Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The crucial roles of the menisci in the human knee are well understood and include load bearing, load transmission, shock absorption, knee joint stability, and lubrication and nutrition of articular cartilage. Meniscectomy frequently leads to irreparable joint damage, including articular cartilage degeneration, flattening of articular surfaces, and subchondral bone sclerosis. Poor long-term clinical results have been reported by many investigators following partial and total meniscectomy. For instance, Scheller and coworkers followed 75 patients who underwent partial lateral meniscectomy 5 to 15 years postoperatively and noted that 78% had Fairbank's signs of radiographic deterioration. Rockborn and Messner reported a 50% rate of radiographic osteoarthritis in 30 patients a mean of 13 years after meniscectomy. Roos and associates found that 48% of 107 patients had advanced radiographic osteoarthritis compared with a control group 21 years after meniscectomy. These authors reported that the relative risk of developing advanced degenerative radiographic changes was 14.0. It is important to note that some problems exist in meniscectomy natural history studies, such as including both partial and total meniscectomy in the same cohort; not assessing the effects of patient body weight, activity level, and overall lower limb alignment on the functional result; failure to include weight-bearing posteroanterior (PA) radiographs in the assessment; and lack of a carefully defined control group for comparison.
At least half of patients who sustain injuries to the anterior cruciate ligament (ACL) also sustain meniscus tears, which is markedly concerning because well over 1 million ACL injuries occur yearly worldwide. We conducted a systematic review to determine the treatment of meniscus tears during ACL reconstruction based on studies published from 2001 to 2011. There were 11,711 meniscus tears in 159 investigations, of which 65% were treated by meniscectomy, 26% were treated by repair, and 9% were left in situ. These results were distressing because the majority of patients in the studies were young athletes in whom resection of meniscal tissue may accelerate the development of osteoarthritis, regardless of the outcome of the ACL reconstruction. This study included investigations from 16 different countries, approximately one third of which were from the United States.
In comparing the incidence of meniscectomy and meniscus repair just within the United States between the years 2005 and 2011, Abrams and colleagues reported that the incidence of meniscus repairs increased 11% in isolated cases and 48% when a concomitant ACL reconstruction was performed. Approximately half of these repairs were done in patients younger than 25 years, and 20% were done in individuals ages 25 to 34 years. These authors attributed the increase in the attempt to preserve meniscal tissue to improved surgeon education, arthroscopic techniques, meniscus-specific rehabilitation protocols, and an overall comfort level with the procedure.
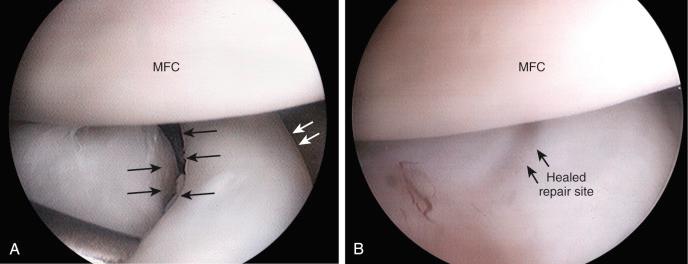
Several studies have reported superior results of meniscus repair compared directly with meniscectomy. In addition, our recent systematic review that encompassed 1326 meniscus repairs for tears in the central third region found an overall clinical healing rate of 83%. The repairs in this review were performed with either newer flexible suture-based all-inside suture devices or the traditional inside-out technique. It is well known that complications and deteriorating results have occurred with rigid all-inside meniscus fixation devices such as meniscal arrows, screws, and darts. More recently, flexible all-inside devices have become commercially available that contain anchors attached to suture that are passed into the periphery of the meniscus. These devices include:
Ultra Fast-Fix (Smith & Nephew, Andover, MA)
RapidLoc (DePuy-Mitek, Raynham, MA)
OmniSpan (DePuy-Mitek)
Meniscal Cinch (Arthrex, Naples, FL)
Sequent (ConMed Linvatec, Largo, FL)
MaxFire (Biomet, Warsaw, IN)
NovoStitch (Ceterix Orthopaedics, Menlo Park, CA)
The lack of long-term, prospective, randomized level I clinical studies precludes definitive recommendations for these devices ; however, the short-term clinical outcomes achieved in mostly single longitudinal meniscus repairs found in our systematic review were encouraging. This chapter focuses on surgical techniques using newer all-inside suture devices and inside-out repair procedures for a variety of meniscus tears and published clinical outcomes. The postoperative rehabilitation program is described in detail in Chapter 25 .
Candidates for meniscal repair are active patients younger than 60 years, including skeletally immature children and adolescents. Trauma during sports activities involving sudden twisting and turning is one of the most common etiologies of meniscus tears. Many meniscus tears that occur during ACL injuries extend into the middle third avascular region and are amendable to a meticulous inside-out suture repair. Magnetic resonance imaging (MRI) provides important information regarding the type of meniscus tear and potential for repair to preserve function. In knees in which repair is deemed possible, it is important to restrict strenuous activities and athletics until surgery to avoid further damage to the joint and meniscus.
Meniscus tear with tibiofemoral joint line pain
Active patient younger than 60 years
Concurrent knee ligament reconstruction or osteotomy
Meniscus tear reducible, good tissue integrity, normal position in the joint once repaired
Meniscus tear classified by location, type of tear, integrity, damage to meniscus tissue, remaining meniscus bed
Peripheral single longitudinal tears: R/R, one plane: repairable in all cases, high success rates
Middle third region: R/W (vascular supply present) or W/W (no blood supply)
Outer third and middle third regions longitudinal, radial, horizontal tears: R/W, one plane: often repairable
Outer third and middle third regions complex double or triple longitudinal, flap tears: R/W, multiple planes: repair versus excision
Degenerative meniscus tears are much less frequently repaired because the meniscus tissue is poor in quality and often fragmented into multiple pieces. Occasionally, MRI will indicate that a repair may be possible, such as in cases of large horizontal tears. Frequently, the symptoms of tibiofemoral pain will diminish over 6 to 12 weeks in degenerative tears in older patients, allowing a conservative approach. In other knees, symptoms of locking episodes and joint swelling are more persistent or severe and require arthroscopic intervention.
Meniscus repair is frequently performed with concurrent operative procedures such as knee ligament reconstruction. Patients with lower extremity varus or valgus malalignment and associated meniscus tears are especially considered for meniscus repair. The malalignment produces high medial or lateral tibiofemoral compartment loads, and a functional meniscus is required to prevent articular cartilage deterioration. Unfortunately, many meniscus tears in varus- or valgus-aligned limbs are degenerative in nature and not repairable.
Candidates for meniscus repair must be compliant and willing to follow the postoperative program of rehabilitation, including crutch support for 4 weeks. Those in whom complex tears are repaired must agree to avoid strenuous activities and deep knee flexion for 4 to 6 months; otherwise, the repair site may be disrupted and fail.
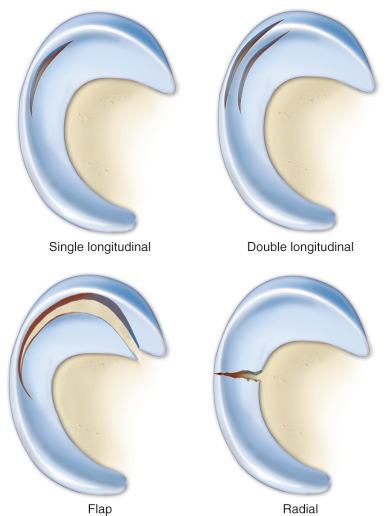
Meniscus tears are classified according to location, type of tear, and integrity and damage to meniscal tissue and the meniscus attachment sites. This classification, along with meticulous arthroscopic inspection of the tear site, allows the surgeon to determine whether a tear is repairable. The meniscus body is divided into anterior, mid body, and posterior thirds. In addition, Anderson and associates recommended a classification system of zone 1 (rim width <3 mm), zone 2 (rim width 3-4 mm), and zone 3 (rim width >5 mm). Tears located at the peripheral attachment sites (meniscofemoral and meniscotibial), or zone 1, are referred to as outer third or red-red (R/R) tears. Single longitudinal tears are usually located in this region ( Fig. 23-1 ). These tears are classified as R/R because both portions have an internal blood supply and are repaired in all cases with high success rates expected.
Tears located in the middle third region (zone 2) are classified as red-white (R/W), and tears located in the inner third (zone 3) are termed white-white (W/W). R/W tears occur at the junction between the outer and middle third regions, approximately 4 mm from the meniscal attachment, with a vascular supply present predominately in the outer third of the tear. White-white tears are located in the region in which no blood supply exists to either portion of the tear. When a repair is performed for these tears, the sutures may provide access to the vascular supply. In addition, rasping of the meniscus-synovial border provides a vascular supply to the repair site from synovial migration of cells on the surface of the meniscus. It should also be noted that the vascular supply to the meniscus, particularly in younger patients, still requires study and may extend greater than 5 mm in depth into the central zone.
Repairs of complex tears and tears that extend into the middle third region are evaluated on an individual basis. Tear patterns in this region include single longitudinal, double longitudinal, triple longitudinal, horizontal, radial, and flap. The rationale for repair of these tears is that removal results in essentially a total meniscectomy because a substantial amount of meniscal tissue is resected ( Fig. 23-2 ). This is especially concerning in younger patients in their second to fourth decades of life and all athletically active individuals. These tears are often repairable with reasonable success rates, as described later in this chapter.
Single meniscal tears occur in a single plane, regardless of location. These include longitudinal, radial, and horizontal tears. These tears are most commonly found in the posterior horn and are usually repairable. Complex tears occur in more than one plane or direction. These include tears in the vertical plane (double or triple longitudinal), in the vertical and horizontal planes, or in the vertical and radial planes (flap tears). Each component of the tear is identified and may or may not be repairable.
The decision for repair is based on the qualitative evaluation of the meniscus tissue's integrity and absence of traumatic or degenerative changes. The meniscus tissue should appear nearly normal, with no secondary tears or fragmentation that would affect its projected function. The meniscus rim should be trimmed of tear fragments. A horizontal tear into the meniscus rim is a negative variable because it is difficult with sutures to fully restore the tear site owing to inner gaps between the horizontal tear arms. This is one indication in which a fibrin clot may provide a benefit. A large flap tear may be reduced and approximated, and if the tissue has adequate integrity, repair is considered in active patients. A meniscus that has been displaced in the notch may shorten and contract within 3 to 4 weeks, preventing reduction, and accordingly, early arthroscopy and repair are indicated. More specific recommendations of repair indications and techniques are provided for specific tears later in this chapter. The role of incorporating a fibrin clot or platelet-rich plasma to aid the healing process remains poorly understood. Clinical studies are lacking at present; the surgeon's judgment is therefore required on a case-by-case basis.
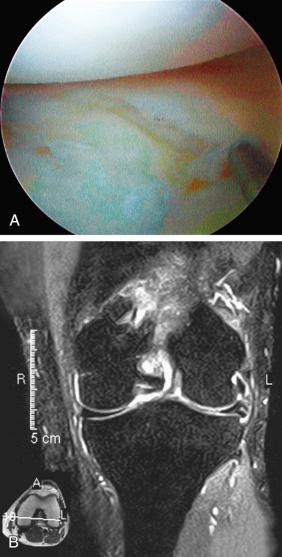
Meniscus tears located in the W/W region are not repairable and require debridement. Chronic degenerative tears usually have tear components in multiple planes and are classified as complex. The surgeon must carefully assess the tear pattern and determine the amount and integrity of meniscal tissue that is present. Many of these tears are not repairable ( Fig. 23-3 ). Chronic degenerative tears in which poor tissue quality is encountered require debridement. The tissue may be thickened or abnormally firm and altered in shape or length. Horizontal tears frequently involve displacement of the meniscus from the joint such that a repair of the horizontal flaps would not result in restoration of meniscus function.
Meniscus tears located in inner third (W/W) region
Chronic degenerative tears in which the tissue is of poor quality, not amendable to suture repair
Longitudinal tears <10 mm in length
Incomplete radial tears that do not extend into the outer third region
Patient >60 years
Patient unwilling to follow postoperative rehabilitation program
Small longitudinal tears less than 10 mm in length are not repaired. In addition, incomplete radial tears that do not extend into the outer third region are either left alone or treated by minimal debridement of the unstable edges. Radial tears should not be debrided into functional meniscal tissue, which would disrupt circumferential hoop fibers and alter meniscus function. The goal in the repair of radial tears is to restore function in the outer and middle zones because the chance of a repair that extends into the inner zone retaining function is highly questionable.
Patient education is required before surgery because complex tears that extend into the avascular region may have a 20% to 40% failure rate and require a repeat arthroscopic meniscus debridement procedure. Patient education is important regarding the goals of the procedure and the failure rate. Patients involved in construction work or other demanding occupations may choose not to have a complex or avascular type of repair. A more difficult problem is the request to remove a repairable R/R tear owing to occupational or athletic pursuits. The senior author (F.R.N.) does not perform this procedure. The senior author categories meniscus tears into three different types. A R/R tear is repaired and, in select small medial tears (15-25 mm in length), an all-inside approach may be considered. However, if there is any associated meniscus tear site damage indicating the need for multiple sutures, an inside-out repair is performed. A R/W tear of either meniscus is repaired with an inside-out technique with accessory posteromedial or posterolateral approaches and multiple vertical sutures because this procedure offers a firmer internal fixation and chance of healing over two to four all-inside sutures. This procedure is performed in all active patients, except older patients (>50 years) who are sedentary. A complex tear that extends into both the R/W and W/W regions may have a success rate of approximately 50%, and the repair of these more difficult tears is usually performed in young patients in an attempt to preserve some meniscal function. In others, a partial meniscectomy is performed.
The menisci provide several vital mechanical functions in the knee joint. They act as a spacer between the femoral condyle and tibial plateau and, when there are no compressive weight-bearing loads across the joint, limit contact between the articular surfaces. The amount of joint narrowing due strictly to the physical absence of the menisci is in the range of 1 to 2 mm.
Spacer, prevents contact between articular surfaces
Load-bearing:
50% compressive load of knee joint transmitted through menisci at 0 degrees of extension
85% compressive load of knee joint transmitted through menisci at 90 degrees of flexion
Increase contact area, reduce contact stress
Partial meniscectomy (15%-34%) increases contact pressures by >350%
Contributes to joint stability
Shock absorption during walking
May assist in overall lubrication of articular surfaces
Studies comparing biomechanic properties of vertical and horizontal sutures, and sutures to meniscus repair devices
Vertical sutures superior initial fixation strength and stiffness during load-to-failure testing compared with horizontal sutures and repair devices
Vertical sutures lower displacements under cyclical loading conditions compared with horizontal sutures and repair devices
Future studies required to determine fixation strength and performance under cyclic loading of all-inside suture-based devices
Under static-loading conditions, the menisci assume a significant load-bearing function in the tibiofemoral articulation. At least 50% of the compressive load of the knee joint is transmitted through the menisci in 0 degrees of extension, and approximately 85% of the load is transmitted at 90 degrees of flexion. The presence of the menisci increases the contact area to 2.5 times the size compared with a meniscectomized joint. The larger contact area provided by the menisci reduces the average contact stress (force/unit area) acting between the joint surfaces. Removal of as little as 15% to 34% of a meniscus increases contact pressures by more than 300%. After total meniscectomy, the tibiofemoral contact area decreases by approximately 50%, and the contact forces increase twofold to threefold.
Lee and colleagues evaluated the effects of serial meniscectomies in the posterior segment of the medial meniscus. Compared with the intact state, the medial contact area decreased from 20% (after removal of 50% of the posterior segment of the medial meniscus) to 54% (total meniscectomy). Medial contact stress increased from 24% (50% meniscectomy) to 134% (total meniscectomy). Medial peak contact stress increased from 43% (50% meniscectomy) to 136% (total meniscectomy). The peripheral portion of the medial meniscus provides a greater contribution to increasing contact area and decreasing contact stresses compared with the central portion. Muriuki and associates created 15- to 20-mm single longitudinal tears in the R/W portion of the posterior horn of the medial meniscus in cadaver knees and reported significant increases in maximum contact pressure and reductions in contact area that were similar to those associated with total meniscectomy.
The menisci remain in constant congruity to the tibial and femoral articular surfaces throughout knee flexion and extension and contribute to stability of the knee joint. Medial meniscectomy performed after sectioning of the ACL results in increased anterior tibial translation at 20 to 30 degrees of knee flexion during a Lachman test compared with that measured in knees with an intact ACL. Thus the loss of the medial meniscus after an ACL rupture is problematic, especially in varus-angulated knees. Spang and associates reported significant increases in ACL strain measured with a variable reluctance transducer in cadaver knees following medial meniscectomy at 60 and 90 degrees of knee flexion ( P < .05). Increases in meniscal strain have also been reported following ACL transection in the laboratory. In knees with posterior cruciate ligament (PCL) ruptures, the increase in posterior tibial translation allows a change in tibiofemoral contact in which the menisci posterior horns have a reduced weight-bearing function. This is sometimes referred to as a PCL meniscectomy . The effect is greater for the medial compartment in which the middle and anterior thirds of the medial meniscus have less weight-bearing function than the lateral meniscus.
The lateral meniscus provides concavity to the lateral tibiofemoral joint owing to the normal posterior convexity of the lateral tibial condyle, allowing the stabilizing effect of joint weight-bearing forces to reduce lateral compartment anterior and posterior translations. Lateral meniscectomy performed after sectioning of the ACL results in increased anterior tibial translation at 30 degrees of knee flexion during a pivot shift test compared with that measured in knees with an intact ACL. Recent studies indicate that the lateral meniscus may be a more important restraint than the medial meniscus to anterior tibial translation during the combined loads applied during the pivot shift test. Partial lateral meniscectomy has been estimated to increase contact pressures by 50% during the stance phase of gait. Total lateral meniscectomy results in a 45% to 50% decrease in total contact area and a 235% to 335% increase in peak local contact pressure.
Loss of the medial meniscus results in a smaller, more medial displacement of the center of pressure. Load is subsequently transmitted through the articular cartilage and subchondral bone to the underlying cancellous bone through this more central route, thus stress-shielding the proximal aspects of the medial tibial cortex. The deleterious effects of meniscectomy on tibiofemoral compartment articular cartilage have been demonstrated in multiple experimental studies. For these reasons, it is paramount to preserve meniscal function, if possible, in knees with varus osseous malalignment.
In addition, the menisci provide specific load-bearing functions to the knee joint during walking and are theorized to assist in overall lubrication of the articular surfaces. Even partial meniscectomy affects knee joint kinetics by reducing range of knee motion and increasing knee adduction moments during stance.
Historically, biomechanical investigations have compared properties of suture techniques with those of rigid all-inside meniscus fixation devices. * Problems with devices such as meniscal arrows, screws, and darts have been well-documented experimentally and clinically. In addition, several studies concluded vertical sutures were superior to both horizontal sutures and meniscus arrows in mean load-to-failure and maximum tensile strength values. †
* References .
† References .
More recently, suture repair techniques, suture materials, and all-inside devices have been tested experimentally to determine initial fixation strength and performance under cyclic loading with varying results ( Table 23-1 ). The majority of studies published to date have been performed in porcine knee models rather than human models. Ultra-high-molecular-weight polyethylene-based (UHMWPE) sutures used in all-inside techniques are now available with newer all-inside repair devices, such as NovoStitch (Ceterix), Hi-Fi (Conmed Linvatec), and FiberWire (Arthrex). Further studies are required to determine the biomechanical properties of these sutures and devices as used for meniscus repair. The lack of both experimental and clinical data precludes definitive recommendations for any one of the currently available all-inside devices over the others. In addition, the reported load-to-failure rates for most of these devices that use one or two sutures is low, justifying consideration for inside-out repairs with multiple sutures to be described. In addition, the low load-to-failure rates and creep properties identify the need for slower postoperative rehabilitation in regard to resumption of full weight bearing, especially for complex meniscus repairs and root repairs. At present, there is little scientific justification regarding when it is safe to resume full weight bearing or return to sports after these types of repairs, although it is appreciated that peripheral longitudinal tears at the R/R junction demonstrate adequate healing within the first 4 to 6 weeks after surgery. The postoperative rehabilitation recommendations are provided in Chapter 25 , with empirical rules build in to protect the meniscus repair.
| Study | Type of Sutures or Devices | Models | Cycles | Results |
|---|---|---|---|---|
| Beamer et al (2015) | Radial tears: one all-inside Ceterix NovoStitch suture or one 2-0 Force Fiber inside-out suture | Porcine | 100, 200, 500 | Load to failure (N): 95 inside-out, 111 all-inside ( P = .03). Stiffness (N/mm): 11.19 inside-out, 14.53 all-inside ( P = .02). Displacement (mm): 2.36 inside-out, 1.52 all-inside ( P < .001). Vertical all-inside technique superior to horizontal inside-out technique. |
| Ramappa et al (2014) | Bucket-handle tears: two running mattress sutures Sequent, two vertical mattress sutures Ultra FasT-Fix, 2 vertical sutures No. 0 Hi-Fi inside-out | Porcine | 100, 300, 500 | Load to failure (N): 138 ± 23 Sequent, 140 ± 30 Ultra FasT-Fix, 188 ± 42 Hi-Fi suture ( P < .001). No differences in stiffness among three groups. Sequent lowest displacement after cycling ( P < .001) but questionable clinical relevance. |
| Feucht et al (2014) | Posterior medial root tears * : transtibial pull-out repair with two vertical sutures TP, or suture anchor repair with two SA | Porcine | 100, 500, 1000 | Load to failure (N): 180 ± 45 TP, 241 ± 45 SA, 862 ± 135 native posterior medial meniscus root. SA lower displacement all conditions ( P < .001), higher stiffness ( P < .05). Both techniques higher displacement, lower maximum load to failure, and stiffness compared with intact menisci ( P < .05). SA technique beneficial; slow rehabilitation recommended. |
| Feucht et al (2013) | Posterior medial root tears: TSS 5 mm apart, one HMS, MAA, two modified LS | Porcine | 100, 500, 1000 | Load to failure (N): 235 ± 39 TSS, 250 ± 57 TLS, 280 ± 65 HMS, 335 ± 59 MMA. MMA highest max load to failure ( P < .01), less displacement after cycling ( P < .05), higher stiffness ( P < .05). |
| Feucht et al (2013) | Posterior medial root tears: one suture No. 2 PDS, Ethibond, FiberWire, FiberTape | Porcine | 100, 500, 1000 | Load to failure (N): 133 ± 35 PDS, 146 ± 21 Ethibond, 169 ± 43 FiberWire, 196 ± 62 FiberTape. None of the suture materials had superior properties over the others. |
| Rosslenbroich et al (2013) | Posterior lateral root tears: transtibial approach one suture or two sutures, 3 mm apart tied over button | Porcine | 1000 | Load to failure (N): 150 ± 24 SS, 301 ± 41 two sutures. Two-suture technique lower displacement, higher stiffness, higher ultimate failure load ( P < .05). |
| Matsubara et al (2012) | Radial tears: DHS, CS | Cadavers | 500 | Load to failure (N): 68 ± 13 DHS, 79 ± 19 CS. CS higher ultimate failure loads, greater stiffness, lower displacement ( P < .05). |
| Herbort et al (2010) | Radial tears: DHS, SS wider distance from meniscal rim | Porcine | 1000 | DHS higher maximum load (108 ± 12 N), highest stiffness, lower displacement ( P < .05) compared with SS configurations. |
| Chang et al (2009) | Single longitudinal tears: single vertical repair No. 2 FiberWire, No. 2 Ethibone, FasT-Fix, RapidLoc, Meniscal-Dart, BioStinger | Porcine | 300 | Load to failure (N): 16 Dart, 34 BioStinger, 41 RapidLoc, 68 FasT-Fix, 114 No. 2 Ethibone, 175 No. 2 FiberWire. Failure strength and stiffness highest in No. 2 FiberWire ( P < 0.05). Failure load higher and displacement lower in suture groups compared with devices ( P < .01). |
| Mehta & Terry (2009) | Single longitudinal tear 25 mm: one HMS Meniscal Cinch, Ultra FasT-Fix, MaxFire | Cadavers | 100, 500 | Load to failure (N): 64 MaxFire, 86 Ultra FasT-Fix, 85 meniscal Cinch. Ultra FasT-Fix and Meniscal Cinch had more desirable biomechanical profiles (lower failure rate, greater stiffness, P < .05). MaxFire larger gap formation and lower load to failure ( P < .05). |
| Nyland et al (2008) | Single longitudinal tear 20 mm: two vertically or horizontally placed FasT-Fix, two horizontally placed RapidLoc devices | Cadavers, implants placed 5 mm apart | 500 | Vertical FasT-Fix less displacement, greater stiffness ( P < .001). |
| Kocabey et al (2006) | Single longitudinal tear 20 mm: two vertical, horizontal, oblique sutures | Bovine, sutures placed 5 mm apart | 100 | Load to failure (N): 89 ± 8 horizontal suture, 146 ± 32 vertical suture, 172 ± 26 oblique suture. Oblique and vertical sutures greater stiffness ( P < .05), load to failure ( P = .001) than horizontal. No difference in displacement. |
| Kocabey et al (2006) | Single longitudinal tear 20 mm: two vertically or horizontally placed FasT-Fix, two horizontally placed RapidLoc devices | Cadavers | 500 | Load to failure (N): 87 ± 13 RapidLoc, 90 ± 14 horizontal FasT-Fix, 125 ± 39 Vertical FasT-Fix. Vertical FasT-Fix less displacement ( P < .01), greater load to failure ( P < .05), greater stiffness ( P < .001). |
| Chang et al (2005) | Single longitudinal tear 20 mm: two Vertical mattress sutures, two Meniscal Viper Repair sutures, two vertical FasT-Fix sutures | Porcine | 500 | Load to failure (N): 111 ± 30 Meniscal Viper, 133 ± 10 vertical mattress sutures, 146 ± 9 Vertical FasT-Fix. Vertical mattress suture less displacement, higher stiffness during cyclic testing ( P < .001), suggesting potential for better healing. |
* Root tear: avulsion of the tibial insertion of the meniscus or a radial tear close to the meniscal insertion.
There are few published experimental studies on the strength of a healing meniscus suture repair (without cell-based therapy or growth factors) subjected to tensile loads or assessed for residual defects and complications. In 1995, Miller and associates reported acceptable healing rates of single longitudinal meniscus tears repaired in the periphery in a goat model. More recently, Miller and colleagues found unacceptably high rates of chondral damage 6 months after implantation of Meniscal Fastners (Mitek, Westwood, MA), BioStingers (Linvatec), and Clearfix Screws (Mitek) in this same animal model. The authors cautioned against the use of these rigid all-inside devices in humans. In 2009, Hospodar and coworkers reported superior healing of meniscus repairs done with an inside-out suture technique compared with the all-inside FasT-Fix device in goats. The FasT-Fix group had longer residual full-thickness defects ( P = .01) and longer residual partial-thickness defects ( P < .001) 6 months postoperatively.
A thorough history includes assessment of the injury mechanism, initial and residual symptoms, and functional limitations. Common injury mechanisms are a sudden twist, change in direction (cut), or deep knee flexion. Meniscus tears are frequently encountered in knees with ACL ruptures. A comprehensive knee examination is performed that includes assessment of knee motion, patellofemoral indexes, tibiofemoral pain and crepitus, muscle strength, ligament subluxation tests, and gait abnormalities.
Tibiofemoral joint line pain, compression pain
McMurray test
Knee flexion and extension
Joint effusion
Patellofemoral (medial and lateral subluxation, Q-angle, crepitus, compression pain)
Muscle strength
Proton-density-weighted, high-resolution, fast-spin-echo sequence
Pivot shift, Lachman
KT-2000 (MEDmetric) 20 degrees of knee flexion, 134 N force
Posterior drawer, 90 degrees of knee flexion
External tibial rotation 30 degrees, 90 degrees of knee flexion
Tibiofemoral rotation dial 30 degrees, 90 degrees of knee flexion
External rotation recurvatum
Lateral tibiofemoral joint opening 5 degrees, 20 degrees of knee flexion
Reverse pivot shift
Medial tibiofemoral joint opening 5 degrees, 20 degrees of knee flexion
Anteroposterior
Lateral, 30 degrees of knee flexion
Posteroanterior, weight bearing, 45 degrees of knee flexion
Patellofemoral axial
Sports Activity and Function Form
Occupational Rating Form
Symptom Rating Form
The presence of tibiofemoral joint line pain on joint palpation is a primary indicator of a meniscus tear. Other clinical signs include pain on forced flexion, obvious meniscal displacement during joint compression and flexion and extension, lack of full extension, and a positive McMurray test result. All ligament stability tests are performed and compared with the opposite knee joint. MRI may be obtained with a proton density weighted, high-resolution, fast spin-echo sequence to determine the status of the articular cartilage and menisci. This evaluation is useful in knees with suspected degenerative tears and chronic ACL ruptures and to determine whether a meniscus cyst is present. A recent investigation that examined the ability of MRI to predict reparability of longitudinal full-thickness meniscus lesions reported high sensitivity and specificity rates (overall, 94% and 81%, respectively).
LaPrade and Konowalchuk described a figure-four test that attempts to replicate symptoms in patients with tears of the lateral meniscus popliteomeniscal attachments. The patient is placed supine, the knee flexed to approximately 90 degrees, the foot placed over the contralateral knee, and the hip externally rotated. A varus loading at the knee joint increases tensile loading in the damaged posterolateral soft tissue meniscal attachments. The primary symptom from popliteomeniscal tears is lateral compartment pain with activities, especially turning and twisting with sports. MRI findings are frequently negative. These authors described an open approach to repair the popliteomeniscal attachments. However, peripheral tears are amendable to an inside-out repair technique, as described.
The clinical examination may reveal tenderness on palpation at the posterolateral aspect of the joint at the anatomic site of the popliteomeniscal attachments. The McMurray test is performed in maximum flexion, progressing from maximum external rotation to internal rotation and then back to external rotation. This test may produce a lateral palpable snapping sensation, representing an anterior subluxation of the posterior horn of the lateral meniscus with maximum internal rotation. The snapping is produced with external rotation as the meniscus returns to a normal position. Of interest, patients with physiologic joint laxity and increases in tibial rotation limits can commonly produce this lateral snapping sign in both knees under examination, which is not painful. Patients with tears of the popliteomeniscal attachments may have a positive snapping sign in only the symptomatic knee, which produces posterolateral joint pain.
Radiographs taken during the initial examination include lateral at 30 degrees of knee flexion, weight-bearing PA at 45 degrees of knee flexion, and patellofemoral axial. Axial lower limb alignment is measured using full standing hip-knee-ankle weight-bearing radiographs in knees that demonstrate varus or valgus alignment. Knees that have deficiency of the posterolateral structures may require lateral stress radiographs. Posterior stress radiographs may be obtained in patients with PCL ruptures.
Patients complete questionnaires and are interviewed to rate symptoms, functional limitations, sports and occupational activity levels, and patient perception of the overall knee condition according to the Cincinnati Knee Rating System (CKRS).
Concomitant injuries should be evaluated and may include cruciate or collateral ligament rupture, extensor mechanism injury or malalignment, chondral fracture, osseous malalignment, or an overuse syndrome. The patient is informed that the rehabilitation program may require modification according to the procedures performed. Knees with ACL or PCL deficiency require concomitant ligament reconstruction with the meniscus repair to achieve knee stability and protect the repair site. Knees with varus osseous malalignment that require osteotomy may also have chronic medial meniscus tears that are occasionally repaired.
Knees with cruciate deficiency: plan reconstruction with meniscus repair
Other concomitant injuries may include collateral ligament ruptures, extensor mechanism injuries, chondral fractures
Associated chronic conditions may include extensor mechanism malalignment, overuse syndrome, varus osseous malalignment. Consider meniscus repair whenever possible in these knees.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here