Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter was originally written by E. Burke Evans, MD. He passed away in May 2012. We are indebted to his knowledge of burn care. Care was taken to preserve as much of his original material while adding new information.
Burn injuries have a tendency, even as they heal, to create musculoskeletal deformity. In addition, the protracted burn illness that accompanies severe burns may result in other skeletal changes. Box 48.1 presents a classification of musculoskeletal changes secondary to burns; from this, the most commonly occurring and clinically significant alterations have been selected for discussion.
Alterations limited to bone
Osteoporosis
Periosteal new bone formation
Irregular ossification
Diaphyseal exostosis
Acromutilation of fingers
Pathological fracture
Osteomyelitis
Necrosis and tangential sequestration
Alterations involving pericapsular structures
Pericapsular calcification
Heterotopic paraarticular ossification
Osteophyte formation
Alterations involving the joint proper
Dislocation
Chondrolysis
Septic arthritis
Spontaneous dissolution
Ankylosis
Alterations involving muscles and tendons
Desiccation of tendons
Fibrosis of muscles
Alterations secondary to soft tissue
Muscle and joint contractures
Malposition of joints
Scoliosis
Soft tissue injury
Compartment syndrome
Nerve injury
Abnormalities of growth
Acceleration and retardation
Destruction of growth plates
Osteoporosis is the most frequently occurring postburn change involving bone. Klein et al.'s ongoing studies suggest that, among persons with serious burns, reduction of bone mass density is pervasive. Stated causes of osteoporosis in thermal burns are bed confinement, immobilization, hyperemia, reflex vasomotor phenomena, and adrenocortical hyperactivity. In Chapter 26 of this book, Klein reviews the effects of burn injury on bone metabolism. Klein et al. noted very limited bone formation after a severe burn. Other endocrine changes that lead to loss of bone after burns have been described by Dolecek et al. This coupled with the relatively high resorption leads to osteopenia postburn. Endogenous corticosteroid production is likely responsible for the decreased bone formation, and inflammatory cytokines are responsible for the bone resorption. In this section, only what is clinically apparent is discussed.
The more extensive the burn and the greater the number of complications, the longer the patient may be confined to bed and relatively immobile. The onset of osteoporosis is accelerated, and its intensity is more marked in the burn illness that features a hypermetabolic state. Klein et al. found that osteoblasts and probably osteocytes underwent apoptosis in response to the glucocorticoid stress hormones. The overall effect of burn is catabolic, and muscle wasting is also noted. If a single extremity of an otherwise normal person is immobilized for a long period of time because of local trauma, as with a fracture, loss of bone density can be easily seen on plain radiographs. So, with burns isolated to the extremities, the bones of affected extremities become osteoporotic, and in persons with generalized burns, the bones of deeply burned extremities may show more profound mineral loss than is observed in nonburned extremities or in the axial skeleton ( Fig. 48.1 ). This tendency for more osteoporosis in severe burns was also noted by Pandit et al., who found that 56% of postburn patients had radiographic evidence of osteopenia. Van der Wiel et al. found in an X-ray absorptiometry study of 16 adults with fractures of one tibia that there was eventual loss of bone mineral density in the contralateral femur and in the lumbar spine but to a lesser degree than in the ipsilateral femur. These findings, although not strictly analogous to those observed in burns, nevertheless point to the occurrence of generalized osteoporosis in other trauma states and the difference in loss of bone density relative to local factors. In fractures or in burns, impaired mobility and local hyperemia could account for this difference.
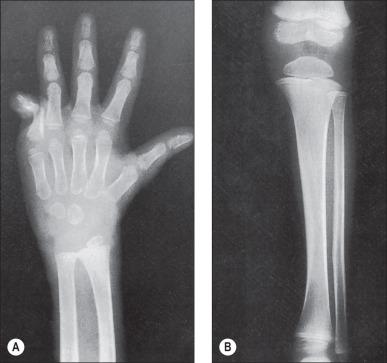
Another characteristic of the osteoporosis of burns that seems to set it apart is its persistence, not just until restoration of the anabolic state but also for months and years after the burn has healed ( Fig. 48.2 ). This phenomenon may be most clearly observed in patients who have survived 90% burns, but Klein et al. record less than normal bone among even moderately burned children as long as 17 months after injury. Muscle atrophy or the failure or inability of the person to return to the preburn level of physical activity may account in part for this protracted state of reduced bone mineralization.
There is no way to prevent osteoporosis in a patient whose burn is of such severity as to require an extended period of bed confinement. Methods of medical treatment described by Klein and Rousseau et al. include anabolic hormones, bisphosphonates, and cholecalciferol. Cholecalciferol was noted to have a positive effect on muscle health but little effect on bone. The advance of bone atrophy can at least be favorably modified even among patients with large burns if mobilization and active exercise are initiated soon after the burn. The bones of the axial skeleton, the pelvis, and the lower extremities are most efficiently stressed by weight bearing. Thus, standing is a priority measure, and it is common practice now to walk patients to tolerance before permanent wound cover. Muscle contraction alone may help forestall bone atrophy, and bone is better stressed if the contraction is resisted. Isometric muscle contraction is possible from even extensively burned patients and is important for bone stress and for maintaining muscle tone and muscle. Passive motion has no effect on bone and thus does not figure in the prevention of osteoporosis. Other preventive measures, such as closure of the wound and maintenance of nutrition, are routine in critical burn care. Treatment of established osteoporosis involves the more aggressive use of measures for prevention. There are no long-term comparative studies, however, that persuasively measure the effectiveness of exercise, diet, medication, or modality in the treatment of osteoporosis in any state. Thus, osteoporosis can be lessened by active muscle contraction and weight bearing. Medical treatments that show promise include anabolic hormones, bisphosphonates, and possibly cholecalciferol.
In burns, bones can become infected by exposure of bone by the burn, by an open fracture accompanying the burn, by extension of infection from a septic joint, by introduction of organisms along traction pins or internal fracture fixation devices, or by bloodborne organisms of bacteremia. Considering the apparent risk for seriously burned patients to develop osteomyelitis, it is surprising that it does not occur more regularly. Clinically significant osteomyelitis in burned patients is uncommon. Antibiotics given for the general state may prevent seeding of the bone or may repress any small focus of bone infection.
The cortex of long bones is a good barrier to surface organisms. Even exposure of cortex will have little adverse effect if the blood supply of the bone remains intact. Prolonged exposure will kill the outer layer of the cortex, which will in time sequestrate, separating at a well-defined fissure between dead and living bone. With minor or moderate exposure, the bone will usually survive long enough for bordering granulation tissue to cover it. For large defects, it may be useful to drill closely spaced holes through the exposed cortex so as to encourage buds of granulation tissue to emerge from the still vascular medullary canal. Another way to encourage granulation tissue formation over exposed bone is with superficial decortication with an osteotome or burr to expose the capillaries of the inner cortex. With these practices, there is little risk for infecting the bone. It may be that there is sufficient centripetal pressure to discourage the invasion of organisms when the holes are fresh and that the holes are rapidly sealed by blood clot and advancing tissue. There are no reports of deep bone infection related to cortex drilling.
With open fractures at the site of a major soft tissue burn wound, bone infection is probably inevitable. These infections can often remain localized to the fracture site and not involve the rest of the bone. Local debridement and stabilization of the soft tissue wound are all that are required for treatment. Dowling et al. reported osteomyelitis of the tibia related to an open bimalleolar fracture in an extensively burned extremity. English and Carmichael showed three cases of osteomyelitis out of 28 fractures, and all were found in open fractures. On the other hand, osteomyelitis developed in neither of the two open fractures reported separately by Choctaw et al. and Wang et al. We treated three patients in whom open fractures of the femur complicated thigh burns. Each case required aggressive and repeated debridement. One fracture was treated in traction, and the other two were treated with external fixators. In one of the patients, who was admitted 8 months after acute burn, there was established osteomyelitis of the femur in relation to the exposed fracture. Osteomyelitis did not develop in either of the other patients; in the end, all three had sound femurs.
When traction pins are directed through burned skin for the treatment of fractures or for suspension of a burned extremity, the factors favoring development of infection along the pin track and the formation of cigarette sequestra are:
The introduction or migration of organisms from the burn wound
Thermal necrosis during introduction of the pins
Linear pressure of the traction pin
Prolonged traction
Excessive movement of the extremity leading to loosening of the pin
Sealing of the skin of the pin sites.
For traction or suspension, pins may be inserted through acutely burned skin, through eschar, through granulation tissue, or later through ischemic burn scar, which may be colonized with uncommon and antibiotic-resistant organisms. No amount of local cleaning is likely to sterilize the surface through which the pin must pass, yet it seems that organisms in sufficient numbers to colonize and infect are rarely introduced in this manner.
Local low-grade infections usually resolve when pins are removed if the pin sites are vigorously curetted of granulation tissue. In one case in which a four-pin custom external fixator was used in the treatment of an open infection of the elbow, diffuse osteomyelitis of the humerus and radius resulted. The infection was controlled with antibiotics and without surgery after the pins were removed. This case was included in Barret et al.'s report of skeletal pinning in 41 severely burned children. In experience with the Ilizarov system for correction of skeletal deformity in burns, one patient developed a pin track infection of such severity as to require removal of the pin, curettage, and intravenous antibiotics for control of meticillin-resistant Staphylococcus spp. In an ongoing yet unpublished study, we treated nine patients with open joints in external fixation for an average of 7.1 weeks, and none of them developed pin tract infections or osteomyelitis. The open joints were treated in joint-spanning external fixators. Most patients had multiple failed skin grafting procedures before fixator placement. The fixators were thought to have decreased the need for additional skin grafting.
Hematogenous osteomyelitis and that caused by spread from an infected joint are rare. There is no report of the occurrence of either entity in association with burns. If bone infection of this sort were be recognized, effective treatment would depend on the identification of the offending organisms for organism-specific antibiotic regimens.
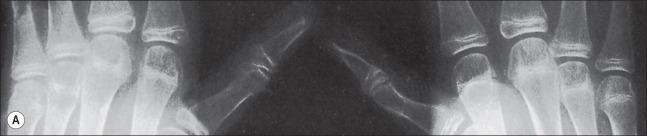
Pathological fractures were at one time common in burn management because of the practice of delayed excision of eschar and of keeping patients in bed until wounds were completely covered. During that time, fractures occurred because of bone collapse when patients first stood or walked or when stiff joints were manipulated ( Fig. 48.3 ). The bones most commonly affected were the femur at its distal metaphysis and the tibia at its proximal one. The only treatment required was support of the extremity until the fracture consolidated, usually in 4–6 weeks. Children were more often affected than adults, and the fractures usually compressed one cortex, producing an angular deformity that rapidly corrected with growth. Klein et al.'s study strongly suggests that fractures occur more frequently in burned children than in a matched normal population even months after the acute burn. Now, however, in acute burn management, the most frequently seen fractures are those occurring at the time of, or in association with, the burn injury. Falls or violent trauma account for many of the fractures, and the sites are those common to the causes, bearing no relation to the burn itself.

Although fractures complicate burn treatment and occasionally delay mobilization of patients, their management need not be complex. Fractures in extremities not burned can be treated by manipulative reduction and cast immobilization, by open reduction and fixation, with an external fixator, or with skeletal traction ( Fig. 48.4 ). Fractures in extremities with first-degree or superficial second-degree burns can be managed in the same way. Deep second- and third-degree burns present a different problem only with respect to the early bacterial colonization of third-degree burns and the degradation of deep second-degree burns to full-thickness burns that will in turn become colonized. There is a precious window of time when fractures requiring open reduction and internal fixation (ORIF) can be definitively treated without increased risk for infecting the bone; however, fracture reduction and stabilization are so important in the functional management of a severely burned patient that the risk for bone infection should be acknowledged and shouldered at any postburn stage. English and Carmichael showed that if fractures were treated with open reductions within the first 48 hours postburn, the risk of infection is minimal. Therefore, early stabilization is encouraged in the first 48 hours before the risk of infection increases. Skeletal traction is used infrequently today. The disadvantages of skeletal traction are the confinement to bed and the imposed relatively fixed position of the affected extremity. External fixators make it possible to align and stabilize fractures in burned extremities without open operation and provide mobility to the patient. Brooker's extensive favorable experience supports this concept. With both skeletal traction and external fixation, there is an added risk for bone infection because of the path from surface to bone provided by the pins. Pin tract infections can be minimized by scrupulous pin site care and by removal and replacement of any loosening pins. Frye and Luterman recognized and discussed the specific and continuous difficulties encountered in the management of fractures and burns.

When casts are used for stabilization of fractures in burned extremities, the wound is made inaccessible, and there is an abiding fear that the unattended wound will seriously degrade or at best not improve. Such fear may be well founded; however, Wang et al. showed that a bivalved circular cast could be used effectively for an open comminuted fracture of a proximal tibia with overlying deep burns, and Choctaw et al. reported successful use of a cast for immobilization of an open comminuted fracture after immediate postburn grafting of the affected extremity. Common sense should dictate which fractures can be treated with circular or bivalved casts or with splints. If casts are used over burn skin, they would need to be removable to allow burn care. If a reduced or moderately displaced but aligned fracture is so stable as to require external support only for maintenance of alignment, then cast or splint immobilization should be all that is needed. On the other hand, if a fracture, because of instability, requires maintenance of reduction by three-point pressure or molding of the cast material, it will be better treated by other means.
English and Carmichael had 28 fractures that were treated over a 20-year span. In that study, 22 of 24 fractures available for long-term review healed in appropriate time. There were five infections noted, including two superficial pin tract infections from external fixation and three cases of osteomyelitis, all of which were open fractures. In contrast, there were no infections among Saffle's 42 fractures, nine of which were treated by ORIF. With two fractures of the femur, each of which was exposed at the base of a deep chronic burn, aggressive debridement of the wounds and the fracture ends was followed by treatment with skeletal traction in one and by external fixation with the Ilizarov system in the other. Both fractures healed without further complication. Coverage of exposed bone can be done with skin grafts, local flaps, and free flaps. Burring of the exposed bone to stimulate bleeding and induce granulation tissue can be used alone or with other procedures to help cover exposed bone. Newer techniques using graft substitute have shown promise in coverage of exposed bones in burn patients.
Among severely burned patients, nondisplaced or minimally displaced fractures may not be detected until unusual local pain in an affected extremity prompts radiographic examination. A radiograph obtained for other reasons may reveal a fracture as an incidental finding. These fractures are usually of no functional significance. Modest angular deformity near a joint is more of a problem in adults than in children who still have remodeling potential. Undetected transphyseal fractures in children can be a major functional threat, however.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here