Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The majority of neurodegenerative diseases (NDDs) discussed in this chapter are definitively diagnosed only by neuropathological examination. Brain biopsy in living patients may be useful in prion diseases, in neoplasms and non-neoplastic disorders that cause cognitive impairment, and in identifying NDD-associated pathologies in a limited sample. For instance, patients with ventriculoperitoneal shunt placement frequently have a biopsy of non-eloquent cortex during the procedure. These specimens may reveal Alzheimer disease (AD)-associated neuropathology (common), vascular pathologies, or cortical Lewy body (LB) pathology (uncommon). However, definitive identification of all of the neuropathologies that contribute to the patient’s disease requires autopsy.
Genetic studies may identify single gene autosomal dominant mutations, or other heritable genetic alterations, allowing a definitive diagnosis to be made during life, but these are exceptional cases. Examples of this include early-onset AD due to presenilin 1 ( PS1 or PSEN1 ), presenilin 2 ( PS2 or PSEN2 ), or amyloid precursor protein ( APP ) mutations (altogether accounting for <5 % of cases). Additional examples include amyotrophic lateral sclerosis (ALS) and frontotemporal lobar degeneration (FTLD) attributable to hexanucleotide expansions on the short arm of chromosome 9 (9p21) within the C9ORF72 gene. In ALS patients the C9ORF72 mutation comprises ∼50 % of familial ALS cases and ∼10 % of sporadic ALS cases. Among the latter group, C9ORF72 expansion may first be detected at autopsy, including patients over the age of 70 years at death. Even in patients with single gene alterations clearly leading to a neurodegenerative syndrome, autopsy may further inform a final, integrated diagnosis based on the sum of clinical, genetic, imaging, biomarker, and pathologic data.
In routine practice the autopsy diagnosis of NDDs frequently confirms and extends clinical diagnoses. Significant revisions of a clinical diagnosis do happen, however. Revision of diagnosis at autopsy is particularly true in three scenarios:
A clinically defined disorder has an extremely low population prevalence (e.g., <5 cases per 100,000 in the population). A presumptive clinical diagnosis of corticobasal degeneration (CBD), for instance, is often based on features of corticobasal syndrome (CBS), which include asymmetric rigidity, akinesia, ideomotor apraxia, and even the “alien limb” phenomenon, as defined on clinical neurological examination. At autopsy, however, the most common pathologic basis of CBS is the related four-repeat (4R) tauopathy of progressive supranuclear palsy (PSP) and not pathologic CBD.
The patient coming to autopsy has a clinical diagnosis of frontotemporal degeneration (FTD), presumptively due to the spectrum of pathologies in FTLD. At autopsy, a clinical diagnosis of FTD, especially when not attributable to single gene mutations, may be diagnosed as early-onset AD. This scenario will likely become even less common as biomarkers for AD improve and positron emission tomography (PET) ligands for tau improve diagnostic sensitivity. This clarification at autopsy is also common in patients with clinically diagnosed FTD and logopenic variant primary progressive aphasia, wherein patients have word finding difficulty and decreased verbal output while other abilities (e.g., naming) remain intact. At autopsy, these patients may have a fairly typical distribution of AD neuropathology, and several groups have even referred to these as logopenic variant AD.
The final and most common scenario for diagnostic revision is for NDDs occurring in the oldest old patients (≥85 years as defined by the US Census Bureau). Patients in this cohort often have a slowly progressive amnestic disorder that spares other domains, such as verbal fluency. These patients may have a clinical diagnosis of mild AD, but at autopsy frequently have multiple underlying pathologies, the most critical of which may be hippocampal sclerosis of aging (HS-Aging), now referred to as limbic-predominant age-related TDP-43 encephalopathy, or LATE. Additional pathologic diagnoses in these patients include primary age-related tauopathy (with little or no amyloid), argyrophilic grain disease, and vascular insults, among others.
This chapter focuses on the salient features that distinguish the various NDDs, as well as their points of overlap. The clinical findings, biomarkers, and imaging findings are briefly reviewed, followed by the macroscopic and microscopic findings of each entity with illustrations of characteristic pathology. The differential diagnosis is briefly discussed, and each section considers the genetic basis for each disorder and its potential relationship to pathogenesis. The NDDs in this chapter are arranged in the approximate likelihood they are encountered in an active autopsy service. Dementia and age-related neuropathologies associated with impaired cognition are covered in the first half of chapter, including AD, Lewy body disease (LBD) and dementia with Lewy bodies (DLB), LATE, primary age-related tauopathy (PART), aging-related tau astrogliopathy (ARTAG), argyrophilic grain disease (AGD), FTLD-tau, and chronic traumatic encephalopathy (CTE). This section is followed by a discussion of parkinsonian and atypical parkinsonian syndromes, including typical (Parkinson disease [PD]) and atypical parkinsonian syndromes (PSP, CBD, and multiple system atrophy), with many of these patients also having cognitive deficits. The third portion of the chapter discusses motor neuron disease, focusing on ALS and ALS with dementia (ALS/FTLD).
In its most typical form, AD is characterized clinically by progressive and irreversible memory loss along with impairments in visuospatial function. The majority of patients with pathologically confirmed AD have an onset of their symptoms after age 65 years, and these patients are referred to as having late-onset AD, or LOAD, distinguishing them from early-onset AD (EOAD). A common initial complaint of patients is forgetfulness, which eventually becomes severe enough to affect daily routine and thus distinguishes itself from more common, age-related memory lapses. As AD pathology progresses, memory loss becomes more profound, and patients experience deficits in visuospatial function, even getting lost in familiar settings, such as their home. Deficits in language frequently arise, including deficits in word finding and verbal fluency in a subset of patients with the logopenic variant of AD (see above). Sensory domains are typically spared even in advanced AD patients. A notable exception to this rule is the rare AD variant of posterior cortical atrophy in which patients have visual dysfunction leading to blindness as a prominent feature of the disease. Regardless of the typical or variant presentation of LOAD, the disease may progress to the point where the patient is noncommunicative and does not recognize family members. Motor system dysfunction is not typical in LOAD, although long-lived patients often experience issues such as dysphagia.
Patients with EOAD also present with the clinical features of LOAD, particularly memory loss. In addition, the family history often reveals one or more first- or second-degree family members with a history of dementia. More unique to EOAD patients, however, is the frequent occurrence of behavioral symptoms, giving rise to an FTD-like picture. Other findings that may confuse the clinical picture in EOAD patients include signs such as myoclonus.
Standard investigations in patients with newly diagnosed AD include brain magnetic resonance imaging (MRI), in particular using arterial spin-label (ASL) imaging of cerebral blood flow (CBF), and PET studies using 18F-fluorodeoxyglucose (FDG-PET), as well as PET ligands that bind to beta-amyloid (Aβ) and tau. In addition, cerebrospinal fluid (CSF) is routinely sent for analysis of Aβ levels (typically decreased) and total tau protein (typically increased, albeit at much lower levels than in rapidly progressive dementias). Other laboratory studies are critical in excluding reversible causes of cognitive impairment, including hypothyroidism and vitamin B12 deficiency.
Structural brain imaging with high-resolution MRI reveals the characteristic pattern of frontotemporal and mesial temporal atrophy in AD. Gradient echo MR sequences, sensitized to hemosiderin deposits and microhemorrhages, may identify superficial cortical microhemorrhages that indicate cerebral amyloid angiopathy (CAA). FDG-PET imaging is also routinely used in the clinical diagnosis of AD, showing good correlation with MRI-ASL. Florbetapir, or other PET tracers that bind to Aβ aggregates, detect even non-neuritic plaque pathology in cortex, as well as more advanced forms of CAA. However, there are several caveats in the interpretation of PET studies. First, one-third of cognitively normal older adults have conspicuous signal on PET amyloid imaging for Aβ. Second, with a slice thickness of 5 mm and voxel size of 2 mm, PET studies for Aβ prevent assignment of a definitive Thal phase regarding the extent of amyloid deposits. Image resolution is insufficient and anatomic coverage is limited in the subcortical and brainstem nuclei and cerebellar cortex, which are crucial to the determination of Thal phases 3–5. Finally, off-target binding of ligands for Aβ is well known, with structures such as the choroid plexus showing prominent signal despite the absence of pathologic Aβ. FDG-PET uses glucose metabolism as an indirect marker of neuronal activity and thus neuronal loss. In AD patients, FDG-PET reveals bilateral and symmetric decreases in glucose metabolism in posterior brain regions, including within bilateral temporal lobes, posterior cingulate and precuneus. Subcortical nuclei, occipital lobe, the perirolandic region around central sulcus, and cerebellum are spared. A variety of tau ligands are also under development, and a sensitive and specific tau tracer might assist in estimating Braak and Braak neurofibrillary tangle stage. Using these techniques, AD patients coming to autopsy in the near future should have a clearer premortem picture as to the level of AD neuropathologic change present.
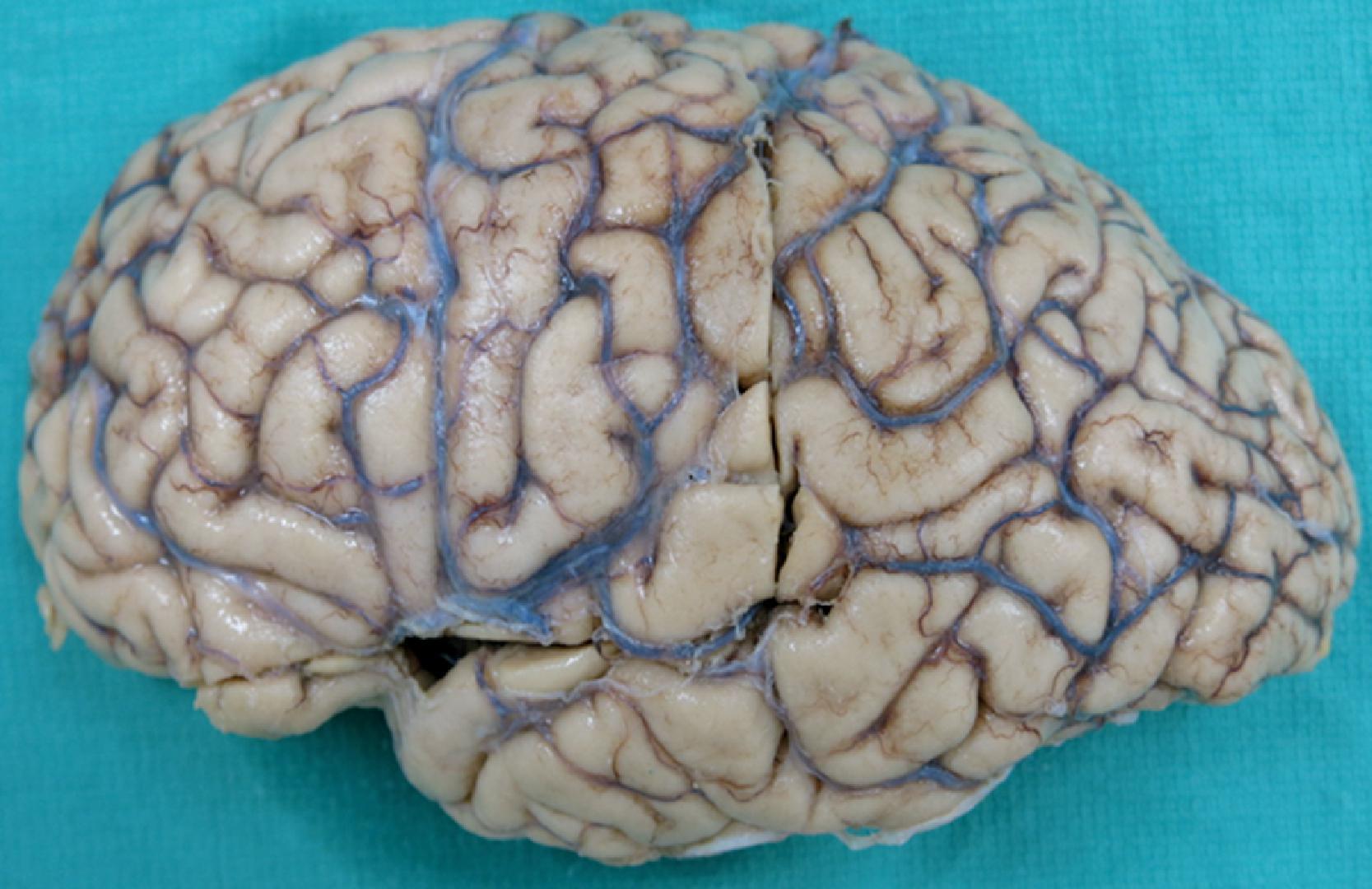
Diffuse cerebral atrophy is the defining macroscopic finding in AD brains ( Fig. 6.1 ). Brain weights are frequently between 1000 and 1200 g, even in advanced AD. The most common pattern of atrophy in AD is symmetric frontotemporal atrophy with sparing of the sensorimotor (perirolandic) and visual cortices. The circumscribed, “knife-edge” atrophy of FTLD is atypical in routine AD, and the transition between atrophic and non-atrophic brain is fairly subtle. The pattern of cerebral atrophy may follow variant clinical features of the disease, including occipital atrophy in posterior cortical atrophy.

Sectioning of the AD cerebrum confirms the frontotemporal atrophy and often reveals moderate to severe dilatation of the ventricular system—hydrocephalus ex vacuo—sometimes presenting clinically as normal-pressure hydrocephalus. In addition, sections of brain show atrophy of entorhinal cortex and amygdala. Entorhinal cortex atrophy is observed by identifying the collateral sulcus on cut sections of temporal lobe and following the sulcus rostrally to the level of the uncus and mid-amygdala and temporal horn of the lateral ventricle (usually enlarged). In AD brains a histologic section from this site is useful in sampling the amygdala, entorhinal and transentorhinal cortex, and neocortex lateral to collateral sulcus. Hippocampal atrophy may be more subtle in AD, especially in the absence of concomitant hippocampal sclerosis. In the setting of AD, markedly atrophic hippocampi, out of proportion to whole brain atrophy and brain weight, is strongly suggestive of comorbid hippocampal sclerosis (LATE) with associated inclusions of TAR DNA-binding protein 43 kDa (TDP-43). The volume of thalamus, subthalamic nuclei, and basal ganglia are typically preserved in AD. Examination of the brainstem usually reveals pallor of locus ceruleus and substantia nigra due to neurofibrillary pathology and neuron loss.
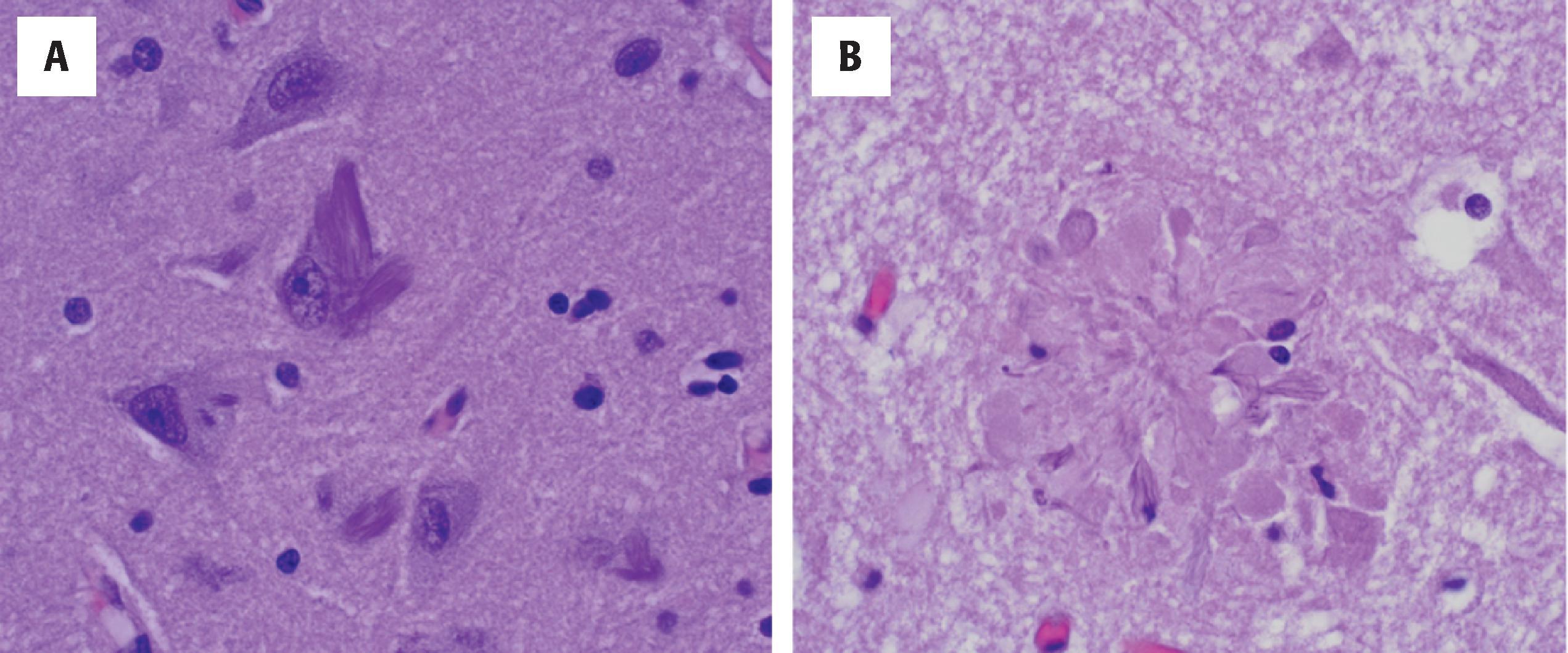
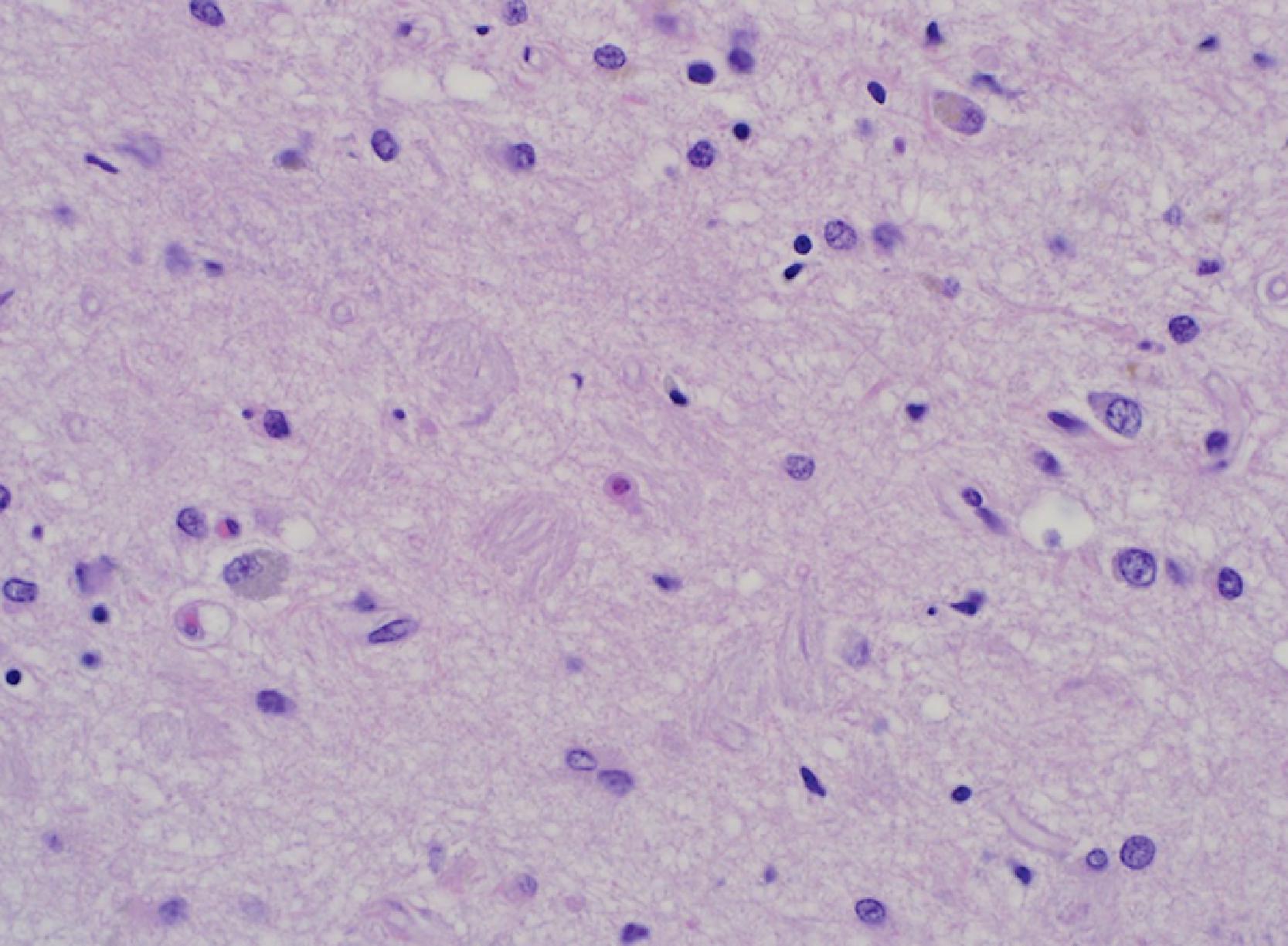
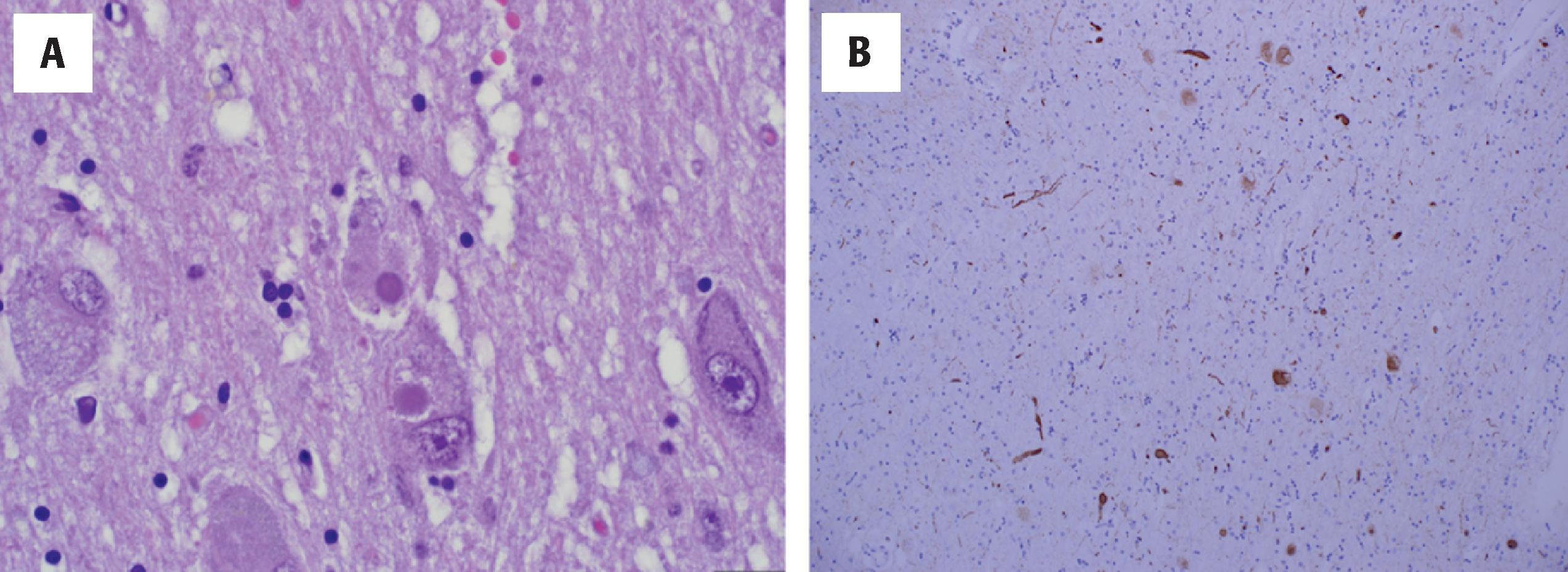
Pathologic confirmation of AD requires a combination of Aβ deposits and tau pathology in the form of neurofibrillary tangles (NFTs). Both pathologies are first recognized on hematoxylin and eosin (H&E) stains ( Fig. 6.2 ). The severity and extent of the pathologies is subsequently documented by immunohistochemical (IHC) methods, silver staining-based methods (Gallyas, modified Bielschowsky), fluorescence-based methods (thioflavin S), or a combination of these techniques. Other special stains, such as Congo red, may highlight a subset of amyloid deposits but, in general, this is not utilized.
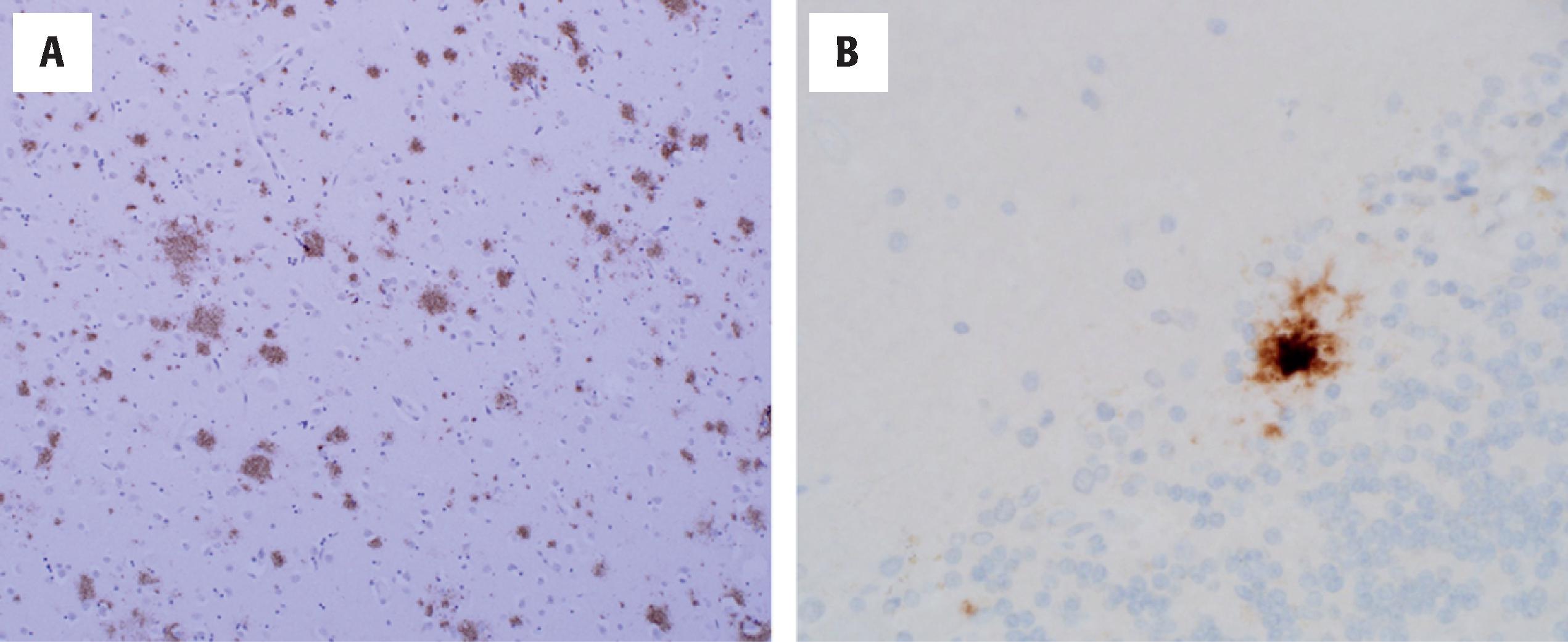
Parenchymal Aβ plaques are a critical element of AD neuropathology. Patients with AD typically have frequent mature, or “cored,” parenchymal plaques that exceed the number seen in non-demented patients. These plaques comprise extracellular deposits containing dense central cores of Aβ, typically associated with neuronal loss and microglial activation. The term neuritic plaque refers to the same structure with the addition of tau-positive, plaque-associated dystrophic neurites. In neuritic plaques microglia are also integrated into the structure at its periphery. At low and intermediate power magnification, H&E stains reveal mature plaques by their disruption of parenchyma, densely eosinophilic amyloid cores, and associated microglia. Evaluation of Aβ plaque distribution and density requires IHC or other methods. A variety of antibodies to Aβ may be applied to tissue sections of interest, often following a brief pre-treatment of tissue with formic acid for antigen retrieval. With this approach, AD brains reveal more extensive Aβ that can be identified on H&E or silver stain-based methods alone. This is because non-neuritic, diffuse deposits of Aβ are detected, often in a band-like and subpial distribution. So-called primitive plaques may also be seen, referring to an intermediate stage of Aβ plaque, between diffuse and mature, and typically characterized only by dense Aβ deposits.
Current guidelines for the diagnosis of AD, released in 2012 by a working group convened by the National Institute of Aging (NIA) and Alzheimer’s Association (AA), requires documentation of the extent and severity of Aβ and neuritic plaque pathologies, respectively. These 2012 criteria in turn evolved from the earlier NIA/Reagan criteria (1997), which generated probabilistic scores for AD neuropathologic change based on Aβ and tau pathologies. The NIA/AA 2012 system uses an ABC scoring system for amyloid extent (Thal phase for a myloid, or “A”), NFT stage ( B raak and Braak stage, or “B”) and neuritic plaque frequency ( C ERAD score, or “C”).
Thal phase describes the stereotypic progression of Aβ in pathologic aging and AD. The Thal phase does not depend on plaque subtype, and IHC methods are essential to identify the diffuse and primitive plaques that are predominant in subcortical nuclei, brainstem, and cerebellum. Five Thal phases are recognized. In Thal phase 1, Aβ pathology is limited to the cerebral cortex—a very common finding in human aging and in other non-AD NDDs. In Thal phase 2, Aβ deposits are detected in structures of the limbic region, particularly amygdala and hippocampus. Thal phase 3 is characterized by deposits in subcortical nuclei, such as striatum, thalamus, and basal forebrain, as well as in select brainstem structures (tectum). Thal phase 4 examples have Aβ in each of the preceding regions, and additionally, within characteristic brainstem nuclei, such as substantia nigra, tegmental gray of the midbrain and pons, locus ceruleus, and inferior olive. In Thal phase 5, diffuse deposits of Aβ are found in the molecular and granular cell layers of cerebellar cortex ( Fig. 6.3 ). It should be noted that CAA is common in leptomeningeal arterioles of the cerebrum and cerebellum in AD, and care must be taken not to confuse vessel wall deposits with parenchymal Aβ deposits. In the 2012 NIA/AA system the Thal phases are assigned A scores of 0–3 as follows: 0 (No Aβ deposits), 1 (Thal phases 1–2), 2 (Thal phase 3), and 3 (Thal phases 4–5).
In addition to Thal phase, the NIA/AA 2012 criteria require the frequency of neuritic plaques to be characterized. This is based on the neuropathologic assessment outlined by the Consortium to Establish a Registry for AD (CERAD) criteria. As originally proposed, the CERAD criteria employed silver stain-based methods to assess the density of neuritic plaques in designated neocortical areas (in practice, this may be estimated using Aβ and tau staining). Based on neuritic plaque frequency, levels of “none,” “sparse,” “moderate,” or “frequent” are assigned. The neocortical site with the highest neuritic plaque frequency is then used in the final CERAD designation. In the 2012 NIA/AA system, the CERAD neuritic plaque frequency is assigned a C score of 0–3 as follows: 0 (none), 1 (sparse), 2 (moderate), or 3 (frequent).
In addition to Aβ deposits, tau-positive NFTs are the other major component of AD pathology and the one that correlates best with cognitive impairment. NFTs comprise insoluble, fibrillar deposits of hyperphosphorylated tau in neurons, and these may be identified in virtually all brain regions. Ultrastructural examination has shown that pathologic tau deposits comprise paired helical filaments ( Fig. 6.4 ). Normal tau protein is a microtubule-associated and organelle-stabilizing protein essential to the integrity of the cytoskeleton. Tau is the product of the microtubule-associated protein tau ( MAPT ) gene on chromosome 17 with alternative splicing leading to both three-repeat (3R) and 4R isoforms of tau, based on the number of microtubule-binding domains present (discussed later in the chapter). In AD, tau is cleaved and phosphorylated and dissociates from microtubules.
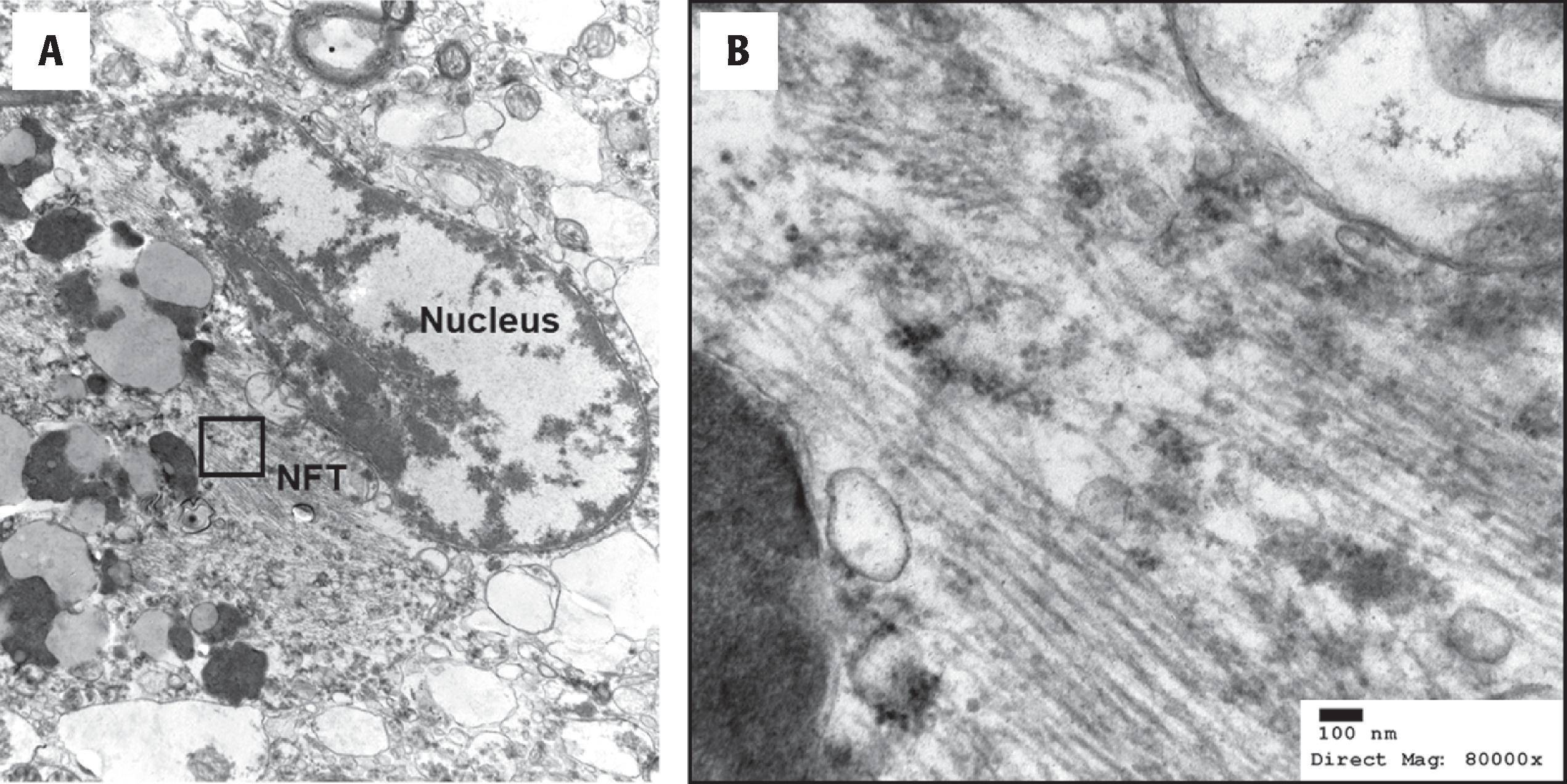
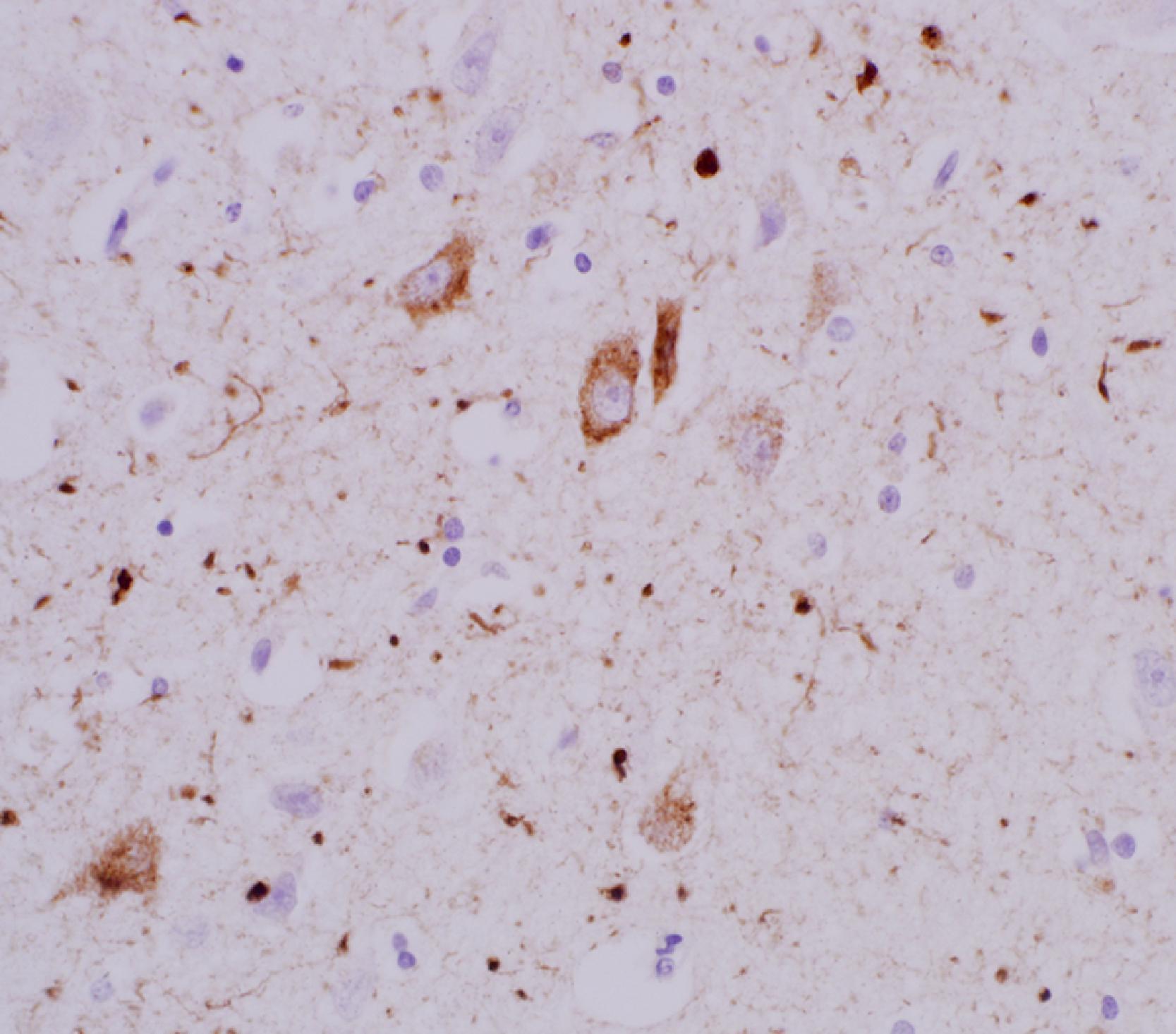
On H&E examination of the AD brain, NFTs appear as either flame-shaped, basophilic cytoplasmic inclusions ( Fig. 6.2 ), or as round aggregates filling the cell body (globose NFTs). Whereas pyramidal neurons of neocortex and hippocampus frequently contain NFTs of the flame-shaped variety, neurons with round cell bodies, such as in amygdala, basal forebrain, and brainstem, frequently contain globose NFTs. NFTs may also be identified by silver staining methods and thioflavin S, which is useful because both techniques simultaneously detect neuritic plaque pathology. Another approach to identify NFTs is to use antibodies to tau, such as clone AT8, which targets tau that is phosphorylated at its serine 202 and threonine 205 residues. This IHC approach has the additional advantage that non-fibrillar, granular deposits of phospho-tau may be detected in neurons as pretangles that are not readily visualized by other methods ( Fig. 6.5 ). In addition to accumulating in the neuronal cell body to form an NFT, or as plaque-associated neurites, tau accumulates in neuronal dendrites as “neuropil threads.” These may be numerous in neocortex, even when NFT pathology is mild.
In regard to tau pathology, the NIA/AA 2012 criteria require the extent of NFT pathology to be documented using the staging system published in 1991 by Heiko and Eva Braak. With a few notable exceptions, such as the rare variant of hippocampal-sparing AD, this staging system is robust and strongly predictive of cognitive status. Patients with Braak and Braak NFT stages of V and VI rarely, if ever, have normal cognition. Likewise, patients with clinical AD but Braak and Braak NFT stages of ≤III have other underlying pathologies contributing to their cognitive impairment. Therefore an accurate and unbiased determination of NFT stage is a critical element in the evaluation of an AD patient at autopsy.
In contrast to the progression of Aβ deposits in aging and AD, the earliest tau pathology appears within brainstem nuclei and in the transentorhinal and entorhinal regions adjacent to collateral sulcus (stages I–II). As the NFT pathology progresses, there is more extensive involvement of amygdala, hippocampal formation, basal forebrain, subcortical nuclei, and eventually neocortex/isocortex (stages III–IV). The neocortical involvement begins in the association cortex with significant NFT pathology in primary visual, auditory, and sensorimotor cortices only occurring in Braak and Braak stage VI. The NFT stages are summarized as follows:
Stages I–II, “transentorhinal”: In stage I, tau pathology is limited to transentorhinal cortex. Stage II is characterized by involvement of large multipolar neurons in lamina II of the entorhinal cortex and early involvement of other limbic structures. Full-thickness involvement of the entorhinal cortex and significant involvement of the hippocampal formation are not seen in stage II. Stages I and II constitute a B score of 1 in the 2012 NIH/AA system.
Stages III–IV, “limbic”: Stage III NFT pathology is indicated by a band-like involvement of hippocampal regions CA2 and CA1, early involvement of CA4, full-thickness involvement of transentorhinal and entorhinal cortex, and neuron loss in superficial entorhinal cortex. The last of these is confirmed on H&E stains, and extracellular “ghost” tangles ( Fig. 6.6 ) occupy the position of the large multipolar neurons that formerly occupied lamina II. Stage IV is characterized by more severe involvement of all limbic regions, including anterior cingulate cortex, involvement of large cholinergic neurons of basal forebrain, and patchy but mild neocortical involvement by NFTs. Although neocortical NFTs are not numerous in stage IV, neuropil threads and plaque-associated neurites may be numerous. Together these limbic stages (III–IV) may correlate with mild cognitive impairment (MCI) in some patients but in isolation are insufficient to account for mild AD or more severe forms of cognitive impairment. Stages III and IV constitute a B score of 2 in the 2012 NIH/AA system.
Stages V–VI, “isocortical”: In stage V, frontal, parietal, and temporal association cortices have more advanced NFT pathology as do the peristriate (Brodmann area 19) and parastriate (Brodmann area 18) areas of occipital lobe. In contrast, the primary visual/striate cortex (BA 17), as well as other primary cortical areas, has little or no NFT pathology. In addition, cases with stages V and VI have a predictable pattern of lamina II, III, and V NFT pathology across patients and cortical regions that is readily identified on low power examination of an AT8 or other suitable stain. Stage VI is characterized by involvement of all preceding regions and more substantial NFT pathology in primary sensorimotor, auditory, and visual cortices. Identification of stage VI thus requires appropriate sampling of motor cortex, Heschl’s gyrus (with auditory cortex), and striate cortex along the calcarine sulcus. Stages V and VI constitute a B score of 3 in the 2012 NIH/AA system.
Atypical patterns of tau pathology, including deposits within astrocytes, at the depths of sulci, within white matter, or aberrant deposits in lamina I, suggest comorbid pathologies and are not AD pathologies changes per se. These are discussed elsewhere in the chapter.
Per NIA/AA 2012 guidelines, the combinations of Thal phase (A score), CERAD neuritic plaque frequency (B score), and Braak and Braak NFT stage (C score) are placed together in a matrix to determine whether the patient has “no,” “low,” “intermediate,” or “high” AD neuropathologic change (ADNC). Two very simple rules of thumb can be derived from this approach. First, a designation of high ADNC requires fairly advanced Aβ + NFT/tau pathology. Second, Thal phase and neuritic plaque frequency alone cannot be used to assign a high ADNC score in the absence of an isocortical NFT stage. In this way, the ABC scoring system relies heavily on the association between tau pathology and cognitive impairment.
Other pathologies common in ADNC are CAA, and other cellular inclusions, such as Hirano bodies and granulovacuolar degeneration (GVD). CAA comprises deposits of Aβ in the tunica media and adventitia of arterioles in leptomeninges and cortex ( Fig. 6.7 ). CAA is most readily seen in leptomeningeal vessels of occipital cortex, cerebellum, and within the depths of the collateral sulcus in the temporal lobe. Mild CAA is seen as diffuse and patchy deposits not occupying the entire vessel wall and is readily detected by immunostains to Aβ. In moderate and severe CAA forms, the Aβ deposits are full thickness, giving rise to a “lead pipe” appearance of arterioles (in the absence of perfusion pressure after death, typical cortical arterioles would collapse). This lead pipe appearance of CAA is best appreciated on low and intermediate power examination of H&E stains and is confirmed by Aβ immunostaining. Severe CAA is also associated with perivascular hemosiderin deposits and microhemorrhages detected premortem by gradient echo MRI. Frequently, patients with severe CAA also have Aβ deposits in adjacent perivascular parenchyma—a pattern termed dyshoric CAA . Capillary CAA is another notable form of Aβ deposits, particularly because this is enriched in carriers of the APOE ε4 allele. This capillary CAA is most readily detected in capillaries of deep cortical laminae. Cerebral white matter and associated vessels in white matter are typically negative for Aβ deposits. Like Thal phase for parenchymal Aβ deposits, a hierarchical progression of CAA has been described beginning in occipital and cerebellar regions and culminating in vessels of the vertebrobasilar system (an uncommon finding). It should be noted that not all CAA is Aβ-derived. Rare pathologies leading to non-Aβ CAA include amyloidosis with deposits of gelsolin, protease-resistant prion protein, or transthyretin. Likewise amyloid angiopathy in the region of pituitary and sella turcica reflects systemic amyloidosis (e.g., senile-type transthyretin or AA or AL-type amyloid), not Aβ. Therefore negative stains for Aβ in the setting of an H&E appearance of amyloid angiopathy should prompt other screening techniques (e.g., Congo red).
Hirano bodies and GVD are nonspecific findings and are most abundant within the hippocampal formation of AD patients ( Fig. 6.8 ). Hirano bodies consist of arrays of actin filaments on ultrastructural examination and by H&E appear as rod-shaped and refractile eosinophilic structures adjacent to the cell bodies of pyramidal neurons in the hippocampal formation. Hirano bodies are actually neuronal cytoplasmic inclusions despite their appearance as extracellular structures. GVD consists of cytoplasmic, basophilic granules with associated vacuoles in neurons. Foci of GVD frequently accompany pyramidal neurons with Hirano bodies in the hippocampal formation. The pathogenesis of GVD is not known, and studies have shown these deposits may be derived from lysozymes.
Additional pathologies in AD brain include TDP-43 deposits, described later, and amygdala-predominant Lewy bodies. Amygdala-predominant Lewy bodies are fibrillar deposits of α-synuclein, often colocalized with NFTs and tau, in large neurons of the corticomedial and basolateral amygdala. Lewy neurites are uncommon in this setting, and these patients lack the widespread Lewy body pathology of DLB and PD. The significance of amygdala-limited Lewy bodies in the setting of AD was previously unclear. However, recent studies have shown that patients with advanced AD path (A3 B3 C3), amygdala-predominant Lewy bodies, and TDP-43 inclusions form a unique subset of dementia patients with a quadruple proteinopathy (Aβ + α-synuclein + tau + TDP-43). Longitudinal studies of these patients have shown a shorter time interval between mild cognitive impairment and conversion to dementia, as well as more rapid disease progression with more significant cognitive impairment.
The most common dementing illness in human aging, characterized by progressive and irreversible memory loss and both beta-amyloid (Aβ) and tau pathology
Memory loss, deficits in visuospatial function, deficits in word finding and verbal fluency. Uncommon variants are well described (see text for detail)
Structural MRI, FDG-PET, and newer PET ligands for tau
CSF studies of Aβ levels (typically decreased) and total tau protein (increased)
Diffuse cerebral atrophy, typically with a frontotemporal predominance
Requires a combination of Aβ deposits and tau pathology in the form of NFTs (see text for detail of pathologic staging)
A highly heritable disease, likely modified by environmental factors
The relative risk of developing AD for individuals with a single first-degree family member dying from AD is ∼1.7; the risk is >2.0 when a second-degree family member is also affected and increases dramatically with additional affected second-degree family members
APP, PSEN1, and PSEN2 in EOAD and APOE ε4 in EOAD and LOAD; Genome-wide association studies (GWAS) continue to demonstrate new genes implicated in AD pathology
The differential diagnosis of AD depends on the patient’s age and clinical presentation. Patients with EOAD, as described above, may present with a unusual mix of behavioral variant and motor symptoms, leading to clinical diagnoses of FTD. Autopsy is thus critical in early-onset dementias to clarify the final diagnosis. Conversely, clinical diagnoses of a behavioral variant of AD, or a primary progressive aphasia variant of AD, may prove to be FTLD with TDP-43 inclusions (FTLD-TDP). Rare 4R tauopathies such as CBD may also present with executive dysfunction and memory disturbance, mimicking a variant of AD before parkinsonian or other disease features become prominent. In current practice, the combination of neuroimaging studies (structural MRI, PET for tau, Aβ, and glucose metabolism) and CSF biomarkers and even genetic studies often clarifies the differential of EOAD. The differential diagnosis of patients with LOAD does not frequently include atypical and rare diseases, such as FTLD. Instead, a different set of common, age-related pathologies are in the differential diagnosis. Among these, hippocampal sclerosis of aging with TDP-43 pathology, now termed LATE, commonly mimics AD in the oldest old patients (≥85 years). In addition, cerebrovascular lesions and, in particular, small-vessel disease significantly impacts the clinical expression of AD.
AD is among the most heritable of common human diseases, and some studies estimate the genetic contribution explains >60 % of all cases, with the remaining contribution attributable to modifiable/environmental factors. Accurate confirmation of AD neuropathology at autopsy, sufficient to explain clinical AD, is thus paramount in providing surviving family members with a better understanding of their own risk. This is because the relative risk of developing AD for individuals with a first-degree family member dying from AD is ∼1.7. This relative risk is greater than 2.0 when a second-degree family member (grandparent, uncle, or aunt) is also affected and is greater than 20 when there is a single first-degree family member and two second-degree family members affected by AD. A better understanding of their own risk for AD may influence the choice of surviving family members to take part in clinical trials or adopt lifestyle behaviors thought to be neuroprotective in aging and in those with increased AD risk. Neuroprotective behaviors include avoiding tobacco, maintaining a physically active lifestyle and healthy diet, and maintaining and developing social connections and cognitively stimulating leisure activities.
EOAD cases with Mendelian genetic inheritance typically have an autosomal dominant inheritance pattern. Although these account for <5 % of all AD cases, identification of three genes in particular ( APP, PSEN1, and PSEN2 ) has been critical in elucidating the important role of Aβ deposits in the pathogenesis of AD. APP is encoded by the APP gene on chromosome 21 and was among the earliest genes discovered as causative in EOAD. It is a ubiquitous transmembrane protein comprising 770 amino acids, found in both neuronal and non-neuronal cells, such as glia. Embedded within APP is the much smaller Aβ fragment, produced when the APP protein is cleaved sequentially by two proteolytic enzymes, β-secretase and γ-secretase. Causative mutations in APP are within or adjacent to the portion encoding Aβ, resulting in increased production of an insoluble and hydrophobic 42-amino acid isoform of Aβ that is critical to AD pathogenesis (Aβ42). In addition to mutations in APP , gene duplications likewise lead to abnormal abundance of APP protein with increased production of Aβ42. Patients with trisomy 21 (Down syndrome) and increased “gene dosage” of APP also have greater levels of Aβ42, developing non-neuritic parenchymal plaques in adolescence and neuritic plaques and NFT pathology in young adulthood.
Among all autosomal dominant forms of AD, mutations in PSEN1 are most common, followed by PSEN2 mutations. Presenilin 1, encoded by PSEN1 on chromosome 14, is a subunit of the γ-secretase enzyme critical to the production of Aβ42. Mutations thus lead to increased Aβ42 levels in affected patients. APP, PSEN1, and PSEN2 altogether explain <10 % of EOAD cases, with other genetic alterations, such as APOE ε4 status and other rare variants ( ABCA7 , SORL1 ), responsible for some examples of EOAD.
For LOAD, the best characterized and replicated genetic risk factor is APOE ε4 carrier status. The three alleles of the APOE gene (ε2, ε3, ε4) are determined by two polymorphisms on chromosome 19. The most common isoform in the population is ε3. The relative abundance of these isoforms and their risk for AD development varies by ethnic group, and the association of ε4 and dementia is strongest in Caucasian populations. The ε4 allele is seen in nearly half of all AD cases, and ε4 carriers have an increased risk of developing AD that is threefold with a ε3/ε4 genotype and up to 14-fold with a ε4/ε4 genotype. In contrast, the ε2 isoform confers a modest protective effect against the development of AD, although this is the rarest isoform and only 0.5 % of the population has a ε2/ε2 homozygous genotype. The mechanism(s) by which APOE isoforms impact a patient’s risk for AD remains an active area of investigation. APOE is a cholesterol transporter, expressed primarily in the brain by astrocytes, but also by other cells, such as microglia. It appears to function in the clearance of potentially pathologic Aβ, and APOE ε4 carriers have not only reduced levels of APOE in CSF and blood but may also have reduced lysosomal degradation of Aβ and reduced transport of amyloid across the blood-brain barrier. In addition to clearance of amyloid, APOE ε4 may promote aggregation and fibrillization of Aβ in the form of parenchymal plaques.
An interesting development in the study of APOE with respect to AD risk was the identification of the Christchurch mutation, a sequence variation in the APOE ε3 allele that may confer protection against AD. A recent report highlighted a patient with a causative AD mutation in PSEN1 (E280A) and a homozygous Christchurch mutation in APOE ε3. Neuroimaging studies (PET) showed that the patient had very high levels of amyloid but only limited tau deposits. Most notably, the onset of cognitive symptoms did not occur until the patient was in her 70s, which was a three-decade delay compared with other PSEN1 E280 mutation carriers. This example reinforces the role of APOE in AD and suggests that modulation of APOE activity itself may constitute a future therapeutic target.
In addition to APOE risk genotype and dominantly inherited genes, the results of high throughput genetic studies, including GWAS, have now expanded the known risk genes in AD to more than 40. None of these genes identified are as strongly associated with AD risk as APOE, though several of these newer genes have further emphasized the critical role of amyloid in disease risk. The newly identified genes have also highlighted the importance of other pathologies (microglia, tau) in disease pathogenesis. For instance, genes identified with relevance to microglial function include TREM2 and SORL1 . In regard to tau, variants in the MAPT gene have recently been described as a risk factor in AD, and genes involved in tau processing (e.g., BIN1 ) have been identified as genetic risk factors. Ongoing studies are likely to substantially expand the list of risk genes in AD, including genes critical to AD risk in different ethnic groups. Early results from GWAS studies of African-American patients, for instance, have found commonality in some, but not all, risk genes previously demonstrated largely in non-Hispanic Whites (e.g., APOE, ABCA7, TREM2, BIN1 ), while identifying novel loci associated with AD risk.
Finally, epigenome-wide association studies in AD have demonstrated the importance of DNA methylation, histone modification, and the expression of long noncoding RNAs and noncoding microRNAs that repress target messenger RNAs. Biochemical pathways are also implicated, and increased production of S-adenosyl-L-methionine (SAM), critical to neuronal methylation reactions and the regulation of AD-associated gene expression, may slow the progression of LOAD. However, this pathway is dependent on methylenetetrahydrofolate reductase ( MTHFR) , which encodes an enzyme required for the interaction of folate and cobalamin (vitamin B 12 ). MTHFR mutations/polymorphisms are very common in LOAD, presumably lowering SAM levels, and leading to the overexpression of AD-related genes.
Dementia with Lewy bodies (DLB) is the second most common cause of dementia, accounting for ∼15 % of all cases. DLB is a clinical designation for patients with this α-synucleinopathy whose symptoms are marked by a unique form of cognitive impairment. Pathologically, these patients have LBD, and the spectrum of neuropathological findings overlap those of PD and PD dementia (PDD) (the pathologies of end-stage PDD and DLB are not readily distinguished). DLB is treated here as a clinicopathologic manifestation of diffuse/neocortical LBD neuropathology with genetic risk factors that overlap both AD and PD/PDD.
The combined incidence of DLB and PDD has been estimated at almost 80 per 100,000 person-years. As with many NDDs, both DLB and PDD have a higher incidence rate in males. In males over the age of 80, the combined incidence is ∼124 cases per 100,000 person-years. Symptom onset in DLB is similar to that of LOAD, most frequently occurring in older adults after the age of 65 years.
Patients with DLB may have an amnestic component to the disease that resembles AD. In many patients, however, there are additional symptoms that distinguish the clinical picture from AD. Among these DLB features, two of the most notable are fluctuations in cognition and visual hallucinations. Fluctuations in the level of cognitive impairment differentiates DLB from the inexorable and unrelenting decline that is typical of AD and other age-related dementias. Caregivers of DLB patients frequently describe both good and bad days in cognition and functional ability. The pathophysiologic basis for this fluctuation of DLB symptoms remains poorly understood. Visual hallucinations are another unique feature of DLB and these typically take the form of stereotypic, recurrent, and often nonthreatening images (e.g., small animals or people). Patients with DLB may have an awareness that the hallucinated object is not real and may delay sharing the disturbing symptom. In contrast, auditory hallucinations are uncommon. Clinicopathologic studies have suggested that the density of LB pathology in the fusiform region of the ventral occipito-temporal region correlates with visual hallucination symptomatology. This finding suggests that the complex visual hallucinations of DLB result from pathologic involvement of extrastriate visual processing areas (the ventral visual pathway) involved in object recognition.
Parkinsonism is another common but not invariable feature in patients with DLB. As with PD and PDD, this may manifest with tremor in the hands, limbs, or trunk, as well as bradykinesia and rigidity. Presumably, this reflects the involvement of brainstem nuclei, such as substantia nigra, involved in both DLB and PD/PDD patients. Patients with DLB also experience a rapid eye movement (REM) sleep behavior disorder with incomplete paralysis of the motor system during REM sleep and “acting out” of dreams. In patients with a clinical diagnosis of AD at the time of autopsy, a history of tremor, rigidity, and REM sleep behavior disorder should prompt a complete neuropathologic work-up for predominant or comorbid LBD pathology.
Risk genotypes in DLB are also shared with both AD and PD/PDD, as discussed below. DLB also shares with AD a clinical response to cholinergic medications, such as donepezil, reflecting the pathologic involvement and loss of magnocellular cholinergic neurons in the basal forebrain, including within the nucleus basalis of Meynert. Furthering the link to AD, patients with DLB typically have concomitant AD neuropathologic change in the form of diffuse, non-neuritic Aβ plaques and limbic NFT pathology. However, comorbid high AD neuropathologic change (Braak and Braak stages V–VI) with neocortical LB pathology is not common.
Several other rare variations in the presentation of DLB should be noted, as these may mimic other NDDs. In the first, DLB patients may present with Balint syndrome, indicative of an insult to the bilateral parieto-occipital lobes, as seen with vascular insults or in posterior cortical atrophy variant of AD. Balint syndrome patients cannot recognize more than one object at a time (simultanagnosia), cannot carry out purposeful eye movements to a visual target (oculomotor apraxia), and are not able to coordinate hand movement using input from the visual field, as in reaching for an object (optic ataxia). Patients with DLB and Balint syndrome frequently have the other clinical features of the DLB described above. Rare DLB patients have a rapidly progressive dementia that mimics prion disease/Creutzfeldt-Jakob disease in the pace of clinical deterioration and in behavioral manifestations. As with any rapidly progressive dementia, caution should be exercised and brain removal at autopsy may be conducted using precautions reserved for prion disease cases.
At this time, there are no CSF or blood biomarkers that can be used to confirm or refute the clinical diagnosis of DLB. CSF studies for total tau and Aβ are nonspecific. This is because the abnormal pattern seen in AD patients (low CSF amyloid, increased total tau) may be seen in DLB, reflecting the intermediate AD neuropathologic change that is typical. Neuroimaging studies are more revealing in suggesting the diagnosis. Structural brain MRI is useful in that the diffuse cerebral atrophy that characterizes AD is typically absent. Mild and focal cortical atrophy, or no atrophy detected at all, is more characteristic of DLB. In particular, the mesial temporal lobe atrophy of AD and HS-Aging/LATE are absent.
DLB also has a more characteristic pattern of hypometabolism by FDG-PET that differs substantially from AD. In DLB patients, hypometabolism is seen even more posteriorly than in AD, with reduced uptake in the parieto-occipital regions in particular and with sparing of posterior cingulate/precuneus (affected early in AD) and frontal lobes (affected in FTLD). The sparing of posterior cingulate metabolism on FDG-PET relative to hypometabolism in the occipital region is referred to as the “cingulate island sign” and is strongly suggestive of DLB. A similar pattern of hypoperfusion in the parieto-occipital region is also seen with MRI-ASL CBF imaging. This pattern of parieto-occipital hypometabolism has even been proposed as a biomarker of DLB. Single-photon emission computed tomography (SPECT) studies, using a 123 I-FP-CIT SPECT or dopamine transporter (DAT) scan, are also useful in demonstrating reduced striatal uptake of dopamine in DLB, as well as in PD and PDD. Unlike radioligands for Aβ and those being developed for tau, there is currently no ligand routinely used to image α-synuclein pathology.
Examination of DLB brains at autopsy reveals only mild frontal atrophy, and brain weights are frequently greater than 1300 g ( Fig. 6.9 ). There is no distinct parieto-occipital or temporal lobe atrophy visible on external examination in the absence of comorbid pathologies. As with prion diseases, patients with profound cognitive impairment in DLB may come to autopsy and brain removal yields a fairly unremarkable cerebrum. The major pathologic finding noted in virtually all DLB cases is loss of pigmentation in substantia nigra and locus ceruleus. Ventricle enlargement and medial temporal lobe atrophy are mild, if even present. The basal ganglia, midbrain tectum and tegmentum, basis pontis, cerebellar peduncle volumes, and cerebellum typically appear within normal limits, in contrast to uncommon entities with parkinsonism.
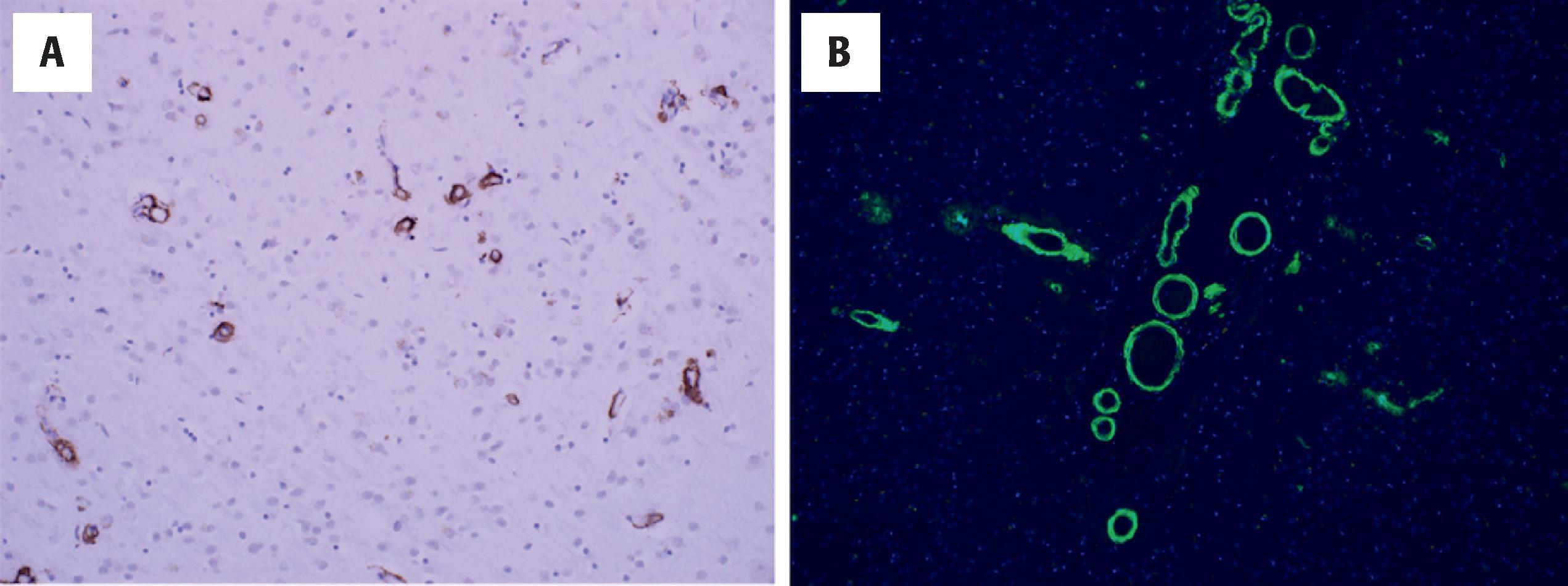
On H&E examination, the characteristic feature of DLB is the presence of LBs in the neocortex, large cholinergic neurons of the nucleus basalis in the basal forebrain, and limbic regions such as the anterior cingulate cortex, amygdala, hippocampal formation including subiculum, and entorhinal cortex. Neocortical LBs occur mainly in deep cortical laminae (V, VI) and are rarely seen superficial to those laminae. By H&E, cortical LBs are recognized by the eccentric displacement of the nucleus and cytoplasm containing homogeneous-appearing and vaguely fibrillary eosinophilic inclusions. Unlike brainstem LBs, or those in large neurons of nucleus basalis or amygdala, cortical LBs lack a halo of surrounding cytoplasm and/or pigment. Their presence is confirmed using antibodies to α-synuclein or its phosphorylated form. In contrast to AD, the extent of α-synuclein pathology is greatly underestimated by H&E findings alone ( Fig. 6.10 ). As such, cases with any limbic or cortical Lewy body pathology on H&E examination require special stains to document their extent. Brainstem nuclei typically involved in PD and PDD are also frequently diseased in DLB cases. These include substantia nigra, albeit often without severe neuron loss, reticular gray of midbrain, raphe nuclei, locus ceruleus, dorsal nucleus of X, and the reticular formation of medulla. As with PD/PDD, fibers of the glossopharyngeal nerve in the medulla are frequently α-synuclein-positive ( Fig. 6.11 ). LBs and neurites may also be found in the peripheral nervous system, including within neurons of cardiac ganglia, adrenal medulla, and celiac ganglia.
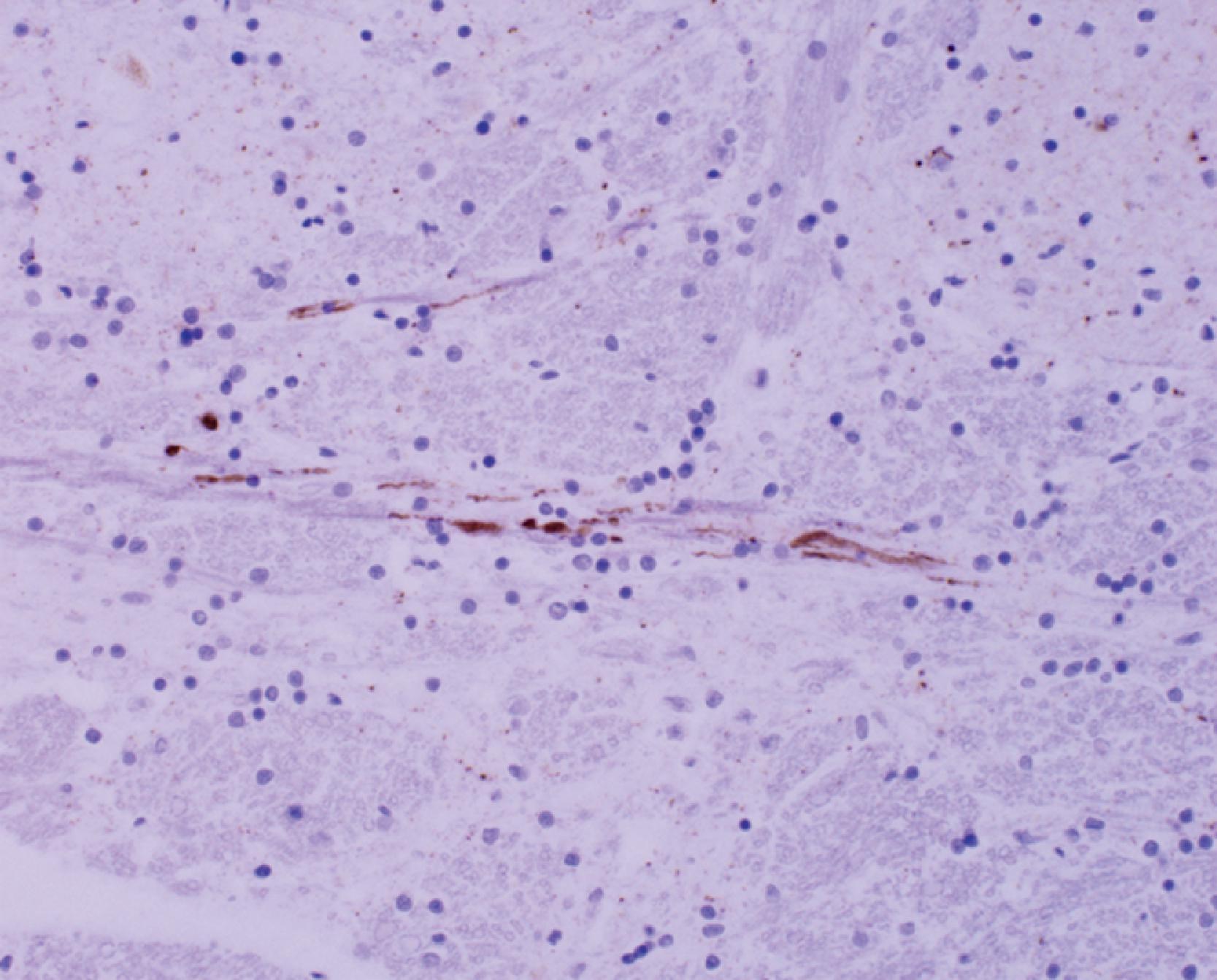
Lewy neurites are α-synuclein-positive structures seen in DLB and are not visible by H&E staining. These are thick, tortuous structures frequently seen in association with intra- and extracellular Lewy bodies by α-synuclein ( Fig. 6.10 ). Lewy neurites and LBs together are used in the pathologic grading schema recommended by McKeith and colleagues. Notable in this grading scheme is that the number of LBs and Lewy neurites are recorded together at low power magnification and are used to provide a designation of severity per region. In contrast to AD, wherein NFTs may be innumerable in neocortex, cases of DLB with pathologic LBD diffuse/neocortical have LB counts that are readily enumerated.
One of the most frequent causes of dementia in patients over the age of 65 years, characterized pathologically by stereotypic deposits of Lewy bodies immunoreactive for α-synuclein
Patients have memory loss, fluctuating cognition, visual hallucinations, and often REM sleep behavior disorder; the latter features may be recognized only late in the patient’s course and an initial clinical diagnosis of LOAD is not uncommon
Structural MRI, FDG-PET (the pattern differs from AD), MRI-ASL CBF imaging, SPECT and DAT scans
No CSF or blood biomarkers, but CSF biomarkers for AD are frequently available
Mild frontal atrophy and loss of pigmentation in substantia nigra and locus ceruleus
Lewy bodies and neurites in neocortex, cholinergic neurons of the nucleus basalis in the basal forebrain, in limbic regions (anterior cingulate cortex, amygdala, hippocampal formation, entorhinal cortex), and brainstem nuclei (see text for detail); immunoreactive for α-synuclein
APOE ε4, SNCA , GBA , and newer variants recognized by GWAS
The most common differential diagnosis of DLB at the time of autopsy is AD. As described above, some AD pathologies are typical in DLB. However, neocortical NFT pathology is sparse in most cases. Amyloid pathology is seen in almost all DLB patients, often in the form of non-neuritic, diffuse Aβ deposits, CAA involving arterioles, and sparse to moderate neuritic plaque pathology. In patients with dementia, amyloid-positive neocortical samples with sparse neuritic plaques and NFTs should be closely reviewed for neocortical Lewy bodies.
Atypical parkinsonian syndromes may also enter the differential of DLB, as patients with multiple system atrophy (MSA), PSP, and CBD may have cognitive impairment. Neuropathologic examination of DLB cases reveals only minimal white matter pathology and none of the characteristic striatal, basis pontis, nigral, or cerebellar atrophy of MSA. In addition, there are no readily identified oligodendroglial cytoplasmic inclusions by α-synuclein staining in DLB cases, further differentiating it from MSA. LB and Lewy body-like neuronal inclusions are not uncommon in MSA samples, especially in long-lived patients with cognitive impairment. However, these MSA cases have the typical distribution of striatonigral and/or olivopontocerebellar atrophy (OPCA), neuronal inclusions, and abundant oligodendroglial cytoplasmic inclusions, or “glial cytoplasmic inclusions” (GCIs).
DLB in large families is uncommon, unlike EOAD, but complex genetic risk factors are increasingly recognized. A common scenario is to perform a brain-only autopsy in a demented patient with a positive family history of dementia, only to identify DLB as the most significant neuropathology. For several reasons, this outcome is to be expected. First, the genetic heritability of DLB and the related synucleinopathy of PD is estimated at ∼30 %, so a family history of dementia may be present. Second, rare examples of familial DLB exist with point mutations in causative genes, similar to the phenomenon of APP , PSEN1 , and PSEN2 mutations driving EOAD. As with AD, both Mendelian and non-Mendelian mechanisms of heritability drive this neuropathology. Among non-Mendelian mechanisms, the most significant risk allele for DLB pathology is APOE ε4, linking this genetic risk factor for DLB to both AD and Aβ pathology. Notably, the association between DLB and APOE ε4 has been replicated in studies using both clinically diagnosed DLB and pathologically confirmed DLB.
Three genetic risk factors have been replicated in familial and sporadic DLB, and these are variations in APOE ε4, mutations and variants in the gene for α-synuclein on chromosome 4 ( SNCA ), and mutations and variants in the gene for glucocerebrosidase, located on chromosome 1 ( GBA, or GBA1 ). In regard to APOE , both ε3/ε4 and ε4/ε4 patients have the same increased relative risk as do AD patients, with the latter group having more than a 10-fold risk of developing DLB. As with AD, ε2 carrier status also appears to be protective against developing DLB. This implicates Aβ pathology as a key player in the formation of the fibrillar, α-synuclein aggregates identified in DLB patients, especially in regions of substantial pathologic overlap (e.g., amygdala, isocortex, basal forebrain). Several groups have also identified that the characteristic cognitive impairment of DLB hinges on the presence of comorbid Aβ pathology, and in practice, DLB cases typically have extensive non-neuritic plaque pathology with a relatively high Thal phase (≥3) and CAA.
GBA1 mutations and polymorphisms, especially the GBA1 E326K polymorphism, are also a risk factor for DLB, as well as PD and PDD. Glucocerebrosidase deficiency, also caused by GBA1 mutations, was previously described in the autosomal recessive lysosomal storage disorder of Gaucher disease. The deficiency of the lysosomal enzyme glucocerebrosidase in Gaucher patients allows the toxic accumulation of glucocerebroside in tissues, particularly macrophages. Thus the link between DLB and GBA1 implicates impaired lysosomal handling of cellular proteins as an additional important mechanism in α-synuclein and LB pathology. How impaired lysosomal function (via GBA1 ) and toxic accumulation of amyloid (via APOE ε4) contribute to the formation of cortical LBD and DLB is an area of active investigation.
Variants in SNCA , which encodes the synaptic protein α-synuclein, also contribute to DLB heritability. The association of SNCA polymorphisms and α-synuclein pathology and MAPT polymorphisms and tau pathology emphasize the potential link between proteinopathy and pathogenesis in NDDs. α-Synuclein is a ubiquitous synaptic protein whose exact function is not known, expressed in all brain regions and in both neuronal and non-neuronal cells. As with the tau protein and MAPT , alternative splicing of SNCA leads to several isoforms of the α-synuclein protein, with the predominant form being 140 amino acids in length. Causative mutations of SNCA lead to increased formation of fibrils of α-synuclein, increasing the likelihood of pathologic aggregates in vulnerable brain areas. Presumably through similar mechanisms, SNCA variants in DLB patients promote the process of pathologic aggregation of α-synuclein.
It is increasingly clear that glial pathology plays a role in both common and rare NDDs. In fact, genetic studies have expanded the basis for AD to include genes involved in microglial activity and the neuroinflammatory response. Although microglia do not conspicuously accumulate pathologic proteins in most NDDs, other glial cells do. Astrocytic and/or oligodendroglial inclusion pathology has long been recognized as a diagnostic feature of rare movement disorders (MSA, PSP, and CBD) and is frequently seen in ALS and FTLD.
A highly prevalent form of phospho-tau astrocytic pathology has also been recognized in older patients, occurring in >50 % of brain bank samples from patients with common dementing illness (e.g., AD, AGD), or with no neurological disease. A consensus panel adopted the term aging-related tau astrogliopathy (ARTAG) to encompass this range of astrocytic tau pathologies. ARTAG is a critical entity for neuropathologists and neurologists to be aware of for two reasons. First, ARTAG is ubiquitous in human aging and may closely mimic rare and serious neurological conditions, including CTE, FTLD-tau, PSP, and CBD. Second, early studies suggest that ARTAG may modify the clinical features of common diseases. Much remains to be learned about the genetics, clinical features, and biomarkers of this very common form of astrocytic tau pathology.
Patients with ARTAG pathology are usually older than age 60, and several studies have shown that male patients are more likely to have ARTAG pathology than female patients. The predominant clinical features, if any, will be those of comorbid pathologies. It is not currently known whether isolated ARTAG contributes to cognitive impairment in an aging brain without significant neuronal pathology. The presence of ARTAG also appears to be influenced by Braak and Braak NFT stage, with higher NFT stages correlating with greater ARTAG pathology, especially at the junction of cortex and cerebral white matter. Several studies have suggested that AD patients with increased ARTAG pathology in superficial lobar white matter are more likely to have language dysfunction and/or visuospatial symptoms. One study identified increased ARTAG pathology in AD patients with primary progressive aphasia symptoms. Much more work remains to be done to determine whether and how ARTAG contributes to the spectrum of symptoms in common dementias and/or the trajectory of cognitive decline. Currently, there are no neuroimaging or other biomarkers for ARTAG.
As described above, ARTAG is a common finding in aging and common age-related dementias. It is also one of the most common comorbid pathologies in rare NDDs that are not primary tauopathies, such as ALS with TDP-43 inclusion pathology. If there is comorbid neuropathology, the macroscopic findings are those of the predominant disease process.
The two most common types of astrocytic tau inclusions in aging are termed thorn-shaped astrocytes (TSA) and granular or fuzzy astrocytes . As discussed below, these are differentiated from less common astrocytic inclusions in rare NDDs, including ramified astrocytes (Pick disease), astrocytic plaques (CBD), and tufted astrocytes (PSP).
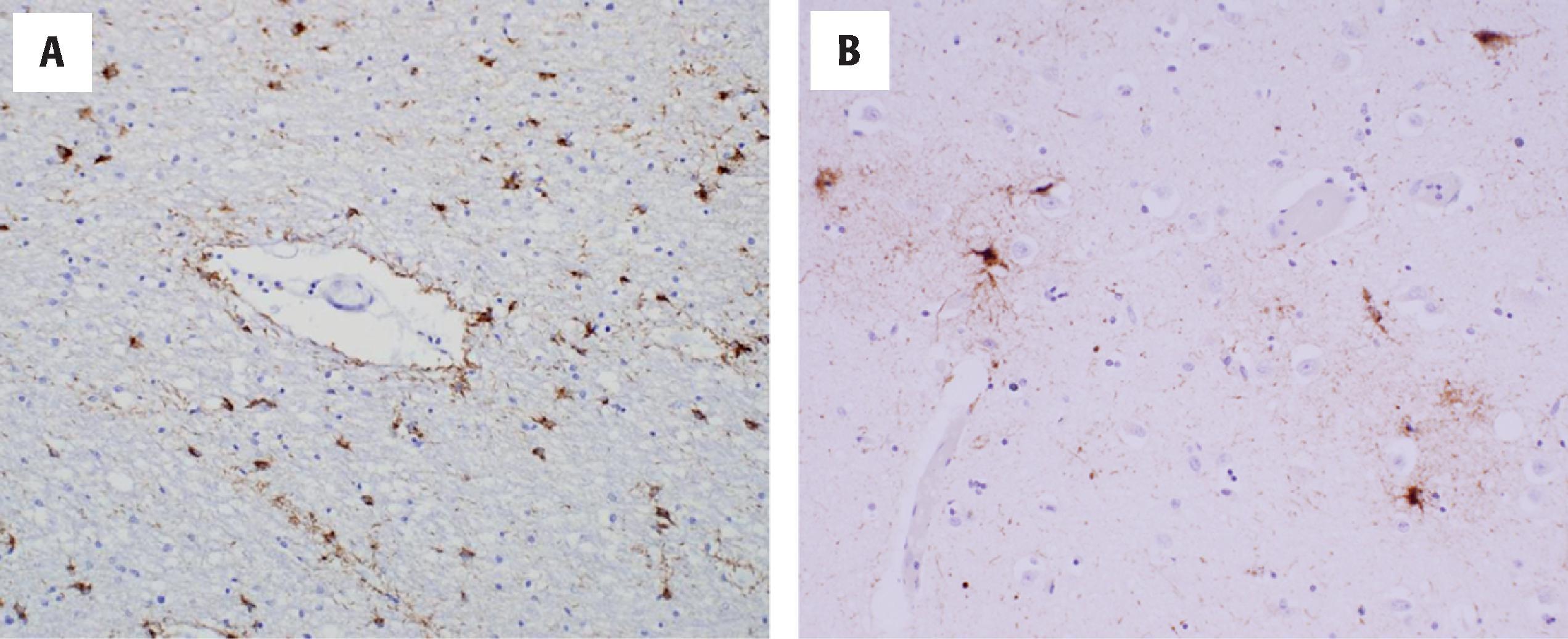
The thorn-shaped astrocyte, or TSA, is a phospho-tau–positive astrocyte that may be located in the subependymal, subpial, perivascular, and white and gray matter regions ( Fig. 6.12 ). In white matter, TSAs are most common in superficial white matter at the interface with overlying cortex, as well as in the perivascular region. Subpial TSAs are one of the most common forms of ARTAG, being most readily seen in autopsy sections that include basal forebrain and anterior commissure (region of anterior perforated substance), with the pial surface intact. In lobar regions, subpial TSAs may be seen in subpial cortex, including at the depths of sulci, which should not be confused with the hallmark lesions of CTE as described below. Within the brainstem, subpial TSAs are readily seen along the dorsolateral midbrain and occasionally in ventral brainstem, including at the cerebral peduncles and medullary pyramids. Subependymal TSAs are commonly seen in the amygdala region, adjacent to the temporal horn of the lateral ventricle, and in midbrain adjacent to the cerebral aqueduct. Gray matter ARTAG is characterized by both TSAs and granular or fuzzy astrocytes (GFAs), which may be seen in amygdala subnuclei, striatum, and various neocortical regions ( Fig. 6.12 ). As the name implies, GFAs are limited to gray matter, unlike TSAs.
A highly prevalent form of astrocytic tau pathology in human aging, occurring in more than half of brain bank samples.
The clinical implications of ARTAG are not known. Recent studies have suggested that ARTAG may contribute to the spectrum of symptoms in dementia patients, but further study is needed.
No specific imaging features or biomarkers of ARTAG have been identified to date.
The macroscopic findings are those of the primary disease process, if a neurological disease is present. ARTAG may also be identified in the aging brain without specific patterns of atrophy or gross abnormalities.
Phospho-tau immunostains and 4R tau stains demonstrate TSA in subependymal, subpial, perivascular, white and gray matter regions, and GFAs in gray matter.
Genetic risk factors have yet to be determined.
TSAs and GFAs may be present in various combinations in the same autopsy specimen and there is not a stereotypic pattern across all cases. TSAs have prominent perinuclear staining by phospho-tau stains, such as AT8, and short, stubby staining of astrocytic processes that give rise to a thorn-like appearance. GFAs also have dense, perinuclear cytoplasmic staining with phospho-tau immunostaining. Unlike TSAs, tau immunoreactivity in the processes of GFAs is more diffuse, patchier, and granular (hence the name granular/fuzzy) ( Fig. 6.12 ). Both TSAs and GFAs are variably positive by silver staining methods, such as Gallyas staining. In addition, both astrocytic lesions show immunoreactivity to antibodies to the 4R tau isoform and are negative for 3R tau. This differs from typical neuronal lesions, where both 3R and 4R isoform staining is seen. In both common and uncommon astrocytic lesions, with the exception of Pick disease, it is 4R tau that predominates. Ultrastructural studies of astrocytic tau pathology in aging (few in number) have shown the tau more closely resembles straight filaments and that the paired helical filaments of neuronal NFTs are not seen.
One of the major entities in the differential diagnosis of ARTAG is CTE, a pathologic alteration that frequently is associated with repetitive head trauma. In contrast to ARTAG, the phospho-tau pathology of CTE is present in both neurons and glia at the depths of sulci. This distinction is critical because the astrocytic pathology in CTE has the morphologic appearance of TSAs, as seen in ARTAG. The combination of perivascular neuronal and glial phospho-tau lesions, at the depths of multiple cerebral sulci, in tandem with other supporting features (described later), is diagnostic of CTE neuropathologic change. Conversely, depth of sulcus, subpial, or gray matter ARTAG limited to TSAs and GFAs should not be used for the pathologic diagnosis of CTE neuropathologic change. A recent community-based autopsy study in older adults showed ARTAG was highly prevalent in older individuals, with TSAs seen at the depths of sulci, but the pathognomonic lesion of CTE was not identified in a single case. Unlike subpial ARTAG, which is ubiquitous, the pathognomic lesion of CTE is extremely rare outside the setting of significant and repetitive head trauma. There does not appear to be a lobar predominance for this type of subpial ARTAG. The shared depth of sulcus location of ARTAG and CTE, and the involvement of astrocytes in both processes, raises the question of whether there are mechanistic links between these entities.
The unique 4R-positive astrocytic lesions of PSP (tufted astrocytes) and CBD (astrocytic plaques) are also in the differential of ARTAG on neuropathologic evaluation. Thorny astrocytes in ARTAG may strongly resemble tufted astrocytes of PSP. Furthering confusion, both astrocytic lesions are 4R-positive, both may be Gallyas stain-positive, and both may occur in frontal cortex, striatum, and limbic structures such as amygdala. A critical element in the diagnostic consideration is the presence or absence of an atypical parkinsonian disorder, or even simply parkinsonism as in less common PSP variants with a lower tau burden. In addition, PSP patients may have comorbid ARTAG, so both diagnoses may be considered in the same specimen. Indeed, one of the earliest descriptions of ARTAG was as a secondary astrocytic pathology in the setting of PSP. On phospho-tau staining, the tufted astrocytes of PSP lack the dense perinuclear staining of TSAs, instead having tau-positivity limited to thick, proximal portions of astrocytic processes. Additionally, tufted astrocytes may be ubiquitinated, staining with immunostains to ubiquitin and the polyubiquitin‐binding protein p62/sequestosome 1 (p62). In contrast, TSAs and GFAs are ubiquitin-negative and p62-negative. The astrocytic plaque of CBD is characterized by phospho-tau reactivity in thin, distal astrocytic processes with no perinuclear cytoplasmic staining, which is not likely to be confused with ARTAG pathology. Lastly, cardinal nuclei implicated in the neuropathology of both PSP and CBD are spared in the much more common astrocytic tau pathology of ARTAG. Structures such as globus pallidus, subthalamic nucleus, red nucleus, and dentate nucleus of cerebellum are rarely if ever sites of ARTAG pathology.
Tau is a protein that binds to and stabilizes microtubules, which is critical for maintaining cytoskeletal stability and cell function. A single isoform of tau is present in the fetal brain, whereas in adult brains there are six tau isoforms. Adult isoforms are generated by alternative mRNA splicing of the gene for tau on chromosome 17 (17q21-22), MAPT. Alternative splicing of exons 2, 3, and 10 of MAPT results in tau isoforms ranging in size from 352 amino acids to 441 amino acids. These tau isoforms differ in the presence or absence of 29 and 58 amino acid inserts toward the N-terminus of the tau protein, as well as by the number of 31 amino acid repeats in the microtubule-binding domain of tau, located toward the C-terminus. The 3R and 4R tau isoforms differ in the number of these repeats. Polymorphisms in the MAPT gene result in two major haplotypes, termed H1 and H2, with the H1/H1 genotype being at greatest risk for the tauopathies PSP and CBD.
In cytoplasmic tau inclusions, including in astrocytes and neuronal NFTs, the soluble tau protein becomes hyperphosphorylated with a decreased binding affinity for microtubules. This form of tau becomes insoluble and filamentous and may be detected by silver stain-based techniques, a range of antibodies to both tau and more specifically phosphorylated tau, and, eventually, antibodies to proteins such as ubiquitin. Various phospho-tau antibodies (e.g., AT8, PHF-1, and AT100) target different phosphorylation sites in the tau protein, and these have largely replaced histochemical techniques, as they are more sensitive to a range of tau pathologies. One of the most commonly used in clinical practice, the AT8 antibody, targets tau phosphorylated at the serine 202 and threonine 205 residues. Immunoblotting techniques in various tauopathies have also demonstrated that various sizes of insoluble/filamentous tau may be present, with 3R-predominant tauopathies containing 60 and 64 kDa bands and 4R-predominant tauopathies containing 64 and 68 kDa bands. Not surprisingly then, the prototypical 3R/4R tauopathy, which is AD, contains all three bands: 60, 64, and 68 kDa. As described above, antibodies to the 3R and 4R isoforms are available and may be useful diagnostically at autopsy.
There is currently very little known about the genetic risk factors that contribute to ARTAG, in large part because the entity has only rarely been codified with a harmonized evaluation system proposed. Whether ARTAG is influenced by APOE status, MAPT haplotypes (H1 versus H2), or other genetic polymorphisms yet to be recognized, is not currently known. Moreover, the basis for 4R but not 3R accumulation in TSAs and GFAs in ARTAG is not understood. This non-ubiquitinated form of phospho-tau has been analogized to the neuronal pretangle in AD, but unlike neurons, astrocytes have very low levels of endogenous tau production. Thus, 4R tau accumulation may result from uptake of neuronal tau in the immediate environment (phagocytosis), spread of tau from neurons to astrocytes, or increased levels of endogenous tau production. It is worth considering that for both ARTAG and PSP, isolated astrocytic tau may be seen on phospho-tau immunostains, without adjacent neuronal tau inclusions. This would suggest that a component of endogenous tau pathology in astrocytes is possible. Conversely, the association of ARTAG with increased Braak and Braak NFT stage in AD would suggest an interdependence of astrocytic and neuronal tau pathologies.
Limbic-predominant age-related TDP-43 encephalopathy (LATE) is a common neuropathology in aging that may occur with or without comorbid AD pathology. LATE is one of the most common neuropathologies in the oldest old patients (those ≥85 years), and patients may have concomitant hippocampal sclerosis (HS). These patients may present with a memory loss predominant form of dementia that mimics a late-onset and mild form of AD. Based on its demographic, pathologic, and clinical features, LATE was previously referred to as HS-Aging or hippocampal sclerosis dementia. Hippocampal sclerosis dementia was first recognized as a non-AD amnestic syndrome ∼25 years ago. This syndrome was recognized in patients with dementia and ubiquitinated inclusions and hippocampus, although with little or no AD neuropathology.
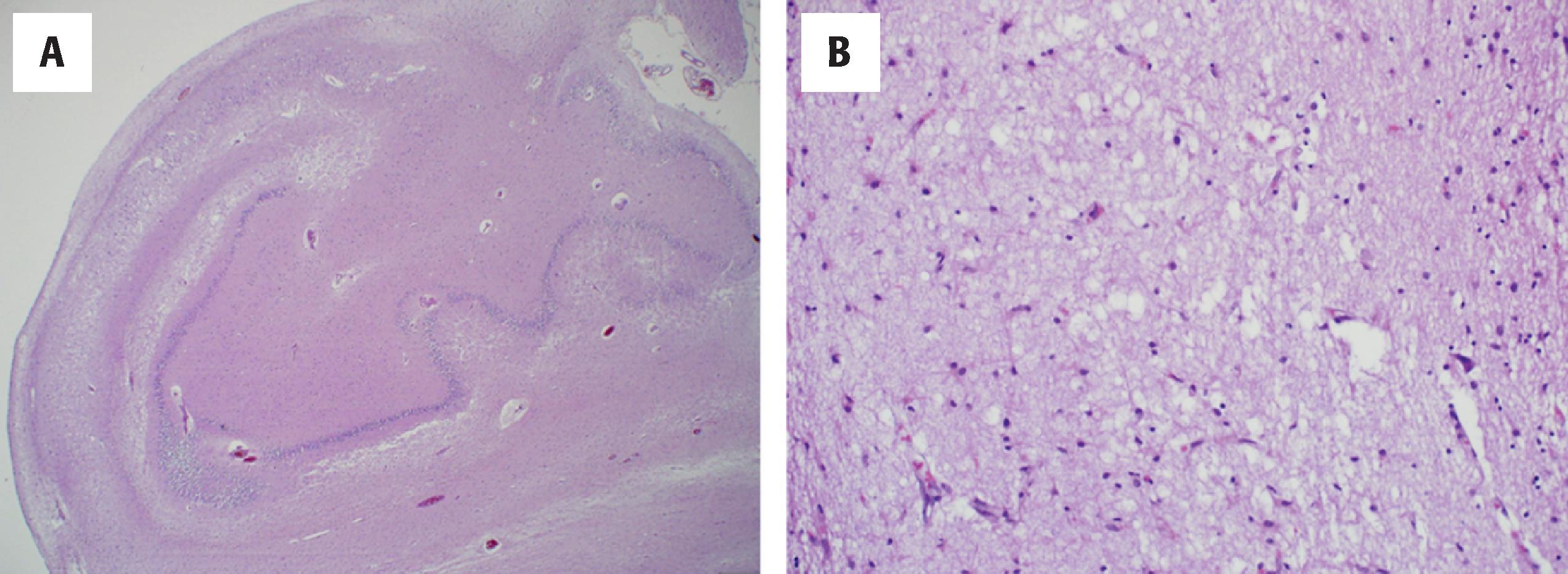
Recently, a working group proposed the term LATE to more clearly define this common entity of aging and clarify its distinction from other forms of HS, as seen in epilepsy and following vascular brain injury. The term LATE is now applied to this age-related TDP-43 proteinopathy of older patients, and its application does not require the presence of pathologic HS ( Fig. 6.13 ).
The clinical features of LATE are an area of ongoing investigation. However, in the oldest old population, patients with LATE pathology and associated HS present with mild cognitive impairment and memory loss. It is a ubiquitous pathology and likely explains many diagnoses of slowly progressive mild AD in very old patients. In fact, studies of community-based autopsy cohorts have shown LATE pathology with TDP-43 inclusions in up to 30 %–50 % of those >80 years at the time of death. Although the pathology may be focal and mild, many cases have sufficient TDP-43 pathology to explain the patient’s cognitive impairment, especially in the absence of significant AD neuropathology. Furthermore, TDP-43 has been shown to exert an independent effect on global cognitive impairment when non-TDP-pathologies, including amyloid, tau, and vascular injury, are controlled for.
Patients with LATE may have concomitant AD neuropathologic change (intermediate and high AD neuropathology). In these cases, the macroscopic features of AD neuropathologic change predominate, including frontotemporal and parietal atrophy with sparing of motor cortex. In addition, LATE and TDP-43 pathology may contribute to HS. Hippocampal sclerosis is characterized by atrophy of the hippocampi that is well out of proportion to the overall level of cerebral atrophy ( Fig. 6.13 ). Coronal sections of the brain in a plane through the posterior hippocampus and lateral geniculate nucleus reveal atrophic, firm, and white-appearing hippocampi in which the typical gray-white matter contrast of hippocampal formation is difficult to discern. In the absence of comorbid AD, LATE with HS reveals the same firm atrophic hippocampi with an even greater discrepancy between hippocampus and non-atrophic neocortical regions.
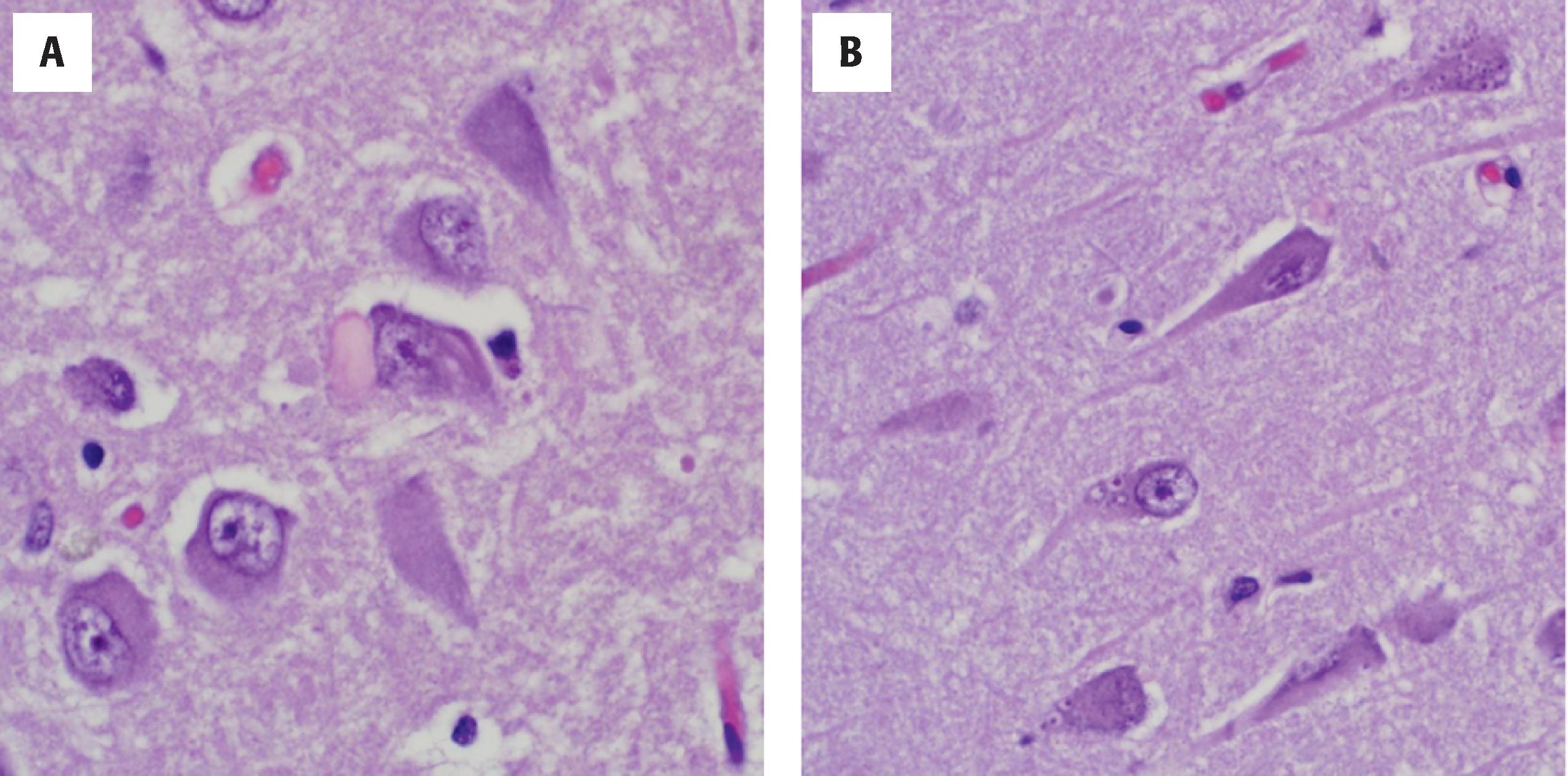
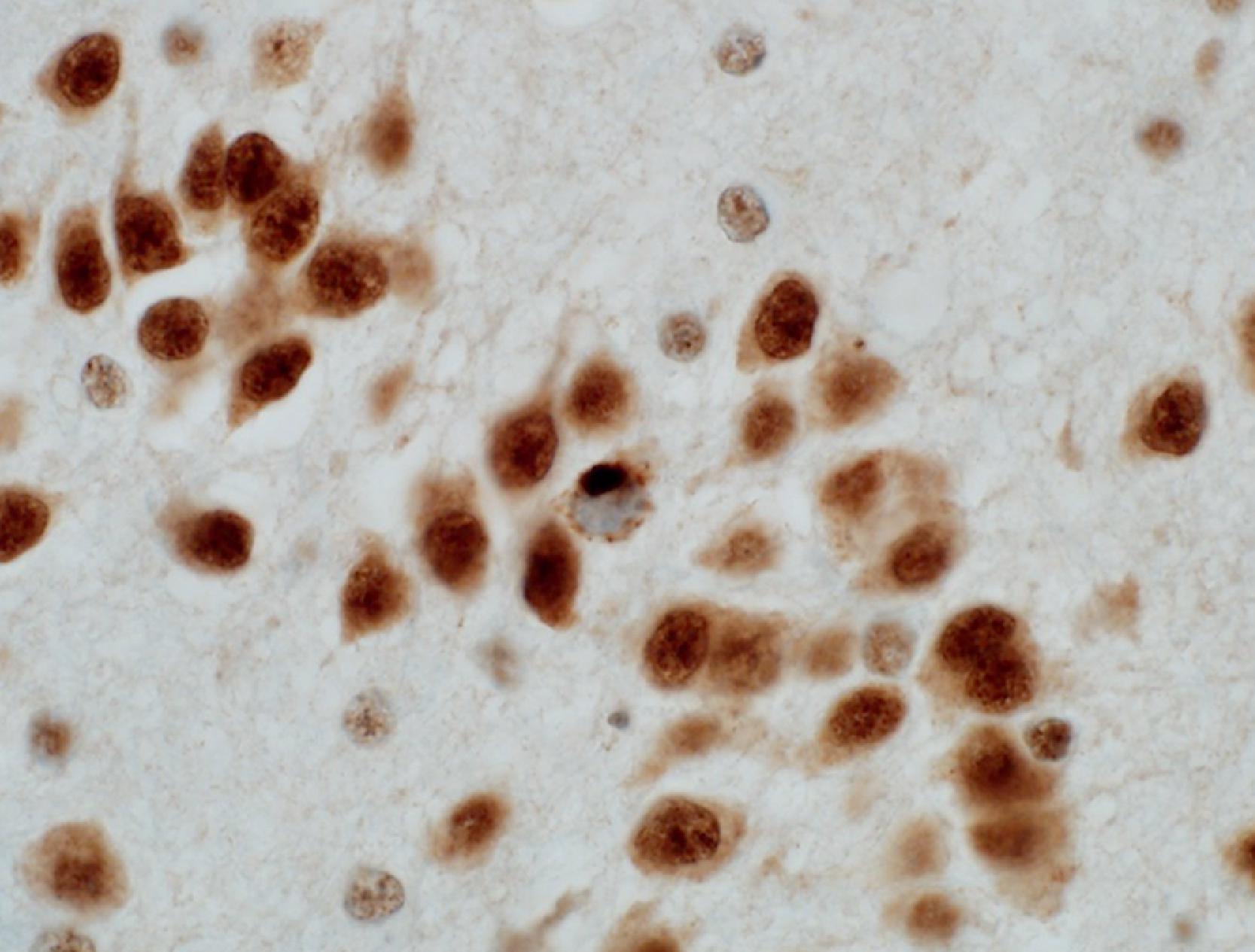
A key microscopic finding in hippocampal sclerosis, seen in some LATE cases, is massive neuronal loss in sector CA1 and subiculum with reactive astrocytosis. In contrast, pure AD without comorbid TDP-43 pathology and/or HS does not typically have the same extent of astrocytosis. Neurons of dentate gyrus and hippocampal formation also have inclusions of TDP-43, the pathological hallmark of LATE and LATE neuropathologic change (LATE-NC) ( Fig. 6.14 ). TDP-43 is a DNA/RNA-binding protein that plays a critical role in multiple human NDDs, including ALS and FTLD. Examination of cases with LATE reveals the earliest foci of TDP-43 pathology are in the region of the amygdala, including within amygdala subnuclei proper, entorhinal and transentorhinal cortex, and in adjacent white matter. The pathologic inclusions are not stereotypic. In two of the more common appearances, TDP-43 inclusions appear fibrillary and NFT-like, colocalizing with tau inclusions in aging and AD. In another pattern, TDP-43 accumulates in neuronal cytoplasmic inclusions in lamina II of the limbic cortex associated with numerous short neurites. This pattern may appear similar to FTLD ( Fig. 6.15 ), albeit more limited in distribution and without the extensive neuronal loss and spongiosis that characterizes FTLD.
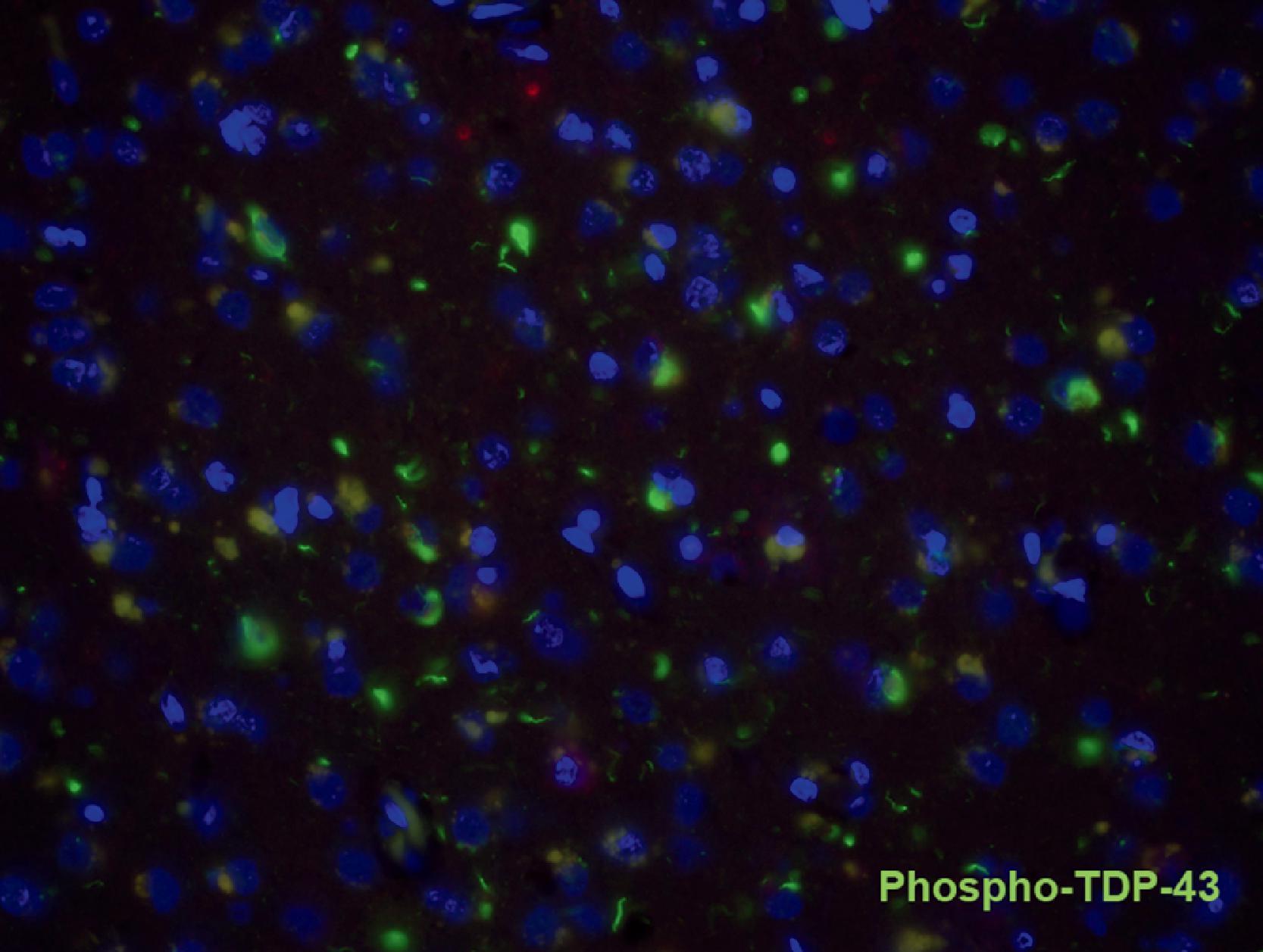
Several staging proposals exist to characterize LATE TDP-43 pathology in the setting of aging and AD pathologies. In the simplest three-tier model, TDP-43 pathology in the amygdala region is designated as stage I. More conspicuous involvement of the hippocampus has been noted in stage II, and in stage III there is involvement of other regions, including the frontal cortex. A critical knowledge gap is that the specific cell populations and structures that are vulnerable to phospho-TDP pathology are not known, even in sites of stage I pathology. Most importantly, how TDP-43 pathology impacts cognition and the patient’s functional status across different pathologic stages is poorly understood. Careful clinical-pathologic correlational studies are required using state-of-the-art pathologic approaches and diagnoses in autopsy-based samples with rich clinical datasets.
A highly prevalent neuropathology in human aging and as a comorbid pathology in AD and DLB; may be present with or without hippocampal sclerosis; most common in the oldest old (patients ≥85 years)
Mild cognitive impairment with memory loss
May be clinically diagnosed as slowly progressive AD
Structural MRI demonstrates hippocampal atrophy out of proportion to the level of global cerebral atrophy
In the setting of hippocampal sclerosis, the bilateral hippocampi may be atrophic and firm; when LATE is a comorbid pathology, the macroscopic features of the primary process may predominate
Massive neuronal loss in sector CA1 and subiculum with reactive astrocytosis in patients with hippocampal sclerosis
TDP-43 inclusion pathology is common in the amygdala, entorhinal cortex, transentorhinal cortex, hippocampal formation, and basal forebrain, and may also involve neocortex (frontal cortex)
Genes associated with LATE and HS include APOE , GRN , TMEM106B , and ABCC9
Although FTLD-TDP typically affects younger patients and has greater TDP-43 pathology, the precise boundary between LATE and late-onset FTLD-TDP has yet to be defined. One major difference is that brains with LATE-NC do not have the circumscribed, frontal, and temporal atrophy that characterizes FTLD-TDP. Patients with FTLD-TDP will typically have greater neuron loss in the cortical ribbon, with a more widespread and severe TDP-43 proteinopathy, than is seen in LATE.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here