Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Echocardiography has greatly enhanced the field of cardiology. However, optimal use of echocardiography requires the ability to recognize and differentiate pathological conditions from normal cardiac structures and their variants that may simulate serious pathology. Although errors can occur with both transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE), they are especially common with TEE. Despite its superior image resolution—in fact, partly because of it—TEE is particularly prone to a variety of pitfalls. Several of these pitfalls are related to embryologic remnants, other to oblique views, and yet others to variants of normal structures. Categories of echocardiographic pitfalls are shown in Box 129.1 . A list of pitfalls that are discussed and illustrated in this subsection is shown in Box 129.2 .
Normal anatomy (e.g., pectinate muscles in the left atrial appendage)
Variants of normal anatomy (e.g., prominent eustachian valve)
Pathology that mimics potentially more serious pathology (e.g., atrial septal aneurysm, caseous mitral annular calcification, valve strands)
Ultrasound artifacts (e.g., reverberations, oblique and tangential “cuts”)
Crista terminalis
Eustachian valve
Chiari network
Lipomatous hypertrophy of atrial septum
Fat infiltration of the tricuspid annulus
Atrial septal aneurysm
Pectinate muscles in the LAA
Ridge between left upper pulmonary vein and LAA
Transverse sinus
Caseous calcification of mitral annulus
Atrial septal aneurysm
Tangential cut of left coronary cusp mimics vegetations/mass
Left coronary artery versus transverse sinus
Off-axis view mimics quadricuspid aortic valve
Valve excrescences
Artifacts mimicking aortic dissection flaps
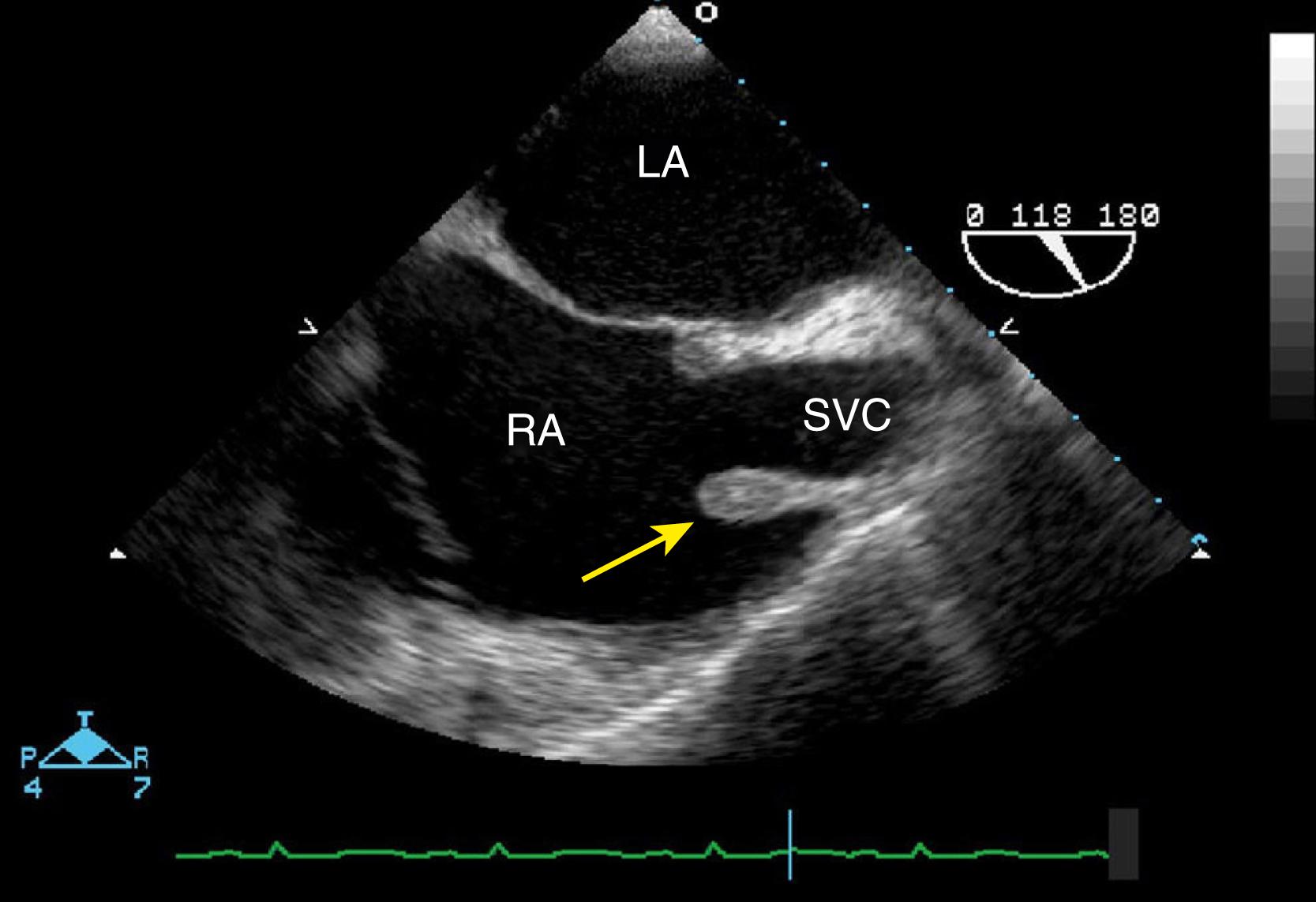
The crista terminalis (CT), or terminal ridge, is a crescent-shaped (or C-shaped) muscular ridge that spans from the anteromedial wall of the right atrium (just to the left of the orifice of the superior vena cava [SVC]) near the right atrial (RA) appendage toward the vicinity of the inferior vena cava (IVC). In some instances the crista terminalis merges with the valve of the IVC (eustachian valve [EV]). Its length is up to 4 to 5 cm, which decreases with age. The CT is derived from the regression of the embryologic septum spurium as the sinus venosus is incorporated into the RA wall. This process of regression varies widely, resulting in considerable variability in appearance in imaging modalities. , When it is prominent, this fibromuscular ridge can protrude into the RA cavity and resemble a mass, such as a neoplasm or thrombus. Thus, awareness of the variable and often prominent echocardiographic features of this structure can prevent the misdiagnosis of a “tumor.” In at least one case, the significance of this structure was not appreciated, resulting in unnecessary open heart surgery for removal of a presumed intracardiac tumor. Using the transesophageal echocardiographic bicaval view, the CT will appear as a protuberance originating from the SVC extending for a variable distance along the lateral RA wall ( Fig. 129.1 ). This anatomic structure has gained increased attention recently because the sinoatrial node lies in its superior aspect and its location is important for electrophysiologic studies. In addition, some authors have described the CT to be larger (greater in height, width, and area) in patients with atrial flutter (AFL) than in those without AFL. , , , Moreover, AFL and other reentry arrhythmias can be eliminated by ablation of the region of the CT.
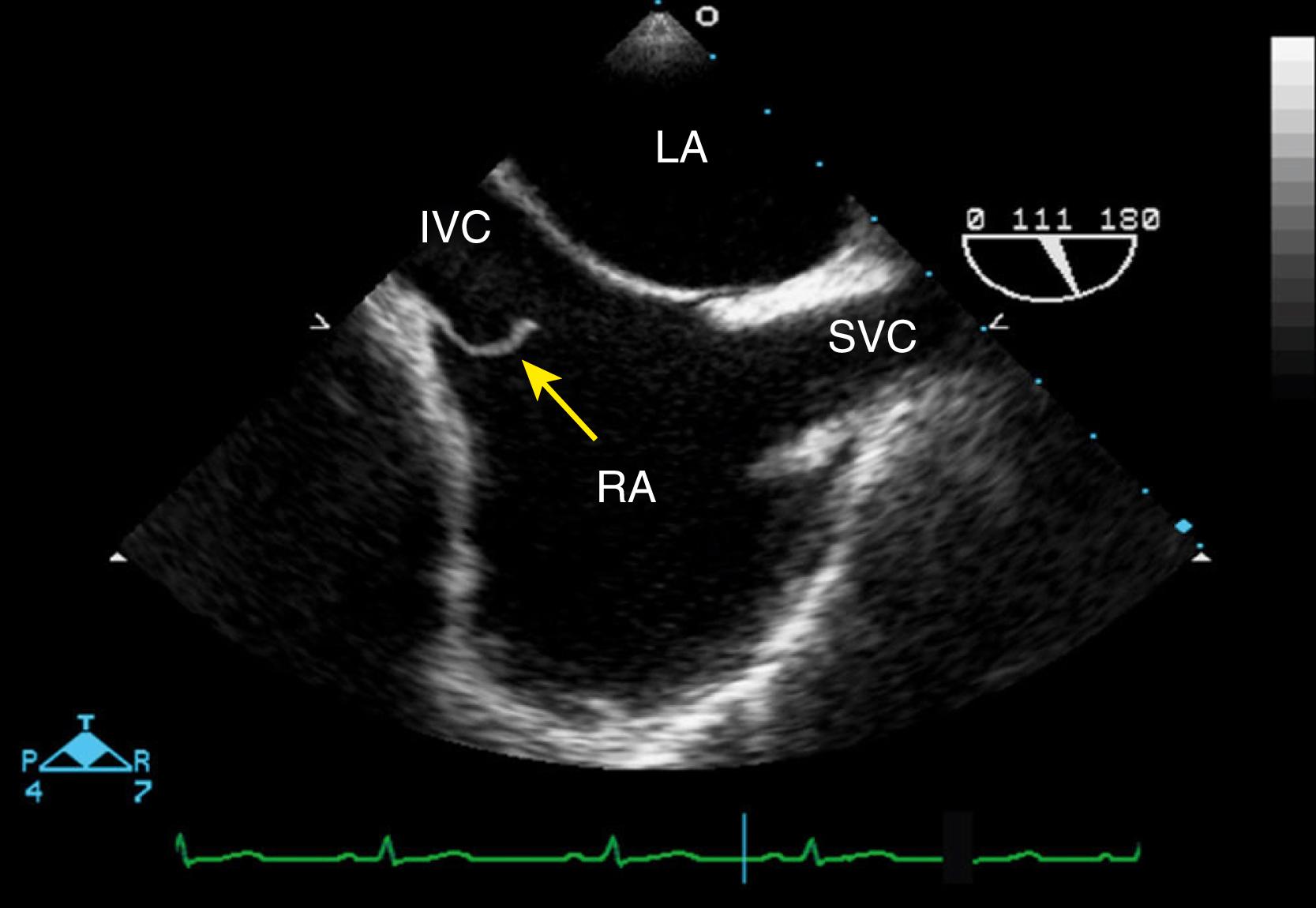
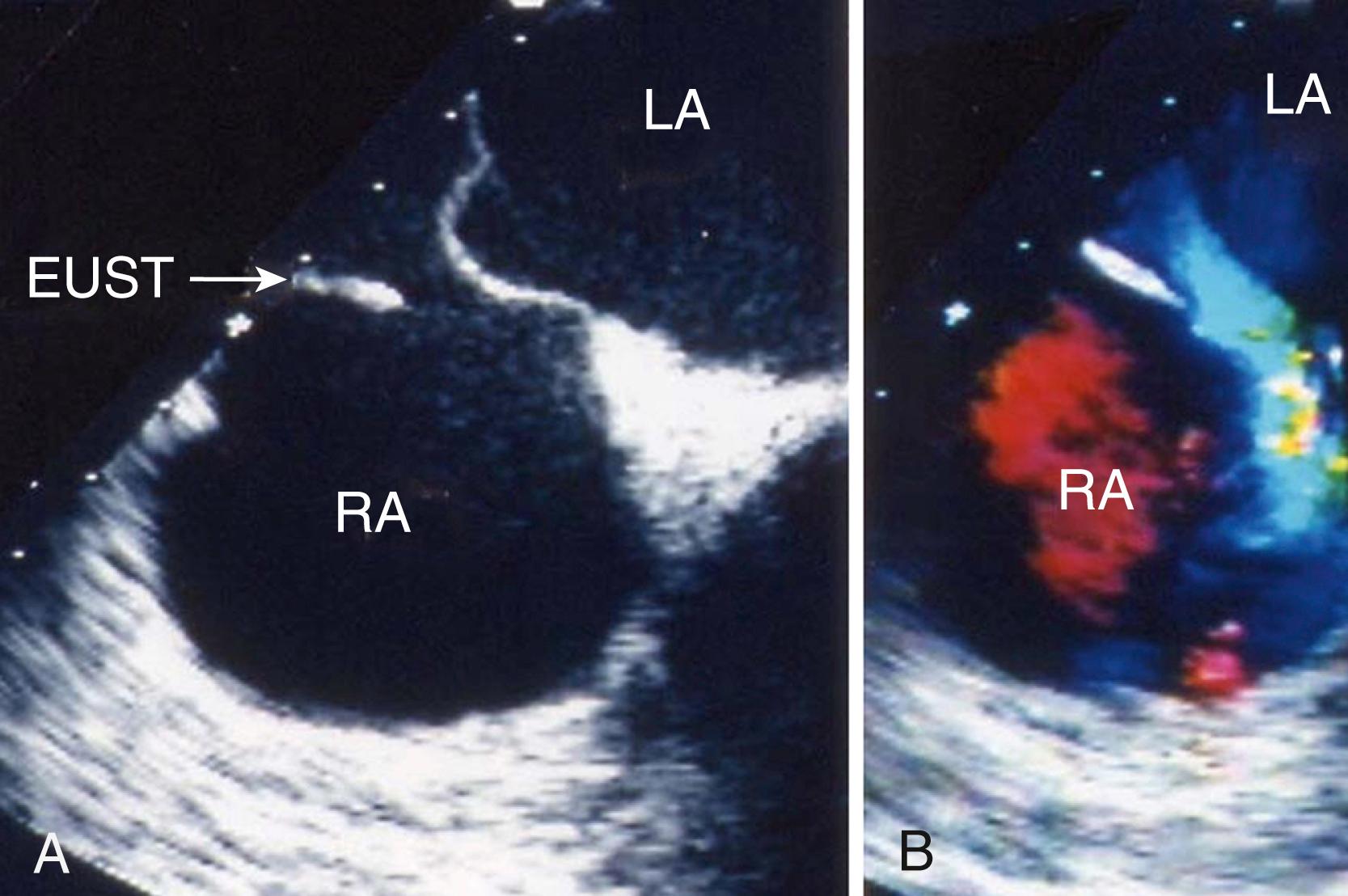
The EV, or valve of the inferior cava, is a remnant of the embryonic right valve of the sinus venosus. In the fetal circulation, the EV performs the important function of directing oxygenated blood from the IVC toward the foramen ovale and into the left atrium. The EV generally regresses during childhood but can persist into adulthood. Although usually vestigial or small, its size and shape in adults can vary considerably. In fact, Eustachius, writing in 1563, was the first to describe and classify its variations. There is also wide echocardiographic variability. At one end of the spectrum, the EV may be totally absent or present only as a thin ridge. Most commonly, it appears as a crescent fold of tissue arising from the anterior rim of the IVC and may be rigid or slightly mobile ( Figs. 129.2 and 129.3 ). At the other end of the spectrum, it appears as an elongated, mobile structure projecting several centimeters into the RA cavity, demonstrating an undulating motion. The average length of the EV has been reported to be 3.6 mm with a range of 1.5 to 22 mm. , On TEE, the EV is best visualized in the midesophageal four-chamber view or the midesophageal bicaval view, where it usually appears as an undulating flap of tissue where the IVC enters the right atrium. When prominent, it may be confused with an RA tumor, thrombus, or vegetation.
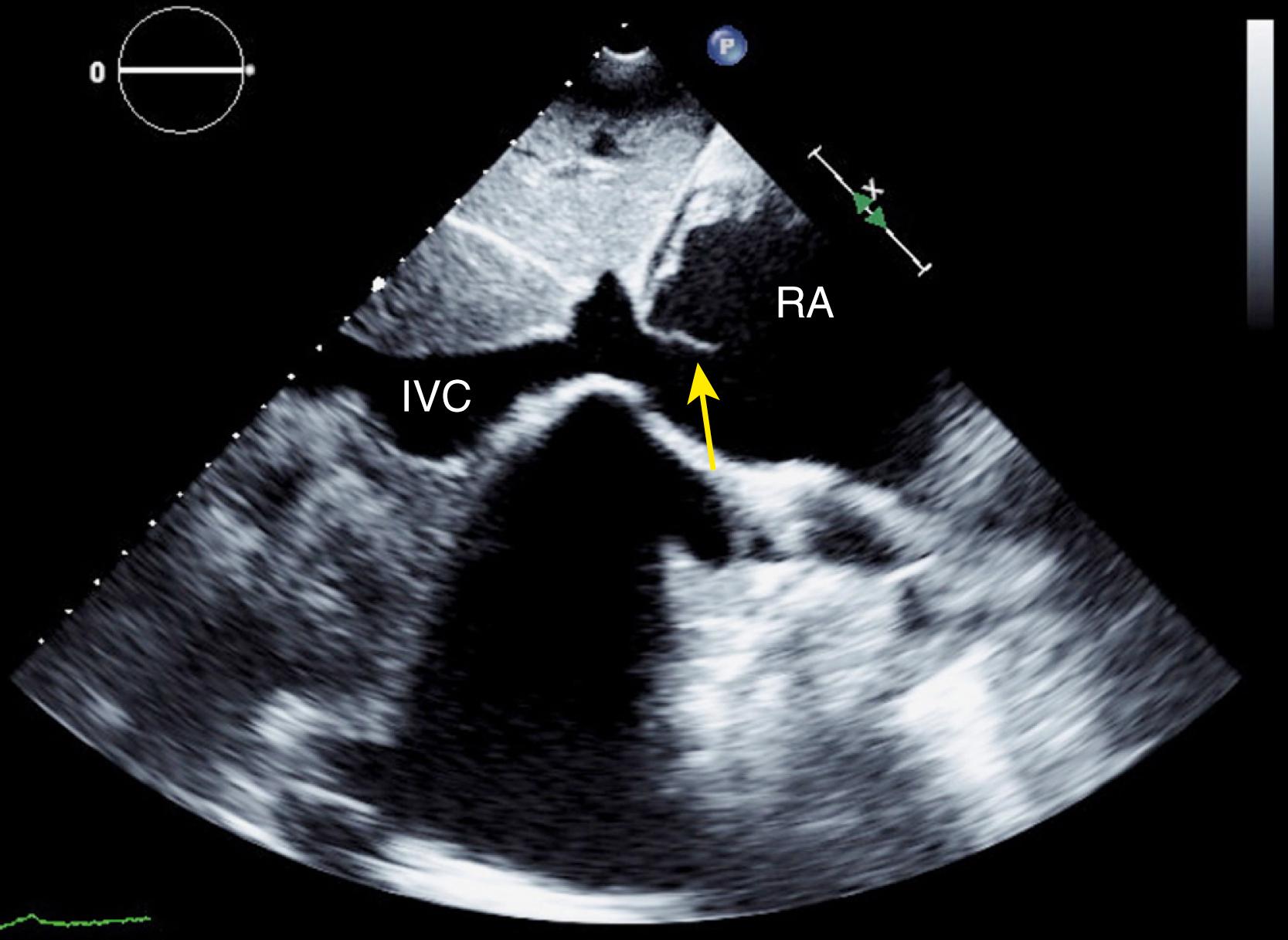
The EV, even when prominent, is a benign and incidental finding. However, complications have been reported. Endocarditis and thrombus formation are extremely rare complications. Even more rare, cases of RA myxoma or papillary fibroelastoma originating from the EV have been reported. Last, there have been reports of a prominent EV causing problems during catheter-based interventional procedures and even surgery, in which a prominent EV was mistaken for an atrial septal defect and inadvertently closed ( Fig. 129.4 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here