Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Primary neoplasms of the vagina, whether benign or malignant, are rare. Primary carcinomas are the most common malignant tumors and account for approximately 2% of all gynecologic malignancies. Among vaginal carcinomas, in situ and invasive squamous carcinomas are most frequent. As a general rule, when evaluating a malignant tumor involving the vagina, it is essential to exclude a metastatic origin. This chapter covers the most frequent primary neoplastic lesions of the vagina. Regarding mesenchymal lesions, most entities are covered in Chapter 4 (including smooth muscle tumors).
This is an uncommon papillary lesion lined by Müllerian-type epithelium that typically involves the vagina or uterine cervix.
Müllerian papilloma typically occurs in girls less than 10 years of age, although it has been reported occasionally in adults. Patients usually present with vaginal bleeding or a mass, which on gynecologic examination may appear as “grape-like cluster.” The lesion is most common in the posterior vagina, followed by anterior and lateral walls. Rarely, it may be intramural.
This lesion is typically well-circumscribed, papillary, or polypoid and measures up to 5 cm.
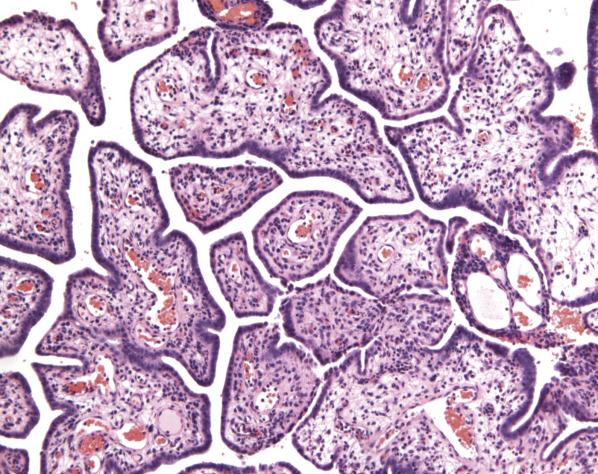
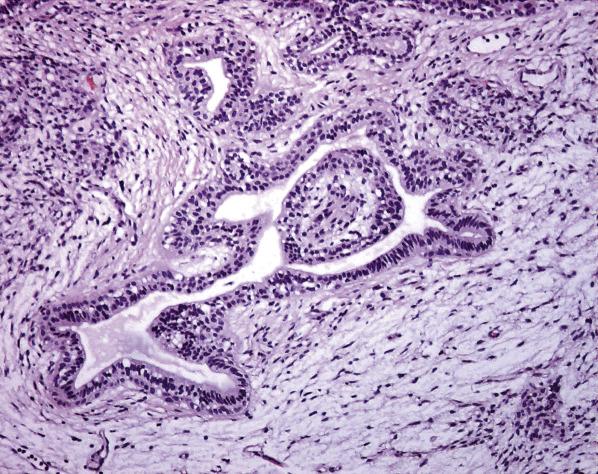
Müllerian papilloma is characterized by papillary fronds lined by columnar or cuboidal epithelium ( Fig. 6.1 ). The fibrovascular core is usually thin but can appear edematous or myxoid. The lining epithelial cells are cuboidal to columnar and have eosinophilic cytoplasm, uniform bland nuclei, and absent or rare mitotic figures. The epithelial lining can form solid nests with scattered glandular lumina containing eosinophilic periodic acid–Schiff (PAS) positive and diastase-resistant globules. Hyaline globules can be seen. Rarely, heavily pigmented melanocytes may be observed within the epithelium.
The epithelial cells are positive for EMA, CEA, and CAM 5.2, and focally positive for CA125.
Fibroepithelial polyp, condyloma acuminatum, embryonal rhabdomyosarcoma, and clear cell adenocarcinoma may enter into the differential diagnosis as they all are characterized by papillary to polypoid growth. Fibroepithelial polyp and condyloma acuminatum typically have blunt papillae and are lined by mature squamous as opposed to cuboidal to columnar epithelium. Fibroepithelial stromal polyps show a prominent vascular core and scattered stellate and multinucleate stromal cells in the subepithelial stroma. Exophytic condyloma exhibits koilocytes, at least focally. Embryonal rhabdomyosarcoma characteristically shows condensation of primitive rhabdomyoblasts underneath the surface epithelium (so-called cambium layer) in addition to spindled or strap-shaped cells with brightly eosinophilic cytoplasm within a loose myxoid stroma; these neoplastic cells are positive for skeletal muscle markers, including Myo-D1 and myogenin, antibodies directed against skeletal muscle-specific nuclear transcription factors. Clear cell carcinoma occurs in an older age population, usually displays haphazard infiltration into the vaginal wall, and shows distinctive tubulocystic and solid growth patterns. Unlike papilloma, nuclear atypia in clear cell carcinoma is significant, comprised of enlarged hyperchromatic nuclei protruding towards the lumen (“hobnail” appearance).
Müllerian papilloma is treated with local excision. It may recur, and rarely progress to a borderline-type neoplasm (i.e., cytologic atypia and conspicuous mitotic activity). Clear cell carcinoma arising in a Müllerian papilloma has been reported.
This uncommon tumor is characterized by a predominance of stromal-type cells with a minor component of glandular and/or squamous elements. Although this tumor has ultrastructural evidence of myoepithelial derivation, phenotypically it lacks true mixed/dual myoepithelial differentiation as seen in other anatomical sites. Therefore, the designation of “spindle cell epithelioma” is preferred.
Patients range in age from 20 to 80 (mean 40) years at presentation. Most cases are detected incidentally during routine pelvic examination as a submucosal mass, typically located in the posterior wall close to the hymenal ring.
The tumor ranges in size from 1 to 9 cm. It is well-circumscribed and on cut section appears gray to white with a rubbery or soft gelatinous consistency.
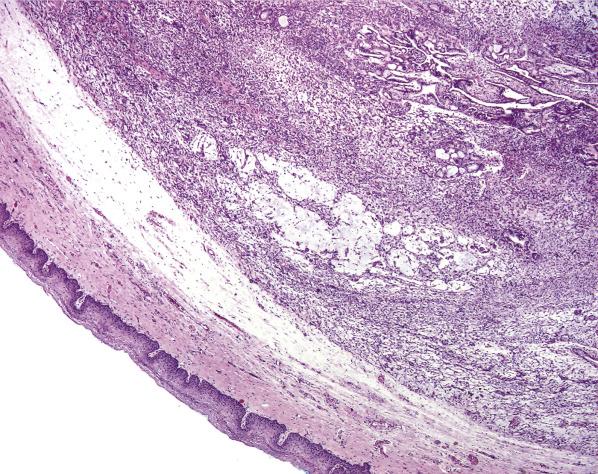
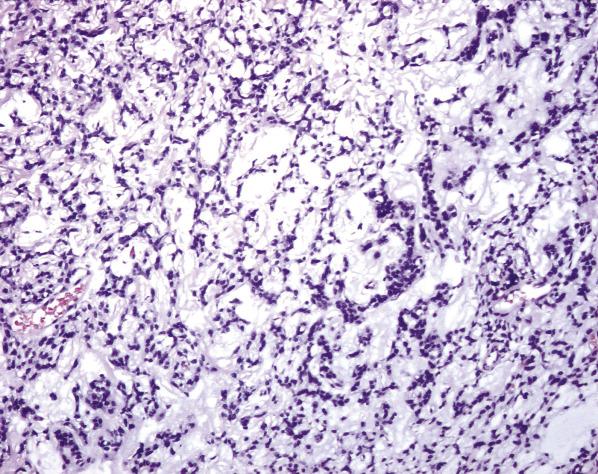
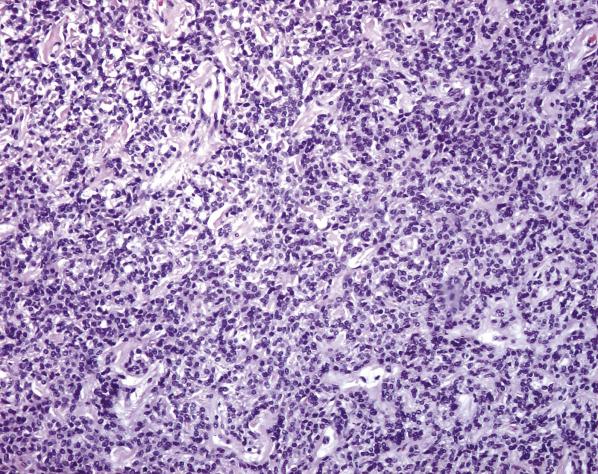
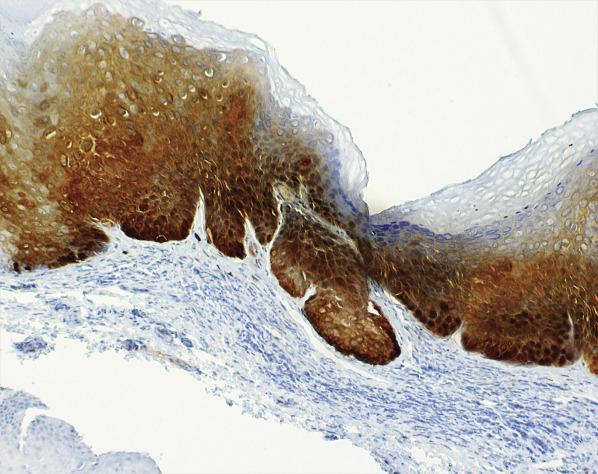
The tumors are well circumscribed and nonencapsulated with a smooth expansile margin ( Fig. 6.2 ). They are typically superficially located, separated from the epithelium by scant connective tissue. The cellular stromal component, which is typically predominant, shows cells with scant cytoplasm and bland nuclei that range from oval or round to spindle. They can grow in sheets, fascicles, nests, or cords, or have a reticulate growth ( Figs. 6.3 and 6.4 ). The background can appear myxomatous or hyalinized; hyaline globules may be seen and are secondary to condensation of stromal matrix. Mitotic figures are usually rare or absent. A minor epithelial component, either glandular or squamous, is generally present towards the periphery of the lesion ( Fig. 6.5 ). The glands are lined by cuboidal or columnar epithelium; they can have areas of squamous metaplasia or contain PAS-positive, diastase-sensitive luminal material. In some cases, there are no glandular elements but only numerous squamous morules.
The epithelial and spindle cells are positive for keratin AE1/E3, WT-1, ER, PR, and CD10. The spindle cells can be variably positive for keratin 7 and EMA (and rarely keratin 20). These cells can also express smooth-muscle actin, desmin, and, less commonly, h-caldesmon. They are typically negative for S-100. By electron microscopy, the stromal-like cells lack myofibrils with dense bodies, pinocytotic vesicles, and basal lamina, features typically seen in myoepithelial cells.
This lesion should be distinguished from squamous cell carcinoma , which can acquire a predominant spindle cell morphology (“spindle cell variant”). In carcinoma, the spindle cells show evident cytologic atypia and conspicuous mitoses; areas of squamous differentiation also appear atypical. In challenging cases, p16 overexpression by immunohistochemistry and demonstration of human papilloma virus (HPV) by molecular techniques will support the diagnosis of carcinoma. Since the spindle cell component usually predominates, the most common differential of spindle cell epithelioma is with mesenchymal lesions such as leiomyoma . Both share similar growth patterns (corded, nested, and fascicular), have a myxomatous background, and show extensive immunohistochemical overlap. In limited samples or when the epithelial component is not identified, heterogeneous staining for smooth muscle markers should raise the possibility of spindle cell epithelioma. Endometrial stromal neoplasms rarely involve the vagina but must be considered in the differential as, similarly to spindle cell epithelioma, they are cellular and are positive for CD10, ER, PR, and WT-1. However, EMA and smooth muscle markers are typically negative or weaker in endometrial stromal tumors than in spindle cell epithelioma.
Spindle cell epithelioma is a benign neoplasm that can recur locally months or years after the initial diagnosis. Treatment is mainly surgical for both initial and recurrent tumors.
Benign tumor with predominance of stromal-type cells and minor component of glandular/squamous elements
Uncommon
Usually lower posterior vaginal wall
20–80 (mean 40) years
Most frequently an incidental finding; rarely presents with vaginal bleeding
Surgical excision
Long-term follow up required, as late recurrences can occur
Well circumscribed
Gray or white with a gelatinous, soft, or rubbery consistency
1 to 9 cm
Nonencapsulated, with well-demarcated expansile margin
Fascicular, nested, reticular, or corded growth of spindle cells; myxomatous background may be present
Minor epithelial component: glandular and/or glycogenated/metaplastic squamous component
Bland nuclei with rare or absent mitoses
Keratin AE1/E3, WT-1, ER, PR, and CD10 positive in epithelial and spindle cells
Keratins 7 and 20, EMA, calretinin, and muscle markers variably positive in spindle cells
S-100 negative in spindle cells
Spindle cell variant of squamous cell carcinoma
Leiomyoma
Endometrial stromal neoplasm
Squamous intraepithelial lesions of the vagina (VAIN) are rare, with an incidence of approximately 0.2–0.3 cases per 100,000 women in the United States. Associated risk factors include concurrent or prior cervical or vulvar squamous intraepithelial lesion, older age, low socioeconomic status, history of HPV infection (most commonly types 16 and 18) or sexually transmitted diseases, multiple sexual partners, smoking, immunosuppression, history of radiation therapy, and diethylstilbestrol (DES) exposure.
Patients range in age from 16 to 84 (mean 47–53) years according to different series. Most patients are asymptomatic. The abnormality is frequently detected after colposcopic examination and biopsy for an abnormal Papanicolaou smear. Less commonly, a vaginal lesion is found during routine gynecologic examination, or patients present with symptoms such as recurrent vaginal discharge or vaginal bleeding. Not infrequently, squamous intraepithelial lesions of the vagina are discovered incidentally during the evaluation of a vulvar or cervical abnormality.
Squamous intraepithelial lesions are more common in the upper third of the vagina and is multifocal in approximately 60% of cases. Usually, there is no grossly identifiable lesion; however, sometimes mucosal irregularities or color changes may be detected on examination. The most common colposcopic abnormality is acetowhite epithelium followed by punctation and, rarely, mosaicism.
Vaginal squamous intraepithelial lesions can be flat or exophytic. Depending on the degree and extent of the squamous atypia, they are classified as low-grade squamous intraepithelial lesion (VAIN1) and high-grade squamous intraepithelial lesion (VAIN2 and VAIN3) as per the lower anogenital squamous terminology (LAST).
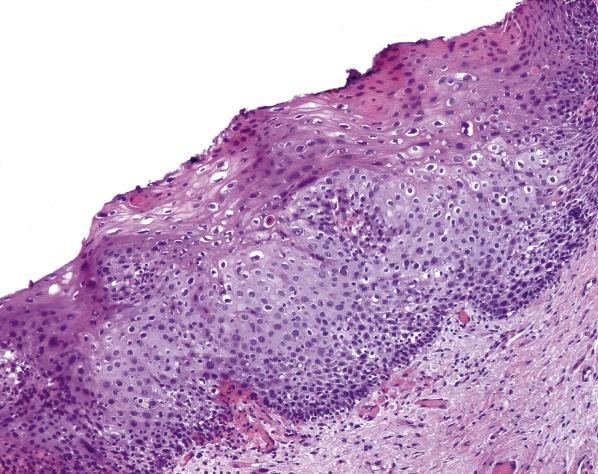
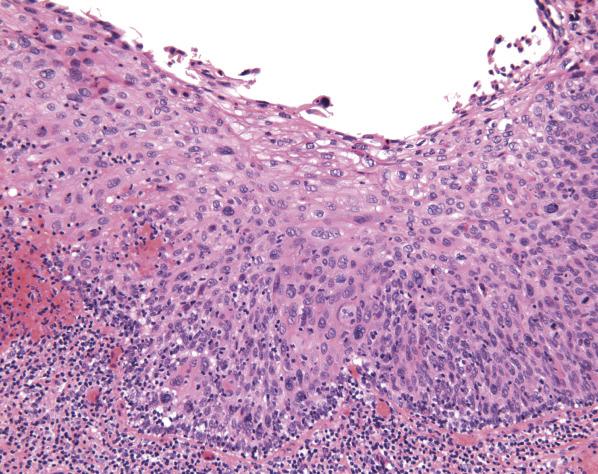
Low-grade squamous intraepithelial lesion (LSIL, VAIN1) encompasses epithelial changes including koilocytosis in the upper third of the epithelium (nuclear enlargement detectable at low power magnification, rigid and clear perinuclear halos of variable size, irregular nuclear contours, hyperchromatic nuclei, binucleation). There is retained maturation and organization of the lower third of the epithelium ( Fig. 6.6 ). High-grade squamous intraepithelial lesions (HSIL) display progressive loss of maturation and cell organization involving the lower two-thirds and moderate to severe nuclear atypia (i.e., cell crowding, high nuclear-to-cytoplasmic ratio, significant variability in nuclear size, coarse chromatin, and frequent mitotic activity, including atypical mitoses). Changes involving the lower third or two-thirds, with preserved maturation of the upper third, have been categorized as VAIN2 ( Fig. 6.7 ) whereas full-thickness atypia and loss of maturation is categorized as VAIN3 ( Fig. 6.8 ); these are now categorized as HSIL. Koilocytosis may or may not be seen.
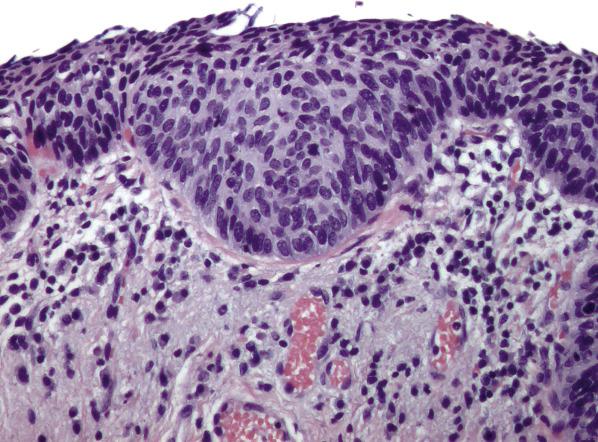
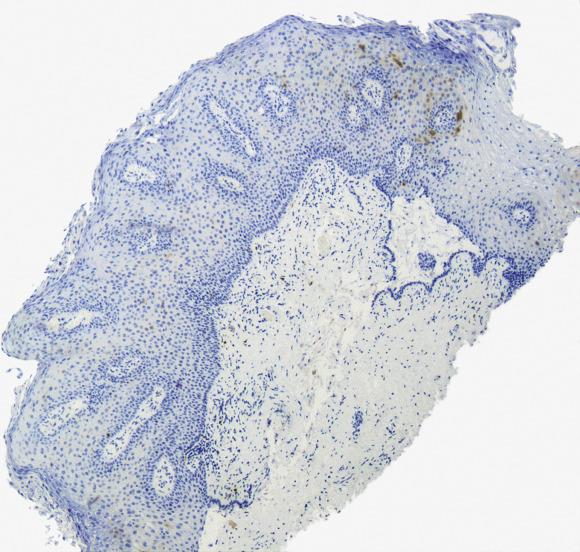
p16 is the most robust immunomarker to distinguish HSIL (VAIN2 or 3) from their mimics (atrophy, and reparative epithelial changes among others). In HSIL, p16 is overexpressed (strong and diffuse nuclear and cytoplasmic staining of at least the lower third of the epithelium, namely “block staining”) ( Fig. 6.9 ). In contrast, mimics including most low grade squamous intraepithelial lesions, show either a negative or nonspecific p16 staining (i.e., cytoplasmic-only or patchy nuclear staining) ( Fig. 6.10 ). Of note, p16 may be strongly positive in low-grade lesions therefore this marker should not be used as the sole criterion in this distinction but rather the morphology should guide the diagnosis. Ki-67 and ProExc may sometimes be used as adjunctive diagnostic markers. In normal vaginal mucosa and LSIL, Ki-67 expression is confined to the parabasal epithelium, whereas in HSIL it shows nuclear positivity in superficial layers.
Distinction between LSIL and HSIL is usually straightforward if orientation and integrity of the specimen is maintained. Challenging issues include tangentially sectioned or partially denuded epithelium. Attention should be focused on the lower epithelial layers as in low-grade squamous intraepithelial lesions the organization and nuclear uniformity are retained. If p16 is applied, one should be aware that both HSIL and LSIL can be diffusely positive; however, if p16 is negative or only patchy positive, it excludes a high-grade lesion. The following issues in differential diagnoses apply more commonly to HSIL. In reactive inflammatory atypia , the epithelial cells may show increased nuclear/cytoplasmic ratio, nuclear hyperchromasia, and mitoses; however, the nuclei are evenly distributed and typically have dispersed chromatin and prominent nucleoli. Inflammatory cells are often interspersed between the epithelial cells, typically showing intercellular edema (spongiosis). Occasional binucleate cells and perinuclear halos (pseudokoilocytosis) may be seen but the nuclei do not show the enlargement (detectable at low power magnification), contour irregularity, and hyperchromasia diagnostic of koilocytosis. p16 may show patchy, but not “block” positivity within the squamous epithelium. Atrophy , including transitional cell metaplasia , is characterized by hypercellularity, lack of maturation, increased nuclear-to-cytoplasmic ratio, and dark evenly distributed chromatin. In contrast to HSIL, atrophy lacks significant nuclear pleomorphism, loss of organization, or mitotic activity. In addition, in transitional cell metaplasia, the nuclei in the upper third of the epithelium are perpendicularly oriented to the basal epithelium nuclei (so-called streaming pattern) and display frequent nuclear grooves. In radiation-induced atypia , the nuclei are enlarged but the nuclear-to-cytoplasmic ratio is low, the chromatin has a smudgy appearance (instead of the more clumped hyperchromasia of intraepithelial lesions) and the cytoplasm is often vacuolated, mitoses are absent or rare, and stroma and vessels appear hyalinized. Caution should be exercised before making a diagnosis of HSIL in a patient with a history of prior radiation. Vaginal micropapillomatosis (mucosal excrescences) has a papillomatous appearance and thus may be misconstrued as low-grade dysplasia, but it has no evidence of koilocytosis.
Patients with LSIL can be followed every 6 months with Papanicolaou test and colposcopy as they have a low risk of progression to high-grade lesions. If persistent, treatment with carbon dioxide laser or topical agents, including 5-fluorouracil (5-FU), imiquimod or trichloroacetic acid is recommended. Patients with HSIL have an overall recurrence rate of ∼33% after appropriate treatment, which includes surgery and, if invasion is excluded, CO2 laser, or topical therapy such as 5-FU, imiquimod, or trichloroacetic acid. Moreover, concurrent or subsequent invasive squamous cell carcinoma has been reported in 10%–28% patients with vaginal HSIL; thus, close follow-up after excision is required.
Squamous epithelium with variable degrees of atypia and loss of maturation, caused by HPV infection
Rare; 0.2–0.3 per 100,000 women in United States
Most common in upper third of vagina
33% overall recurrence rate
2%–5% risk of progression to invasive squamous carcinoma after appropriate treatment
16–84 (mean 47–53) years
Commonly asymptomatic and detected by abnormal cervicovaginal cytology
Vaginal bleeding or discharge (rare)
Commonly associated with squamous intraepithelial lesions of cervix (65%) and vulva (10%)
Low-grade squamous intraepithelial lesion:
Low risk of progression to malignancy
Close observation (i.e., cytology and colposcopy every six months)
Topical treatment if persistent
High-grade squamous intraepithelial lesion:
Risk of concurrent invasive squamous cell carcinoma is 10%–28%
Complete surgical excision
Often multifocal
Commonly no gross lesion; less frequently, mucosal irregularities or color changes; acetowhite epithelium, punctation and mosaicism by colposcopy
Exophytic or flat
Low-grade squamous intraepithelial lesion (LSIL, VAIN1)
Koilocytosis in upper layers
Preserved maturation and polarity in lower epithelial layers, no significant atypia
High-grade squamous intraepithelial lesion (HSIL, VAIN2 or 3)
Crowding, loss of organization and polarity and squamous maturation
Significant cytologic atypia (high nuclear-to-cytoplasmic ratio, pleomorphism, coarse chromatin, mitoses) involving lower two-thirds (VAIN2) to full-thickness epithelium (VAIN3)
Negative or patchy p16 stain favors LSIL
p16 overexpression (strong “block” positivity, nuclear and cytoplasmic) favors HSIL
Ki-67 tends to show positive labelling in superficial epithelial layers in HSIL
Reactive inflammatory atypia
Atrophy, including transitional cell metaplasia
Radiation atypia
Micropapillomatosis (vs. low grade squamous intraepithelial lesion)
This tumor represents <2% of all malignant neoplasms of the female genital tract, but accounts for approximately 90% of those arising in the vagina. According to the International Federation of Gynecologists and Obstetrics (FIGO), a tumor should be classified as a vaginal primary only after extension from other genital sites is excluded. In general, if a tumor involves cervix, vulva, or urethra as well as the vagina, it should be considered as a cervical, vulvar, and urethral primary, respectively, until proven otherwise. Risk factors for vaginal squamous cell carcinoma include HPV infection, repetitive trauma (such as occurring with long-standing an untreated prolapse), low socioeconomic status, smoking, previous pelvic radiation therapy or hysterectomy, history of cervical or vaginal squamous intraepithelial lesion, and immunosuppression. Approximately 80% are HPV-related, mainly HPV 16, followed by HPV 18 and HPV 31. The pathogenesis and precursor lesions in the remaining 20% remain obscure.
Vaginal squamous carcinoma is most commonly seen in patients in the sixth and seventh decade but can occur over a wide age range (16 to 95 years). Age-adjusted incidence is 72% higher in black compared to white women. They most commonly present with vaginal bleeding, followed by vaginal discharge or pain, urinary symptoms, and dyspareunia. Some are asymptomatic and the tumor is detected by routine Papanicolaou smear or physical examination.
Invasive squamous cell carcinomas typically involve the posterior aspect of the upper third of the vagina. Tumors vary in size (ranging from few millimeters to >10 cm) and can be exophytic, plaque-like or ulcerative and may show deep infiltration of the vaginal wall.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here