumor caused by a poxvirus. Small umbilicated nodules are often situated on the lid margin ( Fig. 20.48 , upper panel ) and should be looked for in cases of follicular or chronic conjunctivitis ( Fig. 20.48 , lower panel ). The lesions are usually self-limiting but if conjunctivitis is troublesome then curettage of lid lesions may be needed.
Capillary (infantile) hemangioma is the commonest benign tumor of the eyelid or orbit of childhood and histologically displays abundant endothelial cells with narrow vascular channels ( Fig. 20.49C and D).

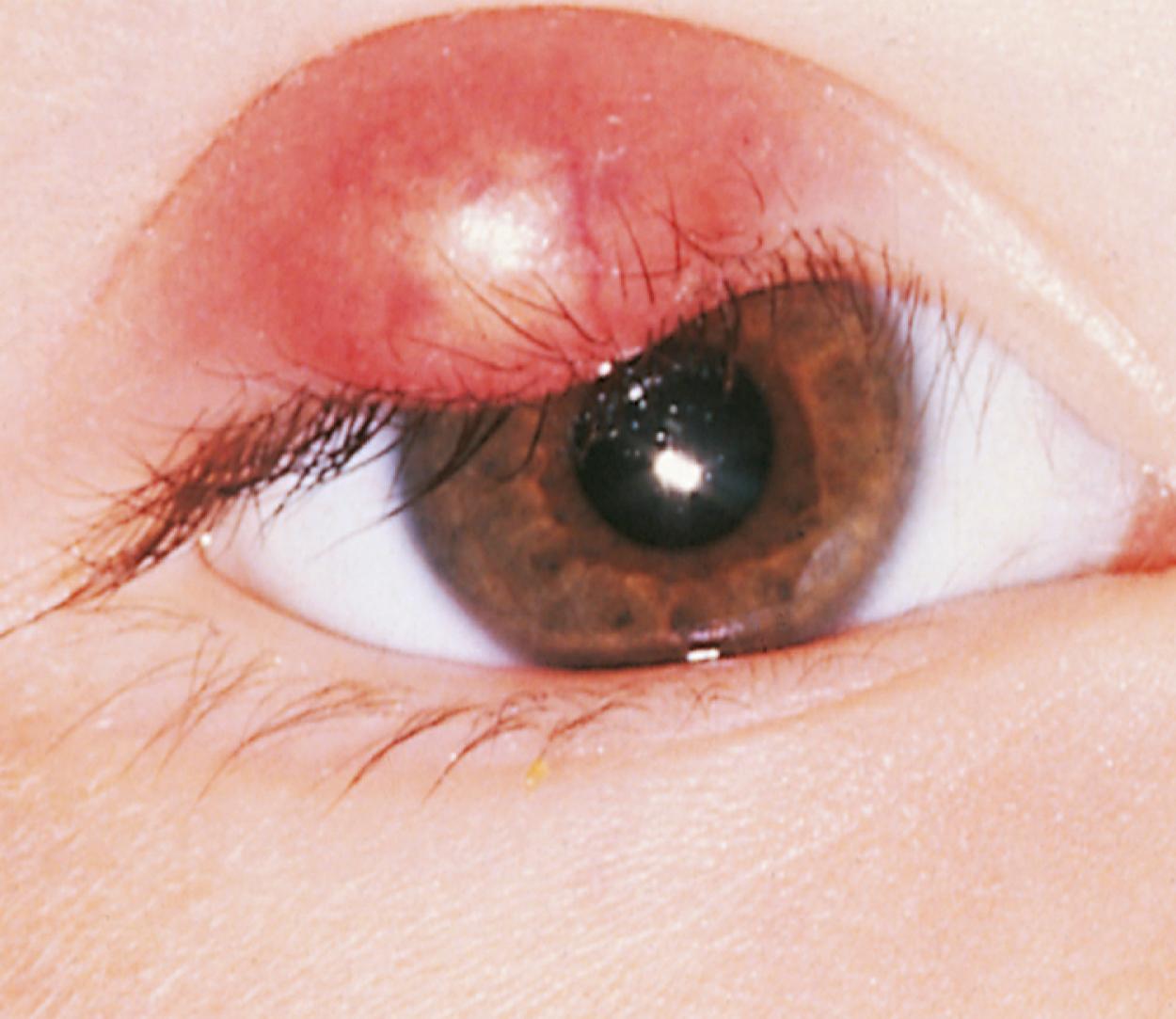
Systemic associations include Kasabach-Merritt syndrome (thrombocytopenia due to platelet pooling and activation within one or more large hemangiomas), Maffucci syndrome (hemangiomas and enchondromas), and PHACES syndrome (segmental facial hemangioma associated with other anomalies; Fig. 20.49A ). Infantile hemangiomas appear 2 or 3 weeks after birth, grow rapidly until 4 months of age with plateau of growth often by 6 months, and usually regress thereafter. The position of the hemangioma may result in visual deprivation by causing a ptosis, amblyopia from astigmatism or rarely compress the optic nerve if the hemangioma is intraorbital. Treatment is systemic or topical beta blockers. Some cases still demand surgical excision. Occlusion of the unaffected eye may be needed to prevent amblyopia from developing in the affected eye. The complication of hypoglycemia should be considered when treating with systemic beta blockers.
Port wine birthmark is a common dermal capillary vascular malformation which may occur in the periocular region. Ocular associations include episcleral hemangioma, iris heterochromia (affected iris darker than unaffected one), choroidal hemangioma, and glaucoma. Systemic associations include Sturge-Weber syndrome and cutis marmorata telangectasia congenita. Periocular lesions are associated with an increased risk of developing glaucoma, and the child should be seen regularly to exclude this ( Fig. 20.49B ).
Lid retraction is rare and causes include thyroid eye disease (e.g., Graves disease) (lid signs such as retraction and lid lag seen in 25% to 60% of pediatric cases) ( Fig. 20.50 ), Parinaud syndrome, Marcus-Gunn jaw winking and primary congenital idiopathic lid retraction. Lower lid retraction can be seen in cherubism (a rare, inherited condition characterized by fibro-osseous lesions of the maxilla and mandible recently localized to chromosome 4p16.3). No treatment is required except lubricating drops or ointment, used at night if there is evidence of lid lag and incomplete closure of the lids when asleep and treatment of underlying cause.

Preseptal cellulitis is a common but serious infection in children, most commonly due to direct infection from external factors such as a wound or hematogenous spread or sinusitis. This is in contrast to orbital cellulitis which frequently is an extension from contiguous ethmoid sinusitis. Examination of preseptal cellulitis usually finds red swollen eyelids which may be tense, but full ocular examination, including visual acuity, eye movements, color vision, pupil reactions, and fundoscopy, is normal. Treatment with systemic antibiotics is necessary, but progression to orbital cellulitis is uncommon. Imaging is needed if the lids are too swollen to allow adequate ocular exam.
Vesicular rash such as herpes simplex and varicella zoster can both cause vesicular rashes on the lids ( Fig. 20.51 ). If the eye is red then it can suggest an accompanying conjunctivitis, with or without keratitis. Varicella zoster is rare in children but a lesion on the tip of the nose indicates involvement of the ophthalmic division of the maxillary nerve and possible involvement of the eye with keratitis, uveitis, and glaucoma.

Phthiriasis, infestation of the lashes with the crab louse Phthirus pubis, manifests as a crusty appearance of the lid margin. Closer inspection reveals egg cases and the adult louse. Ophthalmic ointment, almost any type, used for a few weeks suffocates the organisms. Phthiriasis is another cause of chronic conjunctivitis, and the lashes should be carefully examined in cases of chronic recurring conjunctivitis.
Reflex tears are produced by the lacrimal gland, whereas the basal secretion of tears comes from the accessory lacrimal glands ( Fig. 20.52 ). The tear film consists of three layers: the layer closest to the eye is made of mucin, the next layer is the aqueous from lacrimal glands, and the outermost layer is lipid from the meibomian glands in the lid margins. During the first month of life, the eye remains moist, but reflex tearing, or tearing resulting from emotion, does not occur until the second month of life or early in infancy.
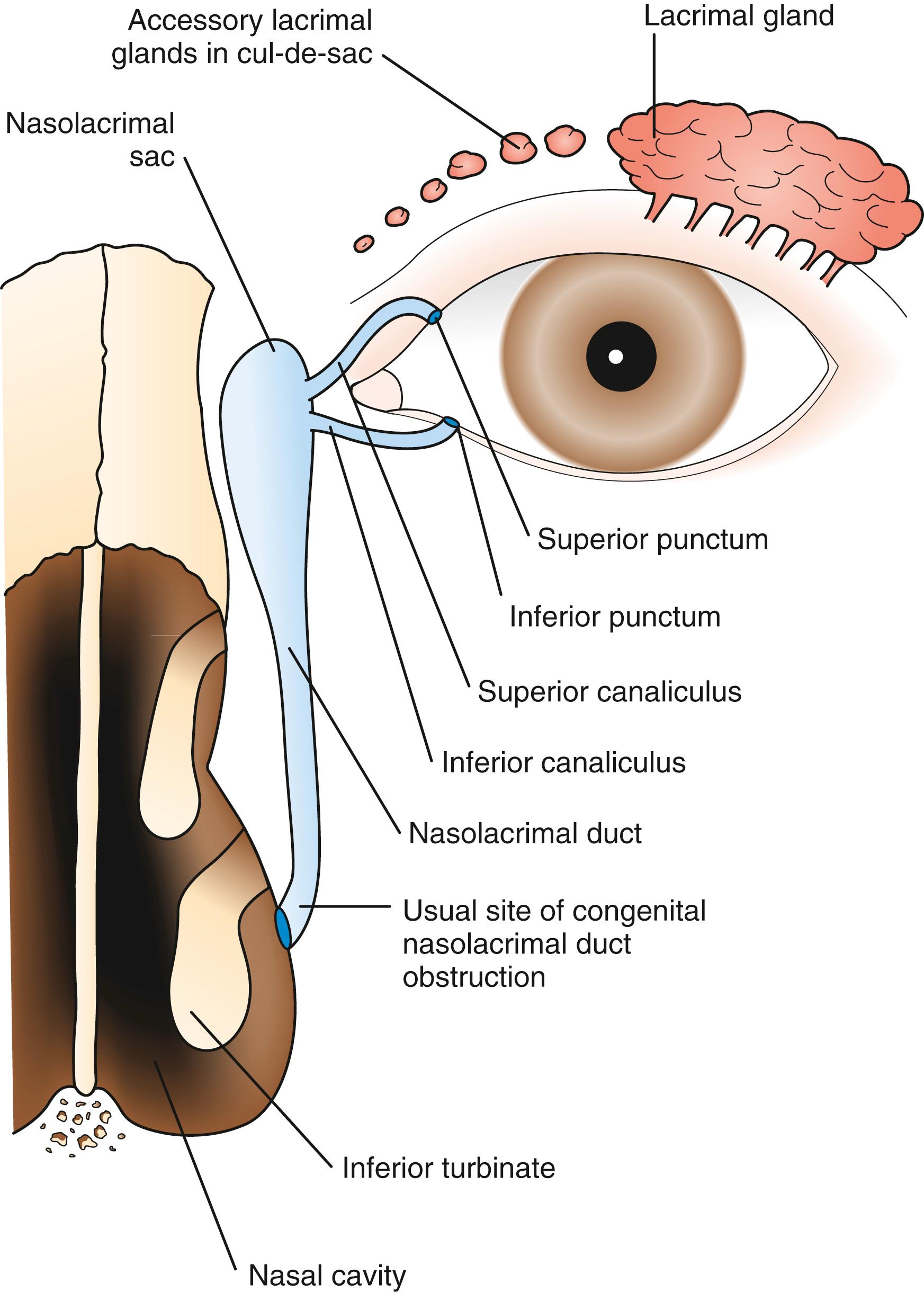
Lacrimal gland disorders: Agenesis of the lacrimal glands occurs rarely. Most lacrimal gland disorders are acquired and include acute viral dacryoadenitis ( Fig. 20.53 ). Chronic diseases such as sarcoidosis, Hodgkin disease, leukemia, and mononucleosis may produce lacrimal gland swelling with a palpable mass in the upper outer portion of the orbit.
Tears are drained from the eye by the superior and inferior puncta, which connect to the superior and inferior canaliculi (see Fig. 20.52 ). The canaliculi may unite into a common canaliculus before they enter the nasolacrimal sac, or they may enter the sac separately. The medial canthal tendon is anterior and superior to the nasolacrimal sac. Disorders of the lacrimal sac are then seen primarily inferior to the medial canthus, unless there is an overlying cellulitis. The sac is connected to the nasolacrimal duct, which is located in the nasal bone. The distal portion of the nasolacrimal duct enters the nasal antrum beneath the inferior turbinate.
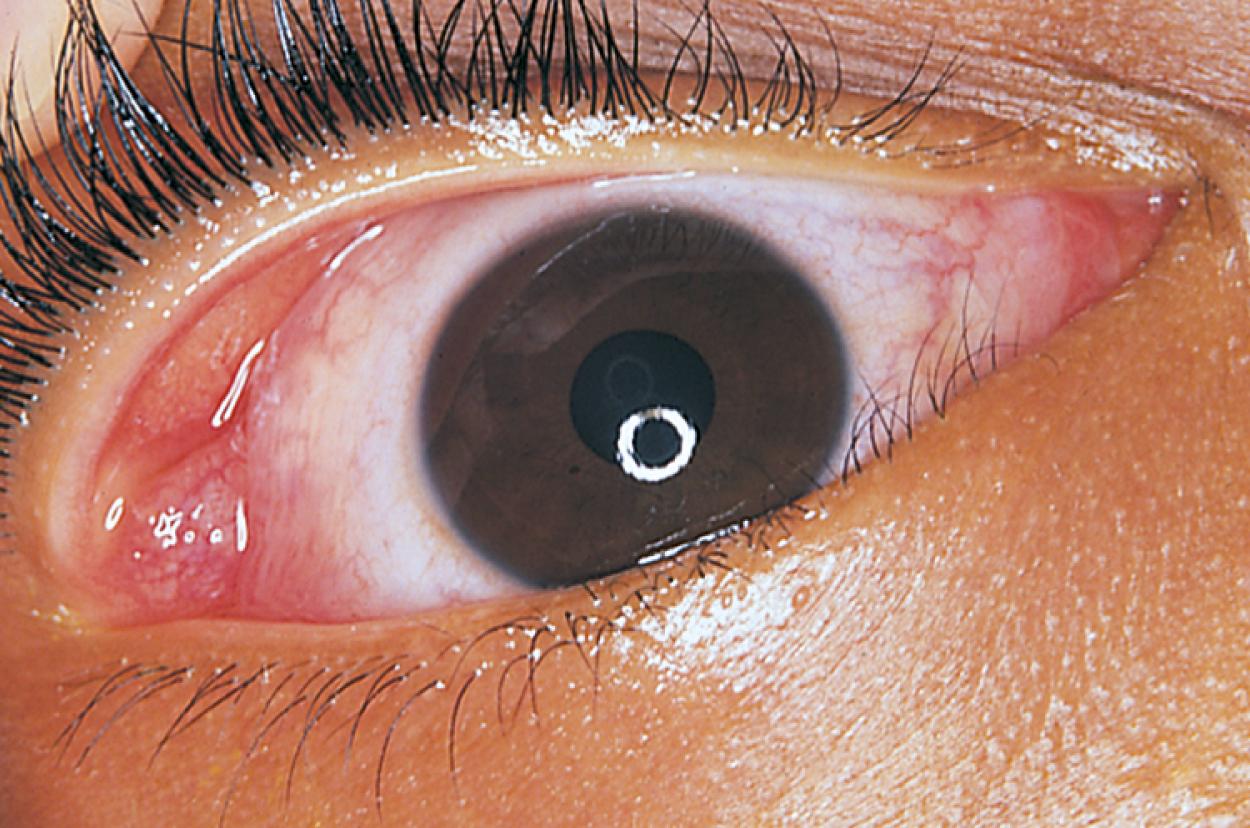
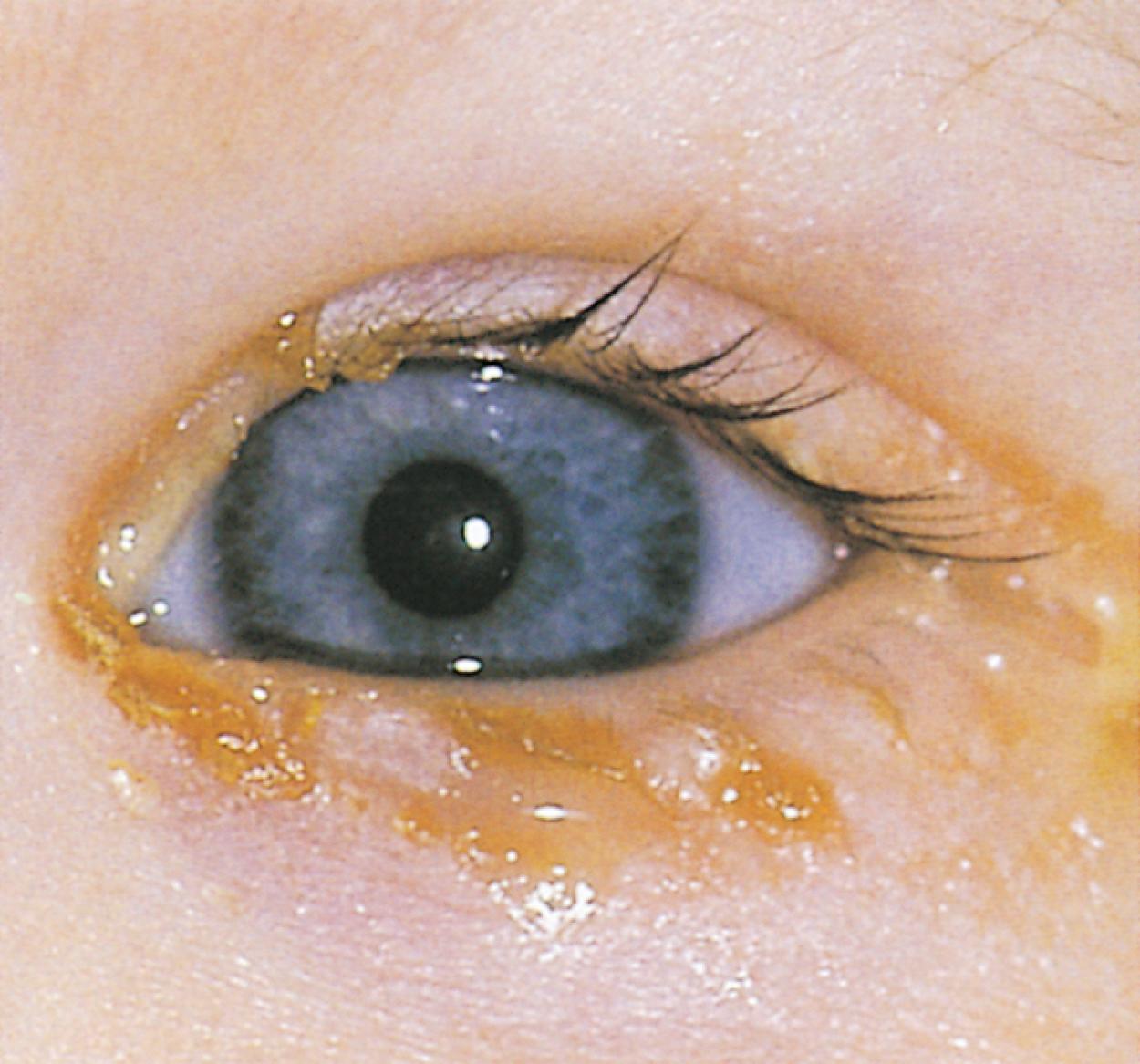
Congenital nasolacrimal duct obstruction or stenosis is present in 30% of newborns ( Fig. 20.54 ). Signs include tearing and mucopurulent discharge, which usually begins 3 to 5 weeks after birth, without conjunctival injection. A helpful diagnostic technique is to apply gentle pressure over the nasolacrimal sac to cause reflux of tears and mucopurulent material from the sac. Spontaneous resolution of the obstruction is common before 6 to 8 months of age. If the obstruction has not cleared by 8 to 10 months old, spontaneous resolution is much less likely, and the patient should be referred for probing of the nasolacrimal duct. Beyond 13 months old, the success rate of simple probing begins to decrease due to the recurring infections, which may cause scarring and stenosis of the nasolacrimal duct, increasing the need for more complicated procedures for treatment.
Rarely, the lacrimal sac becomes expanded due to the distal blockage and the child presents with a dacryocele ( Fig. 20.55 . An infected dacryocele is termed dacryocystitis. Urgent referral for treatment of dacryocystitis should be made to prevent expansion of infection to the surrounding tissues producing a periorbital cellulitis. Treatment is with lacrimal massage and systemic antibiotics if infected ( Fig. 20.56 ).


The conjunctiva is a mucous membrane that covers the posterior aspect of the eyelids. It is reflected into the cul-de-sac and extends onto the globe, where it fuses to the sclera at the corneal scleral limbus. The conjunctiva has goblet cells that contribute mucin to the tear film. When the eyelids are closed, the oxygen supplied by the blood vessels of the conjunctiva is responsible for maintaining oxygenation of the cornea. Conjunctivitis refers to inflammation of the conjunctiva. Infections of the conjunctiva may be bacterial or viral. The conditions that affect the conjunctiva may be due to inflammation (conjunctivitis), pigmentation, or elevated lesions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here