Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The nose maintains the central position on the face and often can be a challenging structure to successfully reconstruct, both its form and the function. The fundamental techniques of reconstruction emerged early in history as a response to the use of nasal rhinokopia (nasal amputation) as a punishment. , Sushruta Samitha (600 BC) described both the use of pedicled cheek flaps and the paramedian forehead flap for nasal reconstruction. , In 15th-century Italy, Antonio Branca first described the use of a pedicled flap from the arm for nasal reconstruction (often known in Europe as the Italian technique). This technique was further popularized by Gaspare Tagliocozzi with his version of this flap (Tagliocozzi flap). Later, a series of surgeons in France further refined the use of the pedicled cheek flap.
In the modern era, nasal defects are commonly encountered after cancer resection and trauma. While there are multiple options available for reconstruction of the nose, the surgeon’s challenge is to select the most appropriate option for the defect. There has been a continuous process of improvement of results as the plastic surgeon now pays closer attention to reconstructing the details of the nose (including color and texture match) while minimizing the donor site morbidity.
The nose is a composite structure composed of three layers: the nasal skeleton, the nasal lining, and the external cover.
The nasal skeleton is the supporting structure of the nose. It consists of the nasal bones and ascending processes of the maxilla in the upper third, the paired upper lateral cartilages in the middle third, and the lateral paired alae in the lower third.
The upper lateral cartilages are attached lightly to the caudal edge of the nasal bones and the dorsal border of the nasal septum, the “keystone area,” allowing them to remain suspended above the nasal cavity. At the junction of septum and upper lateral cartilages, the dorsal border of the septum widens to form a “T.” This broadening is crucial, as it maintains the aperture of the internal valve during nasal inspiration.
The paired alae support the lower third of the nose by uniting to form a tripod configuration with the nasal tip, as first described by Anderson. The paired medial crura form the central leg of the tripod and are attached to the anterior nasal spine and septum in the midline. The lateral crura compose the two lateral legs of this tripod, and they are attached to the pyriform aperture. Between the lateral and medial crura, the dome defines the apex of the alar cartilage. It supports the nasal tip and is responsible for the light reflex of the tip. The region of fibrous connection of the ala with the upper lateral cartilages is known as the “scroll” area. The normal ala does not contain cartilage but a compact stiff fibrofatty tissue. Alar reconstruction has to include cartilage, however, to prevent collapse and retraction.
The nasal lining consists of a thin layer of vascular mucosa. The nasal vestibule is lined by stratified squamous epithelium, while internally it is lined by mucosa. The lining tightly adheres to the deep surface of the nasal skeleton. The mobility of the mucosa is limited by this dense adherence. Consequently, only the smallest of mucosal defects (<5 mm) can be closed primarily. The anterior septal branch of the labial artery and medial internal nasal branch of the anterior ethmoid artery may be used for lining flaps as described below.
From deep to superficial, the nasal skeleton is covered by perichondrium/periosteum, an areolar tissue plane, a musculoaponeurotic plane, a subcutaneous layer (a few millimeters of fat), dermis, and epidermis. In the upper two-thirds of the nose, the skin is thin, loose, and mobile, with a slight excess. It contains few sebaceous glands. Proceeding inferiorly from the glabella, skin thickness decreases over the cartilaginous dorsum and upper lateral cartilages. Conversely, as it reaches the tip and ala, the skin becomes thick, sebaceous, and tightly adherent to the ala, which limits mobility. Thus, regardless of design, local flaps will generally mobilize the upper thirds of skin excess to resurface inferior defects.
Nasal vasculature runs in the subcutaneous layer. On each side of the nose, the blood supply is derived from the dorsal nasal branch of the ophthalmic artery, which creates an axial network for the dorsal and lateral nasal skin. The angular artery, a branch of the facial artery, passes medially along the cephalic margin of the lateral crura, just above the alar groove, supplying the lateral surface of the caudal nose. The columellar artery, a branch of the superior labial artery, supplies the nasal sill, septum, and base of the columella. Finally, the infraorbital branch of the internal maxillary artery supplies the dorsum and lateral sidewalls of the nose. Venous drainage parallels the arterial system.
The anterior septal branch of the superior labial artery, medial internal nasal branch of the anterior ethmoid artery, septal branch of posterior ethmoid artery, posterior septal branch of sphenopalatine artery, and greater palatine artery supply nasal mucosa ( Fig. 30.1 ).
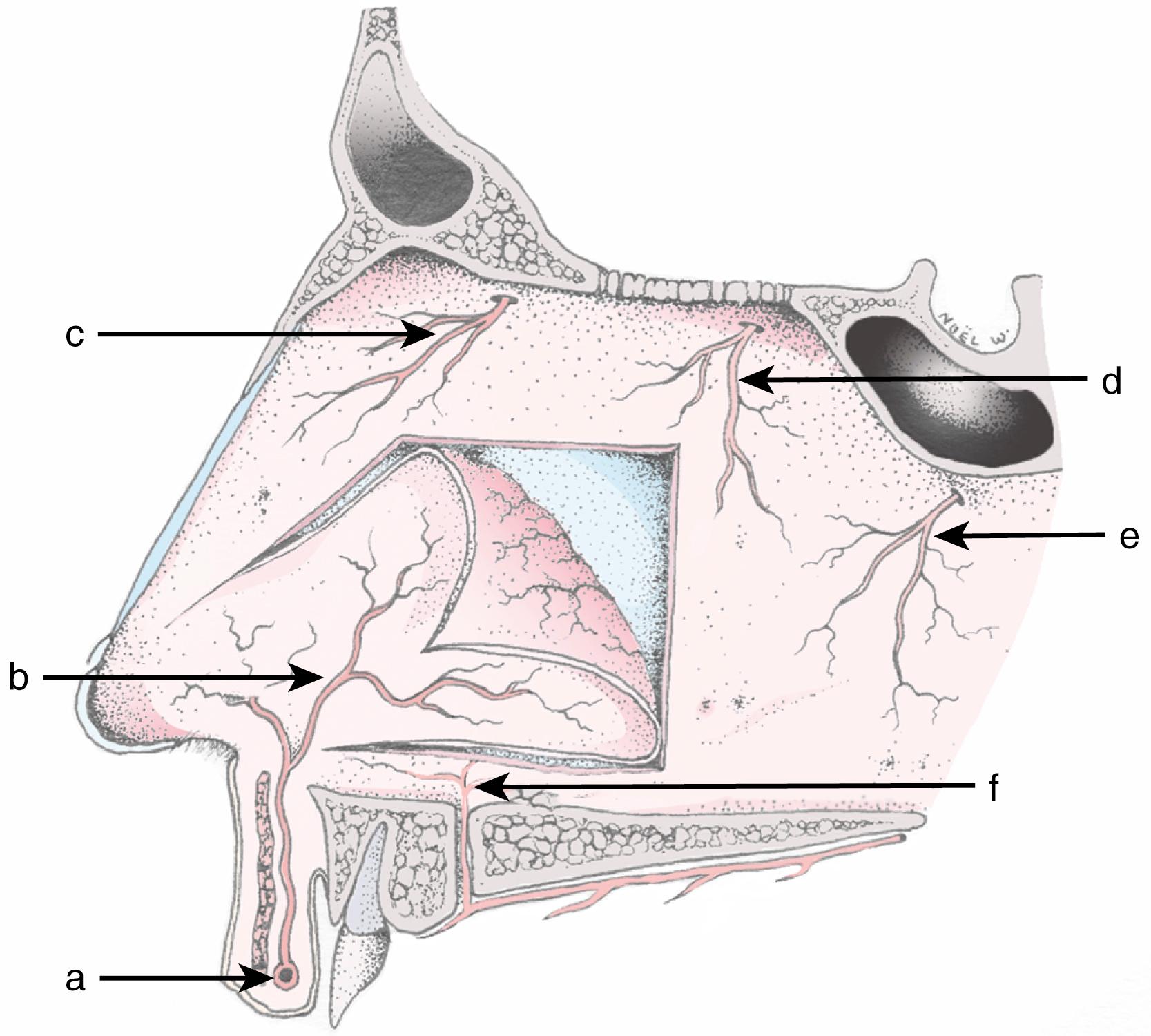
Sensation of the nose is provided by two divisions of the trigeminal nerve. The ophthalmic division (V 1 ) innervates the radix, rhinion, and cephalic portion of the nasal sidewalls, as well as the skin from dorsum to tip. The maxillary division (V 2 ) innervates the lateral tissue on the lower half of the nose as well as the lateral vestibule. The facial nerve supplies the muscles of the nose, specifically the nasalis, procerus, and depressor septi nasi.
The goals of nasal reconstruction are to optimize nasal esthetics while maintaining nasal function and airway patency. After a thorough presurgical evaluation of the patient, the extent of the nasal defect is defined by what tissue is missing. The reconstruction is then designed based on addressing all three layers to obtain a satisfactory outcome. In addition, the defect location will often dictate the best reconstructive option to achieve a satisfactory reconstruction.
To ensure a satisfactory reconstruction, complete patient evaluation must be undertaken. The general health of the patient must be considered, specifically the comorbidities that may limit the reconstructive options available to the surgeon. Health issues may limit the amount of surgical stages the patient can undertake, the type and duration of the anesthesia, materials that can be harvested from the patient, and techniques that can be applied to the problem.
The nasal wound is next examined with a focus on what is missing anatomically (e.g., cover, lining, or support). To obtain a complete understanding of the defect, it is beneficial to review the patient’s old photographs, take normative measurements, and in complex defects consider creating a facial moulage or model. The local and donor tissue are assessed for skin irregularities, overall skin quality, and any existing asymmetries.
When the reconstruction follows the oncologic resection, it is mandatory to confirm negative margins prior to undertaking a reconstruction. Frozen sections obtained at the time of resection risk may not identify residual tumor that will be detected on permanent pathology. If there is any question of the pathology the reconstruction should be delayed with dressing changes or allograft until final pathology results are available.
A functionally patent nasal airway and a good esthetic outcome are the basic reconstructive aims. These goals can be met by careful analysis of the defect and meticulous design of the flaps to reconstruct the defect. Often, the contralateral side of the nose is an ideal guide for planning reconstruction. Defect analysis determines the size, location, and thickness of the defect, as well as the quality and laxity of the remnant skin and lining. It is important to note that wound retraction, when present, will give the illusion of a smaller defect.
Nasal defects are categorized by their size, location, and depth. When a defect is less than 5 mm, it can often be closed primarily. Superficial defects with intact support structure and less than 1.5 cm in size can be reconstructed with skin grafts or local flaps. Larger defects, or defects involving the underlying cartilage, usually require reconstruction with interpolated flaps.
A three-layered reconstruction is often essential to successful reconstruction. The surgeon must consider the lining, support, and cover when planning nasal reconstruction. Each component must be repaired individually if involved in the defect. Overlooking a lining or cartilage loss because it is hidden by skin covering will lead to retraction, collapse that will result in distortion. The surgeon must also assess surrounding structures such as the cheek and lip. These must be reconstructed first, because aberrant surrounding structures will lead to an abnormal-appearing nose, even if the nose itself has a satisfactory reconstruction.
As described by Millard and modified by Burget and Menick, , the naturally lit ridges and shadowed valleys of the nose divide its surface into nine esthetic subunits (dorsum, sidewalls, alar lobules, soft triangles, columella, and tip that can be divided into two hemi‐tips) ( Fig. 30.2 ). Using the esthetic subunits during surgical planning allows for a logical approach to reconstruction that achieves a satisfactory esthetic result. The contralateral subunit may be used as a guide for reconstruction, and if the defect is large, it may be divided into multiple subunits using this principle. When reconstructing an esthetic subunit, the defect should be reconstructed with tissue of similar quantity and quality of the missing tissue. The subunit principle also endorses that when more than 50% of a unit is involved in the defect, the entire subunit is excised and reconstructed. This will position the scars between subunits, camouflaging them and minimizing contour distortion such as pincushioning or trapdoor contraction. ,
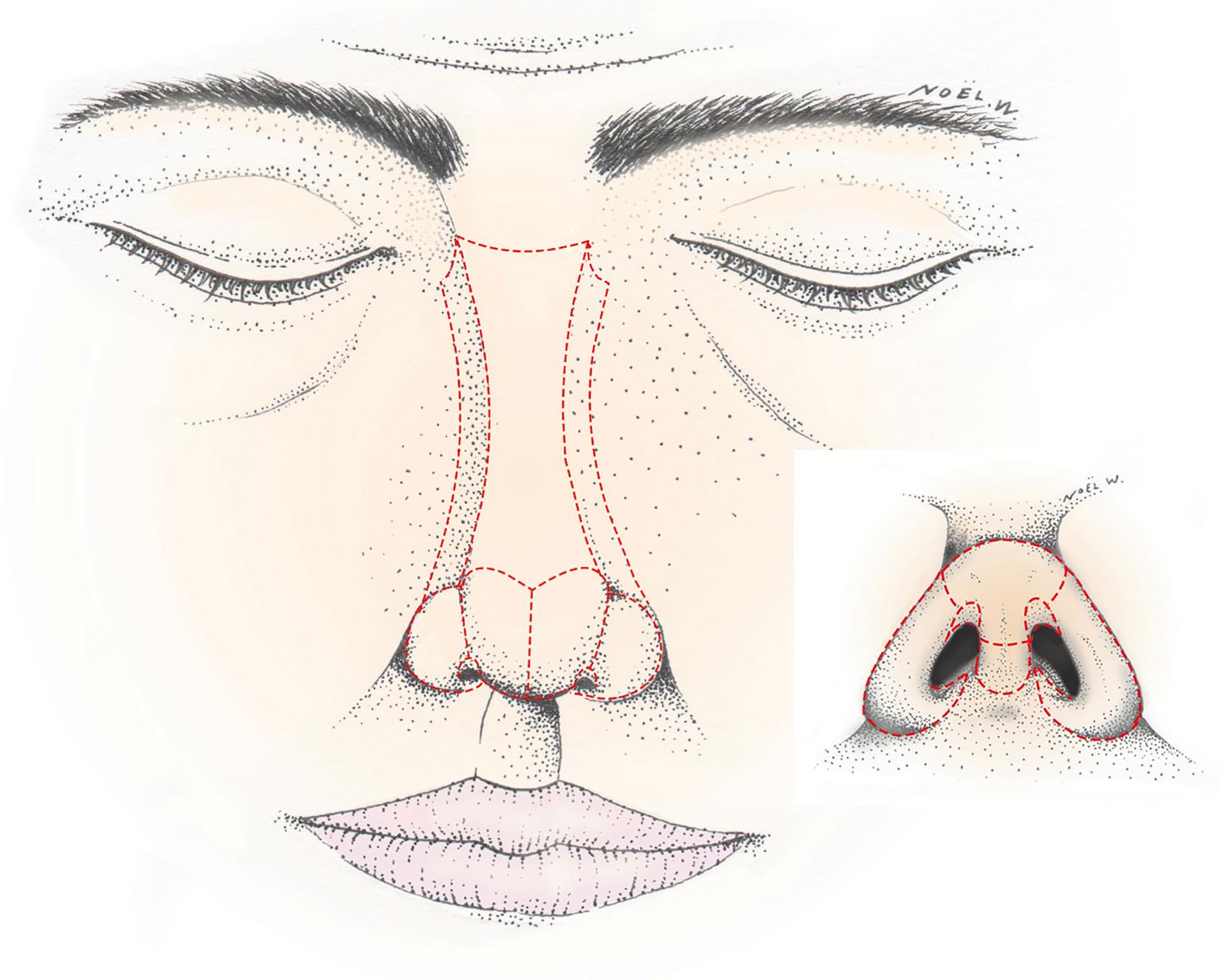
However, the subunit principle should not been seen as an absolute rule and even Menick, does not apply the subunit rule when reconstructing dorsal or sidewall defects. These areas have indistinct border outlines and are relatively flat surfaces, and as such the reconstructions can be limited to the defect alone. It has also been reported that in these areas skin grafts do not undergo trapdoor contraction. Other authors use the subunit principle as a guideline and often use defect-only reconstruction. In defect-only reconstruction, as described by Rohrich et al, the defect is reconstructed without excising healthy tissue in the subunit. These authors use adjunct procedures, such as dermabrasion, to improve the esthetic result and decrease the need for additional revisions.
Nasal defects can be classified into two groups: small superficial defects and large and/or full-thickness defects. The first group typically only requires skin replacement whereas the second will often necessitate a three-layered reconstruction consisting of inner lining, cartilage, and skin. Small and superficial defects entail the loss of skin and underlying subcutaneous fat or muscle that can be left to heal by secondary intention or repaired by direct closure, full-thickness grafts, or local skin flaps. These small and superficial defects can generally be repaired with a single-stage procedure.
All superficial defects on the nose, provided that they are well vascularized, will heal over time. For example, after rhinophyma excision, it is recommended to let the entire nose surface heal by secondary intention. Granulation tissue, epithelialization, and wound contracture will lead to a flat, thin, shiny, and atrophic scar initially. Thus, secondary intention is best suited to thin skin areas and flat or concave surfaces (upper two-thirds of the nose). Conversely, healing by secondary intention for defects encompassing adjacent landmarks or the alar rim would result in distortion of the shape and normal appearance of the nose.
Healing by secondary intention is best indicated on sidewalls (especially near the internal canthus) and dorsum defects. This method can also provide good results on the tip and in alar regions when the defect is small (less than 5 mm) and more than 8–10 mm away from the alar rim. The postoperative care is typically simple for the patient, and involves daily cleansing of the wound and moist dressing changes. Antibiotics or local antiseptic is rarely necessary.
Direct closure is often the best technique when certain that it will not distort the nasal landmarks or result in nostril margin retraction. Primary closure will generally leave an acceptable scar, especially when its axis is longitudinal and in the midline, or the defect is less than 5 mm. Undermining is often necessary in order to decrease tension.
Generally, direct closure is possible in wounds in the upper two-thirds of the nose where there is a slight excess of skin. Conversely, direct closure is not recommended on the ala, tip or columella, which are areas of poor skin laxity, as it would distort landmarks and retract the nostril.
Despite their often unpredictable final outcome, full-thickness skin grafts (FTSG) can be a useful tool in many cases, provided that the recipient bed is well vascularized. Avascular surfaces such as cartilage and bone cannot support a skin graft. Skin grafts can be considered in patients who have superficial defects less than 1 cm in size. Ideally, candidates for skin grafting would be nonsmokers in order to optimize the chances of graft take.
Immobility and direct contact with the recipient bed is vital. Quilting sutures and a tie-over bolster dressing using a petroleum gauze can aid in immobilizing skin grafts. Generally, the bolster is removed within 4–7 days, earlier if any signs of infection are noted. Depending on the wound’s depth, it can be employed as a full-thickness skin graft or as a composite graft if underlying soft tissue is carried with the skin. Skin grafts can provide good results in thin skin and flat areas such as dorsum, sidewall, and columella. Skin grafts are a poor match for defects in thick and sebaceous skin zones such as ala, tip, and supratip; however, when circumstances necessitate utilizing an FTSG to reconstruct these thick, sebaceous areas, McCluskey et al advocate using forehead skin, as this area has similar sun exposure and character to these sites. , If the inferior border of the defect involves the alar rim, an FTSG should be avoided, as alar notching can result.
Skin graft color match is one of the most challenging aspects of this type of reconstruction. The use of FTSGs often result in a patchwork appearance secondary to color mismatch and contour irregularities. This seems to be less prominent when it is performed in individuals with fair skin tone and with superficial defects involving the upper third of the nose. Preauricular, retroauricular, supraclavicular, and forehead skin are often the preferred donor sites. In order to optimize final contour and color match, dermabrasion can be utilized starting 6 weeks postoperatively.
Local skin flaps mobilize the slight excess of skin within the upper two-thirds of the nose and glabellar zone. Unlike skin grafts, the final color and texture of such flaps are predictable since the intrinsic blood supply of the raised skin is preserved. As they are also thicker than grafts, they can better supply missing subcutaneous tissue, but local skin flaps should be avoided when significant cartilaginous support is missing. In such cases, the reconstructed cartilage framework would most likely not resist the skin tension of a local flap and would risk losing its resistance and shape, leading to collapse and landmark distortion.
The dorsal nasal flap and bilobed flap, described below, should be used with caution during alar reconstruction, as they can have limited reach. If placed under tension, these local flaps can result in alar notching and blunting of the alar groove.
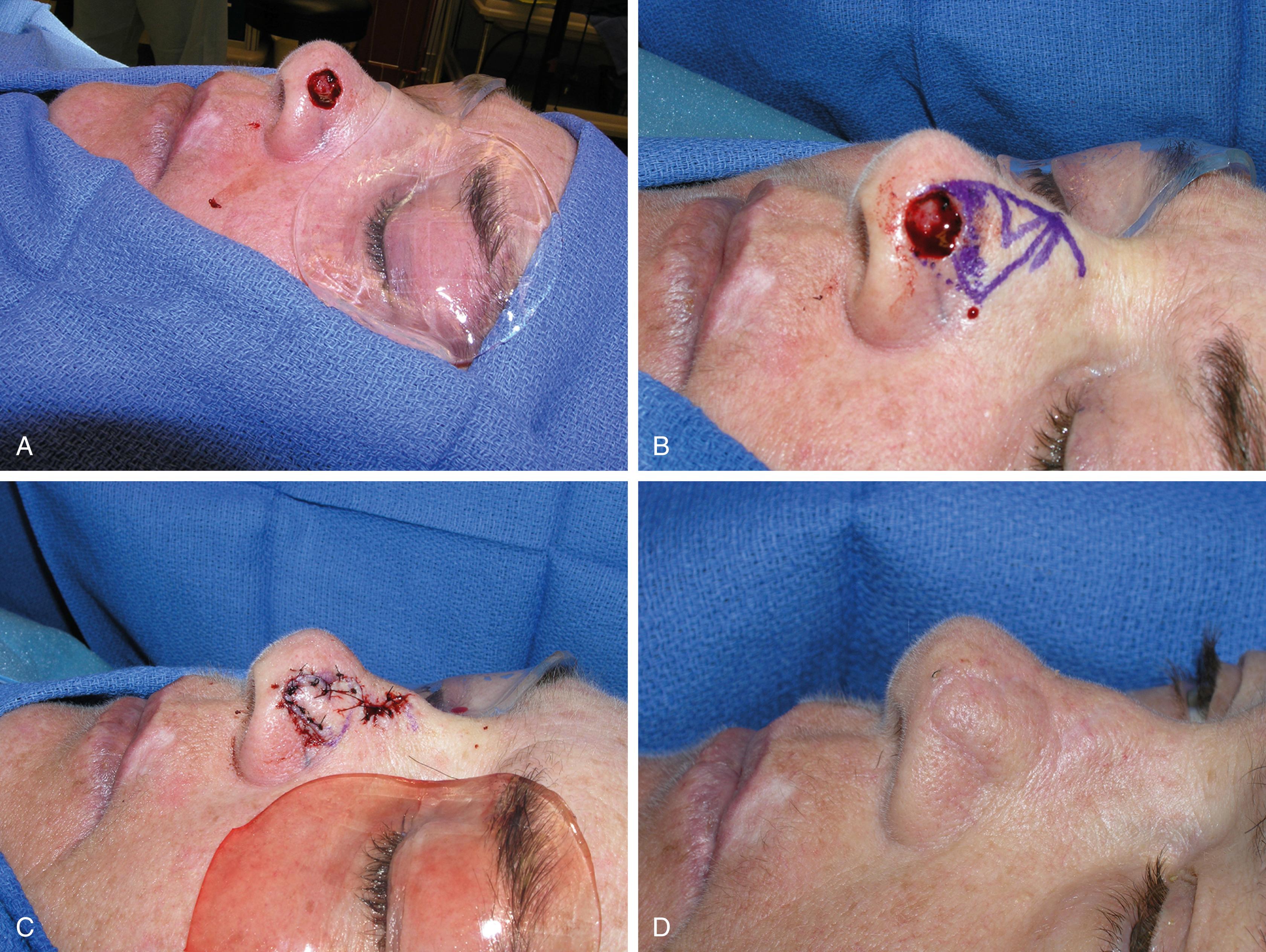
Described by Rieger in 1967, the dorsal nasal flap is vascularized by vessels of the sidewall and medial canthus. The skin, subcutaneous tissue and muscles of the upper two-thirds of the nose and glabellar area are elevated just above perichondrium and periosteum and mobilized toward the lower third of the nose. A dog-ear is excised inferiorly and the glabellar donor site is then closed with a V–Y closure ( Fig. 30.3 ). Mobilization of this flap can be increased by Marchac’s modification, which narrows the pedicle around the medial canthus zone with a counter-incision at the junction between cheek and sidewall.

The dorsal nasal flap is particularly suitable for nasal tip defects that are less than 2.5 cm, and where a forehead flap may be unsuitable or undesirable for the patient. When utilizing the dorsal nasal flap, the defect should be at least 1 cm away from the alar rim, as it tends to retract causing nasal tip and nostril margin displacement. It is also useful for upper third nasal defect ( Fig. 30.4 ). Additionally, this flap approximates the eyebrows and creates a radix fullness that often necessitates a revision.

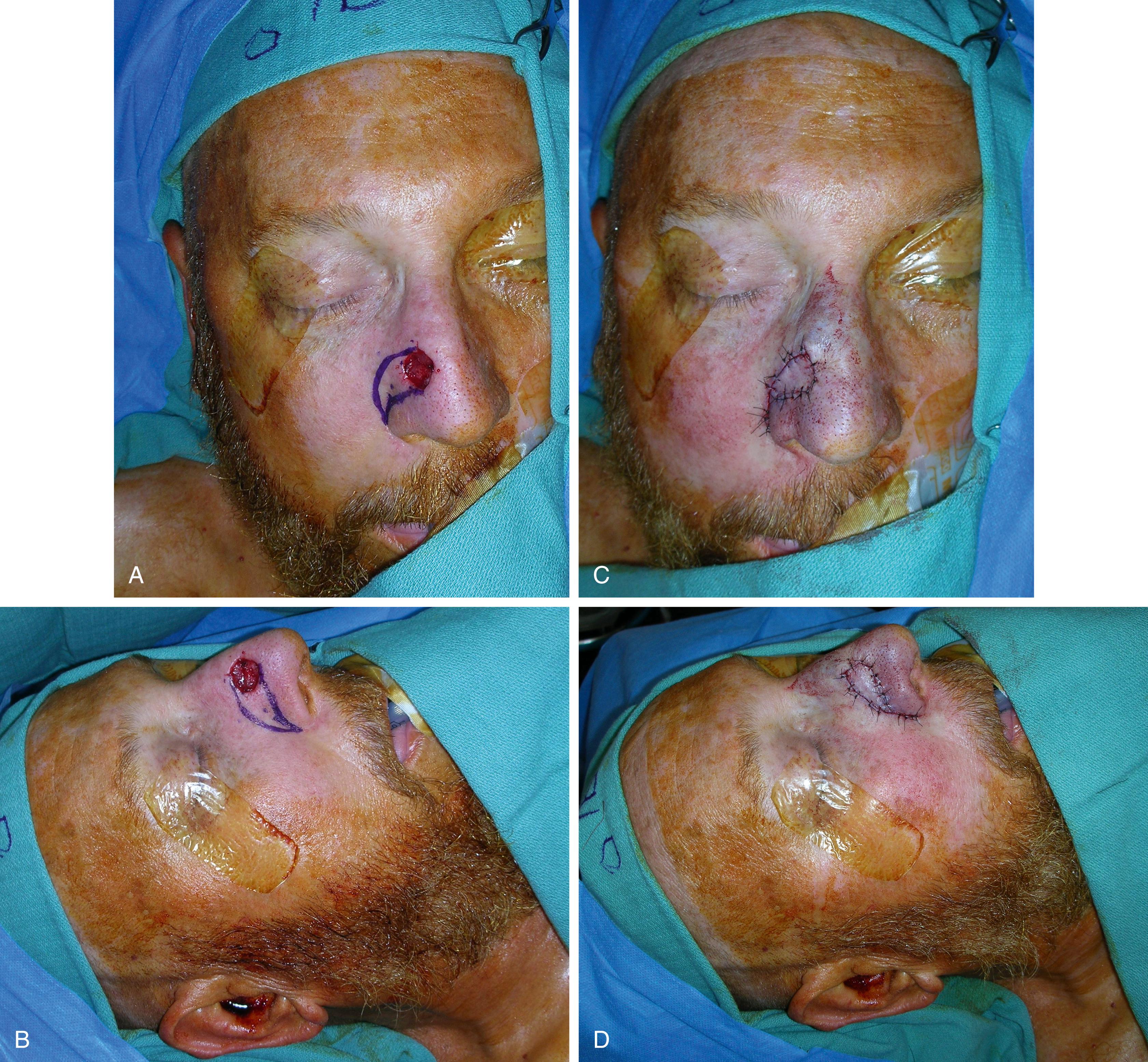
Zitelli’s bilobed flap is a double transposition flap widely used for defects up to 1.5 cm in diameter located within the lower third of the nose ( Fig. 30.5 ). This flap provides excellent skin and texture match, and is particularly suited for defects involving the ala with an intact alar rim, lateral tip, or supratip. In patients with nasal valve collapse secondary to loss of alar support, this flap can accommodate the use of a cartilage graft.
The first lobe is designed adjacent to the defect with the same diameter. The slightly smaller second lobe is designed adjacent to the first one, and has to lie in an area of laxity to allow its direct closure (upper two-thirds). The angle of transposition is approximately 45° for each lobe. In general, the flap is based laterally for tip and supratip defects and medially for alar defects. After resection of the inferior dog-ear between pivot point and defect, the flap is incised and elevated. Wide undermining of the defect borders, flap base, and donor site just above the perichondrium and periosteum facilitates transposition and minimizes distortion. The first lobe is then mobilized to cover the defect and the second lobe shifts to repair the defect created by the first lobe. This final defect is closed directly.
Though a useful single-stage local flap, the bilobed flap does have the disadvantage that it has a complex design, violates the esthetic subunit principle, and can potentially greatly distort the nasal tip and ala if not planned precisely. In addition, the flap often require a revision to treat pincushioning or irregular scars.
This flap can be designed in the nasal-alar groove and is often the first choice for reconstruction of the soft triangle and lateral portion of the nose. It does not lead to pincushioning or have the issues associated with a patterned flap. The defect is measured and a flap designed that has enough tissue to fill the defect and allow the closure of the V to a Y ( Fig. 30.6 ). Once designed, the flap is elevated down to the perforators (these can be identified with a hand-held Doppler). The perforators do not need to be skeletonized as this puts the flap at risk. It is then closed with deep dermal sutures and external nylon sutures.
Regional skin flaps mobilize skin of nearby units of the face from the glabellar and nasolabial area.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here