Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nausea and vomiting (NV) are common symptoms representative of numerous etiologies; however, persistent symptoms of intractable NV are highly sensitive of GI disorders on the gastroparetic spectrum. Due to common prevalence of these symptoms in the general population, gastroparesis is often misdiagnosed in the clinical setting. These symptoms become problematic if recurrent or chronic, as they interfere with nutrition, functional status, and quality of life (QOL). Intractable vomiting can result in complications such as severe gastritis, electrolyte imbalances, nutritional deficits, erratic blood glucose levels, prolonged hospitalizations, and Mallory-Weiss tears, gastric electrical stimulation (GES) has been shown to effectively reduce symptoms of NV in patients with medication-refractory gastroparesis.
The use of neurostimulation of the gastrointestinal (GI) tract has been practiced for the last century. Discoveries of the enteric nervous system (ENS) and understanding of the physiology of the GI tract has facilitated advancements in neurostimulation. The first advancement dates back to 1911 when William H. Dieffenbach placed electrodes in the rectum in attempts to treat constipation, ileus, and atony. In , Bilgutay et al. applied neurostimulation to the stomach by placing electrodes on the distal end of a nasogastric tube to induce motility, in efforts to treat postoperative ileus. In the 1980s, implantable pulse generators (IPG) were developed by investigators working with Medtronic, Inc., and others for neurostimulation for abdominal pain, with use in gastric motility stimulation over the past decade.
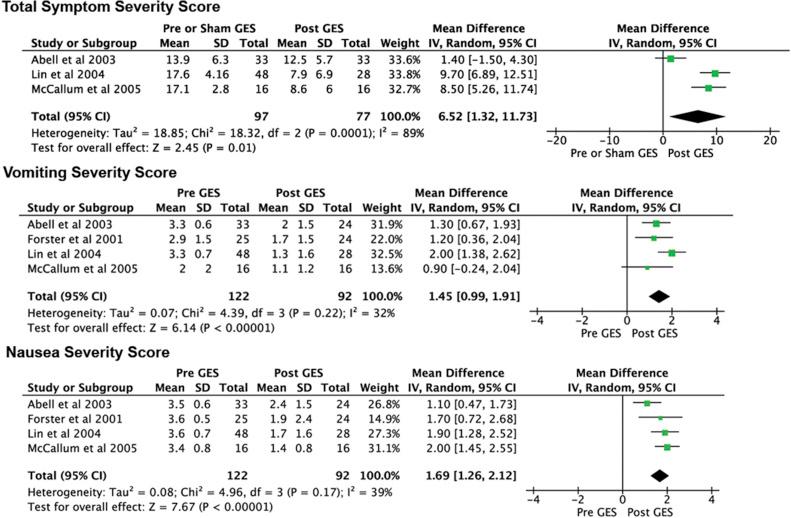
Neurostimulation of the ENS in the stomach has been used by two approaches. The first approach utilizes pulse frequencies, to mimic the physiologic frequencies seen in normal intestinal physiology, with higher energy. This is an attractive approach but is not currently commercially available. Another, more popular strategy utilizes frequencies several times higher than natural GI physiology with lower energy. Initial investigations showed great promise for a high-frequency approach, which was then developed into a device called Enterra produced by Medtronic, Inc. ( ). The device was granted Humanitarian Device Exemption by the US Food and Drug Administration (FDA) for use in gastroparesis. Meta-analysis of 13 studies using Enterra therapy for gastroparesis revealed substantial benefits of high-frequency, low-energy neuromodulation ( ). Parameters studied included total symptom severity, vomiting and nausea severity, gastric emptying, mental composite score, physical composite score, and need for parenteral or enteral nutrition. All factors besides weight were significantly improved with GES ( Fig. 118.1 ) ( ). Another meta-analysis focusing on diabetic gastroparesis yielded similar results ( ).
Implantation of a temporary GES is an increasingly common therapy, which serves as a strong predictor of response to permanent GES implantation ( ). Temporary GES is most commonly done endoscopically with placement of a stimulator in the musculature of the greater curvature of the stomach ( ).
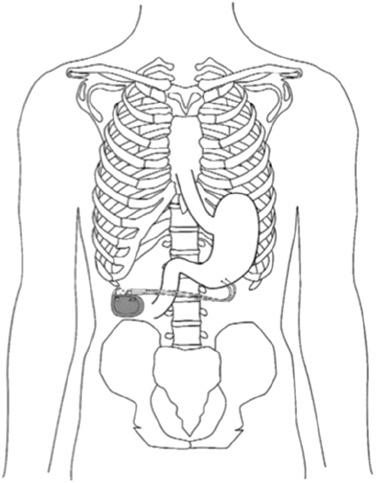
Permanent placement of a gastric stimulator device incurs typical risks and costs associated with surgery ( ). Permanent GES units include a pair of electrodes connected to an IPG. The electrodes are implanted into the muscularis propria along the greater curvature of the stomach, 10 cm proximal to the pylorus, and 1 cm apart ( Fig. 118.2 ) ( ). The IPG is then implanted in the subcutaneous tissue in the right mid-quadrant of the abdominal wall.
Placement of a gastric stimulating device has shown instant antiemetic effects with subsequent improvement in gastric emptying ( ). Studies have also shown overall improvement in NV, irrespective of normal or delayed gastric emptying ( ). In one study, 20 of 22 responders to temporary GES went on to receive permanent placement of GES, with 90% of those reporting response to treatment at continued follow-up ( ). At present, no guidelines exist for temporary GES placement, but they remain in development.
Implantation of a gastric stimulator functions to alter the muscle contractions of the stomach. Those who suffer from the gastroparetic spectrum have shown promising improvements in the most common symptoms of gastroparesis including chronic nausea, vomiting, and bloating. Gastric stimulators can improve the outcomes in those with delayed gastric emptying and inversely can slow motility in those with rapid gastric emptying ( ). Additional utility of these devices includes regulation of cytokine production ( ), increased pancreatic function ( ), temporary gastric stimulation in postoperative ileus ( ), and improved glycemic control in diabetics ( ).
Delayed gastric emptying without evidence of mechanical obstruction defines motility disorders. According to the American Neurogastroenterology and Motility Society, abnormal, solid gastric emptying is defined as greater than 90% gastric retention after 1 h, at least 60% retention after 2 h, and greater than 10% retention after 4 h ( ). These individuals can present with a variety of symptoms; however, the most common symptom upon presentation include nausea (92%), vomiting (84%), and bloating (75%) ( ), as with traditional gastroparesis. Other common features include early satiety and abdominal pain. Due to common prevalence of these symptoms in the general population, those with gastric emptying pathology often receive misdiagnoses of gastroesophageal reflux disease (GERD) and dyspepsia. An alternative way of describing patients with the symptoms of gastroparesis, but without delayed gastric emptying, is the gastroparesis-like syndrome (GLS). A 425-patient study evaluating those with chronic NV noted a group of patients with normal gastric emptying but symptoms and patient profiles indistinguishable from gastroparetics ( ).
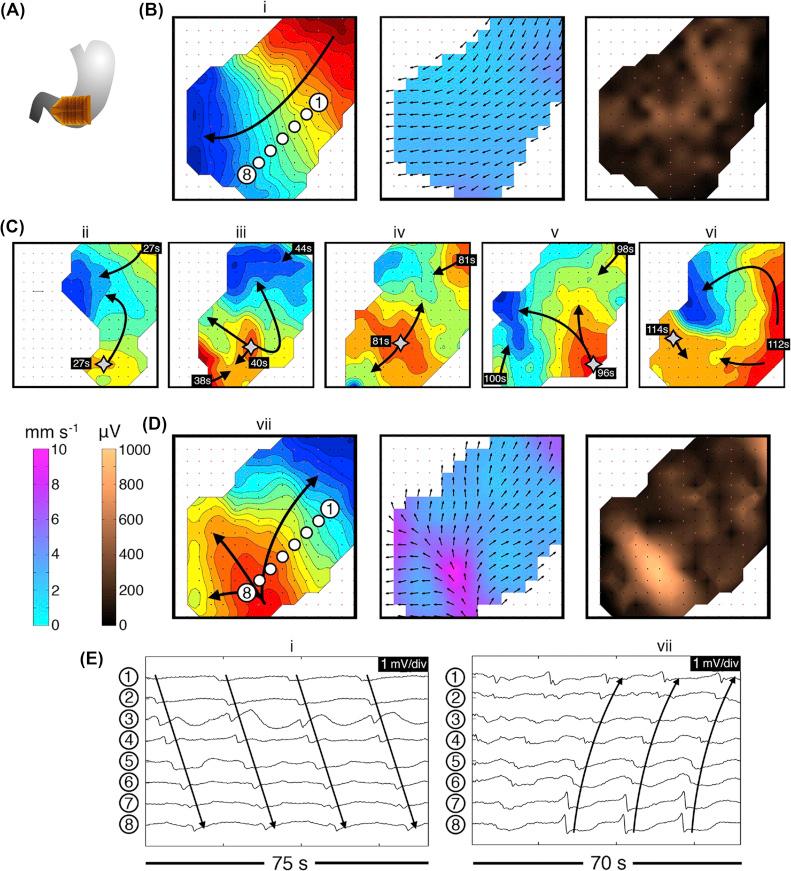
Those with gastroparesis or GLS have known abnormal electrophysiology evidenced by studies using transcutaneous recordings, intraoperative recordings, and new modalities that use hundreds of small electrodes to show motility parameters ( Fig. 118.3 ) ( ). Transmural biopsies of those with gastroparesis revealed reduced or absent interstitial cells of Cajal (ICC), which are identified as the pacemaker cells of the GI tract ( ). Additionally, the same high-resolution methodologies and use of biopsies to evaluate electrophysiology in gastroparesis has been used in GLS.
Despite frequent misdiagnosis, current estimations have the incidence of gastroparesis at 9.6 per 100,000 individuals for men, and 37.8 per 100,000 in women ( ). Due to an increasing prevalence of diabetics in the United States, gastroparetic disorders will provide an increasingly large burden on the patient population. The cause of gastroparesis is often multifactorial, but the most common etiologies include diabetic neuropathy, gastroparesis secondary to diabetes mellitus (DM), malignancy-associated, postsurgical, Parkinson’s-related, and idiopathic.
The condition is diagnosed by exclusion of mechanic obstructions and the use of gastric emptying scintigraphy. This study uses egg meal with technetium and radionucleotide signaling to determine rate of gastric emptying ( ). The speed of gastric emptying in these syndromes is often classified as delayed, normal, or rapid. GLS patients have identical symptoms to gastroparesis patients, except they exhibit nondelayed, solid gastric emptying. Some of these patients had delayed emptying of liquids but not solids, whereas others had rapid gastric emptying ( ). The variability in emptying parameters that is seen with classical gastroparesis and the GLS suggest a spectrum of gastroparetic disorders, which could be known as the gastroparesis syndromes.
Initial treatment of symptoms includes nutritional support (caloric supplementation, enternal tube feeds with jejunostomy, or total paraenteral nutrition), use of prokinetic medications, the use of antiemetic medication to control nausea, and pain management ( ). For patients, refractory to conservative treatments, neurostimulation using a temporary GES may be indicated. Other less successful methods of treating gastroparesis include total enteral nutrition, gastrostomy, pyloric injections of botulinum toxin, pyloroplasty, and variations of gastric resection ( ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here