Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
When practicing innovative therapy for skin cancer treatment, consider which reputable similarly situated skin cancer specialists would support that particular treatment as expert witnesses.
When a complication occurs during skin cancer treatment, maintaining the patient's trust is the key to successful patient care and is helped by availability and close communication between the dermatologist, the patient, and significant others.
Enhanced communication between skin cancer specialists and patients can mitigate malpractice pursuit.
Avoid discussing and making premature conclusions regarding an adverse event/complication in skin cancer care until all the facts are clear.
As the field of medicine evolves, awareness of the rights and responsibilities of physicians and patients is critically important to healthcare delivery. For the most part, those rights and responsibilities parallel good patient care. Yet, the current medicolegal environment in the United States has created a malpractice climate that is causing doctors to limit the care they provide to patients and sometimes leave the practice of medicine altogether. With an ever-increasing demand for documentation, some providers fall into a habit of practicing defensive medicine, focusing more on what is said than what is done. This approach compromises patient care.
While politics will determine part of the outcome of the current malpractice crisis, dermatologists can effect positive change by better understanding the legal issues involved and managing them appropriately to provide good patient care, minimize malpractice exposure, and avoid having to limit care. This chapter will explore these areas.
It is important to point out that the legal responsibilities of patients and physicians are governed by Federal and State laws and may vary from state to state. Therefore, this chapter is not a substitute for the advice of an attorney when potential or actual medicolegal issues arise.
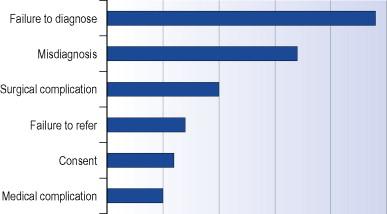
One in five dermatologists will face a medical malpractice claim in their career; however, 35% of the claims are either dropped or dismissed in favor of the physician. According to an analysis conducted on 78,712 malpractice cases, improper medical performance accounted for one-third of all claims, and the second most common medical misadventure claim was for ‘errors in diagnosis’. A significant number of claims against dermatologists are related to conditions and procedures dealing with skin cancer management and surgical procedures. Lydiatt performed lawsuit analysis on 99 cases of medical malpractice involving skin cancers. His results are summarized in Figure 63.1 .
Regardless of validity, the pursuance of malpractice by a patient requires considerable time and resources from the physician; thus, the astute provider must become familiar with basic malpractice law to minimize the initiation of lawsuits. This section discusses medical malpractice as it relates to the Tort Law of Negligence, which compensates individuals for the losses they suffer due to the unreasonable acts of another person. Negligence is the result of a breach of a duty from the standard of care resulting in harm to another person. In order for a physician to be held liable for negligence, four elements must be satisfied ( Table 63.1 ).
|
How is duty established? Consider Example 1 :
You, the skin cancer physician, are at a weekend birthday party when you are approached by another attendee who casually asks you to evaluate a ‘funny mole’ on his forearm. He asserts that if you can just tell him the mole is okay, then you would save him the hassle of going to the doctor's office, and it would assuage his wife's worries. He shows you the mole, which appears clinically to represent a benign nevus.
The above situation is all too familiar to physicians. A duty to a given patient will generally exist when the physician–patient relationship is established. This usually requires some form of interaction with the patient, which can even consist of gratuitous advice or service, and can even lack physical contact. Some may consider the providing of advice to the friend in Example 1 to establish a duty. Therefore, an example of an appropriate response in the above situation would be to confirm the benign-appearing features of this mole, but let the patient know that your assessment is limited by suboptimal lighting, and this mole would be better evaluated in the clinic, where you can perform a full history and physical examination, under proper lighting. This would meet the physician's social obligation while putting the patient on notice that (s)he should not reasonably solely rely on this interaction.
Duty may also be manifest by a patient simply having an appointment with a physician. Thus, it would be legally prudent for a dermatologist to follow up on appointments missed by patients, especially where the physician is the only one capable of providing the service.
The scope of a physician's duty is usually held to the standard of others in the ‘community’ in which (s)he practices; however, the boundaries of the community have become blurred by advances in communication technologies. It is also important to recognize that physicians are held to the standard of specialists when specialty care is given. If a physician performs a procedure traditionally performed by a specialist, the physician will likely be held to the standard of that specialty.
Breach of a duty by a physician requires deviation from the standard of care. Expert testimony is the main determination for the standard of care. Furthermore, the standard of care is subject to constant change; thus, healthcare providers have a vested interest to keep up to date with evidence-based medicine and current treatments as they evolve.
The community in which one practices influences the standard of care. For example, skin cancer specialists may disagree on the extent of the skin examination required for patients. While some specialists advocate that a full body examination is essential for every patient, others contend this is excessive for the patient presenting with a single benign lesion on the face, and places increasing economic strain on healthcare delivery. If full body skin checks are held to be the standard of care in a particular community, then dermatologists in that community who do not offer this to their patients may fail to meet the standard of care in a court of law, depending on the circumstances.
In the era of evidence-based medicine, the right thing to do for a patient may become less clear. Consider the following real-life example of a lawsuit described in the January 7, 2004 issue of JAMA ( Example 2 ):
A physician and residency program were successfully sued for not following the standard of care of the local community despite the disagreement with evidence basis. The patient was seen for routine evaluation and prostate cancer screening was discussed. Given the uncertainty of PSA (prostate-specific antigen) screening, including a high false-positive rate and significant risk to pursuance of procedures in the event of a positive screen, the patient elected not to have this performed. The patient was found to have an aggressive prostate cancer some time after this encounter and he sued this physician for not performing the PSA screen. While the defense argued evidence basis for not screening, including recommendations from the American Academy of Family Physicians, American Urologic Association and American Cancer Society endorsing the physician's approach, the patient ultimately was awarded $1 million because the standard of care of the local community was to perform PSA screening unilaterally without patient input.
This case exemplifies the need for caution when pursuing evidence-based medicine as well as following national guidelines that do not parallel local medical practice. When considering what is the right thing to do, the patient's best interest should come first. Defensive medicine should not dictate a specialist's care, but it should be noted that, should a malpractice suit ensue, it may be easier to find supportive expert witnesses when the specialist conforms to the majority path.
If one is practicing a form of innovative therapy followed by only a few practitioners, finding supportive expert witnesses may be more difficult. The wise practitioner would ensure that the innovative skin cancer approach (s)he uses has been adopted by at least some other reputable practitioners in the community who can be called upon as experts if the need arises.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here