Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

Neck masses are commonly encountered in children, and a wide range of etiologies is possible such that familiarity with anatomic locations and a diagnostic approach is necessary in order to arrive at a specific diagnosis or to narrow the differential diagnosis.
A particularly helpful approach is to determine whether the mass best falls within categories of a cystic, solid, vascular, calcified, or bone-associated mass. Each of these main categories will contain several possible lesions, many of which have helpful clues.
This chapter will illustrate the many common and uncommon etiologies for neck masses in children.


Ultrasound: anechoic
CT: Thin wall; uniform fluid density; no solid component
MRI: Thin wall; nonenhancing; no solid component; T2W hyperintensity; ADC hyperintense
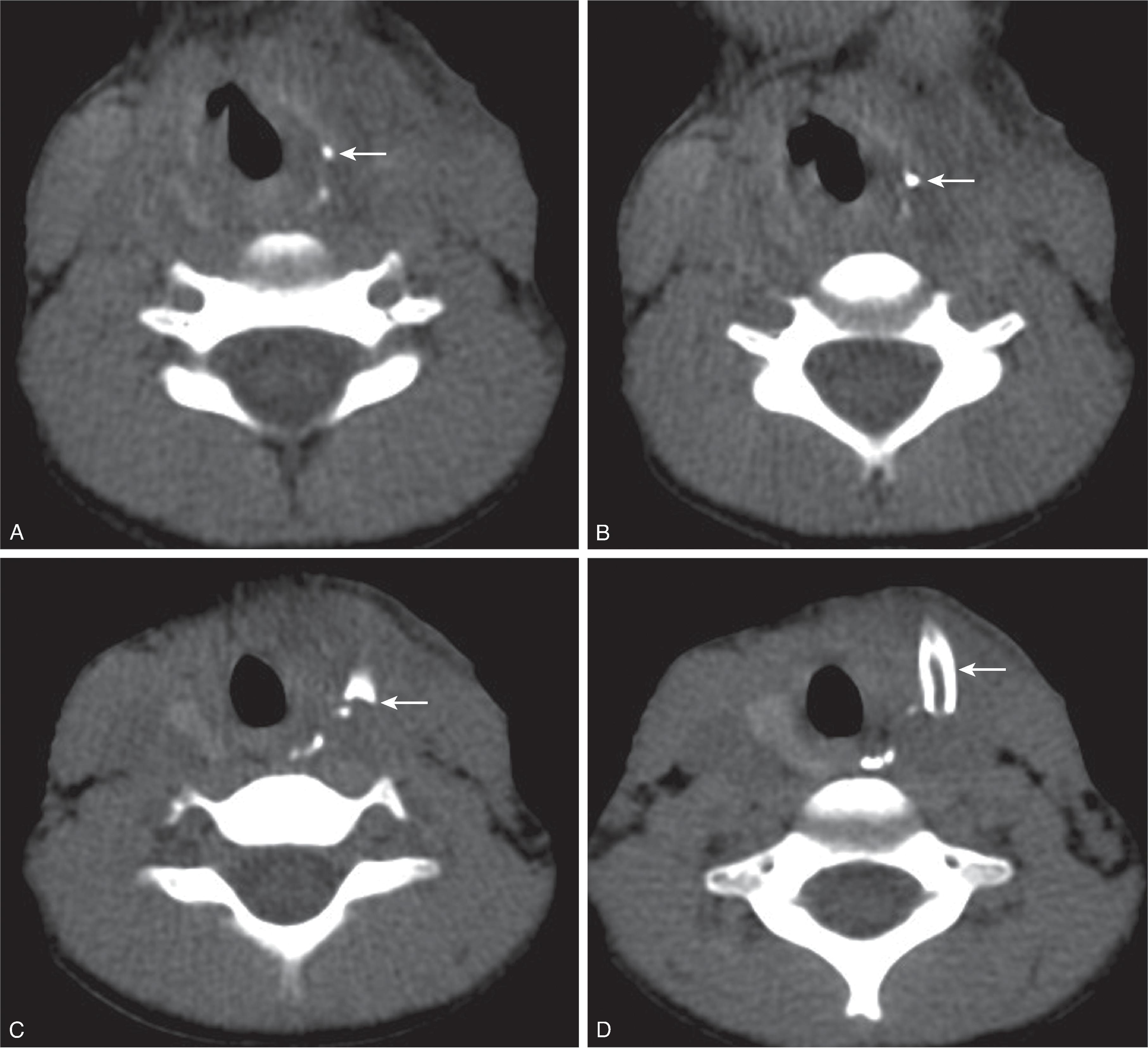
Suprahyoid thyroglossal duct cyst: Comprise 20% of TGDCs; midline location.
Hyoid/infrahyoid TGDC: Comprise 80% of TGDCs; located within 2 cm of midline; associated with strap muscles.
May present with superinfection and demonstrate thickening of the cyst wall surrounding inflammation on imaging as well as secondary skin fistula.
Rarely (<1%) may develop thyroid neoplasm (most commonly papillary thyroid cancer). The presence of Ca 2+ can indicate neoplasm.
Differential Diagnosis: Dermoid/epidermoid cyst.
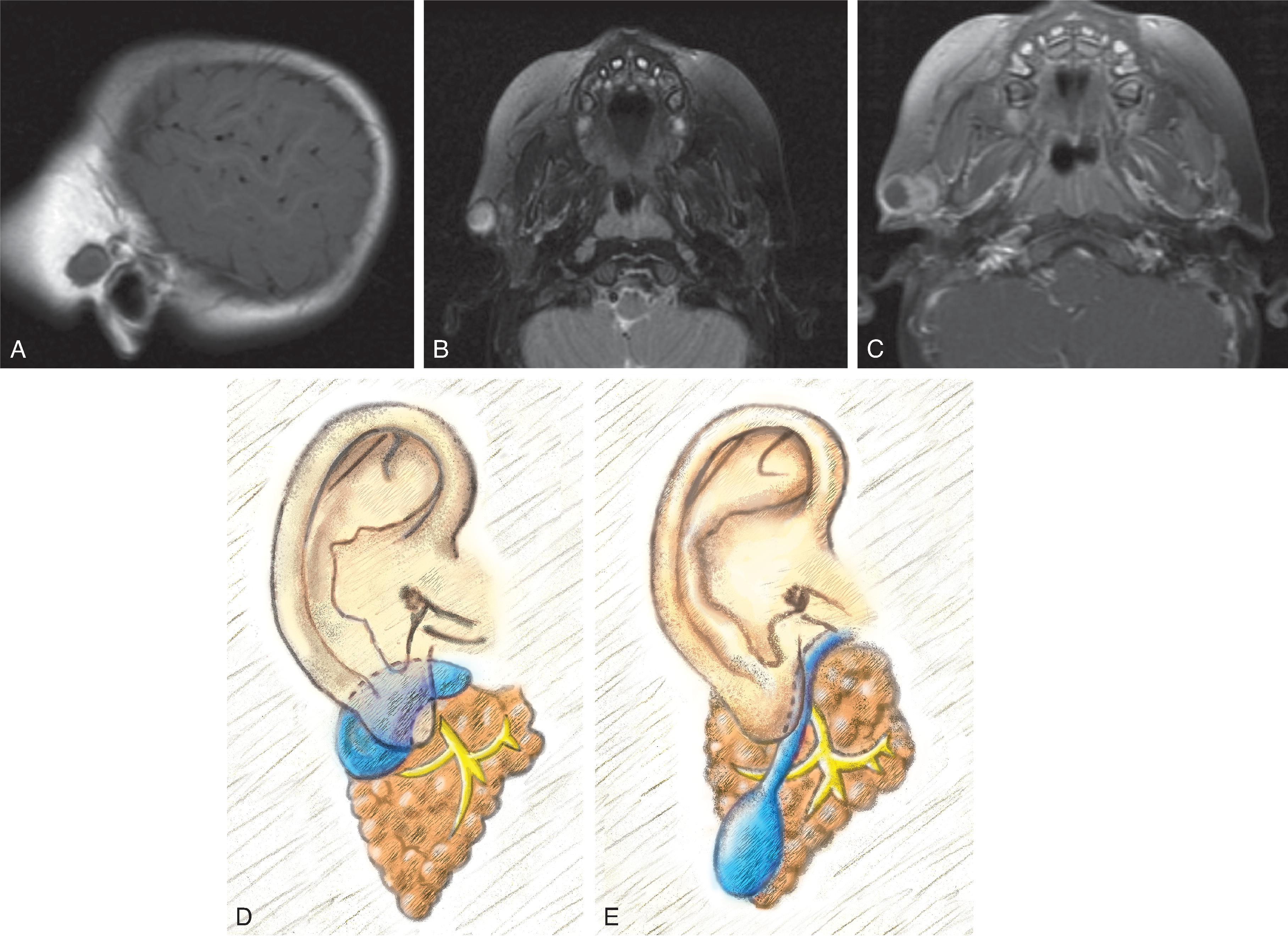
8% of branchial cleft remnants
May become superinfected or lead to otitis externa. Recurrent otitis externa should raise suspicion for a first branchial cleft anomaly.
Subdivided into:
Type 1: Periauricular
Type 2: Periparotid/extending from the external auditory canal (EAC) to angle of mandible
Thin walled fluid filled cyst. Less common to have sinus tract or fistula
Differential Diagnosis: Parotid tumor or necrotic lymph node

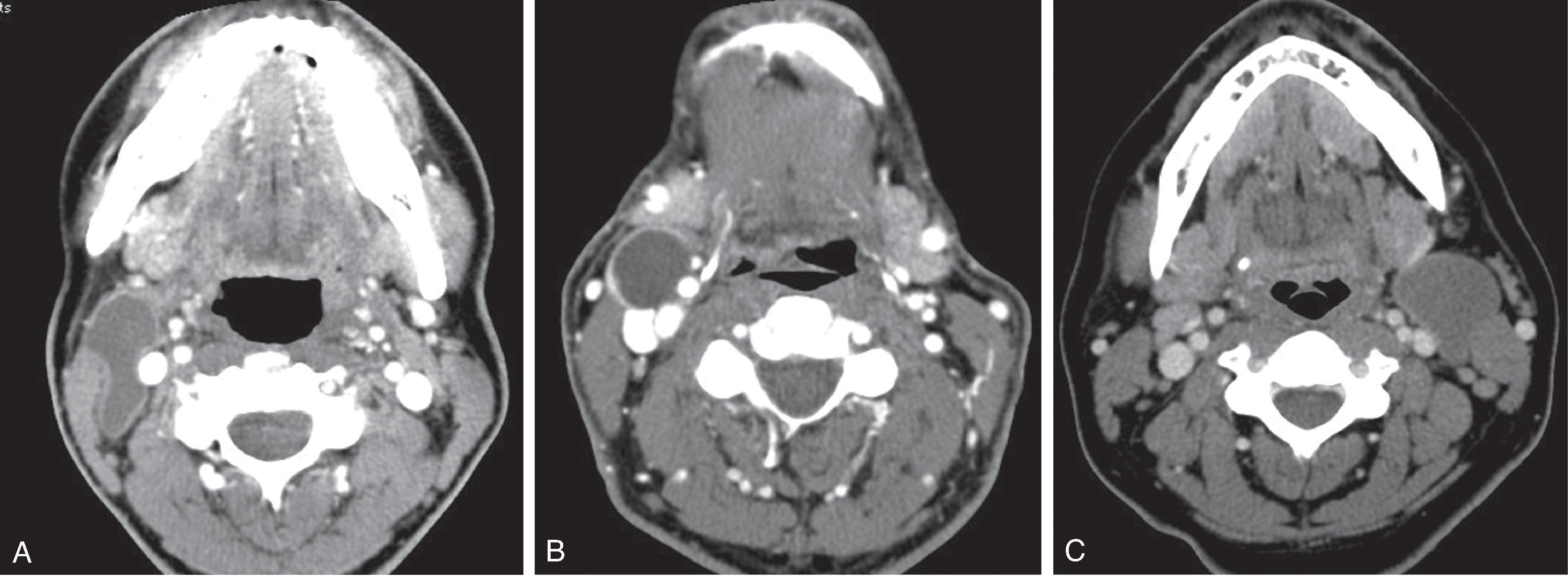
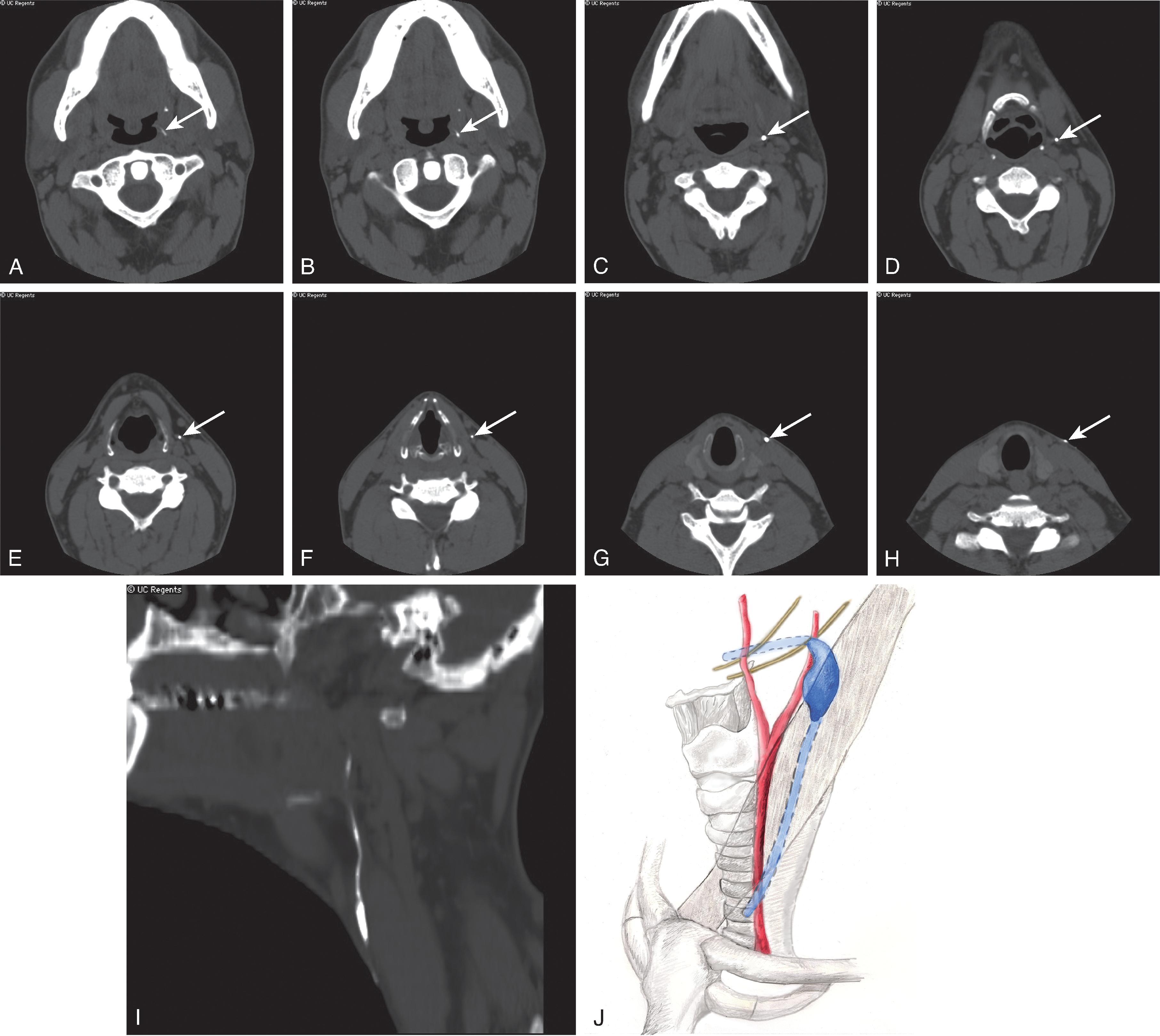
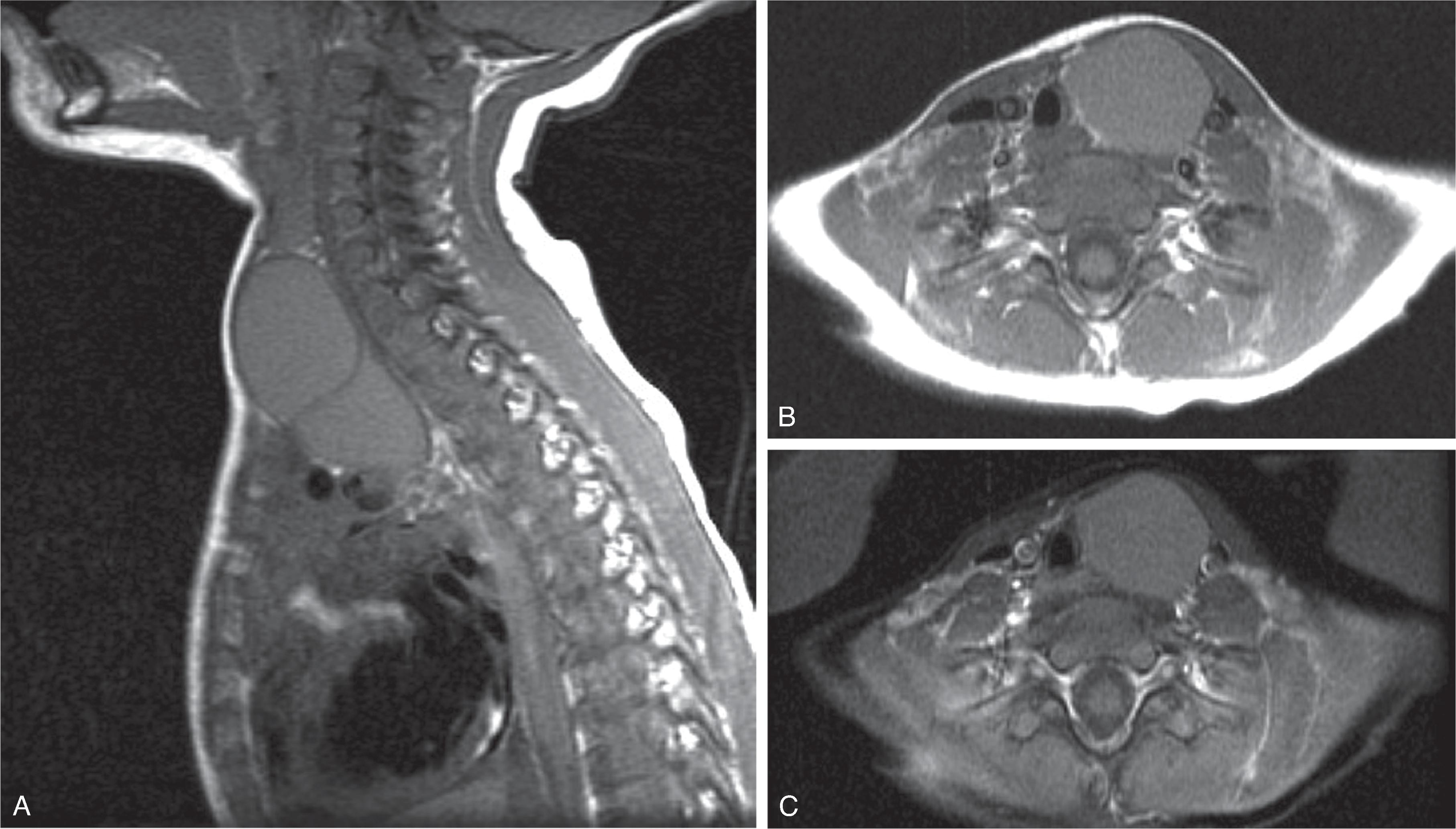
Most common branchial cleft anomaly (children 66%–75% vs adults >90%)
Occurs along a tract that courses from palatine tonsil → anterior and lateral to the carotid space and posterior to the submandibular gland → lateral neck anterior and medial to sternocleidomastoid muscle (SCM) → existing the skin at the level of the thyroid gland anterior to the junction of the middle and inferior thirds of the SCM
Most commonly a cyst but can also occur as a sinus tract or fistula.
Most common location: Lateral neck located posterolateral to submandibular gland, lateral to carotid space, and anteromedial to SCM
Uncommon locations: Inferior along the infrahyoid carotid space; superior into the parapharyngeal or carotid space; lateral pharyngeal wall
Fistula opening usually located at the junction of the middle and lower third of the SCM
Differential Diagnosis: Suppurative/necrotic node, or lymphatic malformation

Includes cervical thymic cyst and third branchial cleft cyst
Third branchial cleft cyst: Rare; unilocular cystic mass.
Location: most are found in the posterior triangle of the neck, lower anterior neck along anterior SCM or submandibular space.
Third branchial cleft fistula courses from the upper pyriform sinus → above the superior laryngeal nerve and between the cranial nerve 9 and 12 → posterior to the carotid artery and posteromedial to the SCM → exiting through the skin along anterior border of lower one-third of the SCM.
Differential Diagnosis: Lymphatic malformation.
Note that a cervical thymic cyst is cyst from the third branchial pouch, which is different from the branchial cleft. See Thymic Cyst section for further details.
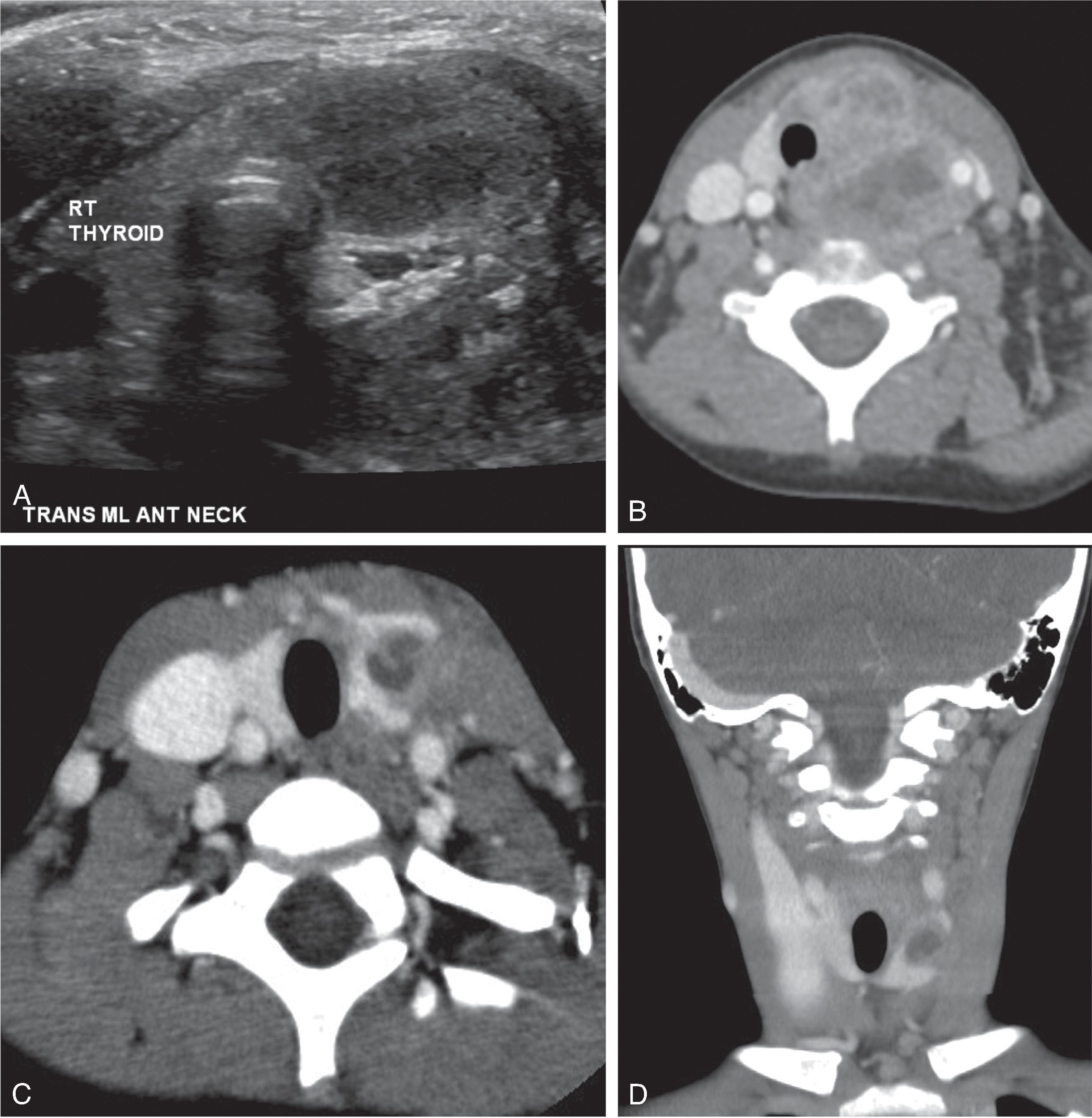
Presents with thyroid gland infection (usually unilateral left thyroid lobe).
Some combine third and fourth branchial cleft anomalies due to difficulty distinguishing the two. The location of the sinus tract with respect to the superior laryngeal nerve is key for differentiating the 3rd and 4th cleft anomalies.
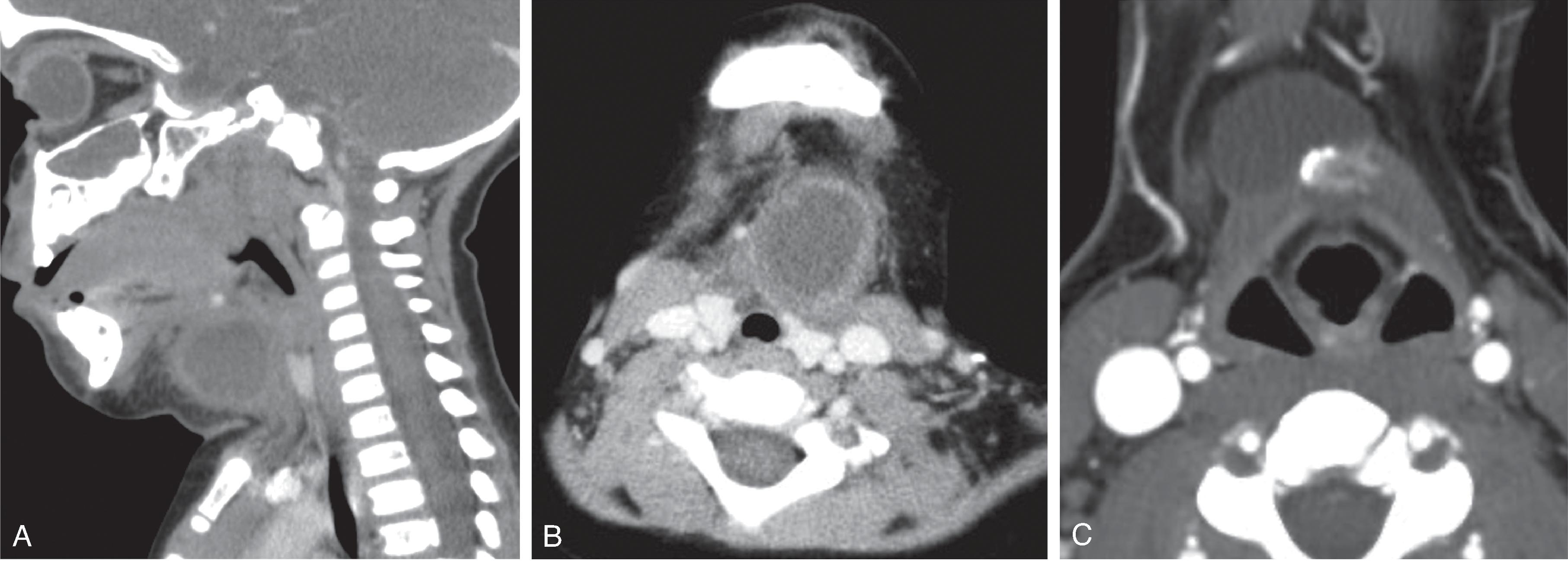
Most commonly a sinus tract from the lower piriform sinus → below the superior laryngeal nerve → tacheoesophageal groove to the thyroid gland, usually the left lobe (80%). Although not clinically seen, the path follows the course of the recurrent laryngeal nerve and continues inferiorly to loop around the aorta in a posterior to anterior direction on the left side and subclavian artery on the right side and ascends posterior to the common carotid artery and exits the skin anterior to the sternocleidomastoid muscle.
Thyroid gland infection typically seen on CT as an enlarged lobe, low-density areas in the lobe, organized fluid collections (abscess), and adjacent soft tissue inflammation and possible SCM myositis
Barium swallow study followed by CT scan can demonstrate the sinus tract


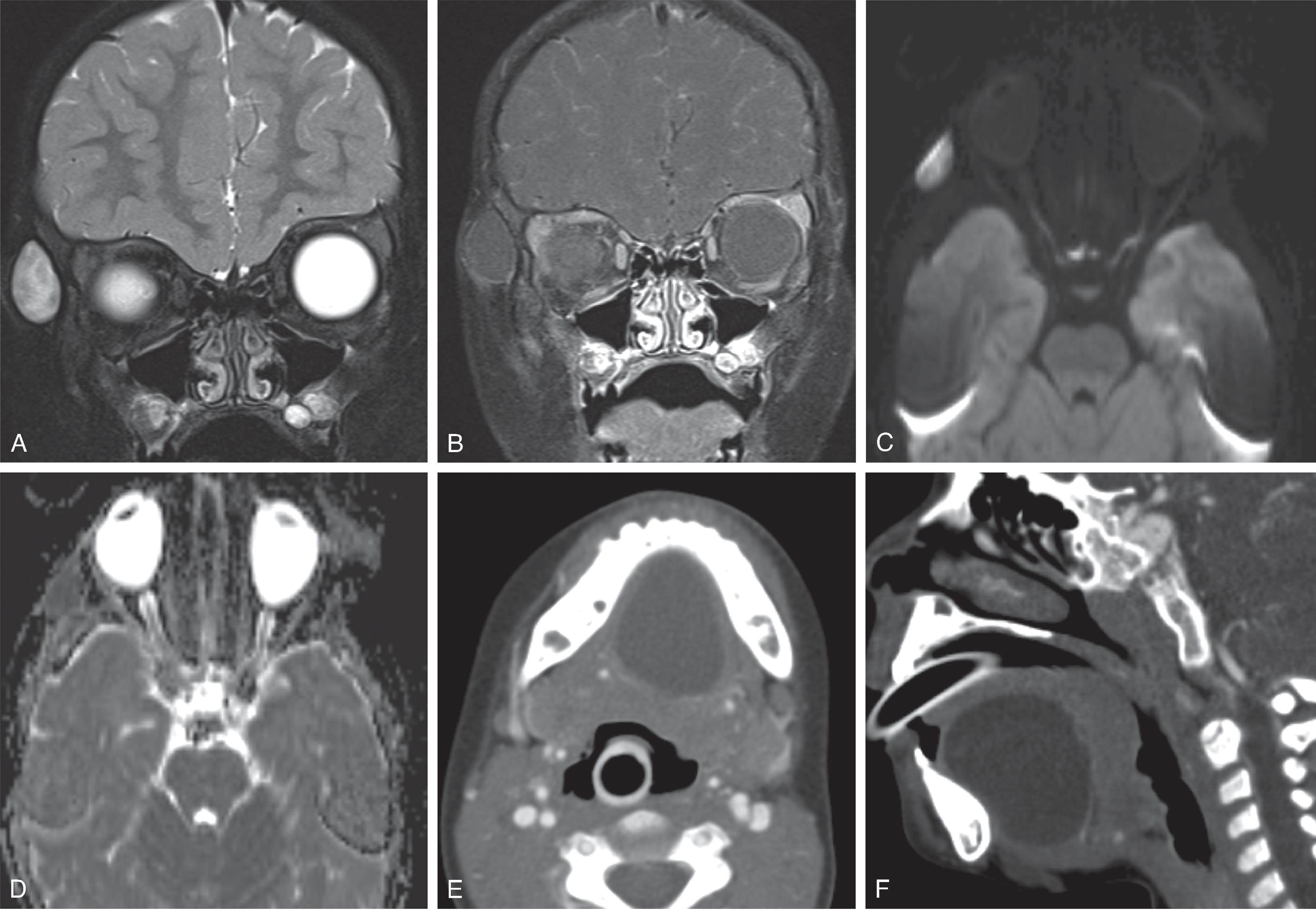
Previously referred to as cystic hygroma or lymphangioma.
Cystic mass composed of chyle-filled endothelial lined channels.
Categorized as a slow or no-flow malformation.
90% present by 2 years of age. 75% occur in the neck.
May present with rapid proptosis or acute neck mass if internal hemorrhage occurs or when a viral infection stimulates fluid production.
Transpatial/multispatial cystic mass in the face and neck.
Macrocystic: Low density, hypoechoic; lobular, cystic areas with fluid-fluid levels; no-flow voids; nonenhancing except for septations or if venous component is present.
Microcystic (<2 mm cyst size) may appear hyperechoic and may simulate an enhancing mass due to the close proximity of the septations.
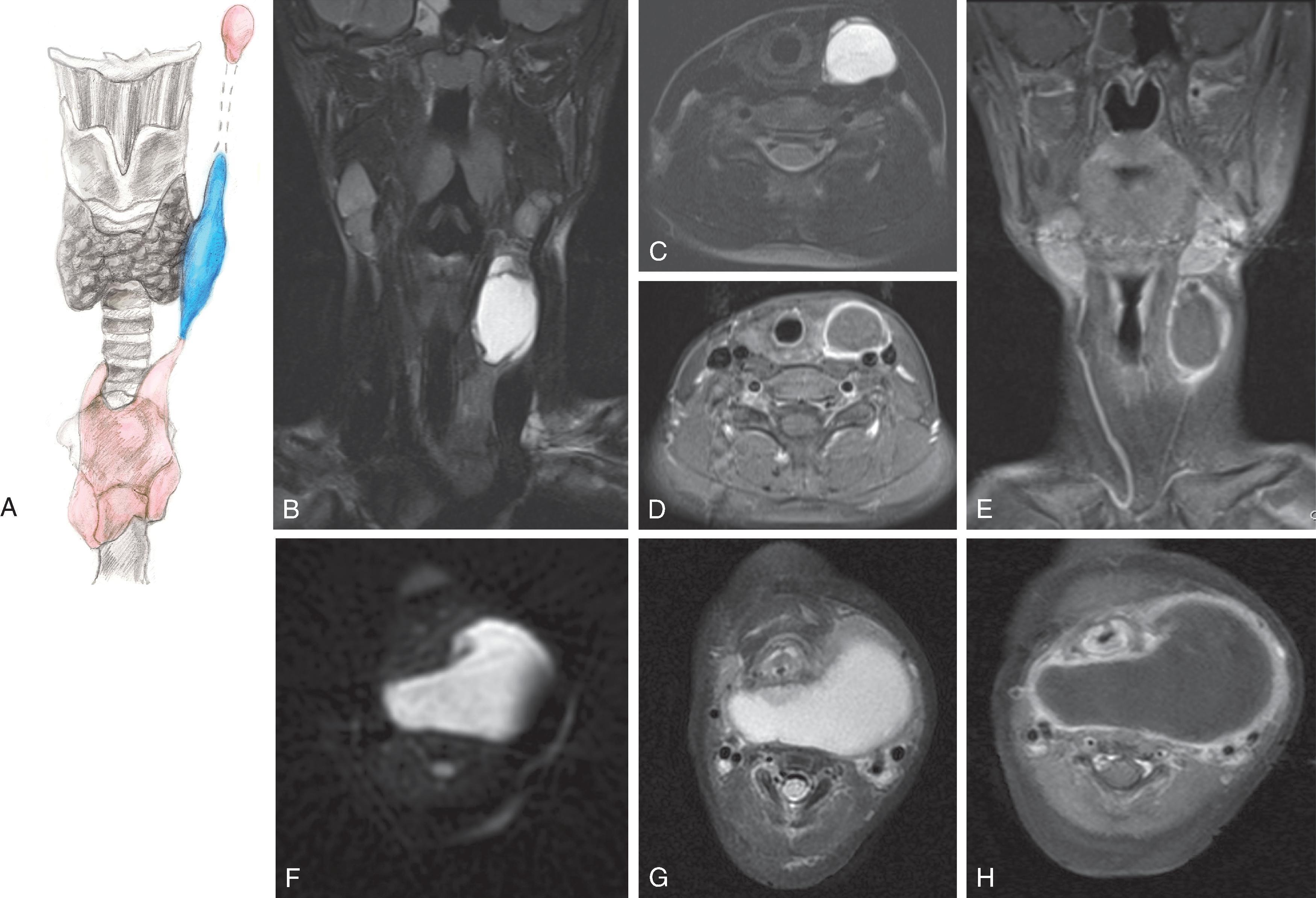
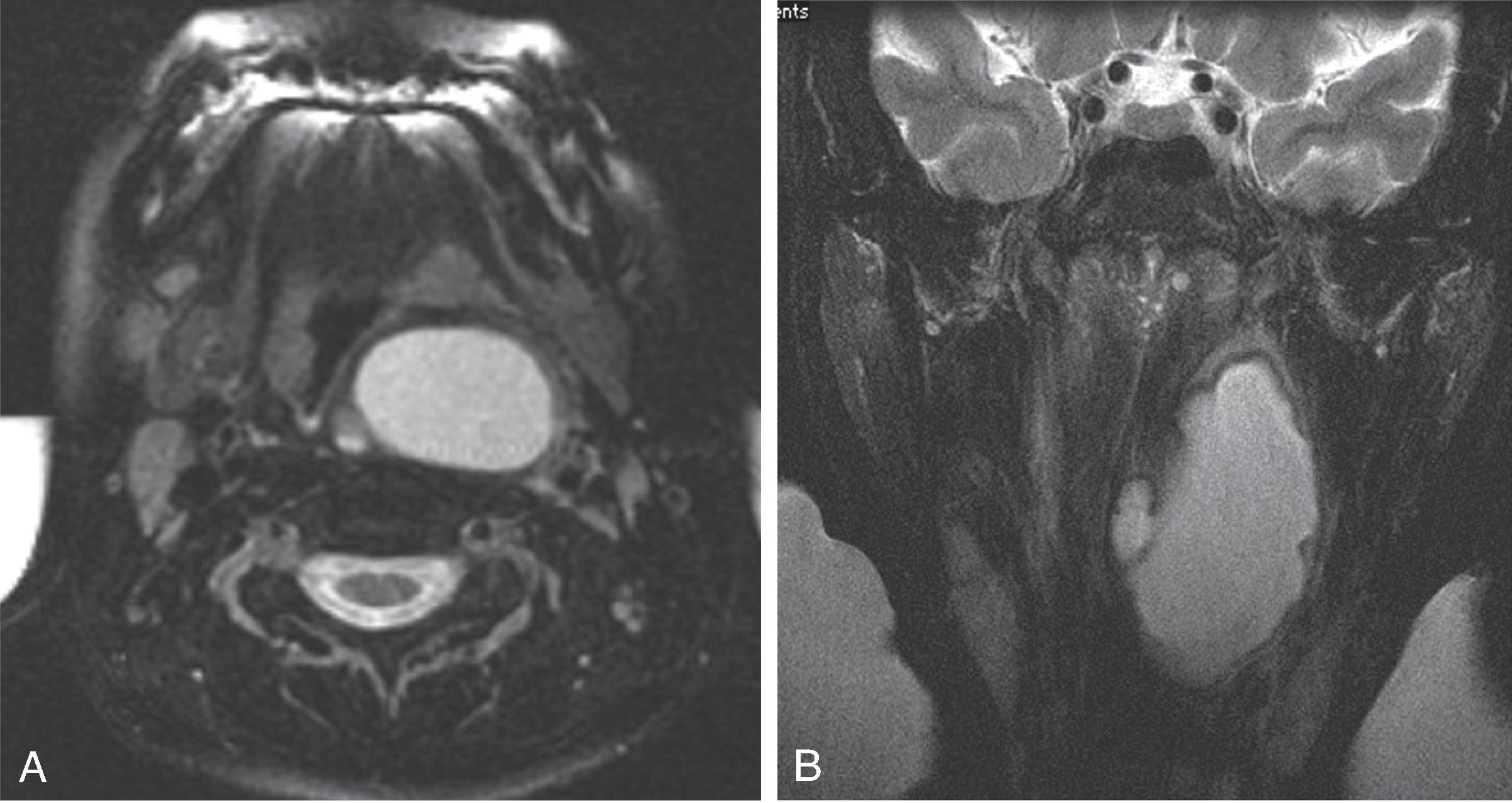
Cystic remnant of the thymopharyngeal duct, which is a derivative of the third branchial pouch (as opposed to branchial cleft)
Course of the thymopharyngeal pouch is from the piriform sinus → anterolateral neck along the parotid sheath → midline mediastinum
A rapidly enlarging neck mass in a neonate can occur from superinfection of a thymic cyst due to communication between the aerodigestive tract and the cyst. Treated with drainage and surgical resection
Unilocular cyst in the lateral neck; typically fluid signal
Superinfection can result in diffusion restriction from purulent material.
Extends into the retropharyngeal space when large
50% are continuous with the mediastinal thymus.
Three types: Bronchogenic, esophageal, and neurogenic.
Duplication cysts can be found from the mouth to the anus. Foregut anlage gives rise to the pharynx, respiratory tract, esophagus, stomach, and first and second parts of the duodenum.
Foregut duplication cysts are usually midline , often infrahyoid, floor of mouth, or posterior mediastinal.
Often discovered incidentally.
Differential Diagnosis: Thymic cyst.
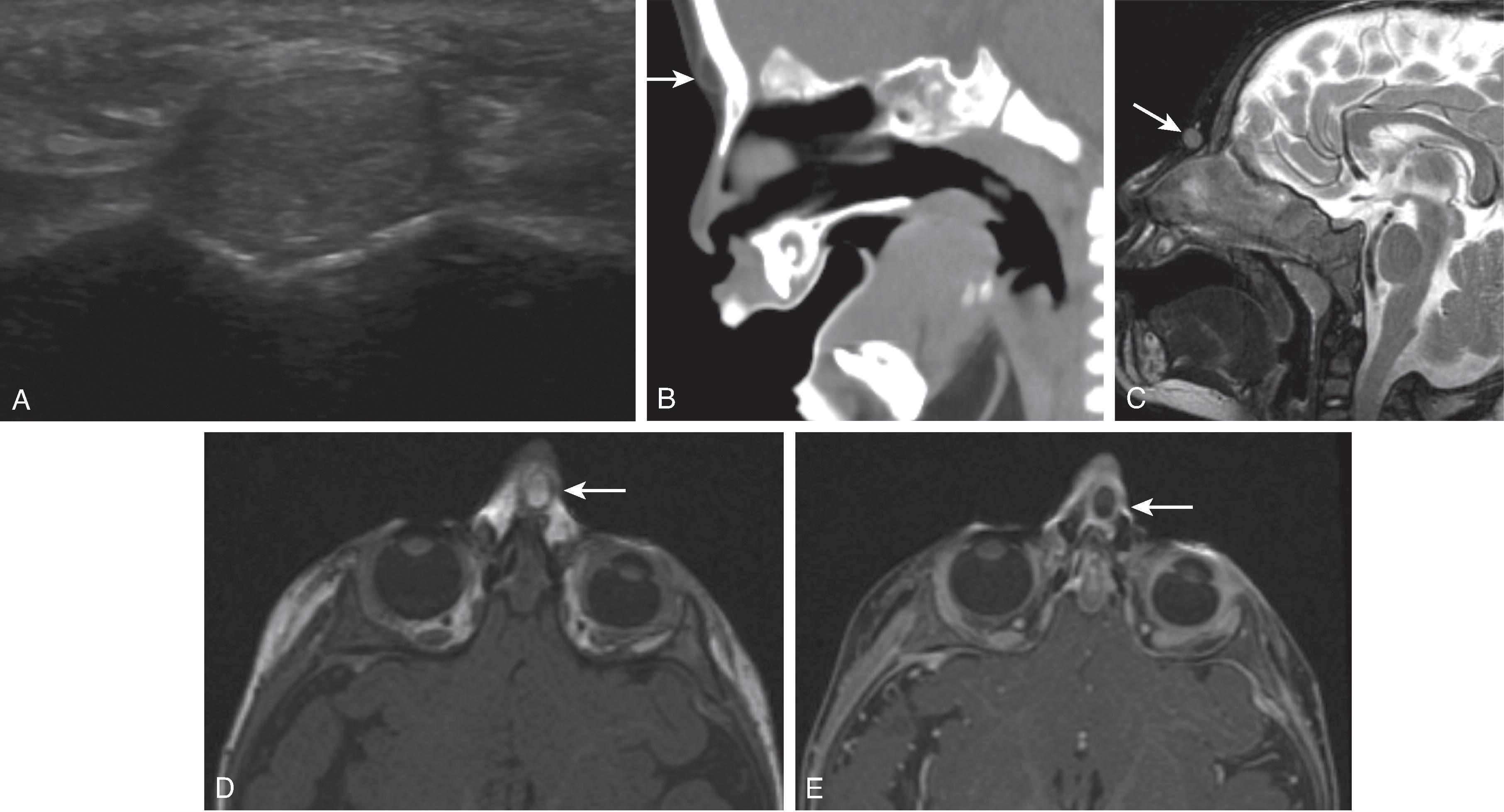
Congenital malformation due to skin elements pulled into the prenasal space along with the regressing dural diverticulum.
Occur from the tip of the nose to the crista galli. More common than epidermoid cysts. CNS connection in ∼50%. Sinus tract opening, dimple or tuft of hair at the skin surface is present in 84%.
Surgical removal to prevent intracranial infection.
CT: Wide foramen cecum; bifid crista galli; fat density
MRI: Nonenhancing; T1 hyperintensity
Differential Diagnosis: Encephalocele, and nasal glioma/hamartoma

Benign cyst arising from an epidermal rest
Common locations: Lateral orbit and floor of mouth
Midline or paramedian in location
Fluid density/intensity; T2 hyperintensity; diffusion restriction
Can become superinfected if a coexistent dermal sinus tract from the skin is present
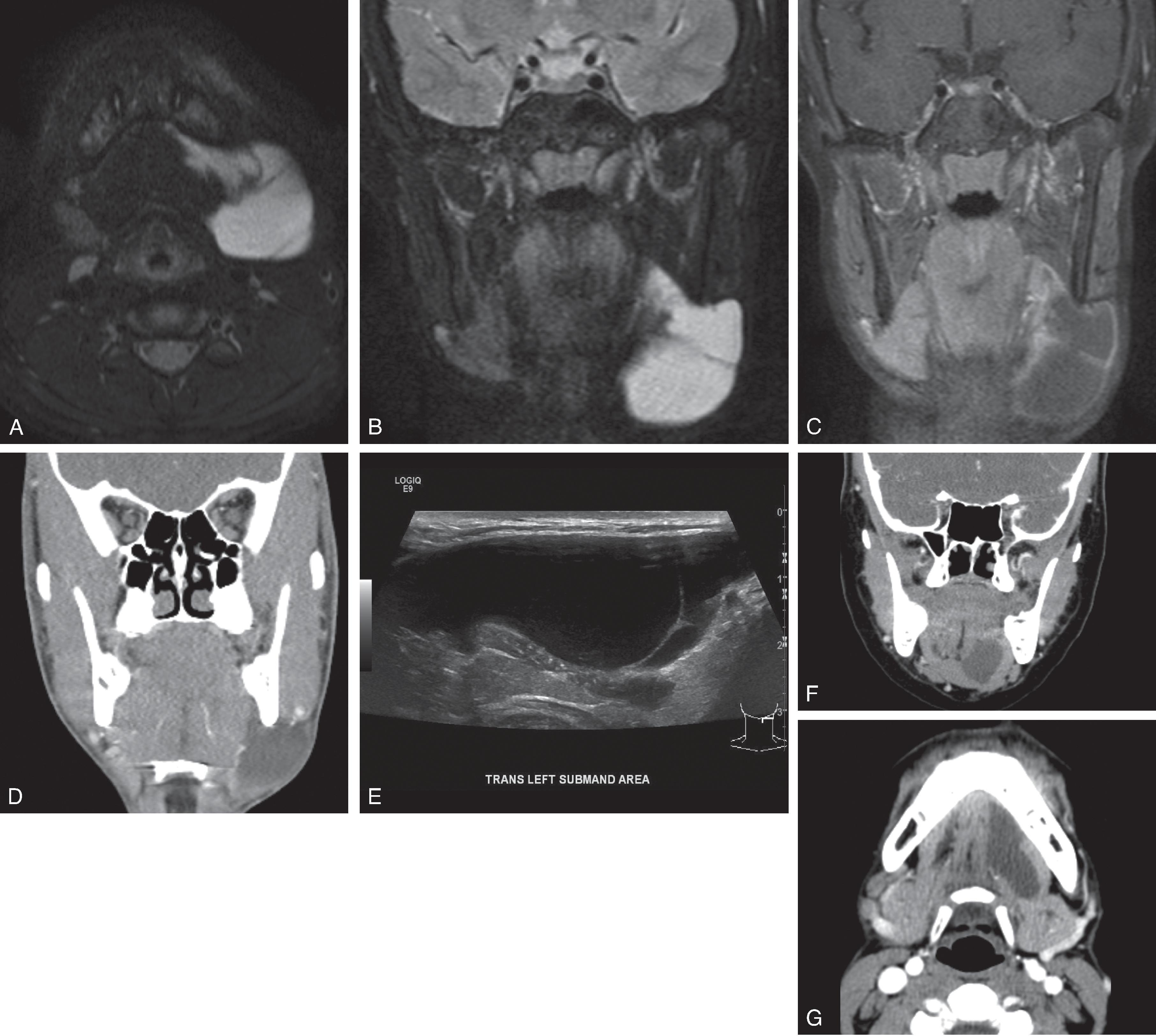
Retention cyst of the sublingual gland or minor salivary glands resulting from trauma or inflammation
Unilocular fluid density/intensity; thin wall.
Simple ranula is confined to the sublingual space.
Diving ranula extends into the submandibular space with a pointed/tail toward the sublingual space.
The annual incidence of thyroid cancer is low in children younger than 15 years (2 per million), although prepubertal children tend to have a more aggressive presentation. The incidence is higher in children aged 15 to 19 years (17.6 per million).
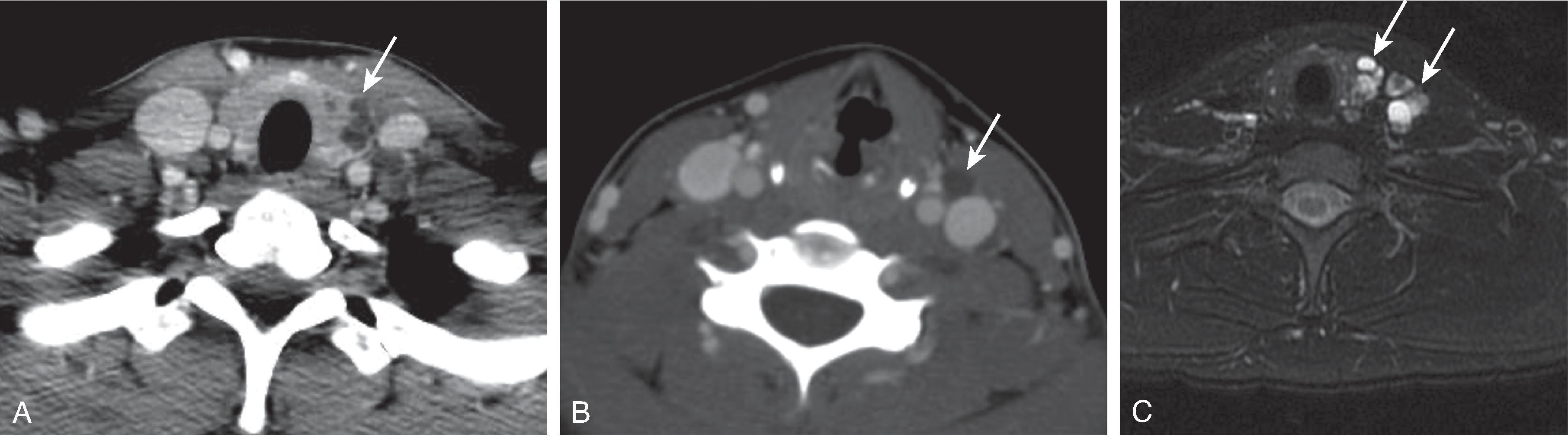
CT: Hypodense nodule/mass compared to thyroid gland and muscles. Often, the mass contains dystrophic calcification. Metastatic thyroid carcinoma can have solid or cystic nodes and may have calcifications.
MRI: Metastatic lymph nodes may have T2W hyperintensity from cystic degeneration and/or intrinsic high T1W signal due to thyroglobulin and/or hemorrhage.
Important to assess for extrathyroidal extension, lymph node involvement, and lung metastasis.

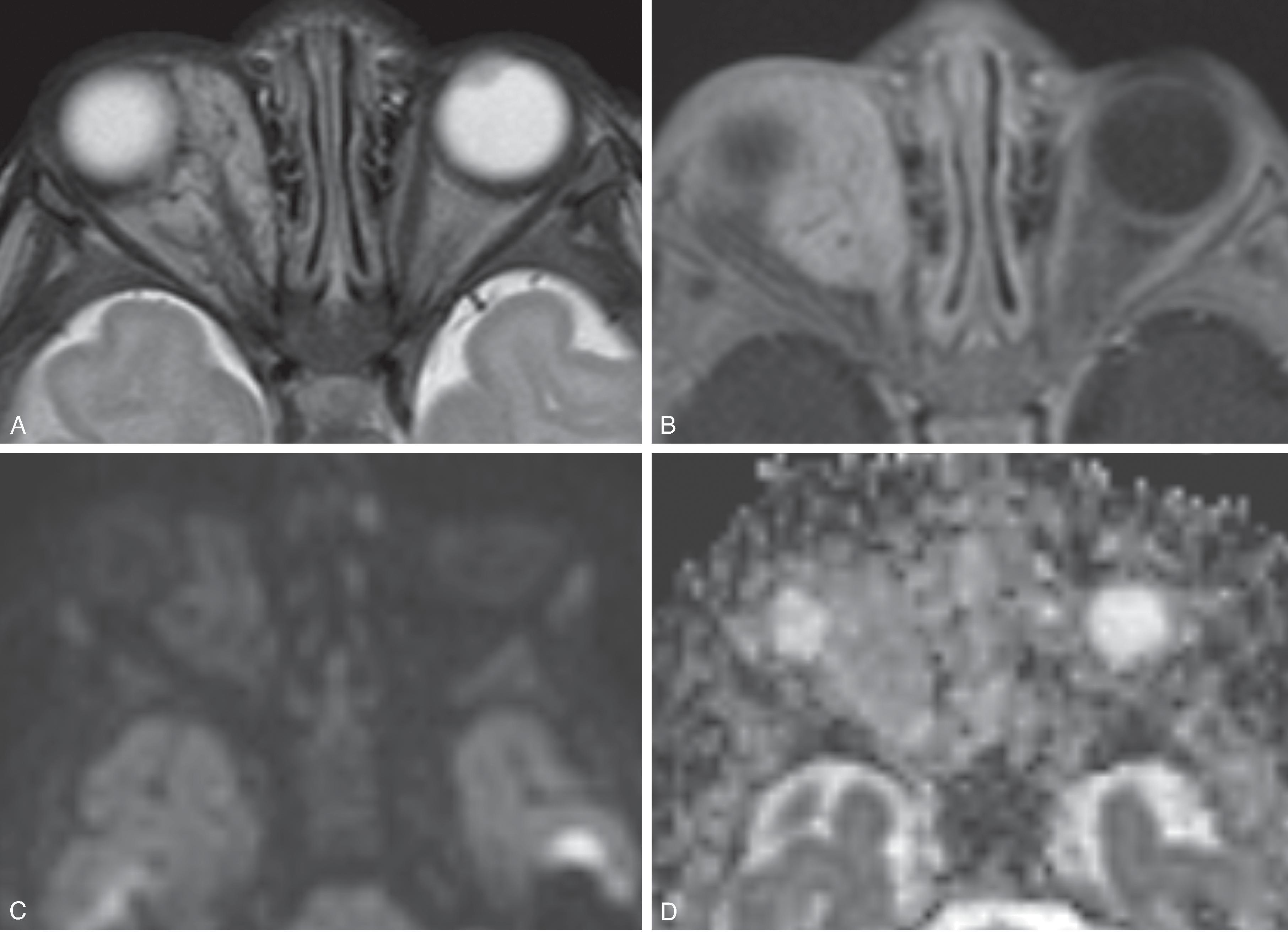
The most common benign tumor of infancy. 95% present before 6 months of age. Often involute spontaneously.
Predilection for superior orbit, eyelid, and supranasal periorbita (can be intraconal and extend to superior orbital fissure).
Associated with PHACES syndrome:
P osterior fossa malformation
H emangioma
A rterial anomaly
C oarctation of the aorta
E ye abnormality
S ternal defect and supraumbilical raphe.
Treatment options include propranolol steroids, interferon, laser therapy, and surgical excision.
Circumscribed or infiltrative
US: Variable echogenicity with high flow velocity
CT: Solid tissue density; homogenous enhancement; no gross Ca 2+
MRI: Mild T2W hyperintensity; flow voids; intense enhancement; ADC hyperintense, which helps distinguish from orbital rhabdomyosarcoma
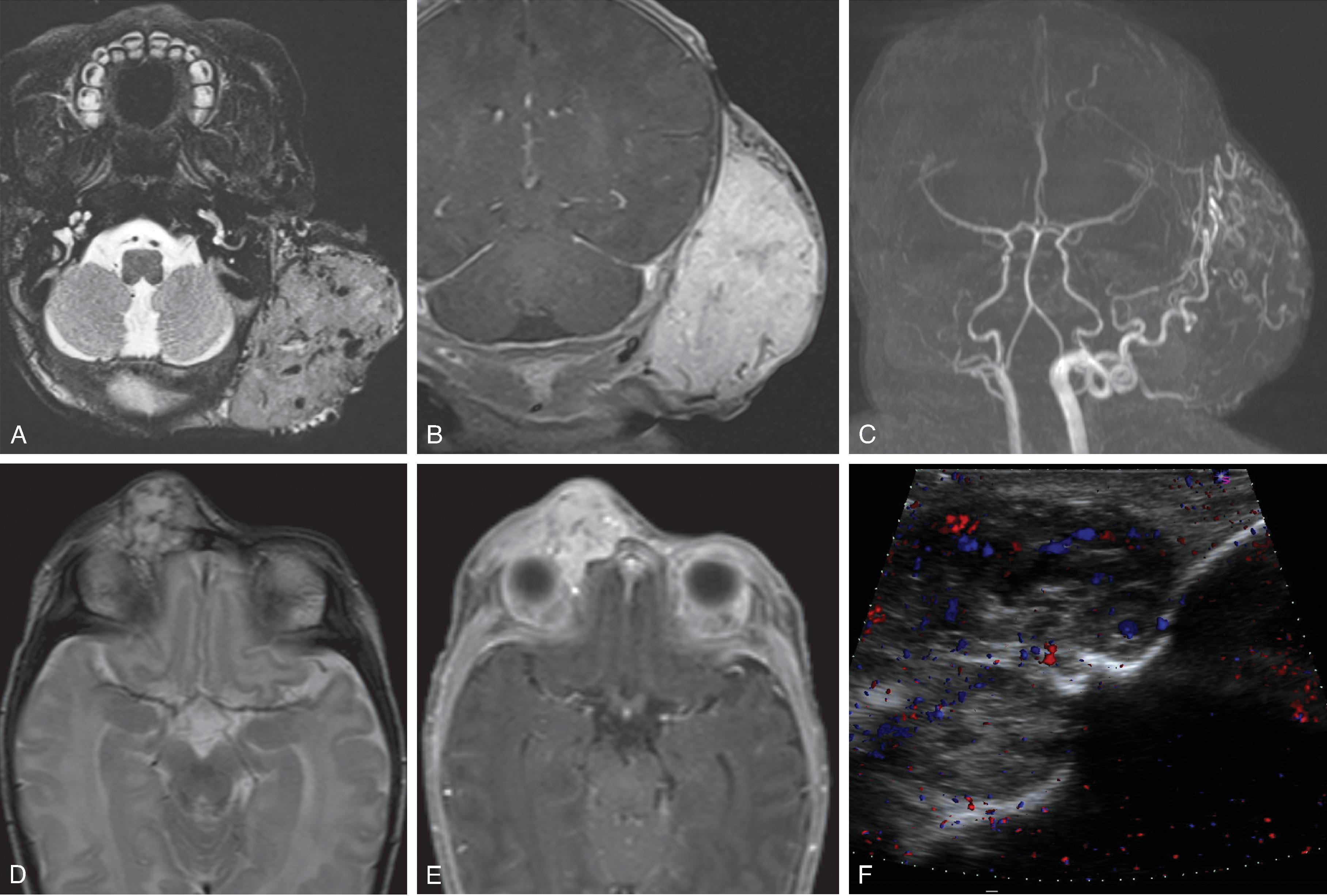
Benign vascular tumor present at birth.
Rapidly involuting congenital hemangioma (RICH) and non-involuting congenital hemangioma (NICH).
RICH usually regress by 14 months, while NICH proportionally grows with the child without regression.
Neither expresses GLUT-1 transporter, which differs from infantile hemangiomas; may result in vascular shunting or thrombocytopenia when large; does not respond to treatment with propranolol.
Avidly enhancing mass with flow voids and enlarged arterial feeding vessels; may contain calcification and visible vessels on US to greater degree than infantile hemangiomas

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here