Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pigmented lesions of the vulva are a concern to patients, their health care providers, and pathologists who interpret the histopathology. Gynecologists are particularly wary of pigmented lesions of the vulva—the prognosis for vulvar melanoma is poor because of the tendency for increased tumor thickness at the time of presentation. For this reason, gynecologists tend to be liberal about performing biopsies on clinically pigmented lesions.
Familiarity with the range of melanocytic lesions encountered that involve the vulva is important. Virtually any variant of a melanocytic lesion that occurs in nongenital sites may also occur on the vulva. A detailed description of the spectrum of cutaneous melanocytic lesions is beyond the scope of this discussion, and the reader is referred to dermatopathology texts or monographs on melanocytic lesions to gain a comprehensive understanding of cutaneous melanocytic lesions. This chapter describes the patterns of melanocytic neoplasia seen in the vulva, acquaints the reader with the terminology used, and addresses the differential diagnosis of this range of entities.
A variety of conditions involving the vulva are pigmented ( Table 8.1 ). It is important to perform an excisional biopsy, when possible, if there is clinical concern for melanoma. Various methods to perform the biopsy include an elliptical excision or punch biopsy. A superficial shave biopsy should not be performed because of the risk of transecting the lesion, which could result in difficulty in histologic evaluation. An incisional biopsy may be performed if the lesion is too large or too close to vital structures to excise completely. Several studies have documented that an incisional biopsy for melanoma does not increase the risk of tumor seeding, metastasis, or decreased survival. Various terms are used to describe the histologic changes of pigmented conditions ( Table 8.2 ).
| Entity | Dominant Features | Exclude |
|---|---|---|
| Melanosis | Hyperpigmented basal keratinocytes | Melanoma in situ |
| Genital-type nevus | Large, often irregularly placed nests or melanocytes | Melanoma |
| Dysplastic nevus | Both architectural and cytologic atypia | Melanoma, genital-type nevus |
| Melanoma | Monotonous severe cytologic atypia with architectural abnormalities | Dysplastic nevus, genital-type nevus |
| Term | Definition |
|---|---|
| Junctional | Refers to melanocytes at the dermal-epidermal junction |
| Lentiginous | Proliferation of single melanocytes along the dermal-epidermal junction |
| Shoulder | Extension of the junctional component beyond the dermal component of a nevus |
| Atypia | Increased nuclear size, irregularities in nuclear outline or chromatin, and prominent nucleoli. Grading of atypia relies on nuclear size of melanocytes compared with intraspinous keratinocyte nuclei (see text). |
| Maturation | Constellation of findings, most notably diminution in cell size with depth |
| Bridging | Nests of melanocytes spanning rete (see Fig. 8.9 ) |
| Moth-eaten | Effacement of the dermal-epidermal junction by the dermal component |
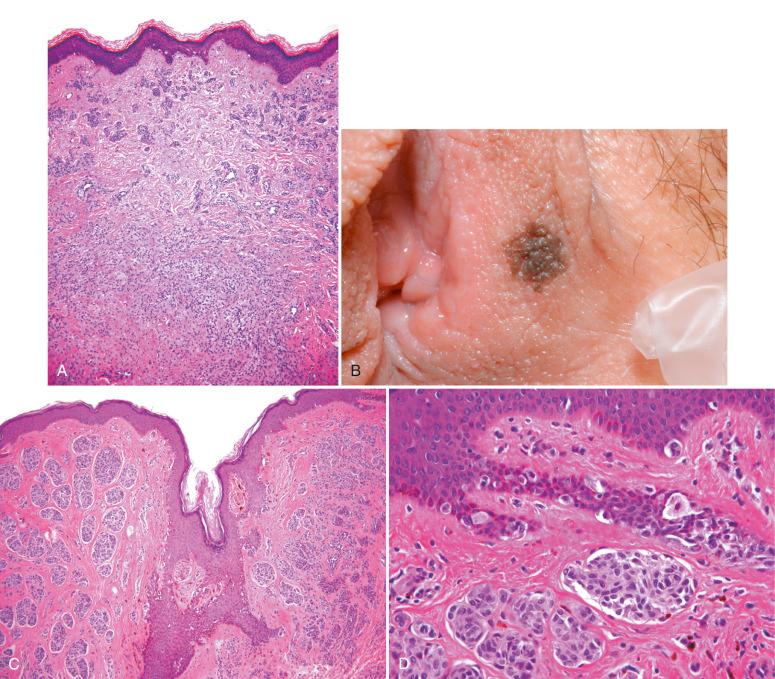
Genital melanosis, also known as vulvar lentiginosis and vulvar melanotic macules, is a benign lesion characterized by macular pigmentation that can involve cutaneous or mucosal sites. It accounts for most pigmented vulvar lesions (≈68%) in women of reproductive age, and the median age at presentation is 40 to 44 years. Lesions are often clinically concerning because they are frequently large, with irregular borders. The macules may be single or multiple, with predilection for mucosal surfaces, including the vulva, vagina, and cervix, rather than hair-bearing skin ( Fig. 8.1A and B ). Typically, pigmentation increases slowly over time. Vulvar melanosis has been associated with hormonal factors after reported cases coinciding with the use of oral contraceptives and the postpartum period. Vulvar melanosis has also been associated with lichen sclerosus (see Fig. 8.1C ) and human papillomavirus (HPV) infection.

In children, the possibility of a genodermatosis should be considered (e.g., Peutz-Jeghers syndrome, Dowling-Degos disease). Laugier–Hunziker syndrome (idiopathic lenticular mucocutaneous pigmentation) is a disorder characterized by genital lesions associated with oral pigmentation. Rarely, Carney's complex may present with lentigines in the genital skin and mucosa.
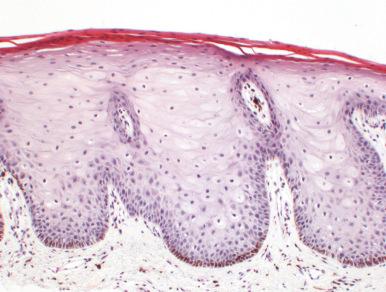
Biopsy of genital melanosis shows increased pigmentation of basal keratinocytes, predominantly affecting the tips of the rete to variable degrees ( Fig. 8.2 ). In many cases, abundant melanin is present within melanophages in the papillary dermis or superficial lamina propria, so-called pigment incontinence. Some authors restrict use of the term genital melanosis to lesions that do not show increased numbers of melanocytes. In contrast, the term genital lentiginosis is applied to similar lesions that are associated with increased numbers of melanocytes. The terminology used is of nosologic but not practical importance. Melanocytic atypia is not a typical feature and, if present, particularly when accompanied by a pagetoid spread of melanocytes, should raise concern for a significant precursor lesion or even melanoma in situ.
This is also known as atypical melanocytic nevus of the genital type, atypical genital nevus, flexural-type nevus, and milk line nevus.
Typical intradermal and compound nevi can be seen in the vulva and are similar to those at other sites ( Fig. 8.3 ). The genital-type nevus (GTN) often shows distinctive histologic features that are also seen in other sites characterized by redundant skin. For this reason, the term flexural-type nevus is sometimes applied to this variant. Other regions where flexural-type nevi are commonly encountered include the axillae, umbilicus, inguinal creases, scrotum, and perianal areas. Familiarity with flexural-type nevi is of great importance because they may be associated with histologic features that raise the possibility of, or may be confused with, melanoma.
It is estimated that the prevalence of vulvar nevi is approximately 2.3%, accounting for approximately 20% of all pigmented lesions of the vulva. GTNs comprise approximately 5% of vulvar nevi. They are most common in young women but may also be seen in young girls and older women. In adults, vulvar nevi are generally encountered on premenopausal women, with an estimated median age range of 28 to 33 years of age for typical nevi and 17 to 26 years for GTN. Compared with common nevi occurring in the vulva, GTNs are more frequently located on the labia minora and equally affect genital hair-bearing skin and mucosal surfaces in adults. In children 10 years of age or younger, GTNs are more common in mucosal sites.
GTNs are often heavily pigmented, irregular, vary in size from a few millimeters to 1 cm or more in their greatest dimension, and may be concerning clinically. They may occur anywhere on the vulva, including the labia majora, labia minora, and clitoris.
As noted earlier, GTNs can be a source of considerable diagnostic difficulty because they are less frequently encountered than common dermal and compound nevi. Consequently, many surgical pathologists are not familiar with their unique histologic features. When atypical features are present, they may be confused with melanoma ( Table 8.3 ).
| Feature | Genital-Type Nevus | Vulvar Melanoma |
|---|---|---|
| Age (yr) | <50 | >50 |
| Size (cm) | <1 | >1 |
| Symmetry | Present | Absent |
| Lentiginous growth | Minor | Extensive |
| Cytologic atypia | Present, punctuated | Present, diffuse, monotonous |
| Maturation | Present | Absent |
| Mitoses | Rare | Readily identified, atypical forms |
GTNs may be junctional or compound. At scanning magnification, they may be symmetric or asymmetric and often have a papillomatous appearance ( Fig. 8.4A ). The junctional component is usually lentiginous and nested (see Fig. 8.4B ). The junctional nests are often large, surrounded by a retraction artifact, and are frequently irregularly placed at the sides of a rete (not a typical feature of nevi at nonflexural sites), as well as rete tips ( Fig. 8.5 ). A common feature is the presence of transepidermal elimination of nests of melanocytes; however, frank intraepidermal pagetoid spread of individual melanocytes is not a prominent feature (see later). In our experience, when pagetoid spread is present, it is usually limited to small numbers of cells and restricted to the lower layers of the epidermis.
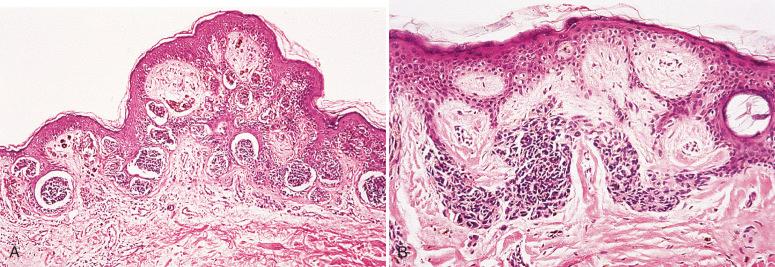
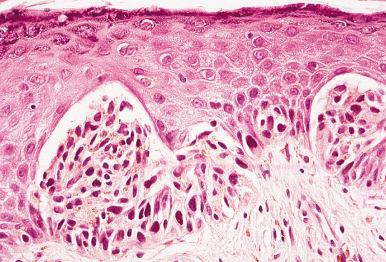
The junctional nevus cells are epithelioid and may exhibit cytologic atypia, such as nuclear enlargement and nucleolar prominence. Hyperchromatism is sometimes a feature. Cytologic atypia, if present, is usually seen only in a subpopulation of cells. When it involves a large fraction of melanocytes, concern for melanoma should be raised.
If a dermal component is present, it shows features similar to that of non-GTNs. In other words, it is the architectural features of the junctional component that allow distinction of GTNs from common compound nevi. The dermal component shows maturation with depth. As with the junctional component, however, the dermal component may show cytologic atypia in the superficial component.
Distinction between severely atypical genital nevi and melanoma can, in some cases, be challenging. Expansile dermal nests with diffuse cytologic atypia, lack of maturation with depth, significant pagetoid spread of intraepidermal melanocytes, effacement of the epidermis, conspicuous mitoses, and asymmetry should all prompt concern for melanoma. A potential diagnostic pitfall is the presence of concurrent lichen sclerosus and GTN because the presence of lichenoid inflammation, sclerosis, and pigment incontinence may mimic regression of melanoma. It is important to remember that melanoma of the vulva is usually seen in older women. Studies have shown that in contrast to melanoma of nongenital sites, which has a peak incidence in early to middle adulthood, vulvar melanoma has its peak incidence around the sixth decade of life. Therefore, one should approach the diagnosis of melanoma with caution in young patients and, similarly, the diagnosis of atypical nevus in older women should be rendered with caution. Nevertheless, vulvar melanoma may occur in the young, and nevi are certainly encountered in older women.
The biologic potential of GTNs has not been carefully studied. For this reason, it is recommended that lesions with significant atypia be completely excised. Although there may be some histologic overlap between dysplastic and vulvar nevi, the former is characterized by elongation of the rete ridges and a more prominent lentiginous growth pattern of junctional melanocytes. Stromal changes that favor dysplastic nevus include eosinophilic and lamellar fibrosis of the papillary dermis and a variable mononuclear inflammatory cell infiltrate.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here