Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Superficial inguinal lymph nodes targeted for harvest lie between the groin crease and inguinal ligament.
The vascular supply of these nodes is typically the superficial circumflex iliac artery.
These nodes typically drain the lower abdomen; however, there are exceptions and in certain cases may contribute to drainage of the lower limb.
Reverse lymphatic mapping (RLM) is a technique that allows the surgeon to identify the physiologic drainage pathways of lymph nodes.
RLM is used to differentiate the lymph nodes that drain the extremity from the lymph nodes that drain the trunk.
RLM can identify lymph nodes in the groin that contribute significantly to lower limb drainage, allowing the surgeon to avoid these nodes or select an alternative donor site, which may minimize the risk for donor site lymphedema.
Vascularized lymph node transfer (VLNT) has steadily been gaining popularity in the treatment of lymphedema as increasing reports of success across multiple centers have surfaced. The concept of a free flap containing vascularized lymph nodes is appealing to many microsurgeons because standard microsurgical techniques seem to be readily applicable to VLNT. However, familiarity with standard free flap harvest and anastomosis is where the similarities between a deep inferior epigastric perforator flap and a vascularized groin lymph node flap quickly fade. The potential for donor site lymphedema and permanent additional disability for the patient makes VLNT a far more technically challenging and stressful procedure. The relative lack of literature on the specifics of anatomy, lymphatic drainage pathways in the groin, and surgical technique is a barrier to using this technique. However, a significant number of patients have had both objective and subjective improvement across multiple centers following VLNT, giving enough credence to this technique to lead to further time and investment in research in this area. Addressing the primary concern of causing donor site lymphedema, the authors have described the technique of reverse lymphatic mapping (RLM) in VLNT to identify which nodes are draining the limb and which nodes are draining the trunk, in order to precisely harvest lymph nodes with the least risk of causing lymphedema at the donor site. An anatomic study of this region using magnetic resonance angiography (MRA) and mapping of nearly 2000 lymph nodes previously published by the authors has clarified the anatomy of this region and has contributed to the evolution of the technique we present in this chapter. Future long-term prospective studies will further refine the indications and allow us to better understand the risk/benefit equation for VLNT. The purpose of this chapter is to describe our surgical technique for vascularized groin lymph node transfer utilizing RLM.
The vascular pedicle for the vascularized groin lymph node flap is commonly based on the superficial circumflex iliac artery (SCIA). This artery originates from the common femoral artery, where it makes a short hairpin turn superiorly and laterally as it nearly parallels the course of the inguinal ligament. The flap is drained from both venae commitantes as well as the superficial circumflex iliac vein (SCIV) and, to some degree, the superficial inferior epigastric vein (SIEV). The SCIV and SIEV join and continue to inferiorly diverge from the SCIA and empty into the saphenous bulb near the junction of the greater saphenous vein and the femoral vein.
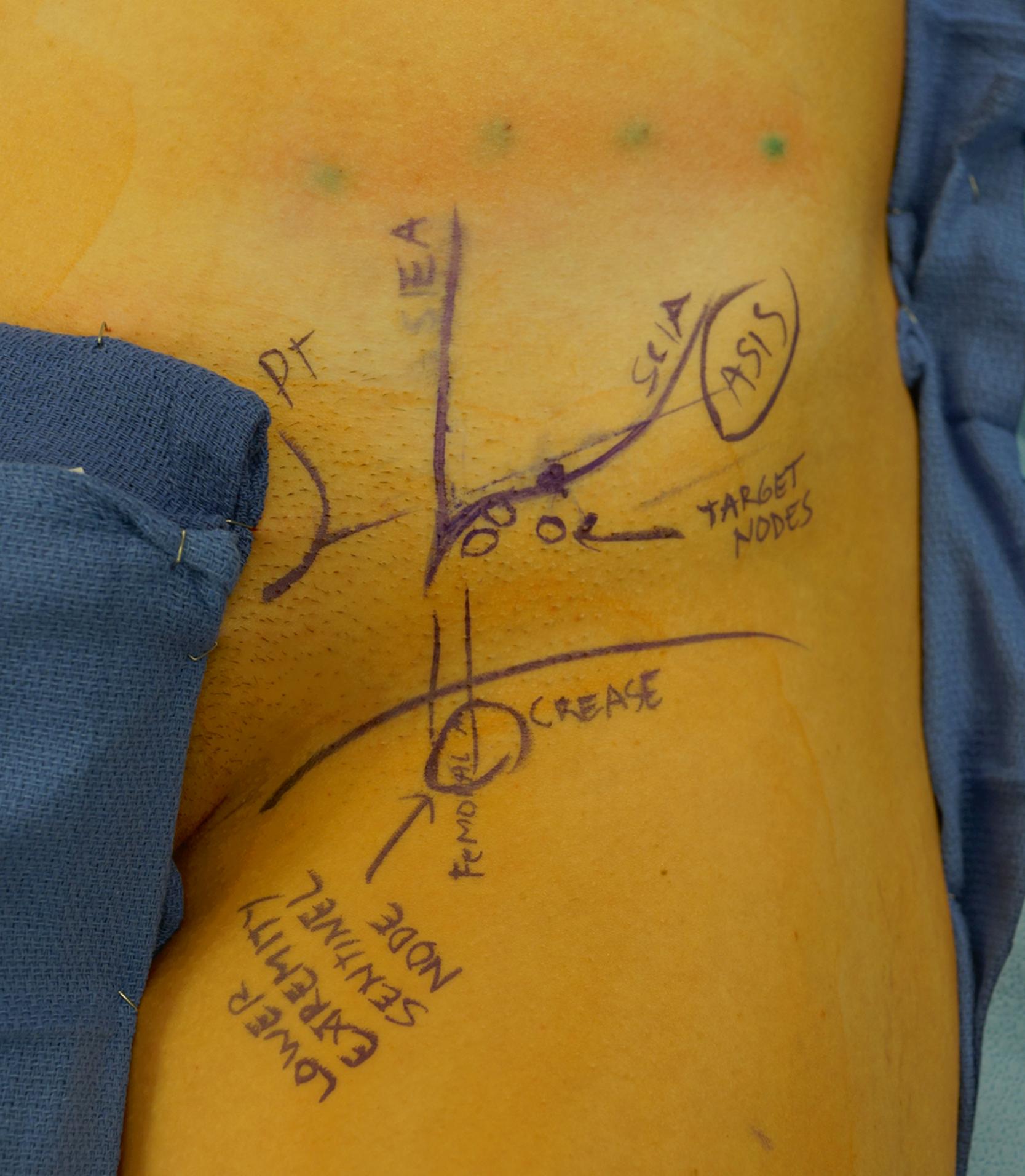
The lymph nodes supplied by the SCIA are concentrated at the junction of the SCIV and SIEV, based on a published anatomic study by the authors. This correlates to a region one-third the distance from the pubic tubercle to the anterior superior iliac spine (ASIS) and 3 cm perpendicularly below this point. These lymph nodes are almost always located above the groin crease but below the inguinal ligament—never below the groin crease. Lymph nodes located below the groin crease typically contribute significantly to drainage of the lower limb, and the sentinel lymph nodes draining the lower limb are commonly along the femoral vessels just below or at the groin crease. Lymph nodes medial to the SIEV may also contribute to lower extremity drainage and may need to be avoided as well. These are solely static anatomic guidelines, not rules, and the physiologic drainage in each individual patient can vary and should be assessed by RLM. In some cases, there are lymph nodes above the groin crease that contribute significantly to lower extremity drainage.
There are also sensory nerves in the operative field: direct branches from the femoral nerve and the lateral femoral cutaneous nerve. Femoral nerve branches may entangle the pedicle, and sacrifice may lead to numbness in the anterior thigh. The lateral femoral cutaneous nerve runs medial to the ASIS and deep to the abdominal wall fascia at this level and is typically not seen during flap harvest.
Anatomic landmarks are marked first: a line is drawn from the pubic tubercle and ASIS corresponding to the inguinal ligament. The natural groin crease is marked, the femoral artery is palpated and marked, and the sartorius muscle border is marked. The femoral triangle becomes easily apparent and is the origin of the pedicle. We typically utilize the groin flap as a buried flap without a skin paddle for transfer to the axilla in upper extremity lymphedema. In this case, the incision is planned over the course of the SCIA, which can be localized with a handheld Doppler and/or by using anatomic landmarks: the SCIA courses obliquely approximately 3 cm below the inguinal ligament, but always above the groin crease ( Fig. 19.1 ). Incision length depends on the amount of soft tissue desired. If there is a large axillary dead space following extensive scar excision, the incision can be extended laterally to create an appropriately larger flap. The flap width is limited inferiorly by the groin crease but can be extended superiorly as needed. A typical flap dimension is 5×10 or 5×12 cm. If a distal transfer is planned to the forearm or wrist, the skin paddle is oriented so that the course of the SCIA is centered within it.
Patients who have a history of lower extremity lymphedema, a history of pelvic radiation or oncologic surgery, or any predisposing factor for developing lower limb lymphedema may not be a candidate for a vascularized groin lymph node transfer. In our practice, patients with a body mass index greater than 32 are generally not operated on until body weight is optimized. Patients who have severe venous insufficiency that cannot be treated may also not be good candidates for lymph node transfer. A reflux Duplex ultrasound can assess for venous insufficiency if there is any question. Elevated venous pressures may compromise the hypothesis of the lympho-venous shunting that occurs at the level of the lymph node. An ideal patient would be someone who is thin, healthy, and compliant, with significant pitting edema. This confirms that there is a large fluid component (as opposed to hypertrophic fat) in the patient's affected limb, which may respond more to a lymph node transfer.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here