Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The melolabial crease delineates the cheek from the caudal nose and from the upper and lower lips. It is created by the insertion of the superficial muscular aponeurotic system (SMAS) into the skin at the junction of the cutaneous lips and the cheek. Medial to the crease, the skin of the lips is tightly attached to the orbicularis oris and there is minimal subcutaneous fat. Lateral to the crease, the skin of the cheek is loosely attached to the deep muscular fascia and there is an abundance of subcutaneous fat. With time the forces of muscle contraction, gravity, and aging result in a progressive deepening of the melolabial crease. The subcutaneous fat immediately lateral to the crease forms the melolabial fold. The melolabial crease serves as a facial divide separating the lips from the cheeks and represents one of the most important of the facial aesthetic boundaries.
Because of the proximity of the melolabial fold to the nose and lips, melolabial flaps have long been used to repair these structures. , During the nineteenth and twentieth centuries, many varieties of melolabial flaps were described. In the past, such flaps have been called nasal labial flaps , but the term melolabial is more accurate in description as the prefix melo- refers to the cheek and the suffix -labial refers to the lips. Thus it is more accurate to use the term melolabial crease rather than nasolabial crease because the crease separates the lips from the cheek, not the nose from the cheek. This chapter will discuss only cutaneous flaps harvested from the mound of skin immediately lateral to the melolabial crease and known as the melolabial fold .
Melolabial cutaneous flaps are skin flaps harvested from the melolabial fold lateral to the melolabial crease. The cheek skin in this region of the face has a rich blood supply from perforating branches of the facial artery and is drained by the facial angular vein. Because of the extensive vascularity of the medial cheek skin, melolabial flaps may be based either superiorly or inferiorly. Skin of the melolabial fold, including the jowl area, is the most redundant of all areas of the face. There is usually sufficient skin to enable the transfer of sizeable flaps for reconstruction and, at the same time, allow closure of the donor site of the flap. In addition, the closure line of the flap donor defect can be positioned in or parallel to the melolabial crease to provide maximum scar camouflage. Because of proximity, the color, texture, and thickness of the skin of the melolabial fold closely matches that of the lips and the caudal lateral nose. Therefore melolabial flaps are particularly suited for repair of cutaneous defects of these areas of the face. In contrast, the skin of the dorsum and cephalic portion of the nasal sidewall are thin and tend to have less sebaceous glandularity than the skin of the melolabial fold. As a consequence, melolabial flaps are less well-suited for repair of cutaneous defects located in these areas of the nose. The skin of the melolabial fold is particularly similar in sebaceous glandularity and texture to the skin of the ala. It is for this reason that skin defects of the ala are preferably repaired using skin from the melolabial fold. This is usually accomplished by using an interpolated cheek flap that crosses the alar facial sulcus and requires subsequent detachment of the flap’s pedicle. Crossing over rather than through the sulcus maintains a perfectly natural alar facial sulcus, an important facial aesthetic boundary.
Local cutaneous flap classification and terminology is discussed in detail in Chapter 6 , but a brief summary here is helpful to understanding the mechanisms of movement of flaps harvested from the melolabial fold. Classifying flaps by method of transfer, which is to say by tissue movement, is usually the most convenient way of discussing flaps relative to their use in repairing facial cutaneous defects. It also contributes to the understanding of where standing cutaneous deformities (SCDs) develop and where the maximum wound closure tension occurs during wound repair. Using this classification, melolabial flaps may be categorized as pivotal, advancement, or hinge. Melolabial hinge flaps are rarely used and will not be discussed in this chapter. Advancement in the majority of situations depends on stretching the flap skin in the direction of flap movement. Such flaps are subjected to an increase in wound closure tension. In contrast, pivotal flaps rotate about a point at their base and in their purest form are not stretched. Thus they are not subjected to wound closure tension greater than the natural tension of the remaining facial skin, although the repair of the donor site of the flap is subjected to increase tension. There are three types of pivotal flaps: rotation, transposition, and interpolated. Transposition and interpolated flaps may be transferred on a cutaneous pedicle or subcutaneous tissue pedicle. In the latter case, the flap is referred to as an island flap because it has no cutaneous connection to the donor site. Island transposition pivotal flaps are occasionally harvested from the melolabial fold but are uncommonly used and will not be discussed. Rotation flaps are pivotal flaps with a curvilinear configuration. They must be designed immediately adjacent to the defect and are best used to close triangular defects. In the author’s practice, local flaps in the form of rotation are rarely designed in the area of the melolabial fold because their curvilinear incision frequently creates a scar that crosses the melolabial crease perpendicular to relaxed skin tension lines (RSTLs). For this reason, rotation flaps will not be discussed.
In contrast to rotation flaps, which must be designed adjacent to the defect, transposition flaps provide the surgeon the ability to construct a flap at some distance from the defect with its axis independent of the linear axis of the defect. The only requirement is that the base of the flap is contiguous with the defect the flap is designed to repair. This is one of the greatest advantages of transposition flaps. This fact enables the surgeon to recruit skin from the melolabial fold, which may be a considerable distance from the defect. Skin elasticity and redundancy is greater in the area of the melolabial fold than any other location on the face, providing a resource for harvesting sizeable flaps. The linearity of transposition flaps can be designed so that they parallel the melolabial fold and this in turn enables the donor site to be closed parallel or in the melolabial crease. Because of these advantages, transposition is the most common design of local flaps harvested from the area of the melolabial fold.
The interpolated flap, like the transposition flap, is transferred by pivotal movement and has a linear configuration so that it can be designed to conform to the linear axis of the melolabial fold. Interpolated flaps differ from transposition flaps in that their bases are not contiguous with the defect. Thus the pedicle must cross over or under intervening tissue. If the pedicle passes over intervening tissue, the flap must subsequently be detached from its donor site in a second surgical procedure. This is known as inset of the flap . This is the greatest disadvantage of such flaps. On occasion, the pedicle can be de-epithelialized or reduced to subcutaneous tissue only (island flap) and brought under the intervening skin to allow a single stage reconstruction. Passing flaps through a subcutaneous tunnel may compromise the vascularity of the pedicle or create a contour deformity along its path. The major advantage of interpolated flaps compared with transposition flaps is the ability to recruit skin for construction of the flap at a site that is more removed from the facial defect. The interpolated melolabial flap is frequently used for nasal reconstruction because of the proximity of the melolabial fold to the nose and its similar skin color and texture to the skin of the nose.
Transposition flaps are the most common type of melolabial flaps used in facial reconstruction. Transposition flaps are pivotal flaps with a linear configuration. They may be based inferiorly or superiorly and have a number of different configurations. Their linear dimension, however, is always longer than their width. Typically, the linear axis of a melolabial transposition flap is oriented directly above and parallel to the linear axis of the angular artery. Although the flap is rarely elevated as a true axial flap incorporating the angular artery, many small peripheral branches of the artery are probably included in the base of melolabial flaps.
The majority of melolabial transposition flaps are designed as a rectangle, parabola, or rhombus. The axes of these flaps are usually oriented along or parallel to the axis of the melolabial fold ( Fig. 12.1 ). Closure of the flap donor site is within or parallel to the melolabial crease. The flap may be lengthy relative to its width, which facilitates closure of the donor defect without excessive wound closure tension. Melolabial transposition flaps used to repair small (2 cm or less) cutaneous defects of the medial cheek may be based superiorly or inferiorly. Transposition flaps used to repair medial cheek defects greater than 3 cm, however, should be based superiorly because there is more redundancy of facial skin in the inferior cheek in the region of the jowl. In older patients, this redundancy can provide a source for a large flap and still enable primary closure of the donor site. Flaps should be designed so that whenever possible, closure of the donor site is in the melolabial and labial mandibular creases. When using superiorly based melolabial transposition flaps, the SCD is removed just medial or lateral to the superior border of the defect depending on whether the flap is pivoted medially or laterally.
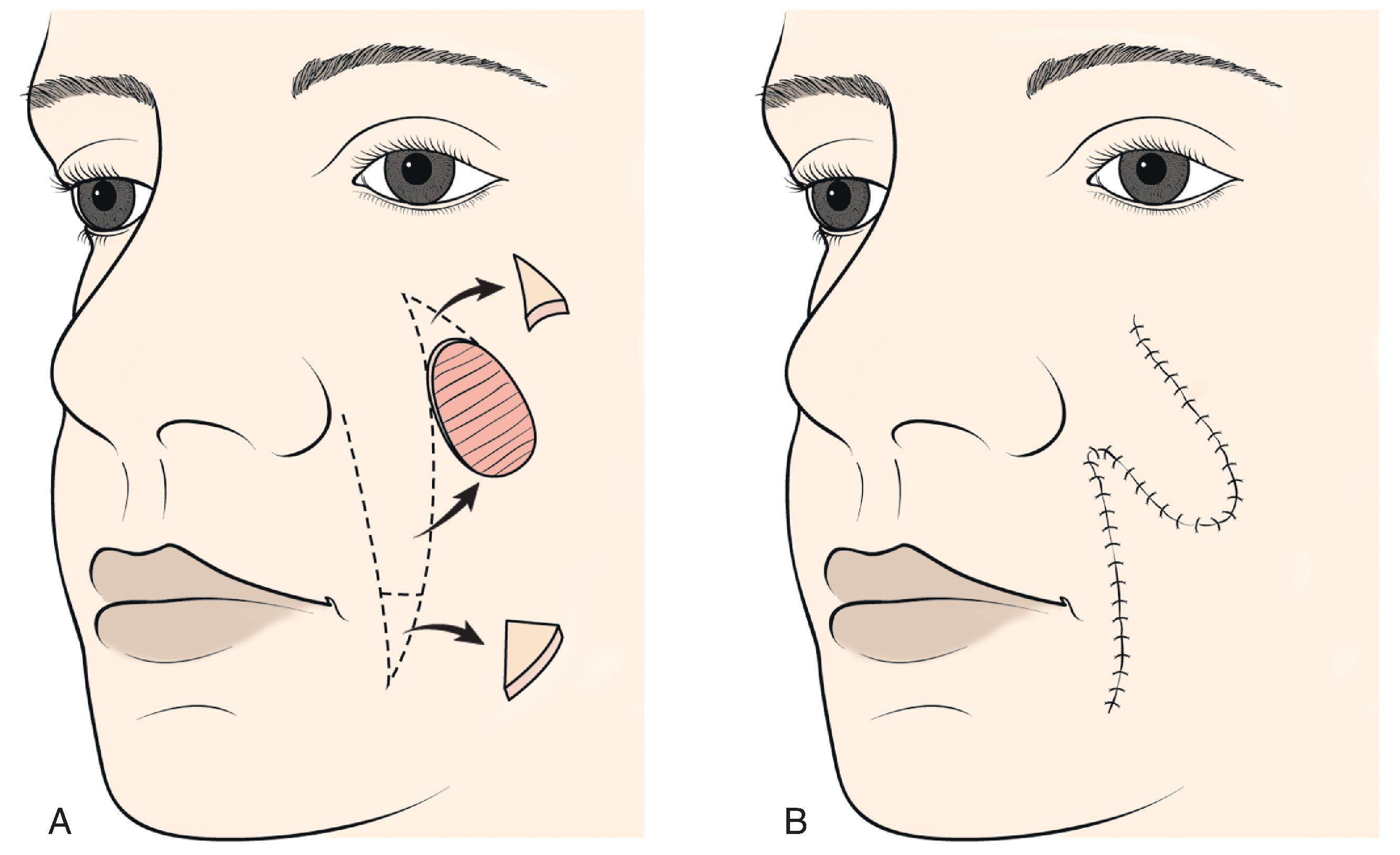
Transposition flaps are pivotal flaps and the greater the arc of pivotal movement, the greater the size of the SCD and the smaller the effective length of the flap (see discussion in Chapter 8 ). The reduction in effective length must be accounted for when designing melolabial transposition flaps so that greater pivoting requires a longer design of the flap. To limit this restricting factor, whenever possible, melolabial transposition flaps should be designed to pivot no more than 90°.
Advancement flaps have a linear configuration and are moved by sliding toward the defect. This involves stretching the skin of the flap. Thus advancement flaps work best in areas of greater skin elasticity and redundancy like the melolabial fold. The most basic advancement flap is the simple linear layered closure, which involves the undermining and direct advancement of tissue side-to-side to close the defect primarily. Sizeable (3 cm) skin defects of the medial cheek can be closed this way by advancing skin from the melolabial region in such a fashion that the resulting SCDs can be excised parallel to the melolabial crease. The term advancement flap , however, usually refers to a flap created by incisions, which allow for a “sliding” movement of tissue. Tissue transfer is achieved by moving the flap on its pedicle in a single vector. The greatest wound closure tension is perpendicular to the distal border of the flap. Advancement flaps may be categorized as unipedicle, bipedicle, V-to-Y, Y-to-V, or island. Only unipedicle and island advancement flaps will be discussed in this chapter because they are the most common melolabial advancement flaps used in facial reconstruction.
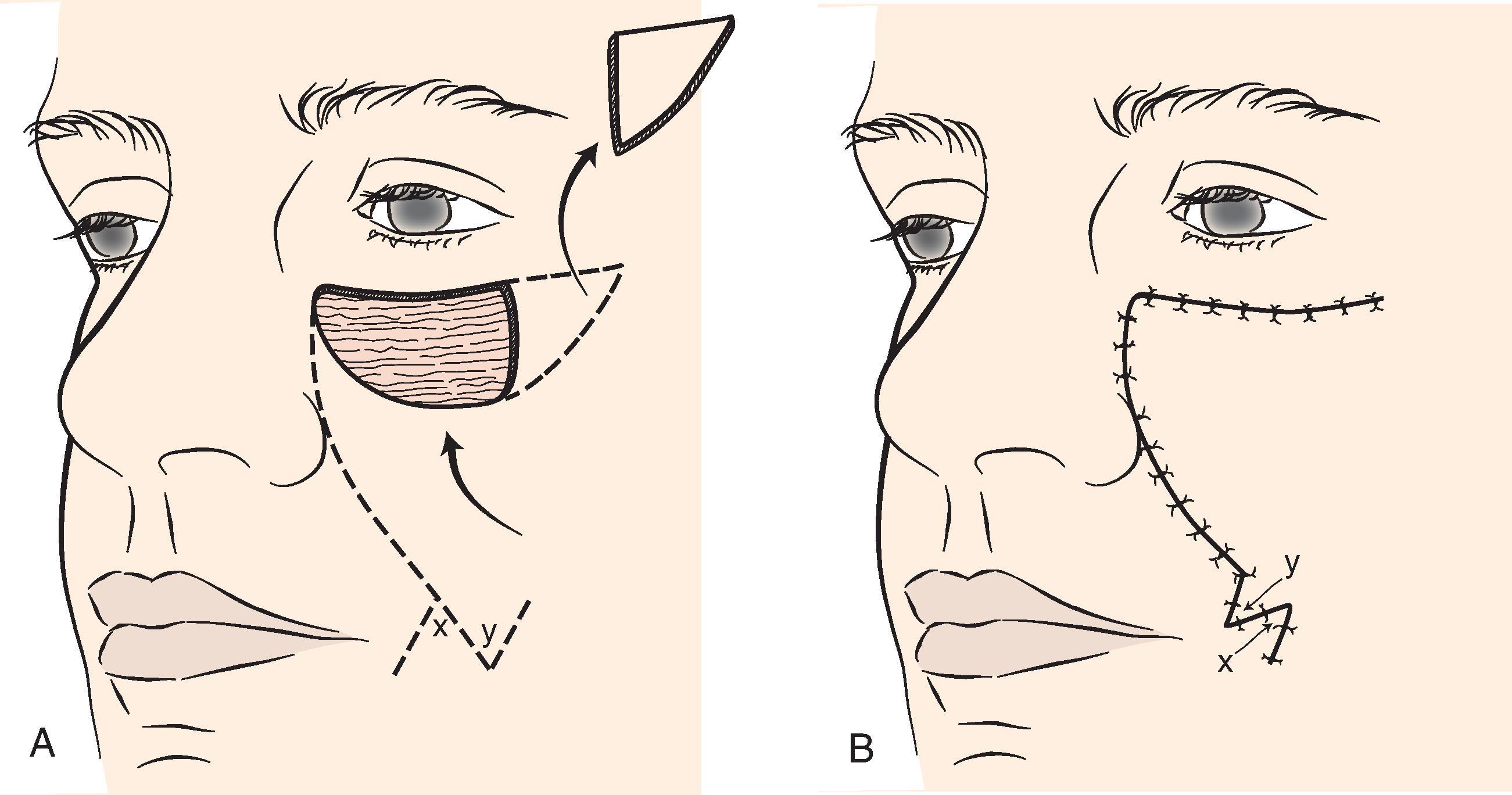
Unipedicle advancement flaps are created by parallel incisions, which allow a sliding movement of skin in a single vector toward the defect. This movement is in one direction and the flap advances directly over the defect. As a consequence, the flap must be developed adjacent to the defect and one border of the defect becomes the leading border of the flap. Melolabial advancement flaps are not frequently designed with two parallel incisions. When used to repair skin defects of the superomedial cheek, melolabial advancement flaps are usually designed making only one long incision in the melolabial crease and undermining the skin of the fold lateral to the incision ( Fig. 12.2 ). Skin is then advanced upward in a vector parallel to the melolabial crease with some additional slight pivotal movement. The pivotal movement, although limited, eliminates the need to make the second incision parallel to the first incision to create and move the flap. An SCD is excised lateral to the skin defect parallel to the inferior bony orbital rim.
The melolabial V-to-Y subcutaneous tissue pedicle island advancement flap is an option for repairing medial cheek skin defects at or below the level of the nasal alae. , The flap is particularly well suited for skin defects located immediately adjacent to the alae ( Fig. 12.3 ). A triangular-shaped skin island is designed with the base of the triangle formed by the inferior margin of the defect. Optimally, the vector of flap advancement is designed parallel to the melolabial crease. The width of the skin island should equal the width of the defect at its widest point. The height of the skin island should generally be twice the height of the defect. The trailing half of the skin island tapers to a point to facilitate donor site closure in a V-to-Y fashion after flap advancement. The flap is therefore sometimes referred to as a V-to-Y island advancement flap . The skin island may extend as far as the inferior border of the mandible if necessary. Positioning the inferior tip of the skin island directly in the melolabial crease optimally conceals the donor site scar. In so far as possible, incisions should be designed so that their scars are parallel to or in borders of aesthetic regions.
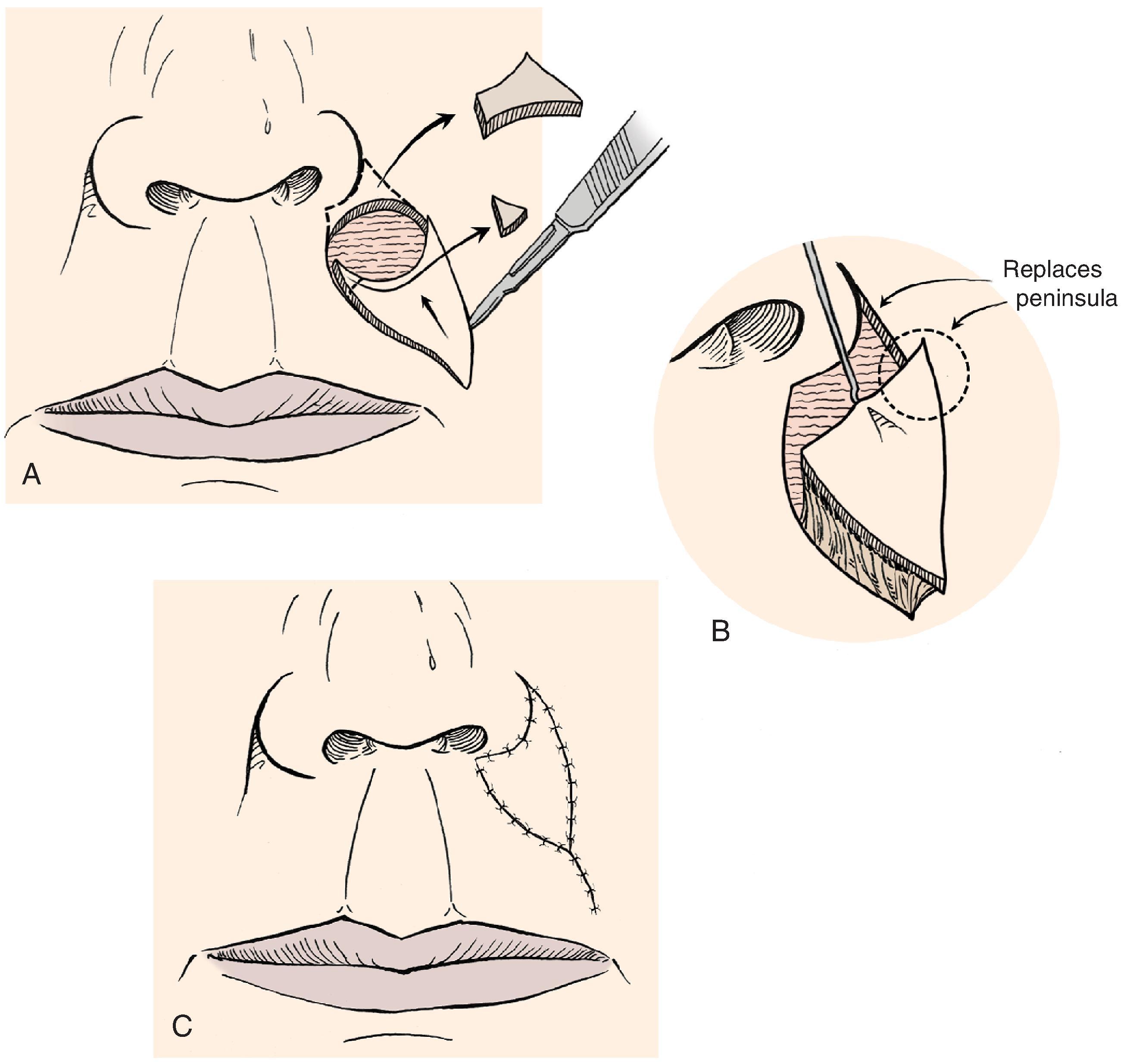
The perimeter of the skin island is incised to the level of the superficial subcutaneous fat. Undermining the adjacent facial skin for a distance of 2 cm is performed at this level. Blunt and sharp dissection is then carried through the subcutaneous tissue surrounding the skin island, beveling slightly away from the skin island down to the level of the fascia overlying the facial muscles. This frees the elastic subcutaneous tissue pedicle from its medial and lateral fibrous attachments to the surrounding cheek fat, while preserving its vascular supply, which is derived from its deep attachments. The skin island is then advanced toward the defect by placing a skin hook at its leading border. At this point, the pedicle can be narrowed to facilitate the advancement of the flap. This is accomplished by back cutting the peripheral borders of the flap in the subcutaneous tissue plane, leaving at least one-third of the total flap surface area attached to the underlying subcutaneous tissue. Further thinning of the subcutaneous tissue of the undermined leading border of the flap may be performed to create an appropriate thickness match between the border of the flap and the recipient site. A central pedicle attached to at least one-third of the total skin island surface area will adequately profuse the flap. Further subcutaneous undermining of the skin adjacent to the flap is required if puckering of the peripheral facial skin occurs with flap mobilization (see Fig. 12.3 ). Subcutaneous undermining is also performed at the recipient site. In addition, the recipient sites’ depth and shape may be modified by removing skin and subcutaneous tissue so that scars will be positioned along aesthetic boundary lines and the defect will more appropriately accommodate the thickness of the advancement flap. The leading border of the skin island is fixed in place and the wound surrounding the remaining perimeter of the flap subsequently closed, such that wound closure tension is equally distributed over the entire length of the flap. The flap donor site is closed in a V-to-Y fashion, taking care to compensate for any differences in the length of the opposing margins of the donor site by suturing on a bias (see Chapter 6 ).
In addition to repair of medial cheek defects as discussed, subcutaneous tissue pedicle island advancement flaps are ideally suited for repair of skin defects of the lateral upper lip. They do not work as well for defects of the lower lip. The flap is dissected in a similar fashion to the method discussed for its use in repairing medial cheek defects except the flap is freed from its orbicularis muscle attachments near the commissure and is based solely on the abundant subcutaneous fat located just lateral to the commissure. This is only when the flap is sufficiently large to necessitate the incorporation of skin of the melolabial fold into the flap.
For sizeable (2–3 cm) lip skin defects located adjacent to the inferior border of the ala, it may be beneficial to excise the small peninsula of skin between the ala and melolabial fold in the process of enlarging the defect so that it extends to an aesthetic boundary. ,
The peninsula is then reconstructed by appropriately designing the island flap so that the superior portion of the flap replaces the peninsula (see Fig. 12.3 ). This technique provides the best scar camouflage because the superior border of the flap is positioned within the aesthetic boundaries of the alar facial sulcus and melolabial crease. When this peninsula is not replaced, the flap must cross the base of the peninsula and may mar an otherwise excellent result.
The major advantage of the subcutaneous tissue pedicle melolabial advancement flaps used to repair cutaneous defects of the medial cheek and upper lip is that there is no need to resect SCDs because these do not develop with this flap. For this reason, these flaps are particularly advantageous compared with transposition and cutaneous-pedicled advancement flaps, which often have sizeable deformities that must be resected and discarded. There is no wasted skin with the island flap. Another important advantage of the island flap is that there is considerably less dead space beneath the flap as well as beneath skin surrounding the donor defect compared with using cutaneous pedicled flaps. Less dead space means less space available for collection of blood and serum. Therefore there is less risk for developing a hematoma compared with using other types of flaps. The major disadvantage of the island flap is a tendency to develop trap-door deformity, especially for smaller flaps (less than 3 cm in size).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here