Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nonimmune hydrops fetalis results from many etiologies.
Management involves correcting the underlying cause.
The condition is associated with significant morbidity and mortality.
Some etiologies are amenable to treatment in utero.
A newborn with hydrops has an abnormal accumulation of fluid. The condition varies from mild, generalized edema to massive anasarca with effusions in multiple body cavities and with peripheral edema so severe that the extremities are fixed in extension. Fetuses with severe hydrops may die in utero; if liveborn, they may die in the neonatal period from the severity of their underlying disease or from severe cardiorespiratory failure.
The first description of hydrops in a newborn twin may have appeared in 1609. Ballantyne suggested that the finding of hydrops was an outcome from many different causes, in contrast to the belief at that time that hydrops was a single entity. Potter was the first to make the distinction between nonimmune hydrops and hydrops secondary to erythroblastosis fetalis by describing a group of infants with generalized body edema who did not have hepatosplenomegaly or abnormal erythropoiesis. Potter's description of more than 100 cases of hydrops included two sets of twins in which one had hydrops and the other did not, thus presenting the first description of twin–twin transfusion syndrome. With the nearly universal use of anti-D globulin and refinement of the schedule and doses for its administration, the occurrence of immune-mediated hydrops has steadily declined and may be as low as 6% to 10% of all cases of hydrops.
Determining the incidence of nonimmune hydrops in the general population is difficult because of biases in the pregnancy cohorts selected, as well as the accuracy of coding for nonimmune hydrops in those pregnancies. Most published studies come from single institutions with the at-risk populations ranging from that of a high-risk pregnancy clinic to infants in a neonatal intensive care unit and generally predating the more routine use of ultrasound investigation in the late first trimester of pregnancy. Incidence rate of hydrops reported in those studies has been highly variable and generally higher than other studies, ranging from 6 per 1000 pregnancies in a high-risk referral clinic in the United Kingdom between 1993 and 1999 to 1 in 4000 pregnancies, 6 per 1000 pregnancies, 1.3 per 1000 pregnancies, and 1 per 1700 pregnancies. Two recent publications using population-based data found lower overall rates: a recent publication from Sweden using more than 1.9 million births extracted from the Swedish Birth Register for 1997–2015 found 309 cases of nonimmune hydrops at birth, which corresponded to an incidence of 1.6 per 10,000 births, while data from California identified 1037 cases using ICD-9CM diagnosis codes from 4,090,950 live births, which corresponded to an incidence of 2.5 per 10,000 births between 2005 and 2012. However, these lower rates may suffer from lack of information on fetuses who died in utero and from potential undercoding of the disorder in live birth infants. Geography also affects the incidence; for example, several causes of nonimmune hydrops, such as α-thalassemia, are more common in certain areas of the world. Hence, the actual incidence of nonimmune hydrops likely falls within a wide range of values reported from population and single center-based estimates.
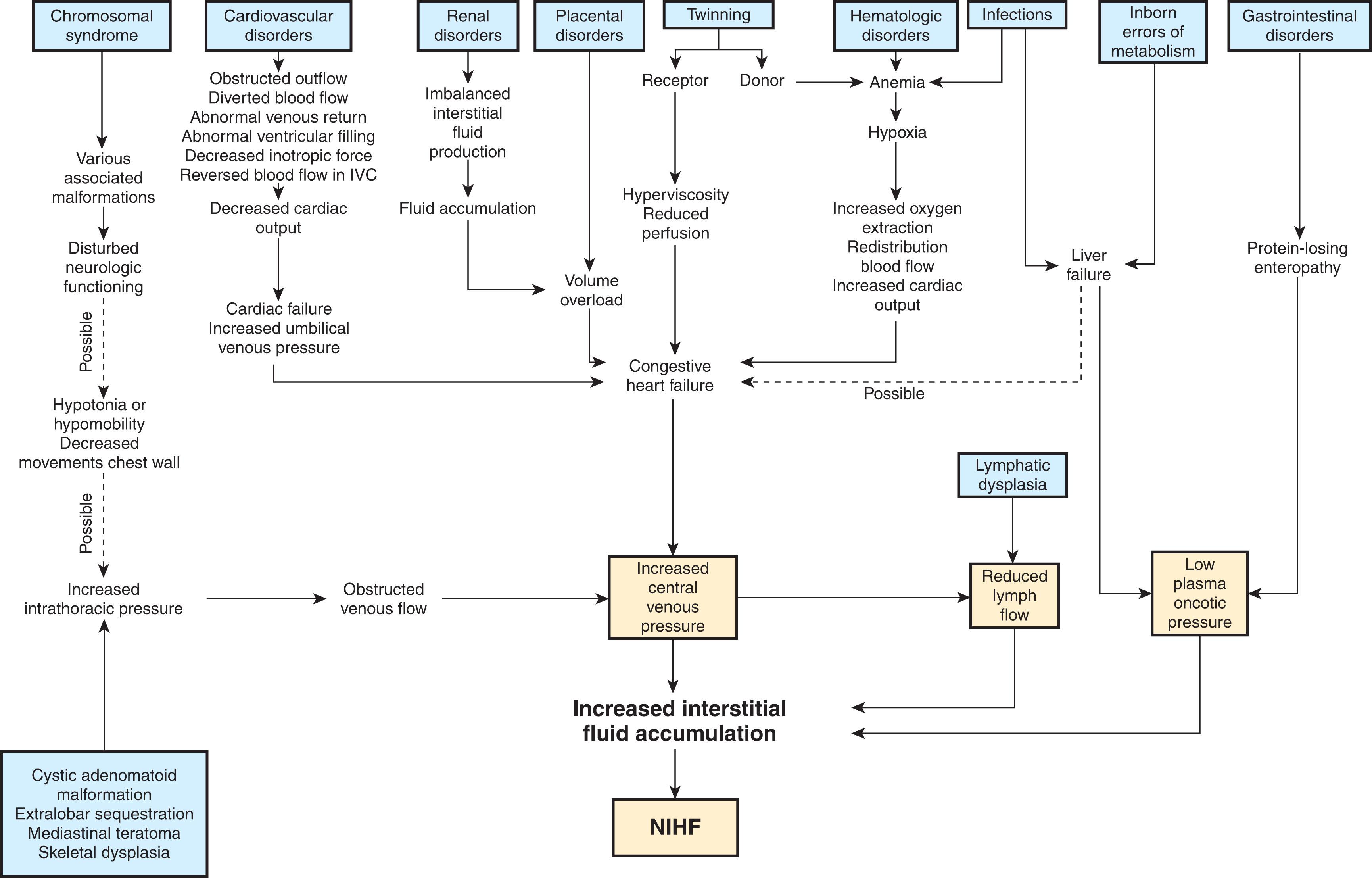
Nonimmune hydrops has been associated with a wide range of conditions (see Table 7.1 ). In many of these conditions, edema formation results from one of the following possible processes:
Elevated central venous pressure (CVP) in which the cardiac output is less than the rate of venous return
Anemia, resulting in high-output cardiac failure
Congenital lymphatic flow disorder
Capillary leak
| Condition Type | Specific Conditions |
|---|---|
| Hemolytic anemias |
|
| Other anemias |
|
| Cardiac conditions |
|
| Cardiac arrhythmias |
|
| Vascular malformations |
|
| Vascular accidents |
|
| Infections |
|
| Lymphatic abnormalities |
|
| Nervous system lesions |
|
| Pulmonary conditions |
|
| Renal conditions |
|
| Chromosome abnormalities |
|
| Bone diseases |
|
| Gastrointestinal conditions |
|
| Tumors |
|
| Maternal or placental conditions |
|
| Miscellaneous |
|
| Idiopathic |
The actual pathophysiology of hydrops for many of the conditions in Table 7.1 , however, is still not understood.
The most common causes of nonimmune hydrops are chromosomal, lymphatic, cardiovascular, hematologic, thoracic, infectious, and conditions related to twinning. As with reported incidence rates, the relative contribution of these causes varies by study. The studies that focus on early fetal presentation of hydrops (postconceptional age of less than 24 weeks’ gestation) have found that chromosomal abnormalities, such as Turner syndrome and trisomies 13, 18, and 21, contribute 32% to 78% of all cases of hydrops. For fetuses whose hydrops becomes evident after 24 weeks’ gestation, cardiovascular and thoracic causes are most prevalent, with rates ranging between 30% and 50%. Studies from Asia have noted a higher percentage of cases from hematologic causes, probably because of the higher rates of α-thalassemia in the population.
A review of studies published between 2008 and 2013 suggests a potential change in the etiologies of nonimmune hydrops when compared with studies published between 1979 and 2008. These more recent studies reported a higher rate of lymphatic etiologies (15.0% compared with 5.7% in older studies) and a lower rate of thoracic or chromosomal etiologies. Idiopathic hydrops, or hydrops of unknown etiology, remained constant at between 18% and 20% of all cases. As with older studies, papers published between 2008 and 2013 varied widely in the prevalence of specific etiologies depending on the ability of the clinicians to complete their diagnostic evaluation, geography, and the inclusion of fetal deaths in the analysis. ⁎ * Finally, population-based data from California births between 2005 and 2012 found similar etiological results for live-born infants. Aneuploidy was found in 116 of 1037 infants with nonimmune hydrops (11.2%), lymphatic causes in 9.2% of all cases, and 29.1% of cases with a diagnosis of hydrops of unknown etiology. It is likely that with increased understanding and the availability of genetic testing for many of the conditions listed in Table 7.1 , the number of infants diagnosed with idiopathic, nonimmune hydrops will continue to decline.
Abnormal body fluid homeostasis is the underlying cause of edema, whether localized or generalized. To understand the pathogenesis of hydrops, the clinician must consider the forces underlying normal fluid homeostasis that underpin a general pathophysiologic pathway for this disorder ( Fig. 7.1 ) as proposed by Bellini et al. The regulation of net fluid movement across a capillary membrane depends on the Starling forces, which were first described by E. H. Starling. Flow between intravascular and interstitial fluid compartments is determined by the balance among (1) capillary hydrostatic pressure, (2) serum colloid oncotic pressure, (3) interstitial hydrostatic pressure or tissue turgor pressure, and (4) interstitial osmotic pressure, which depends on lymphatic flow. The Starling equation defines the relationship among these forces and their net effect on net fluid movement, or filtration, across a semipermeable membrane (such as the capillary membrane) as:
where K = capillary filtration coefficient, representing the extent of permeability of a membrane to water and thus describing capillary integrity; P c = capillary hydrostatic pressure; P t = interstitial hydrostatic pressure or tissue turgor pressure; R = reflection coefficient for a solute, representing the extent of permeability of the capillary wall to that solute; O p = plasma oncotic pressure as determined by plasma proteins and other solutes; and O t = interstitial osmotic pressure ( Fig. 7.2 ).
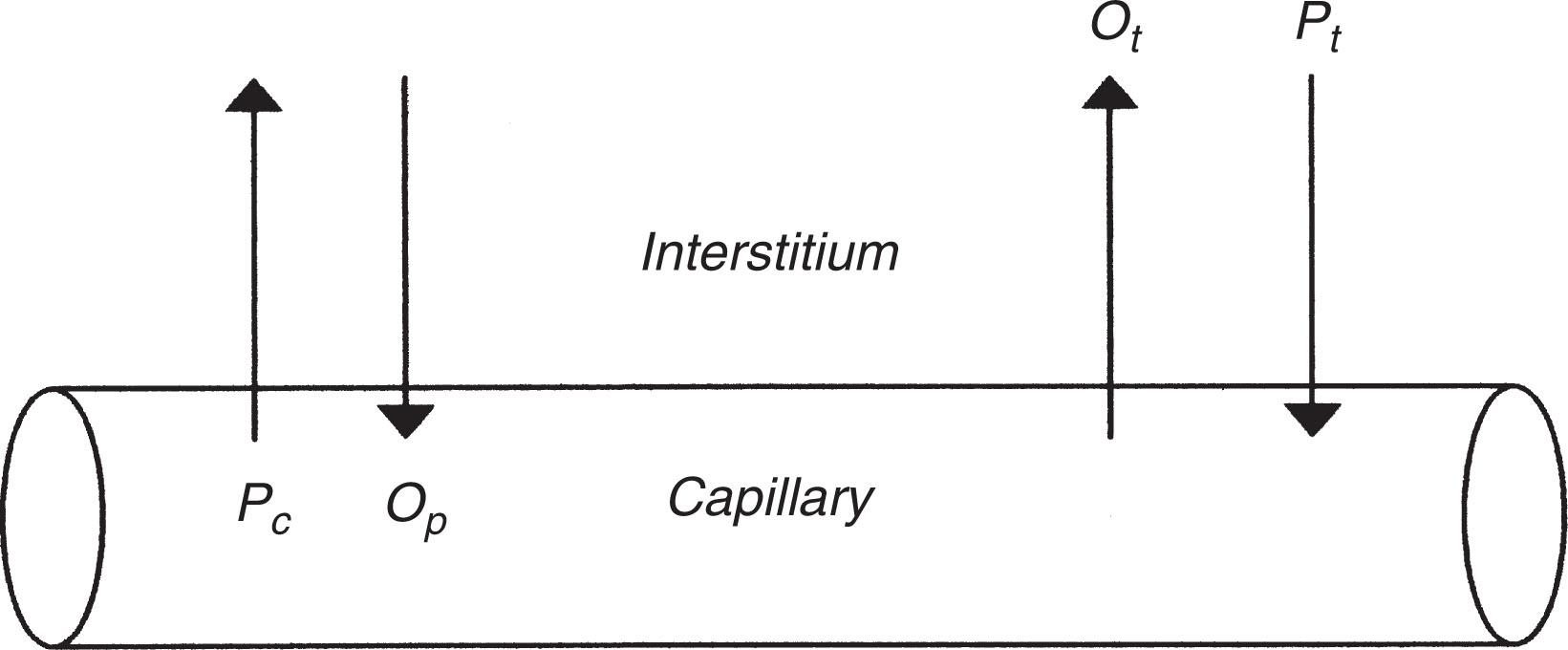
Although an abnormality of any of the components of this equation may, in theory, result in the accumulation of edema fluid, the fetal–placental unit presents a unique physiologic condition that effectively eliminates two of the factors, assuming unimpeded fetal–placental flow and an appropriately functioning maternal–placental interface. Because approximately 40% of fetal cardiac output is allocated to the placenta, there is rapid transport of water between the fetus and mother. Any condition resulting in elevated fetal capillary hydrostatic pressure or low plasma colloid oncotic pressure would likely cause the net flow of water from fetal villi in the placenta to the maternal blood stream where it can be effectively eliminated. This elimination of fluid would counteract the accumulation of interstitial fluid by the fetus. Although the placenta of a fetus with hydrops is also edematous, these changes are believed to occur with, and not before, fetal fluid accumulation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here