Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Interstitial keratitis (IK) is a rare but potentially blinding disease.
Telling symptoms of IK are nonulcerating inflammation and vascularization of the corneal stroma, notably without primary involvement of either the epithelium or the endothelium.
IK is a common endpoint for a number of diseases.
IK is a leading cause of blindness and loss of visual acuity around the world.
Topical therapy is generally effective, especially in the early phases of the disease.
Treatment should be specific to the causal agent. Systemic immunosuppression may be an option in refractory cases.
Interstitial keratitis (IK) is an uncommon and chronic disease. It presents as a nonulcerating inflammation of the corneal stroma further distinguished by cellular infiltration and neovascularization of the cornea. There is, notably, no primary involvement of the epithelium or the endothelium. British surgeon, ophthalmologist, dermatologist, venereologist, and pathologist Jonathan Hutchinson first described this stromal corneal reaction in patients with congenital syphilis in 1858.
The inflammatory response can be triggered by the direct invasion of microorganisms (bacteria, virus, fungus, or parasites) or by an immunologic reaction to exogenous and/or endogenous sources of antigens inside the corneal stroma.
Historically, IK has been classified as syphilitic or nonsyphilitic. Nonsyphilitic IK is described in this chapter, but syphilitic IK is covered separately in Chapter 84 because of its own very specific features.
Mycobacterium tuberculosis and Mycobacterium leprae are classified as acid-fast Gram-positive bacteria due to their lack of an outer cell membrane. Mycobacteria can be classified into several major groups for purposes of diagnosis and treatment: M. tuberculosis complex, which can cause tuberculosis (TB), and M. leprae , which causes Hansen disease or leprosy. Nontuberculous mycobacteria can cause pulmonary disease resembling TB, lymphadenitis, skin disease, or disseminated infection.
TB is an infectious disease caused by the bacillus M. tuberculosis , typically affecting not only the lungs (pulmonary TB), but also extrapulmonary sites. The disease is spread by aerosol when people who are sick with pulmonary TB expel bacteria. M. tuberculosis enters the body primarily via inhalation. Macrophages deliver the bacilli to the lymphatic system, where they gain access to the bloodstream. Hematogenous spread to the eye can result in uveitis, choroiditis, retinal vasculitis, conjunctivitis, scleritis, and keratitis.
TB remains one of the world’s deadliest diseases, killing 1.5 million of the estimated 9 million people affected in 2013.
In terms of geographic distribution, more than half (56%) of the 9 million lived in Southeast Asia and the Western Pacific Regions; one- quarter lived in Africa, which had (and still has) the highest percentage of cases and deaths relative to population. India and China alone accounted for 24% and 11% of total cases, respectively.
HIV plays an important role. Of the 9 million people who developed TB that year, 1.1 million (13%) were HIV positive. Of the 1.5 million who died, 360,000 (24%) were HIV positive. Africa accounted for four out of every five HIV-positive TB cases and deaths among people who were HIV positive.
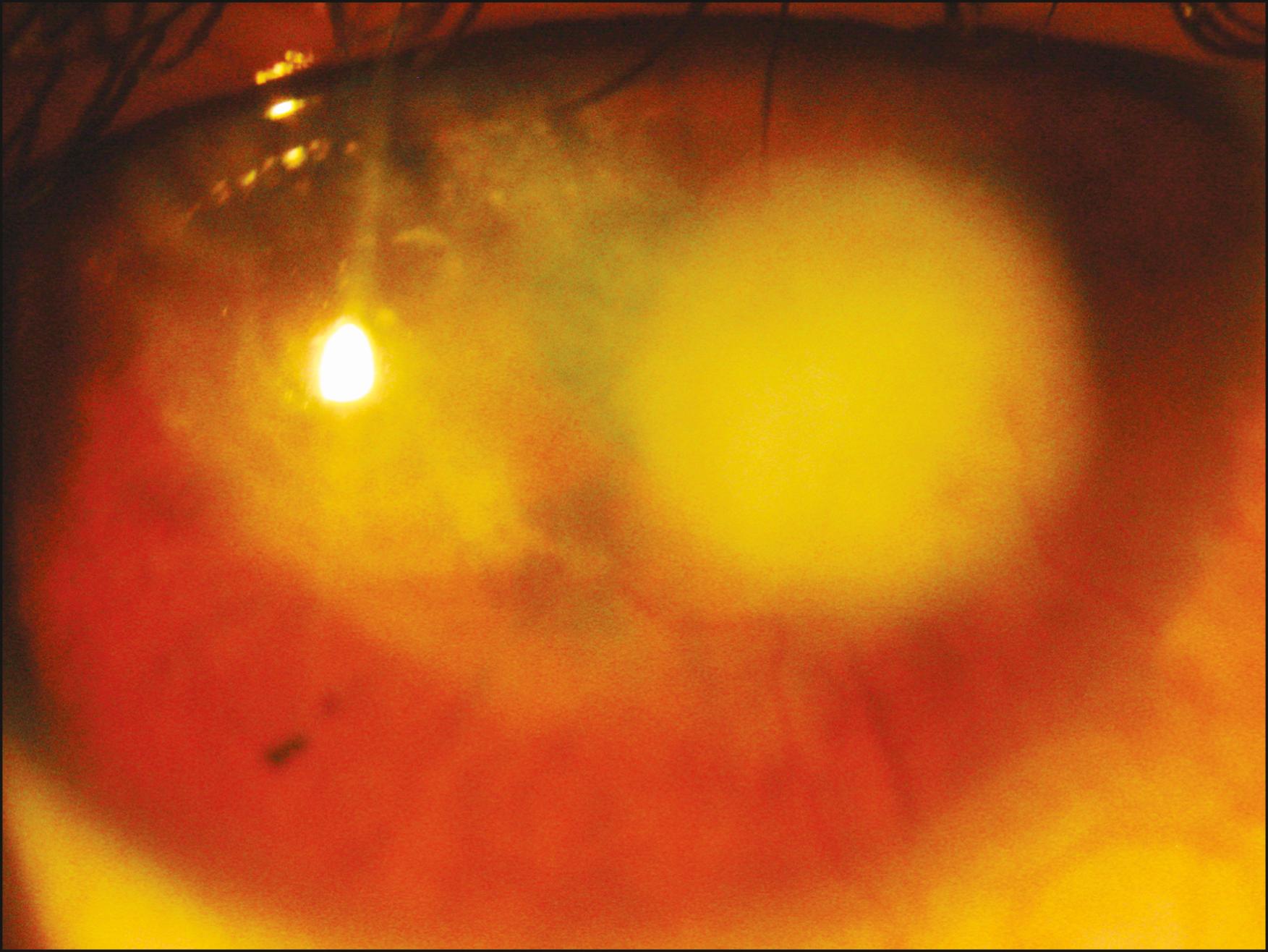
Primary ocular TB is an extremely rare event. IK is usually associated with systemic TB. The process involves the anterior or posterior corneal stroma with neovascularization and lipid deposition. Photophobia, tearing, and hyperemia are common features in the acute phase due to the local inflammatory reaction. Late stages are marked by corneal scarring and loss of transparency and eventually the compromise of best corrected visual acuity ( Fig. 85.1 ).
Nonpulmonary sites tend to be more common among children and those with impaired immunity. To diagnose extrapulmonary TB, appropriate specimens, including pleural, pericardial, or peritoneal fluid or biopsy specimens, lymph node tissue, bone marrow, bone, blood, urine, brain, or cerebrospinal fluid, should be obtained. These specimens should then be tested using acid-fast bacillus (AFB) staining and mycobacterial culture, along with drug susceptibility testing. Tissue specimens should also be examined microscopically after routine and AFB staining; however, the absence of AFB or granulomas, or even failure to culture M. tuberculosis , does not exclude the diagnosis of TB.
The most commonly used diagnostic tool for TB is the Mantoux test or tuberculin skin test, in which tuberculin protein is injected just below the skin of the inside forearm. The size of the skin reaction determines whether the test results are significant. A false-positive test can occur in patients previously vaccinated with the bacille Calmette-Guérin (BCG) vaccine. Although BCG is seldom used in the United States, it is widely employed in countries with high TB infection rates. False-negative results may occur in certain populations who may not respond to the TB skin test such as children, the elderly, and patients with AIDS. A false-positive can also occur in individuals recently infected with TB but whose immune systems have not yet reacted to the bacteria.
After a positive skin test, it may be necessary to obtain a chest x-ray or CT scan to demonstrate pulmonary infiltration. Following a positive result x-ray or CT scan, samples of the sputum must be tested for TB bacteria and can also be used to test for drug-resistant strains of TB.
Samples of sputum or other secretions can be submitted to staining with Ziehl-Neelsen or Auramine and/or cultured on Löwenstein-Jensen medium. PCR techniques are also used in developing countries but are not routine. ,
TB blood tests may be used to confirm or rule out latent or active TB. A blood test may be useful if the patient is at high risk for TB infection but has had a negative skin test.
Interferon-γ release assays (IGRAs) are used to diagnose TB infection. IGRAs cannot distinguish between latent infection and active tuberculous disease and should not be used as a sole method for the diagnosis of active TB, which requires a microbiologic diagnosis. Two IGRAs approved by the US Food and Drug Administration (FDA) and available in the United States are the QuantiFERON-TB Gold In-Tube test (QFT-GIT) and the T-SPOT.TB test (T-Spot). QTF-GIT is an ELISA-based, whole-blood test that uses peptides from three TB antigens (ESAT-6, CFP-10, and TB7.7) in an in-tube format. The result is reported as quantification of Interferon-gamma(IFN-γ) in international units (IU) per mL. An individual is considered positive for M. tuberculosis infection if the IFN-γ response to TB antigens is above the test cutoff (after subtracting the background IFN-γ response in the negative control). ,
The final criterion for the diagnosis of TB can be defined as a combination of clinical, radiologic, and microbiologic data.
Recently, a task force supported by the American Thoracic Society, the Centers for Disease Control and Prevention (CDC), and the Infectious Diseases Society of America established clinical practical guidelines to diagnose TB in adults and children using the Grading, Recommendations, Assessment, Development, and Evaluation (GRADE) approach.
This task force supported the IGRA rather than TB skin test (TST) for diagnostic testing for latent TB infection in most cases. They support TST as an acceptable alternative where IGRA is not available, too costly, or too burdensome. For testing for TB disease, they recommend AFB smear microscopy in all patients suspected of having pulmonary disease as well as liquid and solid mycobacterial cultures, nucleic acid amplification test (NAAT) and other molecular tests, and histologic examination of specimens collected from sites suspected of extrapulmonary TB.
The currently recommended CDC treatment for new cases of drug-susceptible TB is a 6-month regimen (26 weeks) of four first-line drugs—isoniazid, rifampicin, ethambutol, and pyrazinamide—with success rates of 85% or more for new cases. Treatment for multidrug-resistant TB (MDR-TB), defined as resistance to isoniazid and rifampicin, is longer and requires more expensive and toxic drugs. For most patients with MDR-TB, the current regimens recommended by the World Health Organization (WHO) last 20 months, and treatment success rates are much lower.
A number of new drugs are being looked at as add-on therapy to the current drug-resistant combination treatment including Bedaquiline, Delamanid, PA-824, Linezolid, and Sutezolid. ,
IK associated with TB can be treated locally with adjuvant topical steroids to hasten resolution of corneal inflammation along with cycloplegia to reduce pain and photophobia.
Leprosy is a chronic infectious disease caused by M. leprae , the first bacterium to be identified as causing disease in man, and described by the Norwegian physician Gerhard Armauer Hansen in 1873. Infection with the organism affects the skin, peripheral nerves, upper respiratory tract mucosa, and the eyes, among other structures.
According to the WHO, the global registered prevalence of leprosy at the end of the first quarter of 2013 was 189,018 cases, while the number of new cases detected during 2012 was 232,857.
Leprosy can be classified on the basis of clinical manifestations and skin smear results. In the classification based on skin smears, patients with negative smears at all sites are grouped as having paucibacillary leprosy (PB), while those with positive smears at any site are grouped as having multibacillary leprosy (MB).
Among many forms of clinical presentation, lepromatous and tuberculous forms are common. Lepromatous leprosy occurs secondarily to defective cell-mediated immunity against the organism and is characterized by widespread dermal and neural disease and predominant CD8+ lymphocyte involvement. In contrast, tuberculous leprosy is manifest primarily with nerve involvement and minimal skin disease. CD4+ lymphocytes are observed in typical granuloma formations. These mycobacteria accumulate in cooler tissues such as the cornea, typically in the lepromatous or MB form of disease. Ocular findings include punctate epithelial keratopathy, corneal hypesthesia, corneal pannus, corneal nerve involvement, focal avascular keratitis, and IK.
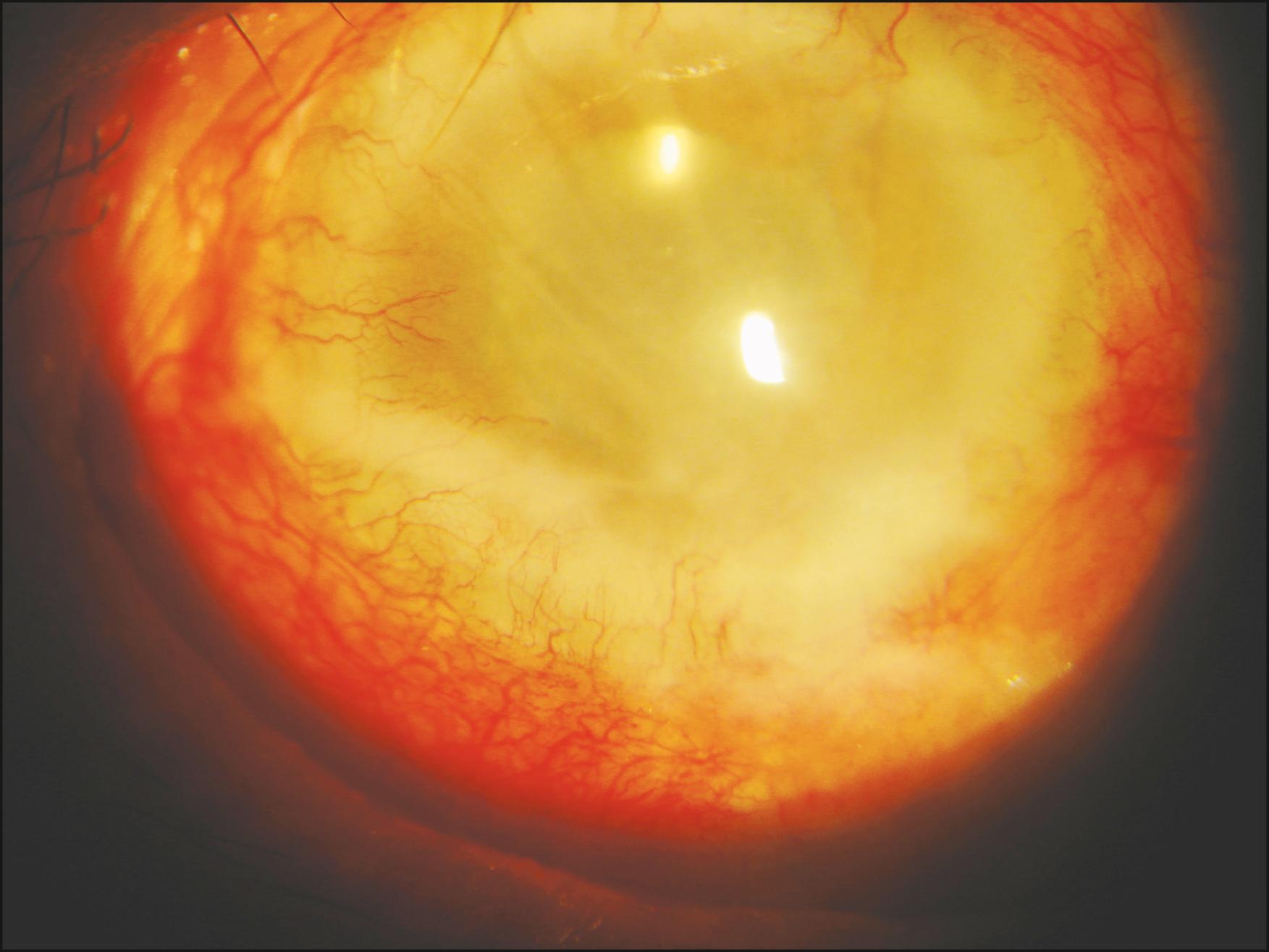
Corneal involvement in leprosy is generally bilateral, and the presence of bacilli throughout the stroma supports an infectious rather than an immunologic etiology. The superior cornea is often involved primarily with deep infiltration of lymphocytes, macrophages, and M. leprae organisms accompanied by stromal edema, which may progress to involve the central cornea.
Vascularization may occur as a late sequel of disease, and corneal opacification is permanent, should it occur ( Fig. 85.2 ). The comorbidity of corneal nerve involvement may contribute to the poorer prognosis.
The treatment of leprosy proposed by the WHO includes a combination of rifampicin, clofazimine, and dapsone for patients with MB leprosy and rifampicin and dapsone for patients with PB leprosy. Rifampicin is the most important antileprosy drug and is, therefore, included in the treatment of both types of leprosy. Treatment of leprosy with only one antileprosy drug will result in the development of drug resistance and is considered unethical.
Topical corticosteroids for IK and cycloplegics for uveitis can be prescribed with careful monitoring of the corneal epithelium for neurotrophic and neuroparalytic disease as well as for toxic reactions.
Lyme disease is caused by the bacterium Borrelia burgdorferi and is transmitted to humans through the bite of infected black-legged Ixodes ticks. The CDC affirms that Lyme disease is the most commonly reported vector-borne illness in the United States. In 2013, it was the fifth most common nationally notifiable disease; however, this disease is not distributed nationwide and is concentrated heavily in the Northeast and upper Midwest.
Typical initial clinical signs include fever, headache, fatigue, and a characteristic skin rash called erythema migrans (stage 1). If left untreated, infection can spread to the joints, heart, and nervous system (stages 2 and 3). Ocular signs manifest during stages 2 and 3, although a follicular conjunctivitis can be seen in stage 1. Ocular inflammatory signs occur in stage 3 and include episcleritis, keratitis, uveitis, vasculitis, exudative retinal detachment, and endophthalmitis.
Although keratitis is not a common feature of Lyme disease, the inflammatory pattern is interstitial. Involvement is usually bilateral, although it may present in one eye only. IK is characterized by multiple poorly defined or nebular stromal opacities. These infiltrates have indistinct borders, can be present throughout the corneal stroma, and do not profoundly affect visual acuity. Unlike other forms of IK, stromal edema is not a common feature. Late vascularization and keratic precipitates with uveitis have been reported. Most cases of keratitis were empirically treated with topical corticosteroids, while one in three untreated patients developed edema, vascularization, and corneal haze. Late administration of corticosteroid drops remained effective. Administration of topical corticosteroids appears to prevent the progression of inflammation to vascularization and scarring; however, appropriate systemic antibiotic treatment must be given.
The diagnosis is based on symptoms, physical findings, and the possibility of exposure to infected ticks in endemic areas.
Laboratory testing is helpful if used correctly and performed with validated methods. The serologic laboratory tests most widely available and employed are the Western blot and ELISA. A two-tiered protocol is recommended by the CDC: the sensitive ELISA test is performed first, and if it is positive or equivocal, then the Western blot is run. , Due to frequent false-positive results, PCR is not widely performed for the diagnosis of Lyme disease. New laboratory tests have been suggested such as the Lymphocyte Transformation Test (LTT-MELISA), but the results of studies are contradictory.
Systemic therapy depends on the individual affected and the stage of the disease. Oral doxycycline (first choice, except in children younger than 8 years of age and women who are pregnant or breastfeeding), amoxicillin, cefuroxime, and azithromycin are the antibiotics of choice.
Intravenous administration of ceftriaxone (2 g once per day intravenously for 14 days; range, 10–28 days) is recommended as the first choice in symptomatic cardiac disease, refractory Lyme arthritis, or neurologic symptoms from meningitis or encephalitis.
Approximately 10%–20% of patients treated for Lyme disease with a recommended 2- to 4-week course of antibiotics have lingering symptoms of fatigue, pain, or joint and muscle aches. In some cases, these symptoms can last for more than 6 months. Although often called “chronic Lyme disease,” this condition is properly known as “posttreatment Lyme disease syndrome” (PTLDS).
Prevention of Lyme disease includes the use of insect repellent, prompt removal of ticks, application of pesticides, and reduction of the tick habitat.
Acanthamoeba is a free-living eukaryotic organism that can cause rare but severe infections of the eye, skin, and central nervous system. Its life cycle includes two vital forms: trophozoites (the mobile and active form) and cysts (the immobile, resistant form).
In the United States, an estimated 85% of cases occur in contact lens users exposed to homemade saline solutions or contaminated water from swimming pools, hot tubs, lakes, or bathtubs. , For people who wear contact lenses, certain practices can increase the risk of Acanthamoeba keratitis: storing or handling lenses improperly; disinfecting lenses improperly (using tap water or topping off solutions when cleaning the lenses or lens cases); swimming, using a hot tub, or showering while wearing lenses; or otherwise coming into contact with contaminated water. A history of trauma to the cornea can also increase risk. ,
Initial ocular symptoms are nonspecific and include foreign body sensation, photophobia, tearing, and blurred vision.
Although a superficial epitheliopathy is an early feature, stromal involvement ensues with infiltration accompanied by edema, which is sometimes mistaken for herpetic stromal disease. At this stage of interstitial inflammation, diagnostic possibilities are vast, and if the patient does not have a history of contact lens wear or freshwater exposure ( Table 85.1 ), the diagnosis may not be obvious. If careful examination of the corneal epithelium reveals a band of intra- and intercellular edema and instability with poor adhesion to the underlying basement membrane, this would suggest the need for diagnostic scrapings and culture using specific media that support Acanthamoeba . The corneal infiltrates progress and often coalesce into frank abscesses in a circumferential pattern (ring infiltrate) characteristic of the disease. Stromal neovascularization is typically not an early finding.
| Disease | Synonym | Agent (Vector) | Endemic Areas | Pertinent History | Characteristic Corneal Findings |
|---|---|---|---|---|---|
| Acanthamoeba keratitis | None | Acanthamoeba | Worldwide | Contact lens wear/abuse, freshwater exposure | Pain out of proportion to findings. Radial keratoneuritis, early superficial epitheliopathy, stromal infiltration and edema without early stromal neovascularization, late ring infiltrate |
| Onchocerciasis | River blindness | Onchocerca volvulus (blackfly) | West and Central Africa, Latin America, Yemen | Travel to endemic areas | Live microfilariae, peripheral stromal edema, centripetal full-thickness stromal vascularization, complete opacification, absence of thinning |
| Leishmaniasis | Baghdad boils, sandfly disease | Leishmania spp. (sandfly) | Asia, Africa, Latin America, Mediterranean | Travel to endemic areas | Focal or diffuse interstitial keratitis with deep neovascularization, late thinning, histologic findings of organisms, and granulomatous inflammation |
| African trypanosomiasis | African sleeping sickness | Trypanosoma brucei (tsetse fly) | Africa | Travel to endemic areas | Diffuse neovascularization, severe scarring and thinning, potential perforation |
| Microsporidiosis | None | Microsporidia | Worldwide | Immunocompromised status | Anterior to midstromal infiltration |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here