Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Like the skin and gastrointestinal (GI) tract, the lung is a mucosal organ with a large surface area exposed to the external environment. Unlike the skin and GI tract, the lung is considered to be largely sterile below the glottis, whereas the skin and GI tract are colonized with bacteria termed commensal flora. Despite the lower airway being sterile, the upper airway becomes rapidly colonized with bacteria that can be aspirated into the lower airway; thus the lung has evolved an array of host defense mechanisms to prevent development of infection in the air space. This robust development of pulmonary host defense mechanisms was an essential step in the evolution of air-breathing animals. The major physiologic aspect of the lung is to perform gas exchange—namely the exchange of oxygen and carbon dioxide across the alveolar capillary membrane. To maintain this function, the lungs must have buffering capacity in the airway and alveolar space to neutralize potentially injurious agents including pathogens. In a 3.5-kg neonate with a minute ventilation ranging from 100 to 150 mL/(kg/min), the lungs are required to filter approximately 30 L of inhaled air hourly. This is a problematic task in that the alveolar surface area requiring protection is 20 times the average neonatal body surface area. In addition to normal tidal breathing or gas exchange, the lung must be able to handle larger insults because of what may occur upon aspiration of oropharyngeal or gastric contents.
Available pulmonary host defenses can be broadly categorized as either structural or immunologic. Examples of structural defenses include the larynx and epiglottis (which are anatomically situated to minimize aspiration of oropharyngeal material), airway angulation, mucus secretion, and mucociliary clearance mechanisms, including the cough reflex. These mechanisms result in progressive filtering of approximately 99% of inhaled particles as they pass through the conducting airways so that overall level of antigen exposure at a given site is inversely related to its depth within the respiratory tree.
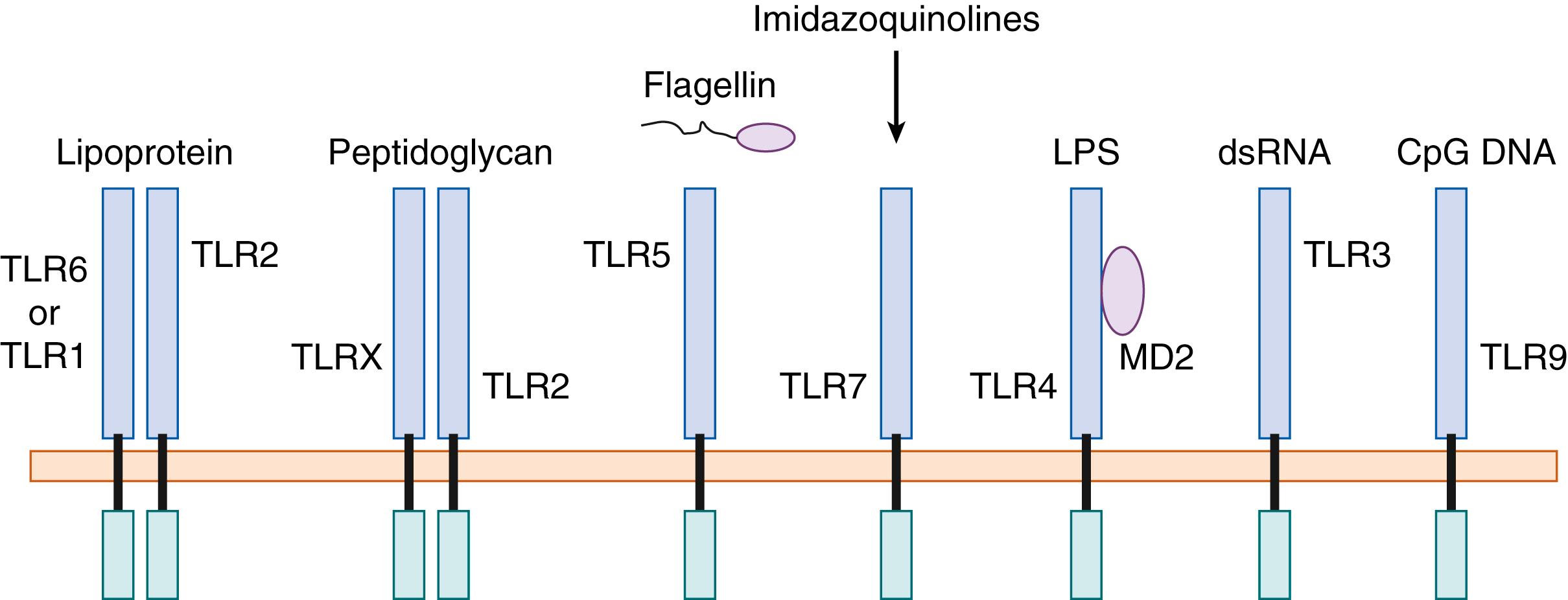
Immunologic mechanisms can be divided into innate immune response and adaptive immune response. Innate immunity is highly conserved from lower-order species such as worms (Caenorhabditis elegans) and fruit flies (Drosophila melanogaster) . Innate immunity is rapid (within minutes to hours) and generally lacks specificity toward the pathogen. Adaptive immunity takes longer to develop (days as opposed to minutes to hours), is more pathogen specific, and is characterized by recombination of cell surface receptors to achieve pathogen specificity in both B-lymphocytes and T-lymphocytes. Adaptive immunity is present in higher-order eukaryotes such as fish and mammals. Although innate immune responses are thought to be nonspecific, they often rely on host recognition of pathogen-associated molecular patterns (PAMPs) or specific molecules such as peptidoglycans, lipopeptides, lipopolysaccharides (LPSs), flagellin, fungal glucans, or specific nucleic acid structures such as single-stranded RNA or unmethylated CpG DNA ( Fig. 123.1 ). These receptors are expressed on both blood-derived cells such as lung dendritic cells (DCs) and alveolar macrophages and on nonmyeloid cells such as the lung epithelial cell. , Ligation of Toll-like receptors (TLRs) can initiate early alarm cytokines such as tumor necrosis factor (TNF)-α and interleukin (IL)-1β in the lung, and these can, in turn, stimulate lung endothelial expression of adhesion molecules, which augments binding of inflammatory cells to endothelium. Additionally, TLR signaling and the alarm cytokines can amplify the production of specific chemokines such as C3a, CXCL1, CXCL2, and CXCL8, which can augment neutrophil recruitment into the air space. Mice deficient in CXCR2, which is the receptor for CXCL1, CXCL2, and CXCL5 in the mouse, have significantly attenuated neutrophil recruitment in response to bacteria and hence have markedly reduced survival as a result of an inability to control bacterial growth in the lung.
The lung is unique among mucosal organs in that it expresses surfactant proteins (SPs). Although surfactant was originally described as the critical phospholipid component of the alveolar lining fluid that reduces surface tension and allows successful transition from liquid breathing in the fetus to air breathing in the neonate, surfactant also plays critical roles in innate immunity. Specifically, the SPs A and D have collagen stalks with lectin-binding domains termed collections . SP-A and SP-D can act as opsonins and have been shown to be critical for host defense against bacterial, fungal, and viral pathogens. , These proteins can interact with carbohydrates on pathogens to directly neutralize the pathogen or augment macrophage-mediated uptake of these pathogens. Macrophages express a variety of phagocytic receptors to ingest and kill pathogens including Dectin-1, macrophage mannose receptors, and scavenger receptors. Immature dendritic cells (iDCs) are also capable of ingesting pathogens-antigens, and when activated, iDCs can become mature DCs that express high levels of class II major histocompatibility complex (MHC) for antigen presentation and costimulatory molecules such as CD80 and CD86. In addition, maturation leads to up-regulation of CCR7, a G-coupled chemokine receptor that is critical for migration of DCs to lymphoid tissue for antigen presentation to CD4 + T cells. Furthermore, it has been shown that cytokines, specifically IL-12p40, are required for DC migration to lymph nodes, possibly through regulation of CCR7. It is partly through these mechanisms that innate immunity can markedly drive adaptive immunity. For example, antigen presentation to CD4 + T cells in the absence of costimulation (via CD80 or CD86) can lead to anergic T cell responses that may be a key mechanism of achieving antigen tolerance in the lung. This is important because the delicate lining of the lung cannot afford to have strong immune reactions to all inhaled particles (such as ubiquitous mold spores) because the inflammation could adversely affect gas exchange. Thus, the lung comprises macrophages and DCs, which likely respond to specific thresholds of stimulus that are important in regulating decision points of antigen-specific tolerance versus antigen-specific immunity.
In addition to macrophages, DCs, and epithelial cells, the lung also contains cells that are capable of bridging immunity. These cells include γδ T cells and natural killer (NK) T cells that often respond to canonical antigens (and cytokines). Thus, these cells can secrete cytokines that control mucosal immunity, but undergo limited T cell receptor (TCR) rearrangement compared with classic αβ T cells, which orchestrate more specific adaptive immunity. In addition a new class of cells have been characterized—innate lymphoid cells (ILCs) that derive from lymphoid progenitors but do not express TCRs. These cells can differentiate into lineages that secrete effector cytokines including interferon (IFN)-γ, IL-5, IL-13, IL-17, and IL-22 analogous to T helper 1 (Th1), Th2, and Th17 cells among the αβ T cell lineage. The recruitment of αβ T cells and B cells heralds the onset of the adaptive immune response. These cells express T cell and B cell receptors that undergo genetic reengagement so that the receptor has high affinity for peptides that are antigen specific. These cells consist of an effector population and a memory population. The latter population is capable of responding much more rapidly than naïve cells if the antigen is reencountered by the host. Adaptive immunity thus initiates a targeted response aimed at containment and clearance of a specific antigen, allowing titration of nonspecific—and potentially host-injurious—alveolar inflammation. Although it is convenient to think of innate and adaptive immunity as innate immunity occurring proximal to adaptive immunity, complex pulmonary immune responses, as seen in pneumonia, require interplay between innate and adaptive elements.
Structural defense exists throughout the respiratory tract. During air entry, the nose performs humidification of entrained air and also serves as an important filter. Particle filtration occurs through nasal hairs and through nasal turbinates. The turbulent airflow that exists in the upper airway facilitates particle deposition in the upper airway. These structures can filter particles as small as 10 μm. The next barrier to protect the lower airway is the larynx, which consists of the epiglottis, aryepiglottic folds, and glottis. Innervation of these structures provides a gag and cough reflux, which minimizes oropharyngeal aspiration. Particles smaller than 10 μm can be inhaled into the lower respiratory tract, and particle deposition is greatest at areas of airway bifurcation. An important clearance mechanism in the lower airways is cough and mucociliary clearance, which is coordinated by specialized epithelial cells.
Airway epithelial cells consist of both ciliated and non-ciliated cells. The cells in the large airways exist as a pseudostratified epithelium with each cell having contact with the basement membrane.These cells express apical-tight junctions that restrict passive diffusion or pathogen movement across the lateral intracellular space, augmenting local mechanical barriers. The cilia extend apically from the epithelium into the airway surface liquid (ASL), which has been estimated to be 7 to 8 μm in height. On top of this liquid layer there is a mucous layer, which is the site of particle deposition. The height of the ASL can markedly affect mucociliary clearance and is regulated by both sodium and chloride transport across the epithelium. Excluding regions of the larynx and pharynx where squamous epithelium predominates, ciliated epithelium is present from the upper respiratory tract to the level of the respiratory bronchioles. In addition to the ciliated epithelium, there are a variety of different non-ciliated cell types including mucus-producing goblet cells, serous cells, club cells, neuroendocrine cells, and basal cells. , Ciliated cells are in physical contact at tight junction desmosomes and in physiologic communication via gap junctions. Columnar ciliated cells may carry up to 200 cilia, ranging from 4 μm in the distal airways to 6 μm centrally. Ciliogenesis commences in the upper trachea early in gestation (week 7) and proceeds distally; by week 24 of gestation, the fetal airway epithelium resembles that of the mature trachea. Although fetal cilia are motile, the function of ciliary activity in utero is unknown.
Epithelial cell types responsible for mucus production include the goblet cells, serous cells, and club cells. Goblet cells are found predominantly in large airways and are the principal source of mucus. Club cells are found only in small airways and produce watery secretions; serous cells have similar location and function but have been identified only in fetal tissues. Club cells also serve as a likely stem cell for regeneration of ciliated epithelium. , A novel population of lineage-negative epithelial stem/progenitor cells has been found to repopulate the epithelium after influenza or bleomycin lung injury. These cells require NOTCH signaling that acts through a splice variant of p63 that regulates cell proliferation. Submucosal glands located in the cartilaginous portion of the airways also contribute to overall mucus secretion and express high levels of the chloride transporter cystic fibrosis (CF) transmembrane conductance regulator (CFTR). Recently, studies using single cell RNAseq have shown that CFTR expression is concentrated in specialized secretory cells termed ionocytes . ,
There is hierarchy of cell populations when traveling from the large airways to the alveolar ducts. In the trachea and large airways, ciliated columnar epithelium forms an essentially continuous epithelium, with a ratio of ciliated cells to goblet cells of 5:1. In the lower airways, ciliated and goblet cell numbers are reduced, a ciliated cuboidal epithelium predominates, and club cells become the only secretory cells present. Single cell technology has identified novel cells in the airway and will likely greatly inform lung repair in response to injury.
As alluded to previously, particle deposition occurs in the mucus layer and the apical situated glycocalyx layer, which consists of mucins tethered to the epithelial cell surface. The epithelium expresses both tethered and nontethered mucins. MUC1 , MUC4, and MUC16 are genes that encode tethered mucins, which are highly glycosylated and extend up to 1500 nm into the airway lumen. These mucins and other glycoproteins in the glycocalyx can bind particles and bacteria, facilitate clearance, and form an anatomic barrier between the particle and the epithelial cell. The glycocalyx has also been shown to be a critical barrier to prevent infection of the epithelium by various respiratory viruses.
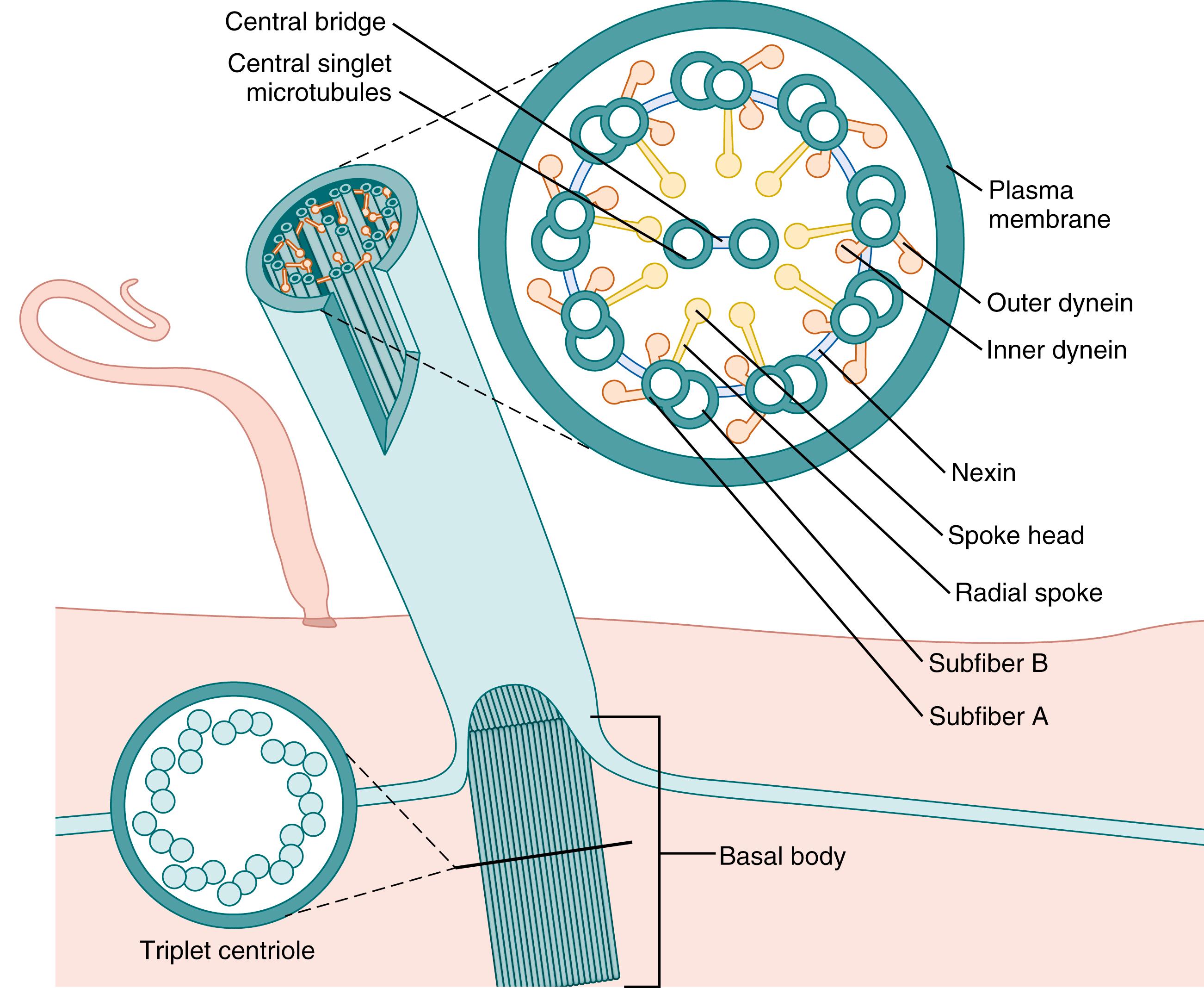
Human cilia are composed of nine doublet microtubules (subfibers) surrounding two microtubules. The major microtubular axonemal proteins are dynein, adenosine triphosphatase (ATPase), and tubulin. At the tip of the cilium, the nine subfibers simplify into nine single fibers that insert into a common cytoplasmic extension ( Fig. 123.2 ) through which they mechanically engage the overlying mucus sheet during the effective ciliary stroke. At the base of the cilium, the nine subfibers end in the basal body, which is anchored to the cytoskeleton. Because all basal bodies of a cell are oriented in approximately the same direction, the effective strokes of all cilia of a given cell have a similar orientation; however, neither the orientation of these structures nor the orientation of the ciliary beats is necessarily identical in adjacent cells. , During ciliary motion, dynein projections from one subfiber transiently interact with the non-dynein-containing subfiber of an adjacent microtubule doublet and, using energy from dynein-mediated adenosine triphosphate (ATP) hydrolysis, induce a conformational change resulting in subfiber movement. Repetition of this process in adjacent doublets, in a unidirectional front circumferentially, causes the sequential movement of fibers that affect cilia motion. From a resting state, a cilium in its recovery stroke swings close to the cell 180 degrees backward, then fully extends and moves through its effective stroke, an arc of approximately 110 degrees in a plane perpendicular to the cell surface. During the effective stroke, the ciliary tip engages the overlying mucus, advancing it in the same direction. Following this, the cilium rests and then repeats this sequence. As a cilium swings backward into its recovery stroke, it engages other resting cilia, stimulating them to begin a recovery stroke; this mechanical recruitment is pivotal for the coordinated beating of airway cilia.
Cilia of human nasal, tracheal, and bronchial mucosa beat at 11 to 15 Hz at body temperature, with progressively slower frequencies noted in proximal bronchi and bronchioles. Because the combined surface areas of the distal airways are exponentially greater than those of the central airways, this differential ciliary beat frequency allows efficient handling of the relatively large mucus loads eventually delivered to the trachea. Endogenous mechanisms that allow such local ciliary beat modulation have been described. Local physiologic loads to airway epithelium, such as increased quantities of mucus, can mechanically stimulate increased ciliary beating in vivo; this effect appears to be mediated by increased cytosolic calcium and can be reproduced pharmacologically by agents that modulate intracellular calcium levels. , Ciliary beat frequency is also exquisitely sensitive to alterations in temperature; cilia of the small airways beat optimally near body temperature, decreasing and increasing their beat frequencies in response to decreased and increased body temperatures, respectively. Increased ciliary beat frequency in response to increased ambient air concentrations of nitric oxide (NO) has been described, suggesting that local cellular production of this bioactive substance may modulate ciliary function. These observations are consistent with in vitro data demonstrating that ciliated epithelium produce NO, which regulates ciliary beat frequency in an autocrine manner via a cyclic guanosine monophosphate signaling pathway. In addition to the dynein ATPase, a cyclic adenosine monophosphate (cAMP)-dependent kinase also facilitates control of ciliary beating. Whether intrinsic neural control of ciliary beat frequency exists is unclear. Although acetylcholine increases ciliary beat frequency in vitro, suggesting a potential role for cholinergic regulation of ciliary tone, there is no cholinergic efferent innervation of the superficial airway epithelium, making it unlikely that neural mechanisms regulate lung mucus transport. Finally, recent interest has focused on autocrine and paracrine airway epithelial signals generated by local purinergic pathways. , In this model, luminal ATP and uridine triphosphate (UTP) induce increased ciliary beat frequency by binding to G protein-coupled purinoreceptors on the epithelial apical membrane. Nucleotide-hydrolyzing enzymes of the airway surface liberate adenosine, which acts through a separate receptor to sustain the ciliostimulatory effects of ATP, while cilia-derived phosphatases hydrolyze ATP and UTP, down-regulating ciliary beat frequency. Nucleotide release by airway epithelia is induced by shear stress and possibly other stimuli so that local mechanical or metabolic perturbations may modulate ciliary activity.
Ciliary function may also be affected by a variety of exogenous substances introduced into the airway. Inhaled β-adrenergic agonists may increase ciliary beat frequency by increasing cellular cAMP. Inhaled NO, via metabolism to S-nitrosothiols, may increase ciliary motility. Conversely, ciliary activity may be diminished by a number of anesthetic gases or by exposure to high concentrations of inspired oxygen or ethanol exposure. , Finally, ciliary function may be impaired by infection. Specific pathogens, including Pseudomonas aeruginosa, Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, and Chlamydia pneumoniae, produce soluble products inhibiting ciliary function. These products may induce ciliary beat slowing, ciliary beat disorientation, ciliostasis, or frank ciliary lysis. Some of these substances are directly ciliotoxic, whereas others act by inducing local macrophages to generate hydrogen peroxide, which has a local cilioinhibitory effect. Lipid-derived inflammatory mediators, such as platelet-activating factor (PAF), induce dose-dependent slowing of ciliary beat, whereas proteins released into the airway lumen during inflammation, such as leukocyte elastase and neutral protease, are also ciliotoxic. Although other inflammatory mediators stimulate ciliary beating in vitro, overall mucociliary function is typically diminished during inflammation in vivo.
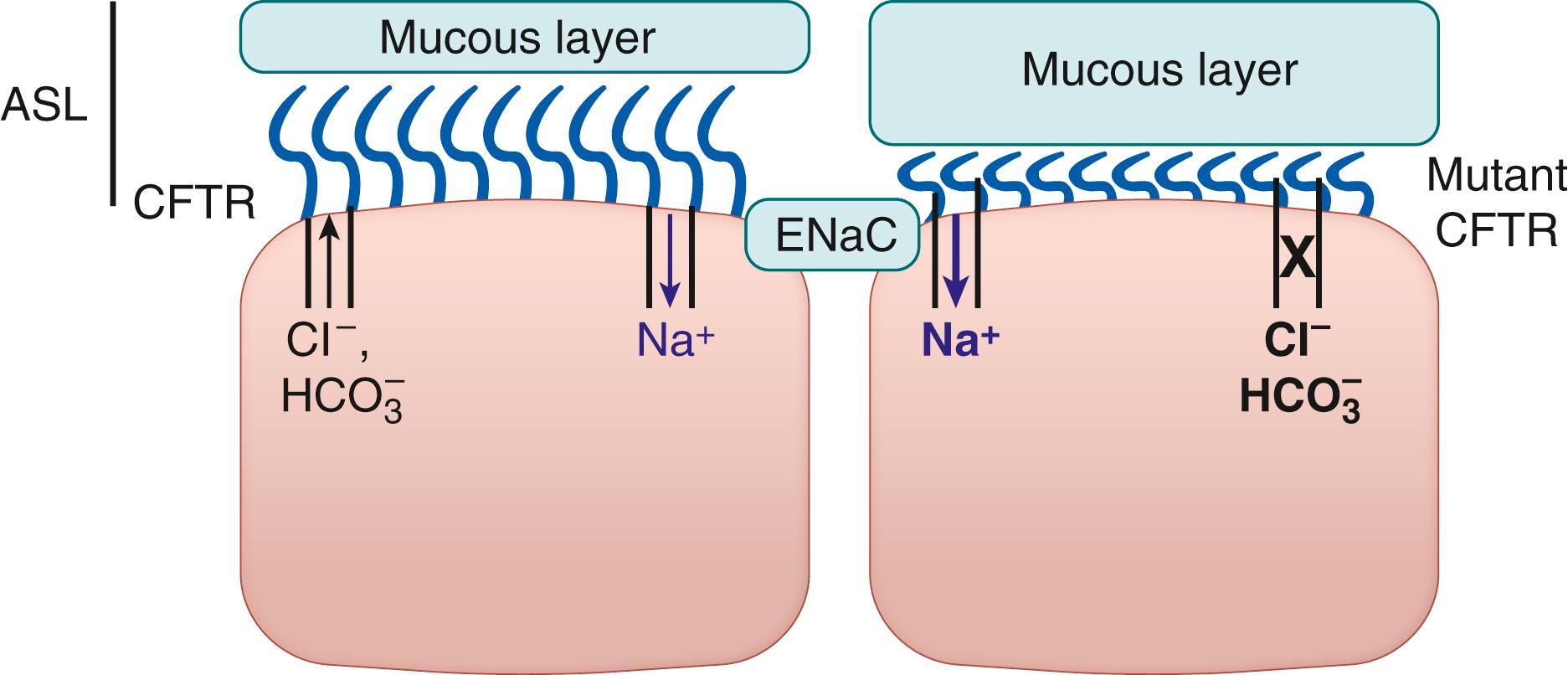
ASL is a thin, nonviscous secretion lying just between the epithelial cell and overlying mucus, bathing the basal portion of the cilia and providing an environment of low resistance for the cilia to move during the backstroke portion of the movement cycle. The level of the ASL is critical for effective mucociliary function. If the fluid level is too high, the ciliary tips will not be able to engage the overlying mucus and effect its movement. If the fluid level is too low, as occurs in CF, the cilia will not be able to disengage from the mucus layer during the recovery stroke and ciliary beating will be impeded. ,
As mentioned, ASL is regulated by active ion transport across the epithelial cells with concomitant fluid movement that is either passive or aquaporin regulated. , The bulk of fluid transport is regulated by both sodium and chloride transport. The predominant apical sodium channel is the epithelial sodium channel (ENaC), and chloride conductance is regulated by the CFTR and calcium-activated chloride channels ( Fig. 123.3 ). These channels are subject to precise regulation by environmental stress such as particle deposition or infection. ENaC is regulated by proteases, as proteolytic cleavage of ENaC subunits can markedly augment channel activity. , CFTR is regulated by cAMP, and thus this channel is subject to influences such as osmotic stress or cytokine stimulation that influence cAMP levels. In addition to these sodium and chloride channels, there are bicarbonate exchangers that regulate ASL pH. Large-animal models of CF have also revealed that CFTR itself also regulates ASL pH and the more acidic pH in CFTR mutant tracheas reduces antimicrobial activity of the ASL. Passive efflux of water across the apical epithelial membrane results in cell shrinkage, triggering release of epithelial-derived mediators, including NO; these mediators increase blood flow and water content of the submucosa. Movement of water from the submucosa across the basolateral epithelial membrane, possibly regulated by aquaporin 4, restores epithelial cell volume. In contrast, fetal lung fluid results from active secretion of Cl − by all respiratory tract epithelia, with passive cation and fluid transit into the airway lumen. In the distal airways these mechanisms persist, providing a source of periciliary fluid and mucus hydration for the rest of the lung. Conversely, tracheobronchial epithelium gradually transitions postnatally from Cl − secretion to Na + absorption, and Na + absorption eventually predominates in the larger airways under basal conditions. At the same time, production of mucus components transiently increases. Mucociliary clearance is reduced in neonates, presumably the result of increased ASL secretion and impaired ciliary tip engagement of mucus. It has also been shown that the reduced ASL in CF results in enhanced mucous adherence and reduced detachment, which would impair mucous transport.
Mucins are high-molecular-weight, heavily glycosylated proteins that contribute to the gel-like qualities of mucus and are critical for mucosal host defense. Multiple mucin genes are expressed in the airways, but the primary gene products in mucus are MUC5AC and MUC5B. Mucins are formed in the Golgi apparatus, concentrated in vesicles, and released by exocytosis from goblet cells and mucus cells of submucosal glands. Once secreted, condensed mucin polymers are hydrated, increasing their volume exponentially. , Mucin proteins typically exhibit several hundred sugar side chains that contribute to their structural and barrier functions. As a result of their extensive glycosylation and their long carbohydrate side chains, mucins are capable of binding virtually any inhaled particle they encounter, facilitating particle entrapment within the mucus layer. Both MUC5AC and MUC5B show extensive regulation by both Th2 cytokines, including IL-9 and IL-13, and Th17 cytokines, namely by IL-17. Additionally, proinflammatory molecules such as histamine, prostaglandins, leukotrienes (LTs), platelet-activating factor (PAF), and TNF-α can regulate mucin expression.
Mucus also contains proteoglycans, other proteins, lipids, water, and DNA. DNA is found in significant concentrations only during infection or inflammation of the airways originating from dead leukocytes or denuded epithelium; large amounts of DNA markedly increase mucus viscosity. , DNA is an important component of neutrophil extracellular traps (NETs), which consist of products of degranulated neutrophils such as granular proteases and antimicrobial peptides. NETs have been shown to serve as traps for bacteria and possibly as a way to concentrate antimicrobial peptides at the host pathogen interface. Other antimicrobial proteins, including lysozyme, lactoferrin, human β defensin-2 (HB-2), and immunoglobulin A (IgA), are secreted into the ASL-mucus layer. Mucus rheology is determined by mucus hydration and by polyionic interactions between mucin molecules. These factors, in turn, depend on the pH and salt content of the ASL, and this may explain the thick, relatively immobile mucus seen with the impaired transepithelial Cl − secretion and accelerated Na + absorption characteristic of CF. ,
Optimal mucociliary function depends on complex interactions among cilia, the mucus layer, and the intervening ASL. Both the mucus layer and the ASL are moved unidirectionally along airway surfaces by ciliary action; cilia effect movement of the mucus layer through direct contact, while frictional interaction with the mucus layer drags periciliary fluid. Beyond their propulsive function, cilia also impart vertical movements within the mucus layer; inhaled particles deposited within the airways are effectively churned into the mucus layer, facilitating binding by mucins and retention within the mucus layer until forced removal by mucociliary transport occurs. Using aerosols of technetium-labeled albumin, one can measure mucociliary clearance in humans. Mucociliary transport has been estimated to be 4 to 5 mm/min in the trachea, decreasing in the smaller airways to less than 0.4 mm/min in the bronchioles. Overall mucociliary clearance of the lung is achieved in two phases: (1) an initial rapid phase (half-life of approximately 4 hours) representing mucociliary clearance of the tracheobronchial tree and (2) a simultaneous slow phase lasting weeks to months, which represents alveolar clearance by non-mucociliary transport mechanisms. Humans exhibit a wide range of mucociliary clearance rates, implying some endogenous control of this process. As noted earlier, purinergic regulatory mechanisms have been postulated, given the demonstrated effect of secreted nucleotides on ciliary beat frequency, goblet cell degranulation, and periciliary fluid secretion. Mucociliary function continues to develop postnatally, gradually becoming adult-like over several weeks.
Mucociliary function can be perturbed by alterations in ciliary activity, changes in ASL composition, pH, mucus secretion, or mucociliary interactions. Relevant environmental influences include temperature and humidity. Ciliary beat frequency and mucus transport rates are diminished at conditions below body temperature. Environmental tobacco smoke also reduces mucociliary clearance. High inspired concentrations of oxygen can also damage the respiratory epithelium and impair mucociliary clearance.
Bacterial exotoxins can also perturb mucociliary clearance. Cholinergic agonists increase mucus clearance by increasing rates of mucus secretion and ciliary beat frequency, whereas atropine decreases mucociliary clearance and transport rates. β-Adrenergic agonists increase intracellular cAMP levels, which increase ciliary beating ion and fluid secretion and mucus elaboration, resulting in the expected increase in mucociliary transport rates. , Methylated xanthines also enhance mucociliary clearance, presumably through similar actions on epithelial cell cAMP levels. Hypertonic saline has also been shown to enhance mucociliary clearance in patients with CF.
The critical role of cilia in mucosal host defense in humans has been clearly demonstrated by disorders that disrupt ciliogenesis or result in impaired ciliary function. These patients often lose sterility of the lower respiratory tract and suffer from sinusitis, bronchitis, and ultimately bronchiectasis. Primary ciliary dyskinesia (PCD) is a group of genetic disorders that result in a congenital ciliary dysmotility state. At least 30 disease-causing mutations in different genes have been reported to date. , Some mutations result in an absence of an intermediate-chain dynein, which is important in assembly and coordination of heavy-chain dyneins of the ciliary shaft. A subgroup of PCD is manifested by the triad of sinusitis, bronchiectasis, and situs inversus and is termed Kartagener syndrome. Other structural defects such as abnormal cilia length and orientation have been described in association with bronchiectasis and recurrent pulmonary infection. There is an ongoing effort to establish a clearer phenotype of these patients to allow better gene association studies to advance the gene-based diagnosis of these disorders. In addition to congenital disorders, many respiratory infections including both viral and bacterial infections can impair ciliary function. It is important to note that PCD can present as respiratory distress in the newborn period. Adenovirus infection, particularly serotype 7, has been shown to cause marked damage to lung epithelium resulting in impaired ciliary function and the development of bronchiectasis. As a result of marked decrease in blood flow to the damaged lung, the patient may develop a hyperlucent lung, as described by Swyer and James.
Another important cause of acquired ciliary dysfunction is the use of positive pressure ventilation in the neonate. Ventilator-associated lung injury and bronchopulmonary dysplasia (BPD) can impair mucociliary clearance. The airway epithelium is exquisitely sensitive to mechanical injury, and manipulations such as endotracheal intubation and/or the use of suction catheters have been shown to cause flattening or denuding of the epithelium in concert with a local inflammatory response. Prolonged mechanical ventilation has been shown to result in squamous metaplasia of the respiratory epithelium. Additionally, BPD is associated with bronchomalacia, which may further impair regional mucociliary clearance.
Shared upper pathways for breathing and swallowing require that these functions be closely coordinated to prevent pulmonary contamination with oropharyngeal contents. In the neonate, multiple protective processes functionally separate the respiratory and alimentary tracts during swallowing. The more cranial position of the larynx provides closer approximation of the epiglottis and soft palate, better isolating the oral cavity from the rest of the upper airway. Because newborns have lower resistance across the nasal passage than across the oral passage, owing to deficient control of oropharyngeal musculature, nasal breathing is favored, especially by preterm newborns; this may also facilitate functional separation between the upper tracts. Finally, it is well documented that neonatal breathing is interrupted by airway closure during nutritive sucking.
Swallowing occurs early in fetal life, and three distinct stages have been identified: oral, pharyngeal, and esophageal. In neonates, the oral stage is coincident with nutritive sucking. During the pharyngeal stage, the bolus moves through the pharynx into the esophagus; the larynx is elevated and pulled forward; the epiglottis covers the laryngeal opening, which is further sealed by contraction of the laryngeal adductors; and inhibition of breathing occurs. At the end of the swallow, the airway reopens, and the esophageal phase follows. This transient apneic response is also seen in nonfeeding swallows, which allow the infant to clear the airway of oral secretions or regurgitated materials before resuming breathing. , Premature infants typically exhibit incomplete integration of swallowing and breathing functions, such that oral feeding may result in pronounced apneic pauses.
When studied, intact cough reflexes were found in only 50% of term infants and only 25% of preterm infants; therefore, when challenged by a swallowing misadventure, neonates are more likely to defend the airway by sustained laryngeal closure than by coughing. Reflex laryngeal closure is mediated by stimulation of receptors in the laryngeal mucosa innervated by branches of the superior laryngeal nerves. Although potentially pathologic, this response is also adaptive because attempts to breathe against an obstructed airway are reduced. Conversely, failure of laryngeal closure and premature termination of the apnea before airway clearance has occurred may result in aspiration. As maturation occurs, coughing replaces apnea as the primary response to stimulation of these receptors.
In addition to mucociliary transport, cough is an important mechanism to accelerate the transport of inhaled or aspirated particulates out of the lung. The accessory muscles of expiration are used for coughing and sneezing. Contraction of the internal intercostal muscles decreases the anteroposterior diameter of the thorax, aiding in expiration. The abdominal muscles aid in forceful expiration (such as coughing) by increasing intraabdominal pressure; the increased pressure is transmitted through the diaphragm to the pleural space. To move the mucus in the direction of the large airways, the shear force generated by the airflow must overcome mucus viscosity and gravitational forces. At high airflow velocities (2500 cm/s), mucus is rendered off the surface as droplets, producing the mist flow characteristic of sputum expectoration from the trachea; such airflow velocities can be reached in the small airways during cough or forced exhalation.
For a cough maneuver, rapid inhalation of a supranormal is followed by tidal volume glottal closure, an intrathoracic pressure increase (50 to 100 mm Hg), and glottal opening with rapid exhalation. Although the cough reflex is quite effective in older children and adults, the cough is not as effective in neonates. This is the result of the markedly enhanced compliance of the chest wall and cartilaginous airways that impairs the ability to transfer pleural pressure to transpulmonary pressure. In addition, as the airways are more compliant, the neonate is subject to more airway collapse during the cough reflex. Coughing is also less effective in settings of respiratory muscle weakness or inability to close the glottis (as when endotracheally intubated). A coordinated cough maneuver relies on local chemoreceptors and mechanoreceptors, vagal afferents, signal integration in the dorsal medulla, and efferent innervation to relevant muscles of inspiration and expiration. The receptors inducing cough are poorly characterized but may be activated by local mediators, including histamine, tachykinins, and substance P. Cough can also be induced by stimulation of other vagally innervated sites such as the external auditory canal or esophagus. The afferent limb involves the vagus nerve and vagally innervated structures such as the larynx and conducting airways. Of these, the larynx and upper airways seem more sensitive to mechanical stimulation, whereas the lower airways are more chemosensitive. Vagal afferents from these sites synapse in the nucleus tractus solitarius of the dorsal medulla, the putative cough center. Efferent pathways include the recurrent laryngeal nerve, which stimulates glottal closure, and spinal nerves from C3 to S2, which innervate intercostal, abdominal, and pelvic muscles required to achieve sufficient tidal volume and expiratory pressure. As noted earlier, the cough reflex of premature neonates tends to be immature or absent, which is attributed to incomplete myelination of vagal afferents.
In the absence of effective cough, additional airway protective reflexes exist. Mechanical irritation of the epipharynx via the glossopharyngeal nerve elicits the snifflike aspiration reflex by which foreign particles can be removed from the back of the nose and then swallowed or expelled by mucociliary clearance. Mechanical stimulation of the vocal folds by means of the superior laryngeal nerve elicits a brief expiratory effort without preceding inspiration (the expiration reflex).
Despite barriers to microbial colonization and invasion discussed earlier, particles of 2 to 10 μm in diameter may still infiltrate the lower airways and alveoli. Furthermore, anatomic barriers may be inadequate in situations of overwhelming pathogen inoculum via the airstream or ineffective in the situation of lung microbial invasion through hematogenous routes. Immune-protective mechanisms are therefore frequently employed to contain penetrant microorganisms. Such mechanisms may be broadly characterized as either innate or adaptive. Adaptive immunity relies on specialized antigen-presenting cells to activate T cells and B cells, resulting in clonal expansion of lymphocyte pools unique for a specific antigen. Although advantageous for their specificity and capacity for long-term memory, such responses are also delayed, owing to the multiple cellular interactions required. This is especially true in the setting of an immunologically naïve host such as the newborn. Because delay in this setting may be deleterious to survival, the capacity for a more immediate immune response must also exist. The soluble and cellular components of this immediate host response constitute innate immunity.
Innate immunity is phylogenetically primitive, nonspecific, immediate, and the primary antimicrobial defense of the naïve host. Innate immune responses recognize and target structurally conserved molecular sequences shared among groups of pathogens; these include LPS of gram-negative bacteria, lipoteichoic acid of gram-positive bacteria, bacterial lipoproteins or peptidoglycans, mycobacterial glycolipids, fungal mannans or β-glucans, unmethylated bacterial DNA sequences, and double- or single-stranded viral RNAs. The structures may vary subtly from one organism to another, but the essential elements are conserved, forming the template for what is referred to collectively as pathogen-associated molecular patterns . In addition to patterns generated as the result of invading organisms, the innate immune system also recognizes molecular patterns released by cells undergoing necrotic death. These molecules are referred to as damage-associated molecular patterns (DAMPs) and include different families of proteins and nonproteinaceous substances such as uric acid microcrystals. Both PAMPs and DAMPs are recognized and ligated by pattern recognition receptors (PRRs) of the innate immune system. PRRs are nonclonal and do not depend on immunologic memory because they are germline encoded. These receptors are expressed on barrier and effector cells—such as epithelial cells, endothelium, and phagocytes—of innate immunity where binding and activation induce either direct phagocytosis or cellular signals, culminating in leukocyte recruitment and nonspecific inflammation. Alternatively, PRRs are also components of soluble or secreted humoral proteins. When present in the airway lining fluid, they constitute an additional chemical barrier and complement mucociliary clearance. ,
As noted earlier, bacterial clearance from peripheral airways by mucus transport may require up to 6 hours; because bacteria can exhibit doubling times of less than 20 minutes, forced mucociliary clearance alone is potentially inadequate to maintain alveolar and airway sterility. Therefore, concurrent mechanisms to contain bacterial growth must be present. Products of the neonatal lung that confer innate, or nonspecific, antimicrobial protection include complement, other opsonins such as fibronectin, antimicrobial peptides (defensins, cathelicidins), lysozyme, collectins, and NO, though evidence shows these mechanisms do not all function at adult levels in early life, leaving the infant airway susceptible to more severe infections. As cells are continuously regenerating, the identification and removal of dying cells, either self or nonself, is a function duplicated throughout immunity. Included in this group are soluble innate immune pattern-recognition proteins, which identify nonself and altered-self molecular patterns and include such proteins as collectins, ficolins, and pentraxins.
The complement system is essential for innate and acquired immune responses. Deficiencies in complement proteins may result in greater susceptibility to infections and/or to the development of autoimmune diseases. As a sentinel limb of innate immunity, it can be directly activated by component recognition of PAMPs. As such, it is a potentially important neonatal host defense mechanism providing direct bacterial lysis in the absence of optimal cellular immune responses. Specific complement components also function as microbial opsonins to facilitate phagocytosis, and as chemotaxins to facilitate granulocyte recruitment. The complement system consists of more than 20 proteins synthesized by cells of the liver or the reticuloendothelial system. Once activated, most components exhibit a proteolytic function responsible for activation of subsequent components in orderly series. Although normally quiescent, circulating and local complement components may be activated by any one of three major pathways.
The classic complement pathway is initiated by the binding of C1q to the Fc portion of either IgG or IgM complexed to antigen. This results in an amplified cascade leading sequentially to activation of C4b2a (C3 convertase), generation of C3a and C3b, and formation of the C4b2a3b complex that cleaves C5 into its split components C5a and C5b. The mannose-binding lectin (MBL) pathway is mediated by MBL, an acute phase protein of the collectin family structurally similar to C1q. MBL possesses domains that recognize and bind membrane glycoproteins of bacteria, yeast, mycobacteria, and certain viruses. , Pathogen binding induces an MBL conformational change, exposing two MBL serine proteases that activate C4, ultimately generating classic C3 convertase. The alternative pathway is initiated by a number of substances, including endotoxin, complex polysaccharides, immune complexes, and surface components of intact cells such as certain bacteria and fungi. Binding of nascent C3b fragments to these substances protects C3b from inactivation by serum factors H and I. Subsequent cleavage and binding of factor B and the stabilizing protein properdin yield C3bBb, alternative pathway C3/C5 convertase, which enzymatically cleaves C5 into the active components C5a and C5b. Each pathway ultimately activates terminal components of the complement system to form C5b-9, which inserts into lipid bilayers to form a transmembrane pore, permitting bidirectional solute flow and ultimately cell wall lysis.
Complement is an essential part of the immune system, but its lack of full functionality in newborns may contribute to the increased risk for severe infections among neonates and unfortunately is not compensated for by a mature adaptive immune system. , Advances in technology have allowed for premature infants surviving birth at earlier gestational ages than ever before. However, we are only beginning to understand the functional capacity of these infants’ immune systems. A study examining the complement system at different gestational ages revealed functional impairment in the classic pathway as measured by CH50 in premature infants, with levels increasing in term infants. Specific components of the classic pathway, including C8 and C9, have shown marked deficiencies, and they are linked with poor killing of gram-negative bacteria in vitro. , Poor crosslinking of C3 may also contribute to decreased lytic and opsonic activity. , Grumach and colleagues showed that the alternative pathway, as measured by properdin, was lower at birth, reaching only 25% of adult levels in preterm and term infants compared with adults. Finally, whereas MBL serum levels of term neonates approach those of adults, values in preterm neonates are approximately 60% of levels in term infants; the absence of increased morbidity or infection suggests only an adjunctive role for the MBL pathway in this population. Taken together, preterm neonates have more consistent impairment of classic and alternative pathways, which improves steadily postnatally and reaches adult levels by 12 to 18 months of age; in contrast, MBL appears ontologically conserved. , , , ,
Aside from MBL, ficolins and collectins are also involved in lectin pathway activation. , Among these, L-ficolin is a serum lectin, which stands out as a ficolin with the greatest capacity for antimicrobial activity. It recognizes and binds various microorganisms, including gram-negative and gram-positive bacteria, DNA, and 1, 3-β-glucans, as well as apoptotic cells. , It is postulated that L-ficolin may confer protection from microorganisms that exacerbate allergic inflammation in the lung, whereas deficiency of L-ficolin may contribute to enhanced susceptibility to respiratory infections. Recent findings revealed that acute-phase pentraxins, including C-reactive protein, serum-amyloid P, and long pentraxin 3, which are capable of selectively opsonizing bacteria, fungi, and viruses, are involved in complement activation and regulation. , Among these, the antibody-like features of long pentraxin 3 (PTX3) enable interaction with MBL, resulting in communication with C1q to boost complement activation. In addition to enhancing activation, PTX3 is able to bind the main fluid-phase regulator of the classical and lectin pathways, C4BP, to avoid overwhelming activation.
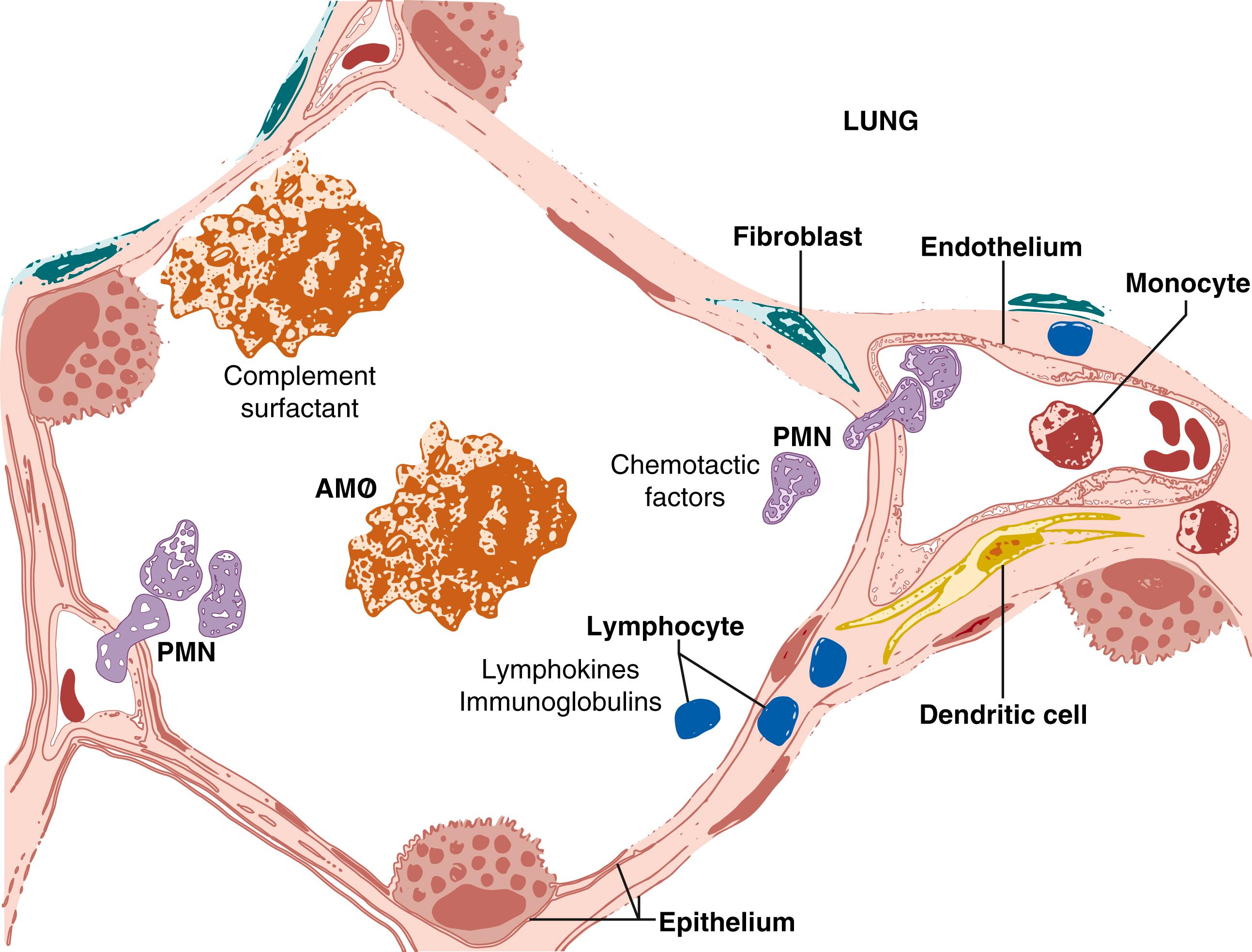
Complement components are found throughout the lower respiratory tract and are produced locally by alveolar macrophages, pulmonary fibroblasts, and type II epithelial cells ( Fig. 123.4 ). In this milieu, complement activation can be initiated by PAMPs or in the immune host by microbial binding to IgM or IgG. Each pathway results in binding of component C3b, which is recognized by specific receptors on neutrophils and macrophages, facilitating phagocytosis. C3a and C5a are potent neutrophil chemoattractants, whereas C5b initiates the membrane attack complex effecting direct, non-leukocyte-mediated bacterial killing. Data from experimental animal models of acquired and inherited hypocomplementemia indicate that complement is critical in clearance of S. pneumoniae and P. aeruginosa .
While deficiencies among individual components of the complement system may fail to effectively defend the infant airway against foreign pathogens, overproduction of activated complement fragments have been implicated in the pathogenesis of asthma. , Asthma is a chronic inflammatory disease of the bronchi caused by inappropriate immunologic responses to common antigens in genetically predisposed individuals. Asthma is typically characterized by T H 2-skewed inflammation with elevated pulmonary levels of IL-4, IL-5, and IL-13 levels. The discovery of IL-17 in the lungs of asthmatic persons has led to important new research linking IL-17 with airway constriction and neutrophil recruitment associated with asthma pathology. Both T H 2 CD4 T cells and IL-17-producing Th17 cells engage C3 or C5 complement components, resulting in the induction of airway hyperresponsiveness.
Fibronectins are extracellular matrix glycoproteins capable of interacting with a number of macromolecules and cells bearing specific fibronectin receptors. The ability of specific mesenchymal cells such as fibroblasts to elaborate fibronectin during embryogenesis is critical to thoracic development. After birth, basal expression of fibronectin is limited primarily to hepatocytes, which produce circulatory fibronectin, and to the respiratory tract, where fibronectin is present in saliva produced by bronchoepithelial cells and constitutively secreted by alveolar macrophages. Serum concentrations of fibronectin are diminished in neonates (particularly in preterm infants), whereas bronchoalveolar lavage (BAL) levels appear inducible in settings of lung injury. Enhanced fibronectin production by pulmonary fibroblasts, alveolar macrophages, and epithelial cells is induced by local production of macrophage-derived cytokines associated with acute inflammation, TNF-α, IL-1β, transforming growth factor-β (TGF-β), and platelet-derived growth factor. In acute lung injury, fibronectin stimulates fibroblast and epithelial cell recruitment and endothelial cell proliferation to facilitate tissue reparative processes. However, the ability of fibronectin to bind certain bacteria and to augment leukocyte adherence and migration suggests an additional role for this molecule in lung antimicrobial defense.
Fibronectin is bound by a number of pathogenic bacteria ( Staphylococcus aureus, Streptococcus pyogenes, Escherichia coli, and P. aeruginosa ) as well as Mycobacterium species, Pneumocystis, and fungi. Because fibronectin binds multiple microorganisms, it was originally thought to promote phagocytosis and destruction of the invasive organism before the onset of a specific immune response; studies demonstrating increased neutrophil and macrophage binding of S. aureus supported this theory. Opposing studies suggested that fibronectin by itself may possess only weak opsonic activity. , More recent data indicate that fibronectin-binding proteins (FnBPs) present on the surface of S. aureus and streptococcal organisms promote adhesion of the bacteria to host tissue, leading to increased colonization and infection. This would be particularly problematic in cases of impaired mucociliary clearance or epithelial cell damage, yielding a partial explanation of pulmonary microbial tropism in these settings. In vitro studies have demonstrated that S. aureus can be internalized by a variety of nonphagocytic cells including epithelial and endothelial cells, fibroblasts, osteoblasts, keratinocytes, and kidney cells. Furthermore, recent studies have shed light on a newly discovered mode of internalization through FnBPs, which may avoid fusion with the degrading lysosomes of phagocytic cells. In the normal lung, the most important host defense role of fibronectin may be to facilitate binding of, and local colonization by, nonpathogenic organisms. New information is needed to better understand the role of fibronectin in pulmonary tropism and infection, particularly as it pertains to the newborns who possess one-third to one-half the level of fibronectin found in adults.
The availability of iron in the host environment and its effect on bacterial growth is one of the best studied aspects in pathogenicity. , Iron is an essential element for bacterial growth and survival; thus, pathogens have evolved various ways to compete for the host’s iron. In response, host defenses have developed several mechanisms to restrict bacterial colonization or invasion by sequestering elemental iron either in cells or complexed to transport proteins.
There are currently five known iron-binding proteins that have been described in human innate immunity: lipocalin, hepcidin, natural resistance-associated macrophage protein (Nramp), the transferrin family of proteins (lactoferrin and transferrin), and ferritin (cytosolic and plasma). Siderophilins are glycoproteins, made up of lactoferrin and transferrin, that are increasingly identified as playing important roles in the regulation of infectious diseases. Transferrin transports iron between cells and is the predominant human siderophilin found in plasma and lymphatic fluids. Transferrin is also found in BAL fluid in concentrations between 1 and 2 times greater than those in matched serum. Transferrin iron saturation is similar in healthy adults and children at approximately 33%, although in times of iron depletion or anemia, transferrin saturation may drop below 10%.
In contrast to transferrin, lactoferrin is the predominant iron-binding protein of airway secretions and is rarely present in deep alveolar lavage unless inflammation is actively occurring; it is also stored in neutrophil granules in addition to its secretion on mucosal surfaces. It binds with high affinity to lipid A and may play an antimicrobial role by depriving invading microorganisms of iron. , Similar to transferrin, lactoferrin transports extracellular iron between cells with high affinity, but unlike transferrin, lactoferrin is usually less than 10% iron saturated.
Iron-binding proteins effectively complex free iron available in mucosal secretions and alveolar lining fluid, thereby limiting the growth of most iron-dependent pathogens; notable exceptions include Moraxella and Neisseria species, which are able to obtain iron from these proteins. In addition to iron binding, human lactoferrin has other antimicrobial activity against specific bacteria, including E. coli, S. pneumoniae, and Legionella pneumophilia. , Lactoferrin binds to LPS, disrupting gram-negative bacterial membranes, and this effect may be synergistic with the effects of other soluble components of the mucociliary layer such as lysozyme. Lactoferrin also demonstrates antiviral activity, binding to human immunodeficiency virus and cytomegalovirus (CMV), preventing their uptake by host cells. Cleavage of lactoferrin by either proteases or pepsin yields a small cationic peptide, lactoferricin, with structure and antimicrobial activity similar to those of the defensins. Finally, recent work suggests a unique role for lactoferrin in prevention of bacterial biofilms. Biofilm formation is a growth mode specialized for long-term bacterial colonization of surfaces, as is seen in chronic Pseudomonas infection; once established, organisms within biofilms are notoriously resistant to host eradication. By chelating iron, lactoferrin stimulates twitching, a pili-mediated bacterial motility that deters biofilm formation. Once a biofilm has been established, however, sensitivity to this lactoferrin effect is lost. However, recent evidence shows that US Food and Drug Administration–approved iron chelators given in combination with aminoglycosides such as tobramycin dramatically reduce P. aeruginosa biofilm formation on CF airway epithelial cells. For reasons that are largely unknown, the iron concentration in the ASL of CF patients is 400-fold greater than in non-CF patients, making iron chelation a viable and important therapeutic target. ,
Beyond these antimicrobial effects, lactoferrin also plays a role in the modulation of local immune responses. As a component of neutrophil secondary granules, lactoferrin is delivered to sites of inflammation. Here, lactoferrin binds LPS, effectively competing with LPS-binding protein (LBP) and minimizing endotoxin presentation to immune cells. Similarly, lactoferrin also recognizes and binds recurrent motifs of bacterial DNA, potentially dampening the broad proinflammatory immune responses that would ordinarily be triggered. Teleologically, this may allow lactoferrin to limit excess immunostimulatory activity at mucosal surfaces with microbial exposure. Most recently, human recombinant lactoferrin was shown to induce human DC maturation via TLRs 2 and 4, suggesting that endogenous lactoferrin may also regulate similar aspects of innate immunity.
In addition to the siderophilins, lactoferrin and transferrin, recent studies have provided insight into the antimicrobial roles of lipocalin, hepcidin, and Nramp. Using a mouse model, host lipocalin has been shown to bind bacterial siderophores, thereby preventing iron acquisition by invading pathogens. , The human analogue of lipocalins, siderocalin demonstrates a dramatic up-regulation following bacterial colonization with S. pneumoniae to potentially bacteriostatic levels, strongly indicating its role as a host defense mechanism in the upper respiratory tract.
Hepcidin, first discovered by Park and colleagues, is a key regulator of iron homeostasis as well as an acute-phase reactant with a critical role in inflammation. It contributes to host defense by blocking the microorganism’s access to iron. Originally, only hepatocytes were thought to produce this iron regulatory protein; however, recent evidence has shown that alveolar macrophages produce hepcidin in addition to expressing the iron importer divalent metal transport and iron exporter ferroportin1 (FPN1) proteins. Further studies suggest that upon exposure to LPS, iron mobilization by alveolar macrophages is reduced and is mediated by hepcidin-induced degradation of the FPN1; as such, less iron becomes less available to the pathogen. This mature iron regulatory system, however, maneuvers its iron stores primarily based on localization of the invading pathogen. In the case of extracellular bacteria, hepcidin targets FPN1 on the cell surface, resulting in its degradation and subsequently reducing macrophage iron release.IFNγ produced during an inflammatory state also inhibits FPN1 through its support of hepcidin production. Iron availability is then reduced for extracellular bacteria, while intracellular iron is incorporated into ferritin. In the event of intracellular bacterial infections, iron stores are shifted out of the cytoplasm and phagolysosome through hepcidin-mediated increases in FPN1 as well as Nramp.
More than 30 years ago, Nramp was discovered to possess antimicrobial properties. It is now widely accepted that the expression of Nramp1 (also called Slc11a1 ) confers innate immune defense against certain bacterial infections. It is thought to work by sequestering iron from bacteria within the phagosome or through a reaction in which iron catalyzes the production of toxic hydroxyl radicals. Nramp1 has further been shown to play a role in early macrophage activation, and its expression is up-regulated by IFN-γ, LPS, and granulocyte–colony-stimulating factor (G-CSF). ,
One form of host defense, found in both plants and animals and therefore predating the separation of the plant and animal lineages, is the production of antimicrobial peptides. These endogenous peptides complement the activity of the larger opsonizing or nutrient-binding proteins in maintaining airway sterility ( Table 123.1 ). They act by disrupting cell membranes of a wide range of pathogens including bacteria, viruses, and fungi; each peptide manifests a broad but fixed spectrum of activity, underscoring the need for multiple peptide classes within the airway lining fluid. Within the respiratory tree they are either produced by epithelial cells (where their expression is both constitutive and inducible) or delivered to vulnerable loci by circulating leukocytes. Apart from their direct antimicrobial activity, which is nearly immediate in onset, these peptides can also activate cellular immunity, amplifying host response as necessary. The major human antimicrobial peptides are lysozyme, cathelicidins, and the defensins.
| Product | Relative Concentration | Source |
|---|---|---|
| SLPI | μg/mL | Epithelia, Paneth cells, macrophages |
| Lactoferrin | μg/mL | Epithelia, Paneth cells, neutrophils |
| SP-A, SP-D | ng-μg/mL | Epithelia, type II pneumocyte |
| α-Defensins | ng-mg/mL | Paneth cells, neutrophils |
| β-Defensins | ng-mg/mL | Epithelia, neutrophils, glands |
| Reg3γ/Reg3 β | ng-mg/mL | Paneth cells |
| Lipocalin-2 | ng/mL | Epithelia, neutrophils |
| CCL20 | ng/mL | Epithelia, neutrophils, macrophages |
| PGLYRP-1 | μg-mg/mL | Neutrophils, M cells |
| PGLYRP-3, PGLYRP-4 | μg/mL | Epithelia, glands |
| Cathelicidins (LL37) | μg/mL | Epithelia, neutrophils |
Defensins are small (3 to 6 kDa, 29 to 40 amino acids) cationic peptides containing six conserved cysteine residues. They are divided into α and β subclasses on the basis of their secondary structure, but their gene locations imply a common evolutionary origin. Structurally, they share a β-sheet conformation that spatially segregates their cationic and hydrophobic amino acid clusters into an amphipathic motif. When secreted, defensins are driven into anionic phospholipid bilayer membranes by electromotive forces where they multimerize into channels, disrupt normal membrane function, and induce cell lysis. , Although host cells are potential bystander targets, their lower anionic lipid content and the presence of cholesterol as a membrane stabilizer imbue significant protection. , Apart from their structural differences, the α and β defensins differ in their sites of expression and roles in airway defense.
The human α-defensins constitute a subclass of six members: four human neutrophil peptides (HNP-1 through HNP-4) and two human defensins (HD-5 and HD-6). HD-5 and HD-6 are secreted by Paneth cells of the small intestine and epithelia of the female urogenital tract and are presumed to attenuate local commensal burden; respiratory epithelium is not a source of α-defensins. , HNPs 1 through 4 are abundant (up to 50% of total protein) in primary granules of neutrophils, where they assist in nonoxidative killing, and are also found in NK cells, monocytes, and lymphocytes. , Individual α-defensins have unique spectra of antibacterial activity against gram-positive and gram-negative species, as well as activity against enveloped viruses (including Herpes species) and against Candida . , , The α-defensins also exhibit both pro- and antiinflammatory activities. As discussed later, they are chemotactic and induce chemotaxins for a variety of immune cells. They also bind to serine protease inhibitors, amplifying polymorphonuclear neutrophil (PMN)–derived elastase activity. Conversely, they can inhibit complement activation by binding to C1q and participate in local wound repair by stimulating epithelial cell proliferation. , Extracellular α-defensins are scavenged by α2-macroglobulin, which minimizes cytotoxicity to host cells and down-regulates defensin concentration at inflammatory sites. Immunohistochemical analysis has demonstrated HNPs on bronchial epithelial surfaces and in mucinous exudate in the air spaces, presumably derived from PMN granule release within the airway. In adults, α-defensins have been found in BAL fluid of patients with pneumonitis, correlating with chemotaxin concentration and PMN counts.
Unlike the α-defensins, the β-defensins are produced by airway epithelium. This subclass contains four identified human β-defensins (HBD-1 through HBD-4), although more than 20 genes are postulated to exist. As a group, these peptides demonstrate antimicrobial activity against several gram-positive and gram-negative organisms, as well as Candida and Aspergillus species; however, differences in antimicrobial spectra exist between individual peptides. , Histologically, β-defensins are expressed in the epithelia of airways and lung and in the serous cells of submucosal glands. , HBD-1 is found in the BAL specimens of healthy adults; its expression in the airways appears to be constitutive and noninducible. In contrast, the remaining β-defensins are all inducible, with HBD-2 the best characterized. Endotoxin, Pseudomonas, and the cytokines TNF-α and IL-1β each induce HBD-2 expression, and this induction may be amplified further by concurrent alveolar macrophage stimulation. Apart from this interaction with alveolar macrophages, HBDs further interface with cellular immunity by functioning as chemoattractants. HBD-1 and HBD-2 are each chemotactic for iDCs, as well as memory T cells by binding to the chemokine receptor CCR6. Sustained β-defensin induction by noncontained microbial stimuli may thus invoke cellular and adaptive immune responses. Tracheal aspirates of term and preterm newborns demonstrate similar levels of HBD-2, with increased levels seen in local and systemic infections. These data imply that β-defensin responses are intact even in preterm infants and that neonates may up-regulate some facets of pulmonary innate immunity in the context of a systemic inflammatory response. More recent information confirms that HBD-2 is the predominant β-defensin in human neonatal lung; however, its abundance in neonatal tracheal aspirates increases as a function of gestational age. Compared with HBD-2, HBD-1 had a lower level of expression, and HBD-3 expression was absent in neonatal airway epithelial cultures. Although no direct correlations have been made, it is likely that the lower levels of HBD-2 in infants may contribute to the increased susceptibility of premature infants to pulmonary infections. More recently, plasma levels of HBD2 have been studied for their potential as a prognostic biomarker for patients with community-acquired pneumonia, whereby lower HBD2 plasma levels on admission predicts worse outcomes in adults. Based on studies showing that HBD increases as a function of age, combined with more recent data demonstrating increased HBDs in neonatal tracheal aspirates during infection, it is postulated that low levels of HBD during infection may contribute to severity of disease and worse outcomes. , ,
Cathelicidins are a diverse family of vertebrate antimicrobial proteins found in leukocytes and on epithelial surfaces where they function like defensins. They are produced as preproproteins, stored as inactive proforms, and require enzymatic cleavage for bioactivity. The sole known human cathelicidin is hCAP-18, which requires proteolytic activation by proteinase 3 to liberate the antibacterial peptide LL-37. LL-37 is a 37-amino acid molecule whose amphiphilic α-helical structure facilitates affinity to and disruption of bacterial membranes. Human LL-37 displays a range of antimicrobial activities. It is a broad-spectrum antimicrobial with effects against Actinobacillus, E. coli, P. aeruginosa, Enterococcus faecalis, and S. aureus, and it demonstrates synergy with the defensins. Though typically considered to have antibacterial activity, LL-37 was recently shown to have activity against respiratory syncytial virus (RSV) in vitro, a virus that typically infects all children by the age of 2 years. LL-37 prevented RSV-induced cell death of epithelial cultures and inhibited the production of new infectious particles. LL-37 also directly binds endotoxin and is chemotactic for eosinophils, neutrophils, monocytes, and T lymphocytes. LL-37 is found in primary granules of neutrophils and has also been shown in NK cells, lymphocytes, and monocytes. Expression of LL-37 in the lung is seen in cells of the submucosal glands and surface epithelia of the proximal airway, where its elaboration can be induced by up to 50-fold in states of inflammation. IFN-γ has been shown to induce LL-37 release, but it concurrently down-regulates gene transcription, perhaps balancing antimicrobial effects against host cytotoxicity. At high concentrations, LL-37 can manifest cytotoxicity toward eukaryotic cells, and hosts have scavenging mechanisms, as exist for the defensins. Comparable levels of LL-37 are found in the tracheal aspirates of term and preterm newborns, with increased levels seen in local and systemic infections. A recent study demonstrated that LL-37 is present in the airway secretions of newborns, but there was no association between concentration and gestational age. A more in-depth look at the structure and function of LL-37 can be found in the detailed review by Wang and colleagues.
Lysozyme is a 14-kDa cationic enzyme that hydrolyzes glycosidic bonds of bacterial cell wall peptidoglycan. This peptide is found in the granules of neutrophils and mononuclear phagocytes and is also secreted by airway epithelial cells of the pulmonary tract where it confers nonspecific antimicrobial protection. Lysozyme is highly active against many streptococci, but resistance to its enzymatic activity is common among other gram-positive organisms and nearly universal among gram-negative organisms. This is likely caused by variable accessibility of vulnerable glycosidic bonds within the cell wall matrix with the outer membrane of gram-negative bacteria providing an additional barrier to the penetration of lysozyme. However, in the presence of other membrane-targeting substances such as complement or hydrogen peroxide, lysozyme enhances the destruction of E. coli and other gram-negative bacteria. Lysozyme is also capable of direct antimicrobial activity toward Streptococcus sanguinis and Streptococcus faecalis species by virtue of its cationic properties and possesses fungicidal activity against Candida albicans by targeting the glycosidic bonds of fungal chitin. Although lysozyme may appear redundant in the presence of other antimicrobial peptides, emerging data suggest otherwise. In a transgenic murine model of lysozyme overexpression, increased resistance to pulmonary infection from either P. aeruginosa or group B Streptococcus (GBS) was observed. Furthermore, lysozyme exhibits important antimicrobial synergy with HBD-2, LL-37, and lactoferrin. More recently, immunodepletion studies have suggested that lysozyme is a major antibacterial component secreted by submucosal glands within the tracheobronchial airways. Moreover, several studies have examined lysozyme’s potential as an exogenously delivered biotherapeutic. Bhavsar and colleagues administered aerosolized recombinant hamster lysozyme to hamsters infected with pulmonary P. aeruginosa. Following aerosolized delivery for 2 hours on 3 consecutive days, the bacterial burden in lung homogenate and bronchoalveolar lavage fluid (BALF) was reduced.
Similar to other antimicrobial peptides, short palate, lung, nasal epithelium clone 1 (SPLUNC1) has demonstrated antimicrobial activity against P. aeruginosa, S aureus, M. pneumonia, and K. pneumonia. , SPLUNC1 is also considered to have antibiofilm activity that functions to reduce of the surface tension by regulating the ASL volume. SPLUNC1 is expressed in serous cells within the airway and has bactericidal/permeability increasing protein (BPI)-like activity to mediate gram-negative bacteria endotoxin LPS-induced bacterial killing. , Similar to BPI, SPLUNC1 can also bind LPS and is thought to scavenge LPS to minimize its inflammatory properties.
LBP is a soluble 60-kDa glycoprotein that recognizes and binds the lipid A moiety of LPS, enhancing host immune response to endotoxin. LBP is homologous to other phospholipid transport proteins and functions as a transport protein that disaggregates soluble LPS and presents it to targets on cellular membranes. Membrane-bound CD14 is a PRR for LPS; however, it does not contain a cytoplasmic domain and cannot transduce activating signals across the cell membrane. Instead CD14 complexes with TLR4 to form the cellular PRR for LPS, with TLR4 acting as the transmembrane signal-transducing portion of the receptor. LPS-induced signaling through the CD14/TLR4 complex, expressed on inflammatory cells, is distinctly enhanced by the presence of LBP, resulting in the production of early response cytokines TNF-α and IL-1β. , LBP is produced primarily in the liver as an acute-phase protein, and its plasma concentration increases exponentially during acute inflammatory responses. LBP is also a normal constituent of lung fluid, with alveolar concentrations estimated at 1 μg/mL; these concentrations also increase exponentially with pulmonary inflammation, likely owing to capillary leak of plasma LBP and enhanced local generation. The relevance of LBP to pulmonary host defense is suggested by murine transgenic models of LBP deficiency, which exhibit blunted alveolar bacterial clearance with increased bacteremia and lethality in response to pneumonia. Human alveolar type II epithelial cells demonstrate capability ex vivo to up-regulate LPB production in response to mediators (TNF-α, IL-1β, IL-6) that similarly induce hepatic acute-phase production of LBP. Additionally, animal models suggest that, in the neonate, alveolar macrophages may be a concurrent source of LBP in the lung. Although elevated serum levels of LBP have been reported in neonatal sepsis, pulmonary LBP expression in response to respiratory infection remains uncertain in this population. The most recent studies of infant LBP suggest its use as a viable diagnostic tool for neonatal bacterial infections.
Pulmonary surfactant is a bioactive material that bathes the alveolar surfaces and keeps alveoli from collapsing during expiration by reducing surface tension at the air-liquid interface. It is a mixture of lipids and proteins, whereby dipalmitoylphosphatidylcholine (DPCC) functions as the primary lipid for lowering surface tension. The four known SPs are SP-A, SP-B, SP-C, and SP-D. Together, they have several important functions including regulation of surfactant lipid metabolism, lipid membrane organization, and pulmonary host defense. As with the lipid components of pulmonary surfactant, SP-B and SP-C are extremely hydrophobic and function primarily to reduce surface tension and maintain pulmonary homeostasis after birth. The role of pulmonary host defense rests with SP-A and SP-D, which along with mannan-binding lectin, make up a family of carbohydrate-binding proteins known as collagenous C-type lectins or collectins . These proteins are characterized by a discrete, four-domain primary structure consisting of a cysteine-containing amino terminus, a subsequent collagen-like region, a coiled neck region, and a carboxyl terminus carbohydrate recognition domain (CRD). Collectins function as soluble scavenger receptors, interacting through their lectin CRDs with microbial carbohydrate and glycolipid PAMPs to enhance phagocytosis and pathogen clearance; through this mechanism, collectins exhibit activity against a broad range of bacterial, viral, and fungal pathogens. Beyond these opsonizing qualities, SP-A and SP-D each exerts specific immunomodulatory effects that titrate the magnitude of inflammation and influence pulmonary immune responses. ,
SP-A and SP-D share many characteristics related to their synthesis and bioactivity. Both collectins are produced by type II alveolar epithelium and club cells and are secreted into the alveoli and distal airways. Production and secretion of both proteins increase dramatically during the third trimester of fetal lung development and appear to be further inducible in utero in response to dexamethasone; both proteins are also up-regulated in response to acute lung injury or epithelial activation by microbial products such as LPS.The pulmonary collectins directly interact with a variety of microorganisms. Both SP-A and SP-D bind with broad specificity to bacteria including Klebsiella pneumoniae, P. aeruginosa, H. influenza, S. pneumoniae, S. aureus, E. coli, M. tuberculosis, and M. avium. Pathogen encounter with lung collectins results in agglutination and/or opsonization. Agglutination impedes microbial invasion and colonization and facilitates clearance by the mucociliary escalator, whereas agglutination of viruses enhances their internalization by neutrophils. Alternatively, SP-A or SP-D may act as opsonins by bridging between PAMPs on the microbial surface and collectin receptors on phagocytes. The pulmonary collectins also enhance specific leukocyte functions. Both SP-A and SP-D are chemotactic for neutrophils and macrophages, although SP-D is more potent in this regard. SP-A and SP-D both enhance alveolar macrophage phagocytic function and oxyradical production. Induction of this latter effect requires the collectin CRD(s) to concurrently engage ligand; this presumably minimizes spurious up-regulation of potentially injurious mediators. Finally, although earlier studies suggested a direct inhibition of T cell proliferation by SP-A and SP-D, recent evidence demonstrates that this inhibition may be a result of the presence of TGF-β in SP preparations. Although the relationship between SP-A and TGF-β has not been fully described, it is postulated that SP-A acts as a storage site for latent TGF-β in the lung, thereby indirectly participating in the control of inflammation. Recent evidence indicates that SP-A functions in a more purposeful manner to maintain homeostasis in the airway through TGF-β–mediated induction of regulatory T cells (Tregs). Work by d’Alessio and colleagues recently reported that Tregs are important in the recovery of acute lung injury via TGF-β, a cytokine known to induce Treg function. Mukherjee and colleagues showed that SP-A-/- mice have impaired expression of Foxp3 Treg cells ex vivo compared with wild-type mice, which could be fully restored with the addition of exogenous SP-A. Despite their many shared functions, SP-A and SP-D exhibit several biochemical differences that result in distinctive, unshared activities in vivo. Relevant differences include solubility, CRD specificity, length of collagen domain, and affinity for available collectin receptors.
Approximately 30% of the pulmonary collectin pool is made up of SP-D, the product of a single gene. SP-D exists primarily in a cruciform structure: four homotrimeric subunits radiating from a disulfide-linked hub. Unlike SP-A, it is relatively impervious to proteolytic or elastase degradation. Its up-regulation secondary to LPS-induced cytokines confirms its role in innate host defense. SP-D binds specifically to carbohydrates containing glucopyranosides, resulting in affinity for the core oligosaccharides of LPS, the mannose-rich oligosaccharides of influenza A hemagglutinin, and fungal cell wall glycoconjugates of Candida and Pneumocystis carinii. SP-D binds to the putative collectin opsonin receptor, gp-340, a macrophage scavenger receptor, and CD14 via interactions between the CRD and the N-linked oligosaccharides on CD14; SP-D inhibits the interactions between CD14 and LPS. , Attempts to further clarify the role of SP-D in host defense have led to the development of transgenic murine models of SP-D deficiency. Such mice exhibit a phenotype of pulmonary alveolar proteinosis, with foamy activated macrophages, hypertrophy of alveolar type II cells, and increased inducible inflammatory responses. SP-D-deficient mice show impaired functions of host defense against H. influenzae, GBS, influenza type A virus, and RSV, but lack of SP-D does not affect newborn survival from infection. A recent study by Kotecha and colleagues, conducted in premature and newborn infants, demonstrated sizeable and functionally relevant variation in the expression of SP-D between preterm and term newborn lung secretions. Moreover, the percent of neonatal SP-D capable of binding zymosan rarely surpassed 50% in BALF samples and was 3.5 times lower in preterm infants than in term infants on the first day of life.
In contrast, approximately 70% of the pulmonary collectin pool is made up of SP-A, the product of two genes, SP-A1 and SP-A2, each producing different chain types. The SP-A subunit can therefore exist as a homotrimer or heterotrimer, introducing heterogeneity to this protein. Differential tissue expression has been reported, with SP-A1 expressed in the lower respiratory tract and SP-A2 expressed in the tracheal and bronchial epithelium and submucosal glands. Its production is up-regulated by IFN-γ and other LPS-induced cytokines. Its short collagen domain and preferred hexameric structure result in a “flower bouquet” pattern, and this clustering of CRDs influences ligand selectivity. SP-A binds specifically to carbohydrates including fungal wall glycoconjugates and some capsular polysaccharides. It also binds a variety of lipids including the lipid A moiety of LPS. Leukocyte receptors for SP-A include the C1q receptor, SPR210 (the 210-kDa receptor specific for SP-A), the gp-340 receptor, and CD14. Multiple studies suggest that SP-A influences LPS-CD14 binding; however, reports disagree on whether SP-A promotes or inhibits this interaction. , , SP-A–deficient mice exhibit increased susceptibility to many pathogens including GBS, H. influenza, RSV, P. aeruginosa, and Pneumocystis jirovecii. ,
SP-A exhibits a variety of immunoregulatory activities within the alveolus. It suppresses IFN-γ, an activator of leukocyte and macrophage inflammatory activity and an essential mediator for transition to a lymphocyte-mediated adaptive immune response. SP-A may also dampen LPS-dependent cellular activation by competing with LBP. Taken together with the reported SP-A/TGF-β inhibition of T cell proliferation, these functions suggest that SP-A acts, at least in part, by tempering inflammation that might induce alveolar injury. Such a host-protective role would be consistent with transgenic models of SP-A deficiency, where microbial challenge results in delayed pathogen clearance, increased pathogen dissemination, and enhanced inflammation with increased production of TNF-α, IL-1β, and IL-6. This paradigm, however, is complicated by contradictory data regarding SP-A induction of proinflammatory cytokines and up-regulation of inducible NO synthase (iNOS). These disparate findings are reconciled by recent observations that the response to SP-A is determined by the state of cell activation and concurrent stimuli. Thus SP-A up-regulates iNOS in alveolar macrophages primed by IFN-α and stimulated by LPS, but conversely inhibits LPS-induced iNOS if IFN-γ priming has not occurred. SP-A, therefore, augments an inflammatory response already under way but dampens similar responses evolving de novo. In this context, SP-A induction of iNOS also exerts host protective effects. In a murine model of tuberculosis, exogenous SP-A enhanced pathogen entry into alveolar macrophages by almost five-fold. This enhanced entry resulted from SP-A ligation of the SPR210 receptor with increased endocytosis of the SP-A:BCG complex. Furthermore, SP-A–mediated up-regulation of NO and TNF-α production enhanced mycobacterial killing.
SP-A and SP-D exhibit only partial redundancy of their bacterial specificities, owing to their distinct structures and their differing affinities for specific carbohydrates and lipids. These differences may result in complementary functions that enhance the antimicrobial activity of surfactant in total. One example of such synergy is illustrated by collectin interactions with Klebsiella, a pulmonary pathogen that can reversibly switch between encapsulated and unencapsulated phenotypes. Unencapsulated forms of this organism allow optimal adhesion to the epithelial surface, facilitating colonization; these forms predominate early in infection. As noted earlier, SP-A binds to lipid A of LPS, whereas SP-D preferentially binds to the LPS core sugars. Because lipid A is embedded within the bacterial cell wall and inaccessible to SP-A, SP-D is the primary collectin ligand for LPS expressed on the surface of unencapsulated forms. Encapsulation limits interaction of SP-D with the underlying LPS, but invokes significant binding by SP-A, which recognizes the capsular polysaccharides expressed by this pathogen. In this scenario, SP-A and SP-D thus fulfill distinct but complementary opsonizing roles in the innate host response ( Fig. 123.5 ). Similar complementary function is illustrated by collectin interaction with influenza A virus (IAV). SP-D binds viral envelope glycoproteins (hemagglutinin and neuraminidase) through its CRD and induces massive agglutination of IAV particles; this agglutination is facilitated by higher-order oligomerization, most achievable by SP-D by virtue of its longer collagen domain. Such agglutination generates particle size sufficient for mucociliary clearance and also directly enhances neutrophil uptake and respiratory burst. Alternatively, SP-A activity results from IAV recognition and binding of sialic acid residues on this collectin. SP-A has much less agglutinating capacity but interacts with a broader range of IAV strains including those that are highly resistant to inhibition by SP-D or serum collectins. SP-A forms much smaller aggregates, resulting in less augmented neutrophil uptake but enhanced uptake by alveolar macrophages. As before, the differing collectin structures and binding affinities result in a broader range of antimicrobial activity and immune cell activation, which ultimately prove to be beneficial to the host.
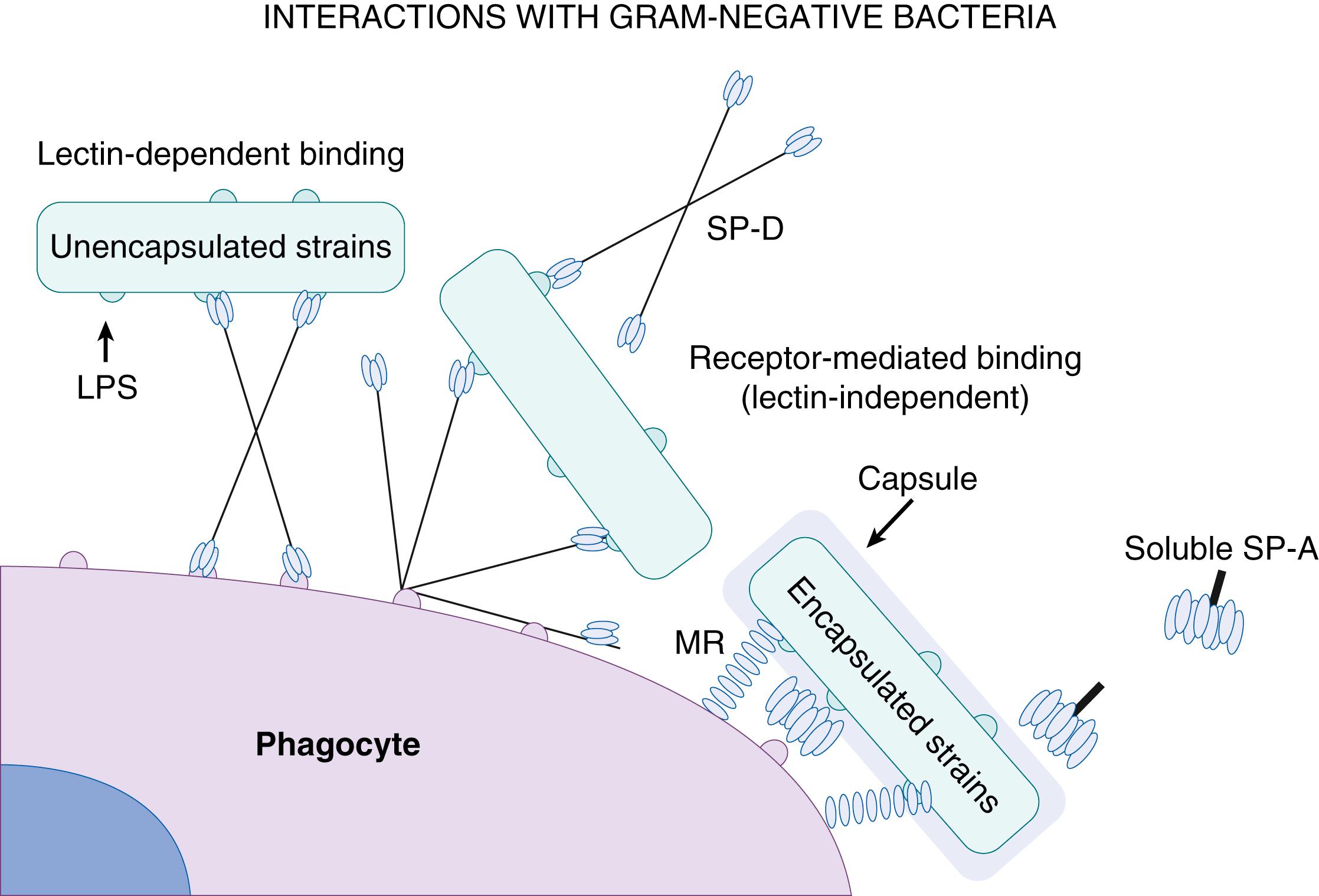
Apart from the specific actions of its collectins, surfactant also exerts a host of immunomodulatory effects within the alveolus. Surfactant enhances phagocytosis by means of a mechanism separate from the actions of SP-A. Interestingly, this prophagocytic effect is more pronounced for resident alveolar macrophages than for recruited peripheral blood monocytes. Whole surfactant reportedly suppresses mononuclear cell oxyradical production by inhibiting the intracellular assembly of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, impairing hydrogen peroxide generation. However, specific lipid components of surfactant may exert different modulatory effects. Therefore, macrophage oxidative burst is blunted by phosphatidylglycerol moieties; however, it is enhanced by phosphatidylcholine components. Enhanced microbicidal function of phagocytes and down-regulation of Fc receptors have each been reported and attributed to the lysophospholipid and free fatty acid components of surfactant. Whole surfactant also modulates phagocyte chemotaxis. Macrophage movement into the alveolus postnatally coincides with increased surfactant synthesis, suggesting a chemotactic effect, which is possibly SP-A mediated. Conversely, DPCC treatment of alveolar macrophages in vitro decreases their migration in response to serum chemotaxins; this is consistent with a teleologically preferred default attenuation of inflammatory response designed to preserve alveolar function. Lastly, surfactant reportedly modulates lymphocyte function as well. Lymphocytes exposed in vitro to surfactant are less responsive to mitogens and exhibit depressed function; under similar conditions, cytotoxic T cells, B cells, and NK cells are all inhibited to various degrees. As discussed earlier, however, some lipid components (DPCC, phosphatidylglycerol) are more suppressive, whereas less abundant components (cholesterol, sphingomyelin) stimulate lymphocyte proliferation. This suggests that conditions that alter these phospholipids ratios may alter adaptive immune responses. Additionally, the differing effects of SP-A and surfactant lipids on lymphocyte proliferation are consistent with the hypothesis that, in some scenarios, surfactant lipids and proteins may be counterregulatory.
In contrast to whole surfactant, conventional surfactant analogues (e.g., beractant, calfactant, poractant) contain neither SP-A nor SP-D.Thus, collectin-mediated immune effects are not provided by exogenous replacement therapies. Moreover, the surfactant replacements are generally immunosuppressive, presumably owing to their nonphysiologic lipid/protein ratios. These products inhibit production of the early-response cytokines TNF-α, IL-1β, and IL-6 by stimulated alveolar macrophages, putatively by depressing activation of nuclear factor kappa B (NF-κB). Similar suppression of fibroblast-derived IL-6 and prostaglandin E2 (PGE2) has also been described, suggesting impairment of those inflammatory responses up-regulated by alveolar cytokine networks. During shorter (10 minutes to 2 hours) exposures, regulation of human macrophage responses by SP-A occurs through reduced kinase activity required for proinflammatory cytokine production. Nguyen and colleagues recently showed that long-term surfactant-mediated suppression of proinflammatory cytokine production in response to TLR 4 activation was regulated by IL-1 receptor-associated kinase M (IRAK-M), a negative regulator of TLR-mediated NF-κB activation. Exposure to beractant, the natural bovine lung extract lacking SP-A, also enhanced IRAK-M expression, but at a lower magnitude and for a shorter duration than SP-A. In response to surfactant, IRAK-M is up-regulated in macrophages thereby suppressing TLR4-mediated TNF-α and IL-6 production in response to LPS. Additionally, beractant has been shown to blunt lymphocyte proliferation, killer cell cytotoxicity, and adhesion molecule expression, possibly through down-regulation of lymphocyte receptors for IL-2. Much of this is in vitro data and must therefore be interpreted cautiously. However, it suggests that available surfactant replacement therapies, although efficacious in normalizing pulmonary compliance, may concomitantly attenuate normal alveolar immune cell responses. For a detailed review of surfactant replacement therapy, including modes of administration and clinical practice standards, refer to the recently published review by Hentschel and colleagues.
NO is a short-lived, oxyradical-related bioactive mediator with potent vasodilatory actions. It mediates and modulates pulmonary transition from fetal to postnatal life and plays a role in both immune regulation and innate host defense. NO is synthesized by three isoforms of NO synthase (NOS-1, -2, and -3), all of which are expressed in the airway epithelium from the bronchus to the distal air space. Thus NO is produced along the entire length of the human airway, and its metabolic product, nitrite, is present in airway-lining fluid at concentrations of approximately 15 μM. NO isoforms exist in either constitutive (NOS-1, NOS-3) or inducible (NOS-2) forms; cells with constitutive NOS include neurons, vascular endothelium, neutrophils, and platelets. Cells with inducible NOS (iNOS, NOS-2) include mononuclear phagocytes, alveolar macrophages, vascular smooth muscle cells, epithelial cells, type II pneumocytes, and hepatocytes. All NOS isoforms are detected early in lung development, and ontogeny shows no significant changes in abundance or distribution with advancing gestational age.
NO exerts potent cytotoxic and inflammatory effects, which support its role as an antimicrobial molecule during host response to infection. NO production from cells containing iNOS is induced by microbial products such as lipoteichoic acid, endotoxin, and bacterial DNA. Locally produced NO inhibits sodium uptake from the apical surface of airway epithelial cells, increasing airway hydration and enhancing mucociliary clearance. Specific NO products such as nitrosylated thiols exert antimicrobial activity by killing the pathogen directly or by inhibiting the pathogens’ replication. NO inhibits the growth of a wide variety of organisms including viruses, bacteria, parasites, and fungi, presumably by targeting microbial DNA and cysteine proteases, which are critical for virulence or replication of these pathogens. NO appears to be particularly important in the innate immune response to intracellular organisms such as Listeria monocytogenes, Salmonella, and M. tuberculosis . NO products also inhibit viral RNA synthesis, inactivate a broad range of microbial proteins by S-nitrosylation, and induce membrane damage through lipid peroxidation. By up-regulating inflammatory cell function; NO augments macrophage motility, up-regulates surface expression of complement and immunoglobulin Fc receptors, and stimulates leukocyte respiratory burst. Concurrent synthesis of NO increases microbicidal activity of the leukocyte respiratory burst by generating additional cytotoxic radicals such as peroxynitrite, which generates potent activity against bacteria and Candida . In vitro, phagocytes demonstrate diminished microbicidal activity after NOS inhibition, and this correlates with in vivo models in which diminished NOS activity impairs microbial clearance.
The role of NO in pulmonary microbial clearance is consistent with recent data from neonates. BAL specimens from preterm (≤32 weeks estimated gestational age) infants exposed to intrauterine infection demonstrated a strong association between inability to express iNOS or up-regulate NO and subsequent development of fulminant pneumonia. Conversely, newborns of similar age and risk who did not develop pneumonia exhibited iNOS up-regulation and increased NO products on BAL analysis, relative to either their pneumonic cohorts or noninfected control subjects. A separate retrospective analysis of lung tissue from neonatal autopsies yielded similar findings; alveolar macrophage-derived iNOS could not be detected in specimens from fulminant pneumonia patients but was demonstrable in control subjects. Taken together, these data suggest that delayed or diminished macrophage-derived NO in the setting of neonatal pulmonary infection correlates with increased morbidity. Etiology of this impaired response is speculative but may result from a paucity of mediators (TNF, IFN-γ) known to up-regulate iNOS expression. Based on the important antimicrobial function of NO, recent studies have evaluated the role of inhaled NO on pulmonary infections in humans. These studies have generated mixed results; however, it is likely that infections caused by intracellular organisms will be more likely to benefit from inhaled NO therapy.
In general, NO exerts antimicrobial effects; however, not all pathogens are inhibited by NO, and in some instances, NO may contribute to injury to the host. In an influenza pneumonia mouse model, targeted deletion of iNOS or treatment with NOS inhibitors led to less severe disease compared with control mice. Similar observations were made in mouse models of M. avium pneumonia and herpes simplex virus encephalitis. , It is postulated that in these disease processes, cytotoxic effects of NO on host cells may contribute to pathogenesis.
Beyond the functions just detailed, NO exhibits additional immunomodulatory activities relevant to pulmonary host defense, which is demonstrated through its up-regulation by immune activating cytokines such as IFN-γ, TNF-α, IL-1, and IL-2. NO has been shown to reduce T helper 1 (Th1) proliferation and IL-2 synthesis while increasing IL-4 synthesis by T helper 2 (Th2) cells. Th1 cells produce IFN-γ, which is an essential cytokine in viral cell–mediated immune responses. Alternatively, Th2 cells selectively produce IL-4 and IL-5 that participate in the development of humoral immunity. NO-induced imbalance in the Th2/Th1 ratio may promote inflammation in allergic diseases like asthma while inhibiting the inflammatory response to viral and bacterial pathogens. RSV is a common pulmonary infection in infants, which has been linked to a large Th2/Th1 cytokine immune response; it has been associated with the pathogenesis of RSV bronchiolitis and the severity of infection in infants. Several studies have associated poor IFN-γ production to greater disease severity and subsequent development of allergic asthma. Although IFN-γ induces NO production, no studies have directly linked NO with RSV disease outcomes. However, a recent study by Gadish and colleagues showed reduced levels of exhaled NO among infants with acute RSV bronchiolitis, possibly secondary to reduced IFN-γ production.
NK cells are specialized cytotoxic lymphocytes and a primary source of IFN-γ within the alveolus; they are normally activated by IL-12. Transgenic iNOS deficiency induces a phenotype of IL-12 deficiency despite normal IL-12 levels. This phenotype is characterized by diminished IFN-γ and increased TGF-β, a cytokine milieu suppressing local macrophage function. Analysis of these data subsequently identified iNOS-derived NO as an essential co-signal for IL-12 signal transduction and activation of NK cells. In this model, the signaling role of NO was therefore critical in maintaining a cytokine microenvironment that allowed normal immune cell function. NO exerts a biphasic effect on NF-κB activity, which is dependent on local NO concentrations. Therefore, NO is able to both up- and down-regulate the expression of a number of inflammatory mediators. In this paradigm, immune activation up-regulates iNOS, generating increased NO. Initial NO activation of NF-κB promotes expression of adhesion molecules and proinflammatory cytokines, facilitating immune cell recruitment. NF-κB up-regulation of iNOS amplifies NO production, eventually generating local NO concentrations sufficient to inhibit NF-κB activity. At this point, both inflammatory cytokine and adhesion molecule expression are down-regulated, effectively dampening the component of inflammation sensitive to modulation by NO. In summary, the putative actions of NO in immune cell signal transduction suggest a sentinel role for this molecule in both the initiation and suppression of cellular immunity. It is reasonable to consider that disruption of NO homeostasis, elicited by a pulmonary-tropic organism such as RSV at a very early age, would break down the barriers against infection and decrease mitigators of inflammation, leading to prolonged infection and increased inflammation.
As with NO, evolving data suggest a potential role for carbon monoxide (CO) in pulmonary host defense. Endogenous CO derives from degradation of heme from molecules such as hemoglobin, myoglobin, and cytochromes by the enzyme heme oxygenase (HO). HO immunoreactivity is found throughout the airway in respiratory epithelium, alveolar macrophages, seromucous glands, and nose and paranasal sinuses. Like NOS, HO exists in constitutive (HO-2) and inducible (HO-1) isoforms. Whereas HO-2 is basally expressed in most tissues, HO-1 is identified as a heat shock protein inducible by a variety of stimuli including microbial toxins, proinflammatory cytokines, and reactive oxygen or nitrogen species; both isoforms are substantially expressed in human lungs. HO-1 is a cryoprotective and antiinflammatory enzyme that plays a critical role in defending the body against oxidant-induced injury during inflammatory processes. It catalyzes the first and rate-limiting step in the oxidative degradation of heme to CO and two other molecules (biliverdin and ferrous iron) with cytoprotective properties. The antiinflammatory properties of HO-1 are related to inhibition of adhesion molecule expression and reduction of oxidative stress, while exogenous CO gas treatment decreases the production of inflammatory mediators such as cytokines and NO. Like iNOS, HO is induced by many infectious agents, and levels of carboxyhemoglobin and/or exhaled CO are reportedly elevated in patients with viral or bacterial respiratory tract infections. Unlike NO, however, the direct effects of CO appear less microbicidal and more antiinflammatory, or host cytoprotective. In vitro and in vivo, CO has been shown to inhibit endotoxin-induced proinflammatory cytokines, including TNF, IL-1β, and macrophage inflammatory protein-1β (MIP-1β) while concurrently up-regulating antiinflammatory IL-10. Furthermore, in a murine model of influenza A pneumonitis, overexpression of HO-1 resulted in diminished respiratory epithelial cell apoptosis and decreased lung inflammation. Interestingly, HO appears to counteract the cytotoxicity caused by excessive production of NO. The up-regulation of iNOS in inducible pulmonary cells upon exposure to LPS results in a burst of NO generation that is essential for bactericidal effects. However, increased amounts of NO are also associated with deleterious effects such as tissue damage. Thus induction of HO-1 significantly reduces NO production and potentially restores cellular homeostasis. , It is well accepted that HO-1 and CO play an important role in minimizing injurious inflammatory processes during infection and other inflammatory states. Recent evidence, however, has identified an antimicrobial role for CO during infection. In vitro and in vivo studies have demonstrated that CO increases macrophage and neutrophil phagocytosis of the pathogenic organisms E. coli and E. faecalis, respectively. , Based on its anti-inflammatory properties, particularly in patients with chronic obstructive pulmonary disease, inhaled CO is currently being investigated in a phase I study to assess its pharmacologic potential to reduce acute airway inflammation (NCT00094406). Due to concerns regarding poor precision in the delivery of CO in the form of a gas, chemical carriers known as CO-releasing molecules (CO-RMs) have been developed. , Recent studies by Murray and coworkers demonstrated that CO-RM-2, a ruthenium-containing CO-RM soluble in dimethyl sulfoxide, attenuated biofilm formation and planktonic growth of the majority of both mucoid and nonmucoid strains of P. aeruginosa isolates.
Because of its anatomic location at the interface between the vascular and alveolar compartments, the endothelium is uniquely situated to regulate pulmonary immune responses requiring recruitment and facilitated passage of intravascular inflammatory cells. Vascular endothelial cells express MHC class II molecules and may present antigens to T cells. Endothelial cells also participate in immune processes by elaborating or responding to cytokines in the local microenvironment. For example, TNF-α is an endogenous mediator of inflammatory immune responses secreted by alveolar macrophages in response to bacterial endotoxin. Endothelial cells manifest a pleiotropic response to TNF-α, including increased expression of adhesion molecules, increased prostaglandin production, increased MHC antigen expression, and increased cytokine release including IL-1, IL-6, IL-8, granulocyte-macrophage colony-stimulating factory (GM-CSF), and monocyte chemotactic protein-1 (MCP-1). , , The net effect of these signals is an increased chemotactic recruitment and activation of inflammatory cells at the interface of the vascular space and the interstitium; the TNF-induced increase in endothelial cell-leukocyte adhesion further enhances this response. Endothelial cells also express the TLRs TLR4 (constitutive) and TLR2 (inducible by IFN-γ or TNF-α); this allows a direct response to endotoxin, manifested by up-regulation of adhesion molecule expression and induction of IL-1, IL-8, MCP-1, and GM-CSF expression. By responding either to endotoxin directly or to endotoxin-induced macrophage-derived TNF-α, the endothelial cell may either generate an initial immune response or participate in amplifying a local inflammatory cascade. The up-regulation of adhesion molecules on the endothelium allows for neutrophil attachment, rolling, firm attachment, and ultimately diapedesis.
Whereas most studies of fibroblasts have focused on their production of structural and matrix proteins, it is now evident that fibroblasts may also function as important immune-effector cells at sites of inflammation. When appropriately stimulated, fibroblasts may generate bioactive amounts of multiple cytokines, including IL-6, IL-8, IL-1α, IL-11, colony-stimulating factors (CSFs), and growth factors such as TGF-β. TNF-α or IL-1 can each induce fibroblast-derived IL-6, IL-1, IL-8, and IL-11, and their combined action synergistically further up-regulates fibroblast elaboration of these cytokines. , Although fibroblasts and alveolar macrophages are often capable of elaborating the same inflammatory cytokine(s), maximal production of these cytokines typically occurs in response to different signals. This is illustrated by the distinct response of these cells to endotoxin. Endotoxin is a potent stimulator of macrophage-derived TNF-α and IL-1 but exerts little direct stimulation of fibroblasts. Conversely, pulmonary fibroblasts elaborate inflammatory cytokines in response to IL-1 and TNF-α, whereas macrophage response to these cytokines is more diverse. This suggests that, although classic immune cells such as alveolar macrophages produce inflammatory cytokines in a stimulus-specific fashion, fibroblasts produce inflammatory cytokines in response to macrophage-derived TNF-α or IL-1, independent of the precipitating stimulus. This response serves to amplify local pulmonary inflammation and illustrates the potential immunologic role of the fibroblast, transcending its putative structural function. IL-17 can induce chemokine generation by lung fibroblasts, which also may be important in establishing chemokine gradients with lung tissue.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here