Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Current rates of anesthetic complications are low regardless of the type of anesthesia (general, regional, or local). Yet among the complications that may occur, those affecting the nervous system are perhaps the most feared ( Table 55-1 ). This chapter reviews anesthetic-related perioperative neurologic problems as well as perioperative complications that are not caused by anesthesia but are often erroneously attributed to it. Considerations regarding the challenges of anesthesia in patients with established neurologic disease are considered but are discussed in more detail in Chapter 54 .
| General Anesthesia |
| Postoperative coma and delayed awakening |
| Postoperative delirium |
| Postoperative cognitive dysfunction |
| Seizures |
| Malignant hyperthermia |
| Worsening or relapse of pre-existing neurologic disease |
| Ischemic optic neuropathy |
| Regional Anesthesia |
| CNS toxicity |
| Postoperative cognitive dysfunction |
| Seizures |
| Headache after dural puncture |
| Epidural hematoma |
| Epidural abscess |
| Neuropathy |
| Transient pain in buttocks and legs |
| Worsening or relapse of pre-existing neurologic disease |
| Ischemic optic neuropathy |
| Transient hypoacusis |
| Cranial nerve palsies |
| Local Anesthesia |
| Neuropathy |
Failure to arouse and delayed awakening are the most common early neurologic problems following general anesthesia. True prolonged postoperative coma is relatively uncommon, with estimates ranging from 0.005 to 0.08 percent following general surgery, but with higher rates reported after cardiac surgery. Advanced age, urgent surgery, pre-existing brain disorders, perioperative hypotension, postoperative organ failure, and sepsis are independently associated with postoperative coma.
Delayed emergence from anesthesia is the most common cause of early failure to regain alertness after surgery; although this situation is benign, more serious alternative causes include stroke, hypoxic-ischemic brain injury, and status epilepticus. Sepsis and multiorgan failure may produce severe encephalopathy and prolong unresponsiveness, sometimes for days after their resolution. The main causes of impairment of consciousness following surgery are found in Table 55-2 .
| Prolonged Anesthetic and Analgesic Effect |
| Advanced age |
| Decreased metabolism and clearance |
| Toxic Encephalopathy |
| Perioperative drugs (e.g., benzodiazepines, opiates, serotoninergic agents) |
| Drug interactions |
| Metabolic Encephalopathy |
| Renal failure |
| Liver failure |
| Hypercapnia and hypoxia |
| Hypoglycemia |
| Hyponatremia and other electrolyte abnormalities |
| Hyperosmolality |
| Acidemia |
| Septic Encephalopathy |
| Acute stroke |
| Ischemic |
| Thromboembolism |
| Fat embolism |
| Air embolism |
| Hemodynamic hypoperfusion |
| Hemorrhagic |
| Seizures and status epilepticus (convulsive and nonconvulsive) |
| Hypoxic/ischemic global brain injury |
When a neurologist is asked to evaluate an unresponsive patient following surgery, the principal goal is to determine whether any form of severe acute neurologic disease is responsible. It is therefore important to obtain a detailed history of the patient’s preoperative status, review pertinent intraoperative information, and clarify the condition of the patient since surgery. In these situations, direct communication with the anesthesia and surgical teams may provide additional relevant information, such as the presence of clinical features suggesting seizure occurrence or a history of immediate awakening followed by unconsciousness, the latter suggesting cerebral embolism or seizures. It should be determined whether the patient during or immediately after surgery became hypoxemic, hypotensive, or had marked lability of blood pressure; profuse blood loss; poor hemostasis; or cardiac arrhythmias. Intraoperative hypotension and fluctuations in hemodynamic parameters are common in patients with postoperative coma following cardiovascular surgery.
The general clinical examination is important. A slow respiratory pattern and darkened skin color raise the possibility of CO 2 narcosis. An irregular pulse may signify atrial fibrillation and its increased risk of postoperative stroke. Splinter hemorrhages in the conjunctiva or nail bed suggest fat embolism after long-bone fracture surgery. The neurologic examination should focus on the assessment of level of consciousness, brainstem reflexes, gaze (conjugate versus dysconjugate, presence of skew deviation), eye movements (roving, ocular dipping or bobbing, nystagmoid jerks), muscle tone, response to central (sternal or supraorbital) and peripheral (limb) pain, and presence of adventitious movements. The presence of lateralizing signs requires brain imaging. Brainstem findings or bilateral focal signs should raise suspicion of basilar thromboembolism, prompting vessel imaging. Subtle abnormal movements of the eyes, facial muscles, or fingers may be the only manifestations of underlying status epilepticus and necessitate urgent electroencephalography (EEG). Drug toxicity should be suspected in patients with rigidity, hyperreflexia, and tremors, with or without concurrent fever. Myoclonus may occur with any toxic or metabolic encephalopathy, but can also follow severe global brain anoxia. Asterixis may be a sign of hyperammonemia but also occurs in other metabolic encephalopathies and as a side effect of medications. In patients lacking motor responses following pharmacologic neuromuscular blockade, it must be determined—sometimes by nerve-stimulation studies—whether blockade is continuing; when paralysis is persistent, administration of an antidote may require consideration.
Additional testing is directed by the history and physical findings. If the examination is reassuring and nonfocal, further investigations can be postponed. Brain imaging is indicated in patients with new focal deficits. Computerized tomography (CT) scan is reliable for the detection of acute hemorrhage and can document territorial ischemic infarctions and massive brain edema. Magnetic resonance imaging (MRI) may be necessary to diagnose an embolic shower and subtle manifestations of global hypoxic-ischemic injury such as early cortical injury. In patients with brainstem signs, MRI of the brain can be combined with MR angiography to exclude vertebrobasilar occlusion. EEG should be reserved for those with suspected seizures, and the use of continuous monitoring may increase the diagnostic yield. Lumbar puncture is rarely necessary in patients with postoperative encephalopathy unless central nervous system infection is suspected. Serum studies should be used judiciously, including arterial blood gas to exclude CO 2 retention, as well as determination of glucose, sodium, creatinine and blood urea nitrogen, and ammonia to exclude various metabolic disturbances.
A history of delayed arousal after a previous surgery makes a diagnosis of delayed emergence from anesthesia more likely. Older age and renal and hepatic insufficiency may compromise drug metabolism and clearance, increasing the risk of delayed arousal. Review of the anesthesia course may guide the use of naloxone (for reversal of opioid effect), flumazenil (to reverse benzodiazepines), and physostigmine (to reverse neuromuscular blockade) in appropriate cases.
The prognosis of patients with postoperative coma varies markedly depending on etiology. Although the prognosis is favorable in patients with reversible toxic or metabolic causes, the mortality may exceed 80 percent in patients with multifocal infarctions revealed by brain MRI. In survivors of prolonged postoperative coma, long-term functional outcome is frequently poor.
Postoperative delirium is common, with a reported incidence as high as 40 to 60 percent of patients. Delirium can occur immediately following anesthesia or after some interval from a seemingly normal recovery from the anesthetic; the latter is more commonly persistent and often multifactorial in etiology. The risk of delirium is increased in the elderly and in patients with previous cognitive impairment, a history of substance use (including alcohol), and those receiving polypharmacy before surgery and narcotics or benzodiazepines perioperatively. A previous episode of postoperative delirium predicts recurrence. Perioperative hypoxemia and hemodynamic instability, profuse intraoperative blood loss, and postoperative organ failure may also increase the risk of postoperative delirium. There is limited evidence that the type and route of anesthesia influence the risk of postoperative delirium, with higher rates following general anesthesia.
Evaluation of patients with postoperative delirium begins by considering risk factors for its development (see Table 54-2 in Chapter 54 ). Time should be spent reviewing the medications that the patient was taking prior to surgery and those administered during and after the operation. Toxic and metabolic factors are the most frequent causes. Exclusion of acute structural brain injury, seizures, and meningoencephalitis (a rare cause of perioperative coma) is the primary responsibility of the consulting neurologist. Primary neurologic diagnoses to be considered include ischemic infarctions (often bilateral or in the brainstem), intracranial hemorrhage (intraparenchymal, subdural, or rarely subarachnoid), nonconvulsive status epilepticus, and posterior reversible encephalopathy syndrome.
Management of delirium depends on its cause. Discontinuation of sedatives and narcotics is often the only intervention required. When agitation is present and patients may harm themselves or others, oral quetiapine, olanzapine, or, in more severe cases, intravenous haloperidol may be necessary, although these medications have not been shown to be effective in usual cases of delirium. Dexmedetodimine, a central α 2 -adrenergic agonist, is particularly useful for additional sedation or when agitation is accompanied by sympathetic hyperactivity. Benzodiazepines may worsen delirium and therefore should be reserved for specific indications, such as alcohol withdrawal.
In most cases, postoperative delirium is transient and reversible. Complications sometimes stemming from it include aspiration, self-removal of the endotracheal tube or indwelling catheters, and delays in mobilization that, in turn, result in an increased risk of thromboembolism, infections, and deconditioning. In addition, the occurrence of postoperative delirium is related to a greater risk of postoperative cognitive dysfunction, particularly during the first few months following surgery.
Postoperative cognitive dysfunction after exposure to general anesthesia occurs more often in older patients and in those with postoperative delirium. Mild global cognitive decline is typically observed, although short-term memory and executive function are predominantly affected. Its incidence is greatest after major cardiovascular surgery, ranging from 30 to 80 percent during the first few weeks after surgery and 10 to 60 percent after 3 to 6 months. Patients undergoing noncardiac surgery may also develop postoperative cognitive dysfunction, which has been shown to be associated with the occurrence of perioperative infarctions detectable by MRI. Additional risk factors include alcohol abuse, lower educational level, and previous stroke. Patients affected by this complication, even when transient, may have worse long-term cognitive outcomes, greater disability (particularly in the elderly), and a higher mortality. The impact of anesthesia exposure in early life (i.e., neonates and infants) on subsequent intellectual development has been quite extensively investigated but remains a matter of persistent debate due to inconsistent results across studies.
There is no definitive evidence that the choice of anesthetic regimen (such as general or regional anesthesia) or the depth of anesthesia alters the risk of postoperative cognitive dysfunction. Activation of neuroinflammatory responses has been proposed as a key mechanism underlying the development of cognitive changes after exposure to anesthesia and surgery. Maintenance of physiologic homeostasis during and after surgery may minimize the risk of this complication.
Epidural hematoma is probably the most feared complication of spinal and epidural anesthesia ( Table 55-3 ). Although rare, patients at higher risk include those with advanced age, alcoholism, anatomic abnormalities of the vertebral column leading to difficulties with needle placement, and, most importantly, coagulopathy due to a bleeding diathesis or anticoagulant effect.
| Type of Anesthesia | ||||
|---|---|---|---|---|
| Complication | Epidural Block | Intrathecal Block | Caudal Block | Block and General Anesthesia in Combination |
| Death | 1 | – | – | – |
| Brain damage | 1 | – | – | 1 |
| Symptoms of cauda equina lesions | 12 | 20 | 2 | 5 |
| Spinal/epidural hematoma | 2 | – | – | – |
| Subdural hematoma | – | 2 | – | – |
| Subarachnoid hemorrhage | 1 | – | – | – |
| Significant paresis | 10 | 7 | – | – |
| Purulent meningitis | – | 2 | – | – |
| Deep local infection | – | 1 | – | – |
| Somatosensory disturbances | 18 | 21 | – | 4 |
| Chronic back pain | 7 | 8 | 1 | 2 |
Symptoms of epidural hematoma typically present within the first few hours after the surgery. Attributing them to anesthetic effects may delay the diagnosis and decrease the chances of recovery after surgical evacuation. The neurologist should contact the anesthesiologist to clarify the anesthetic approach used, the effects of the drugs administered, and the expectation of the duration of their effect. In the acute phase, it may be difficult to differentiate between a compressive epidural hematoma and spinal cord ischemia. Preservation of posterior column sensation is expected with an anterior spinal artery infarction. Spinal CT scan allows visualization of the hematoma in most cases, but its sensitivity is suboptimal when hardware is present. Therefore, MRI of the spine should be obtained urgently if possible. Urgent surgical evacuation of the hematoma may result in excellent functional recovery.
The American Society of Regional Anesthesia and Pain Medicine has published recommendations for the management of patients receiving antithrombotics who require regional anesthesia. Warfarin should be discontinued 5 days before planned regional anesthesia, and anticoagulation with warfarin should be reversed until the international normalized ratio is 1.5 or less before urgent interventions. Patients at high risk of thromboembolism should receive bridging with unfractionated heparin (to be stopped 4 hours before surgery) or low-molecular-weight heparin (reduced to half of the usual daily dose and stopped 24 hours before surgery). After surgery, warfarin can be resumed on the first day and heparin products restarted after 24 hours following minor surgeries or 48 to 72 hours after major surgeries. Although continuation of aspirin is acceptable if necessary, clopidogrel should be discontinued 5 to 10 days before the surgery and can be restarted 24 hours after it. It is recommendable to discontinue dabigatran 5 days before the procedure, although 3 days may be an acceptable interval in patients with creatinine clearance greater than or equal to 80 mL/min. Dabigatran should not be restarted until at least 6 hours following removal of the neuraxial catheter. The factor Xa inhibitors rivaroxaban and apixaban should be discontinued 3 days before the intervention and not restarted until at least 6 hours after removal of the neuraxial catheter. Neuroaxial blocks are discouraged in patients with severe impairment of renal function (creatinine clearance ≤30 mL/min).
Epidural abscess can also cause postoperative paraparesis, but its presentation is usually delayed (at least for days after surgery), and cases exclusively related to neuroaxial blockade are rare ( Table 55-4 ).
| Neurologic Syndrome | Onset of Symptoms | Resolution of Symptoms |
|---|---|---|
| Aseptic meningitis | <24 h | <7–10 days |
| Cauda equina syndrome | Immediate or several days’ delay | Permanent or temporary |
| Adhesive arachnoiditis | Weeks after block | Permanent |
| Epidural abscess | Days to months after block | Permanent or temporary |
The incidence of neuropathy has been estimated to be less than 0.04 percent after neuroaxial blockade and less than 3 percent following peripheral blockade, although these rates should be considered general approximations. Neurologic symptoms and deficits are typically transient. Although prospective studies with blinded assessment are lacking, persistent postoperative neuropathy after regional anesthesia is quite infrequent.
Neuropathies can occur due to various mechanisms, some of which are not strictly related to anesthesia. Mechanical stress from stretch or compression of nerves as a result of malpositioning during surgery is a common cause; neuropathies are more likely to occur after prolonged surgeries. Other risk factors include male sex, diabetes mellitus, smoking, hypertension, vascular disease, obesity or extremely thin body habitus, and pre-existing clinical or subclinical nerve dysfunction. Some of these associations suggest that ischemic and metabolic insults play a role in pathogenesis.
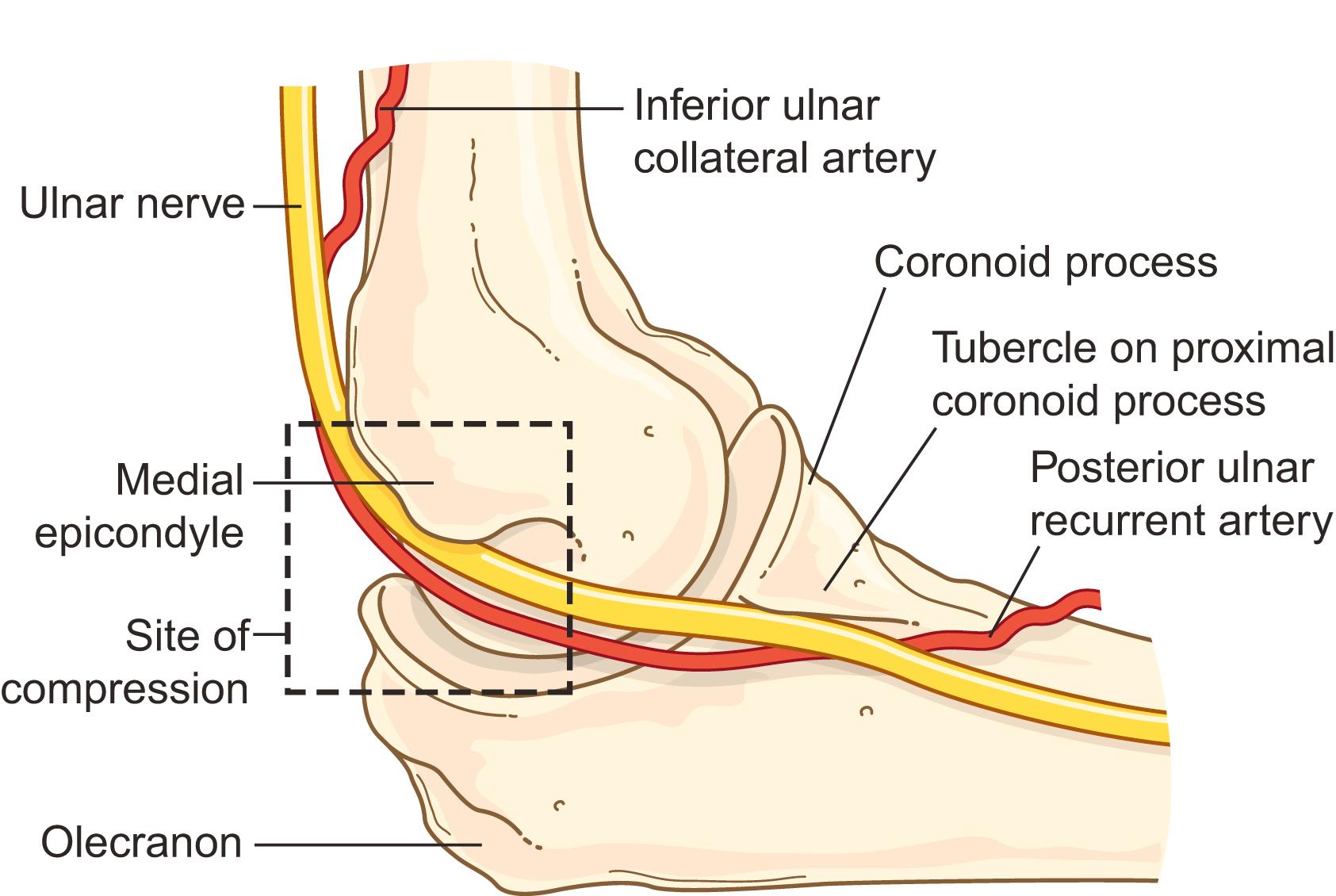
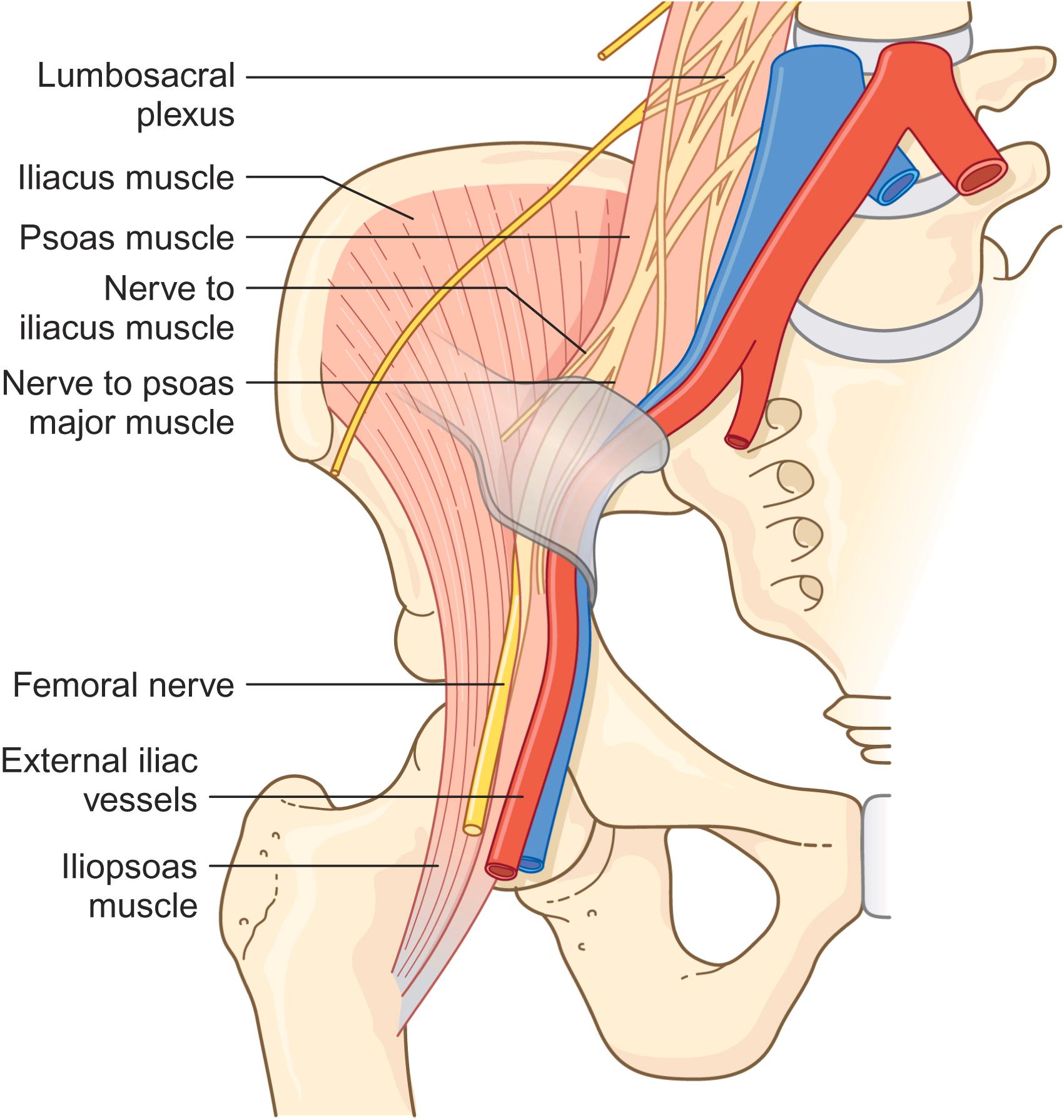
The most frequently affected nerves in the upper extremities are the ulnar nerve and brachial plexus and in the lower extremities the sciatic, femoral, and fibular (peroneal) nerves and the lumbosacral plexus. The predisposition of these particular nerves probably relates to their susceptibility to stretch and compression. The most common deficits that result are pure sensory and sensorimotor disturbances. Positioning strategies to reduce the risk of each of these peripheral neuropathies have been described. Avoidance of arm abduction beyond 90 degrees in supine patients diminishes stretch of the brachial plexus. Minimizing pressure over the ulnar groove, avoidance of excessive flexion of the elbow ( Fig. 55-1 ), and use of protective elbow padding are recommended to reduce ulnar nerve injuries. Restricting stretch of the hamstring muscle and the degree of hip flexion when the patient is in the lithotomy position lessens the risk of sciatic neuropathy. Perioperative fibular (peroneal) neuropathies can be averted through careful avoidance of prolonged pressure over the fibular head and the use of protective padding. Limb position and external compression play a lesser role in the pathogenesis of perioperative femoral neuropathies, which are attributed most often to damage from inappropriate retractor placement or pelvic hematoma ( Fig. 55-2 ).
Cauda equina syndrome is a rare complication of spinal anesthesia, attributed speculatively to maldistribution of the local anesthetic into the subarachnoid space. Most reported cases have occurred after continuous spinal anesthesia, and the predominant manifestations are localized to the S1 nerve roots, presumably because of their more posterior location.
Full recovery from these neuropathies is often seen after days to weeks, but some patients suffer persistent disability. There is insufficient information to guide prognostication, except that electrodiagnostic evidence of demyelination (conduction block) rather than axonal loss implies a better prognosis than otherwise.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here