Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Medial ligament injuries of the knee are often assumed to be only medial collateral ligament (MCL) injuries. However, the medial ligament includes not only the MCL but also posteromedial structures that play a vital role in the stability of the knee. The work of LaPrade and colleagues has demonstrated that the posterior oblique ligament (POL) is an important valgus and rotational stabilizer of the knee. The management of the MCL has evolved during the past 30 years. Most isolated MCL injuries are treated conservatively, with a rare role for surgical intervention. However, the treatment of MCL sprains with anterior cruciate ligament (ACL) injury (or any other concomitant ligamentous injury for that matter), along with the timing of ACL reconstruction, continue to be controversial. This chapter describes the anatomy of the medial knee (including the increasingly important posteromedial corner), the evaluation of the knee, the treatment of medial ligament injuries, and the role of rehabilitation.
The history will depend on whether the injury is witnessed by the physician on the sidelines or elicited from the patient in the clinic. Most of these injuries present in the office setting as potentially chronic conditions. A description of the mechanism of injury should be elicited in as much detail as possible. It is important to ascertain when the patient was hurt and how. Typically, the injury is the result of a blow to the lateral aspect of the leg or lower thigh. Up to 70% of MCL injuries in athletes are from contact mechanisms. The mechanism may be the result of a clipping injury in football or a noncontact injury from cutting, pivoting, or twisting. Skiers are prone to medial side injuries, with 60% of skiing knee injuries affecting the MCL. The majority of medial-sided knee injuries occur in competition rather than practice. In addition, it is important to ask the patients about pain, onset of swelling, ability to ambulate, the sensation of a “pop,” and the presence of a deformity necessitating a reduction, such as patellar dislocation or a more severe knee dislocation. In addition, a history of knee injuries or surgeries should be elicited because they can cloud an acute knee injury examination.
Ideally, the examination of the knee should occur at the time of injury before the onset of muscle spasm. However, most of these injuries are examined in the office setting after some time has elapsed after the injury. A thorough knee examination includes observation of the patient's gait, documentation of the neurovascular status, palpation of the knee for tenderness, swelling, and ecchymosis, and assessment of stability. The physician should follow some basic principles: (1) assess the ligaments and muscles while the patient is as relaxed as possible, (2) perform the physical examination as gently as possible, and (3) examine the uninjured knee before assessing the injured knee.
The patient's gait should be observed as the patient walks into the room or at some point during the examination. However, gait may be misleading because patients with a complete MCL tear may walk with a barely perceptible limp. Hughston and colleagues found that 50% of athletes with grade III injuries could walk into the office unassisted, and reported that a complete disruption of the medial compartment can occur “without subsequent significant pain, effusion, or disability for walking.” However, patients with an MCL tear may exhibit a vaulting-type gait in which the quadriceps are activated, allowing stabilization of the medial-sided structures during gait. This gait differs from that of a patient with an ACL or meniscus tear who may walk with a bent knee gait because of pain or an effusion. As with any orthopaedic injury, the neurovascular status of the limb should be assessed. Pedal pulses should be palpated and sensation should be assessed over the dorsum, plantar, and first web space of the foot. If a knee dislocation is a possibility, ankle brachial indices should be performed to evaluate for vascular injury. Compartments should be examined to rule out compartment syndrome. The ability to passively and actively dorsiflex and plantarflex the ankle and great toe should be assessed.
On the skin, the physician should look for edema, effusion, and ecchymosis to help localize the site of injury. It is important to differentiate between localized edema and an intra-articular effusion. Isolated MCL injuries usually have localized swelling. Hemarthrosis of the knee may indicate intra-articular pathology, such as an ACL or peripheral meniscal tear. Severe medial complex injuries with an ACL tear frequently show no evidence of effusion because the capsular rent is large enough to allow extravasation of fluid and blood. If hemarthrosis is present, the examiner should exclude other injuries such as a torn cruciate, patellar dislocation, an osteochondral fracture, and a peripheral meniscal tear. Along with assessment of swelling, palpation of the anatomic sites of attachment can provide clues to the diagnosis. The entire course of the MCL should be palpated from proximal to distal. Pain at the medial femoral epicondyle signifies injury at the femoral insertion of the MCL. With tibial-sided injuries, patients have pain along the proximal tibia around the pes anserine adjacent to the tibial tubercle. Midsubstance tears result in pain at the joint line, and such pain may also present with a medial meniscal injury, posing a diagnostic dilemma. Hughston and colleagues showed that point tenderness can accurately identify the location of injury in 78% of cases, and localized edema can identify a tear in the medial meniscus 64% of the time. A valgus injury that disrupts the MCL may also result in lateral meniscus tears or osteochondral fracture to the lateral femoral condyle or lateral tibial plateau. Therefore a thorough examination of the lateral knee should also be performed.
Valgus stress testing at 30 degrees of knee flexion is still the gold standard for assessing isolated injury to the MCL. This test should be performed with the foot in neutral rotation because increased laxity will be noted if the knee moves from internal to external rotation. To relax the hamstrings and quadriceps muscles, the thigh should rest on the examination table and the foreleg should move freely off the edge of the table at 30 degrees of flexion. The examiner then grasps the ankle and applies a valgus stress with the other hand resting on the medial side of the knee to assess the amount of opening and the quality of the end point compared with the uninjured side. The laxity of the MCL can be recorded based on a grading system or the amount of opening. The American Medical Association Standard Nomenclature of Athletic Injuries uses the following grading system : grade I, localized tenderness without laxity; grade II, increased tenderness and gapping but with an endpoint signifying a partial tear; and grade III, laxity without an endpoint indicating a complete tear. Other classification systems are based on the amount of opening with grade I, 0 to 5 mm laxity; grade II, 6 to 10 mm laxity; and grade III, over 10 mm of laxity. As described by Noyes, 5 to 8 mm of medial opening signifies a significant collateral ligament injury with “impairment of the ligament's restraining effect.” There is no consensus on which grading system is best. It is important to compare findings to the contralateral knee. After assessing the degree of opening, a repeat valgus stress should be performed with the examiner palpating the medial meniscus to assess if it subluxates in and out of the joint, indicative of injury to the meniscotibial ligament.
In addition to valgus testing in flexion, opening of the medial joint should be assessed with the knee in full extension. The cruciate ligaments, POL, posteromedial capsule, and MCL all contribute to knee stability in full extension. Asymmetric joint opening in extension compared with the contralateral side should alert the physician to the possibility of a combined MCL/POL injury with a cruciate tear. If any increased laxity is observed in full extension compared with the uninvolved knee, it is unlikely that an isolated MCL injury is present; rather, it is likely that the patient has a concomitant injury to the posteromedial capsule and POL in addition to the MCL lesion. The ACL should be assessed with the Lachman test because the pivot shift is difficult to perform as a result of guarding and the loss of the pivot axis with medial instability. In addition, the posterior cruciate ligament and lateral ligamentous structures should be examined. Along with cruciate injury, patellar instability and tearing of the vastus medialis oblique are associated with laxity in full extension. Hunter and colleagues found 18 of 40 laterally displaceable patellae on stress radiographs in patients with medial-sided injuries and a 9% to 21% incidence of damage to the extensor mechanism with medial ligament injury. In addition to valgus testing at 30 and 0 degrees, the Slocum modified anterior drawer test and an anterior drawer test in external rotation should be performed to assess for medial-sided injuries ( Table 101.1 ). Finally, varus stress testing and dial tests at 30 and 90 degrees should be performed to evaluate for lateral and posterolateral-sided knee injuries. However, it is important to note that dial testing can appear positive in patients with severe medial sided knee injuries. In this case, it is important to determine the direction of rotational instability of the tibial plateau in relation to the femoral condyles to distinguish if the positive result is due to a posterolateral knee injury or from anteromedial rotatory instability.
Radiography, arthrography, magnetic resonance imaging (MRI), and arthroscopy can provide information regarding knee injuries. Radiography with anteroposterior (AP), lateral, and sunrise views should be performed for both knees. These radiographs should be evaluated for occult fractures, the lateral capsular sign (Segond fracture), ligamentous avulsions, old Pellegrini-Stieda lesions (i.e., an old MCL injury) ( Fig. 101.1 ), and loose bodies. Stress x-rays must be performed in skeletally immature patients who have medial knee pain associated with a normal x-ray to rule out physeal injury.

In addition to ruling out physeal injuries in skeletally immature patients, stress radiography can be used to evaluate the severity of medial-sided knee injuries as well as the presence of concomitant ligament injuries. LaPrade and colleagues have noted that stress radiographs allow better objective measurements of knee instability than traditional physical exam maneuvers. However, this modality is often limited by pain in the acute setting and may be more beneficial for the evaluation of chronic injuries. Previous studies have demonstrated that normal, intact knees may have side-to-side gapping differences of up to 2 mm. Cadaveric sectioning studies have provided guidelines for expected medial gapping with stress radiographs based to the severity of injury in comparison to the contralateral knee: (1) isolated superficial MCL tear, 3.2 mm gapping at full extension and 20 degrees flexion; (2) superficial MCL and POL injury, 6.8 mm and 9.8 mm gapping at full extension and 20 degrees flexion; (3) complete medial side injury and ACL tear, 8.0 mm and 13.8 mm gapping at 0 and 20 degrees; (4) complete medial side injury and posterior collateral ligament tear, 11.8 mm and 12.6 mm gapping at 0 and 20 degrees; and (5) complete medial side injury and tears to both cruciates, 21.6 mm and 27.6 mm of gapping at 0 and 20 degrees.
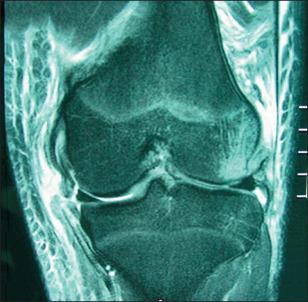
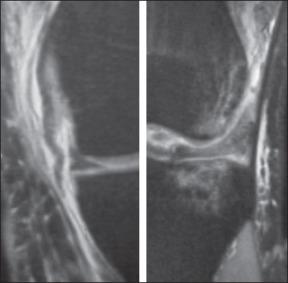
MRI without contrast is the imaging study of choice for evaluating MCL tears because it is less invasive than other studies and provides detail including location of tear, meniscal injury, superficial MCL, POL, posteromedial complex, and semimembranosus tendon ( Fig. 101.2 ). MRI can reveal a Stener-type lesion of the distal MCL with the distal MCL retracted superior to the pes tendons or into the knee joint. In addition, MRI is beneficial in assessing injuries to anterior and posterior cruciate ligaments and osteochondral structures. A 45% incidence of bruising of the lateral femoral condyle of lateral tibial plateau has been identified in isolated medial knee injuries. Loredo and associates showed that intra-articular contrast may help to highlight and to better define the structures of the posteromedial complex, but still concluded that the assessment of the posteromedial complex was difficult. They found that the posteromedial complex was best visualized on coronal and axial images. In addition, increased T2 signal extending beyond the posterior border of the superficial MCL may indicate a posteromedial corner injury. Indelicato and Linton stated that MRI can provide advantages in four circumstances: (1) when the status of the ACL remains uncertain despite physical examination; (2) when the status of the meniscus is in question; (3) when surgical repair of the MCL is indicated and localization of the tear will help limit the exposure; and (4) when an unexplainable effusion occurs during rehabilitation.

However, MRI does not always provide concrete diagnosis, and the clinical examination becomes the deciding factor. Examination after administration of an anesthetic is another tool the physician can use to assess the injury pattern in patients who present long after an injury has occurred or in patients for whom the office examination and MRI do not provide a diagnosis. Final confirmation and planning must occur at the time of diagnostic arthroscopy, which confirms under direct vision zone of injury as well as amount of opening. Upon examination with use of an anesthetic, Norwood and coworkers found that 18% of patients had anterolateral rotatory instability that was not suspected preoperatively. In addition to MRI, arthrograms can be used to evaluate meniscal disease and capsular tearing with extravasation of contrast material. Kimori and colleagues found arthrography to be more useful than arthroscopy in diagnosing tears of the meniscotibial and meniscofemoral ligaments.
With the increased use of MRI, arthroscopy is used infrequently as a diagnostic tool. ACL and meniscal tears may be identified on MRI. Also, it is rare to find an intrasubstance medial meniscal tear in an isolated MCL rupture because meniscocapsular separation occurs, and thus the fulcrum to load the medial compartment and tear the medial meniscus is lost. However, a series by Ra et al. demonstrated a 27% incidence of medial meniscus posterior root tears in patients with acute, severe medial knee instability. Over 30% of those injuries were not diagnosed on MRI and were found only during arthroscopy.
When considering treatment of the MCL, one must remember that the majority of MCL injuries heal reliably with conservative management, and treatment decisions should involve the functional demands of the knee. It is also imperative to determine the involvement of the POL in patients with MCL injuries. If the medial sided injury extends past the MCL, involving the POL and the posterior capsule, rotational laxity occurs. While the majority of people, as well as high-performance athletes, can tolerate small amounts of valgus laxity, rotational laxity is not well tolerated.
The debate continues regarding nonoperative versus surgical treatment for primary repair of the MCL/POL with concomitant ACL injury. With most MCL injuries, clinical outcomes will be satisfactory after a period of immobilization and recovery of motion and strength, followed by progressive activities. In the small subset of patients with continued pain, instability, or impaired performance, surgical management must be considered. Surgical treatment should be provided to patients with chronic symptomatic valgus instability, an MCL that is incarcerated in the joint, a distal tibial MCL avulsion that is interposed in the pes tendons (a Stener lesion), and a grade III MCL tear with rotational instability or with grade III valgus laxity in full extension resulting from a complete POL tear. Surgical management of chronic laxity of the medial structures can be quite difficult, and therefore anatomic repair of the medial support structures in the acute setting is preferred when indicated.
A review of literature for nonoperative versus operative treatment of complete isolated MCL injuries does not delineate the site of injury. The site of injury may have a role in the functional recovery of patients who place a high demand on their knees. In our practice, caring for Division I collegiate athletes, several complete soft tissue avulsions of the MCL/POL complex off the tibial insertion failed to heal reliably with nonoperative treatment. After recovery, athletes may have varying amounts of valgus knee instability preventing return to competitive sports and resulting in dysfunction in activities of daily living. Most MCL sprains should be treated nonoperatively. Complete avulsions of the superficial and deep MCL from the tibia with disruption of the meniscal coronary ligament have a poorer prognosis with nonoperative treatment and may be optimally managed with acute surgical repair for improved valgus stability of the knee.
Before proceeding with a treatment plan, it is essential to know the extent of injury. Initially we perform a thorough history and physical examination. With MCL injuries, we assess the grade of injury of the MCL and any associated ligamentous, meniscal, posteromedial corner, or patellar injuries. We obtain radiographs as a routine diagnostic tool to rule out fracture or any signs of chronic medial insufficiency (Pellegrini-Stieda lesion) and chronic ACL deficiency (the deep femoral notch sign, peaked tibial spines, or a cupula lesion). The use of MRI is dependent on the grade of the MCL lesion and associated injury posteriorly. Isolated grade I or II injuries can be diagnosed with clinical examination and do not require MRI. However, in a grade I or II injury with an indeterminate cruciate examination and effusion, we order an MRI. We also obtain MRI for all grade III injuries because the site of involvement—tibia or femur—is important in our decision-making, particularly the extent of injury to the POL and posteromedial capsule. With grade III laxity in full extension and complete involvement of the POL and capsule, avulsion of the posterior horn of the medial meniscus root may be seen ( Fig. 101.3 ) and demands surgical intervention. In addition, most grade III lesions are associated with concomitant ligamentous injuries. Our treatment algorithm is outlined in Fig. 101.4 .
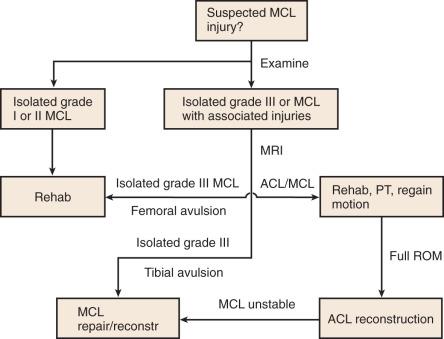
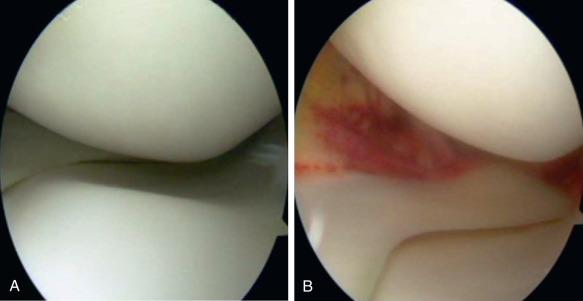
Management of grade III injuries is controversial. Even with physical examination and advanced imaging, it remains difficult to gauge the extent of damage to the POL and the posteromedial capsule in combined injuries. The treatment of grade III MCL sprains has significantly evolved. The general consensus has been to treat isolated grade III injuries conservatively. Generally agreed upon operative indications include: tibial-sided MCL injury with a Stener lesion, joint entrapment of the MCL, a medial meniscal tear requiring repair, persistent instability following a nonoperative trial, and persistent medial instability after ACL reconstruction. We believe that the treatment of grade III injury is dependent not only on the specific location of the MCL rupture but also on the degree of laxity on physical examination, as well as the degree of the arthroscopic drive-through sign. It is the posterior extension of the medial-sided injury into the POL and posterior capsule that is critically important in the decision-making in the athletically active patient. Nonoperative management of these injuries is inferior in this setting and may lead to a rotational instability in addition to valgus laxity, which is not well tolerated by athletes involved in pivoting sports.
Management of the MCL and medial-sided knee injuries can be divided into operative and nonoperative approaches. Numerous factors, including the timing, severity, location, and associated injuries such as an ACL tear need to be considered when formulating a treatment plan. The MCL has the greatest capacity to heal of any of the four major knee ligaments because of its anatomic and biologic properties. As a result of multiple biomechanical, clinical, and functional studies, the trend has been toward a conservative, nonsurgical method for the majority of MCL injuries.
Grade I and II isolated tears of the MCL generally respond well to nonoperative management. Partial tears are treated routinely with temporary immobilization and protected weight bearing with crutches. Once the swelling subsides, range of motion (ROM), resistive exercises, and progressive weight bearing are initiated. Nonsteroidal antiinflammatory drugs can be used to help with pain and swelling. Studies have shown no deleterious effect of nonsteroidal drugs on ligament healing.
Management of grade III injuries remains much more controversial. Even with physical examination and advanced imaging, it remains difficult to gauge the extent of damage to the POL and posteromedial capsule in combined injuries. Nonoperative management of these injuries may lead to a rotational instability in addition to valgus laxity, which is not well tolerated by athletes involved in pivoting sports. Grade III injuries not only involve complete disruption of its fibers but also are frequently associated with additional ligamentous injuries. Posteromedial corner injuries have been recognized as a separate entity from MCL injuries and may need to be addressed more aggressively because of rotational laxity and instability that can result from their injury.
In the last 5 years, multiple surgical techniques have been described for treating Grade III injuries. Surgical options include direct repair, repair augmented with tendon reconstruction or suture, and anatomic reconstruction. The most described reconstruction techniques in the literature include (1) triangular reconstruction of the superficial MCL and POL ; and (2) the use of two separate grafts and four tunnels to re-create the medial-sided structures. For grade III injuries requiring surgery, the reconstruction techniques addressing the POL offer improved clinical stability, restoration of knee mechanics, and lower failure rates.
We treat isolated grade I and II MCL injuries conservatively. In the first 48 hours, we encourage rest and the use of ice, compression, and elevation to help reduce swelling. In addition, we have all patients use a hinged knee brace and provide crutches for protected weight bearing. If patients have significant pain and valgus laxity, initially we lock the brace in extension. Once the swelling subsides and pain is improved, we encourage aggressive range-of-motion (ROM) exercises and straight leg raises with quadriceps exercises. Once the patient has regained full ROM and ambulation without a limp, the use of crutches and the brace can be discontinued. Stationary bicycle and progressive resistive exercises are instituted as tolerated. Once full ROM and 80% strength of the opposite side have been achieved, closed-chain kinetic exercises and jogging are allowed. Once athletes have achieved 75% of the maximal running speed, sport-specific training is allowed. Return to sports is permitted after the patient has strength, agility, and proprioception equal to the other side. We recommend a functional brace for contact or high-risk sports.
Patients with grade I sprains usually return to sports in 10 to 14 days; because immobilization is temporary, these patients regain strength and motion quickly. However, return to play (RTP) after grade II sprains is much more variable. With grade II sprains, the period of immobilization can be up to 3 weeks to allow the pain to dissipate. Therefore patients can lose more strength and motion with an increased time of immobilization compared with patients with grade I sprains. Patients are allowed to RTP when they have equal strength of both knees and no pain is experienced with valgus stress.
The treatment of grade III MCL sprains has significantly evolved during the past 20 years. The general consensus has been to treat isolated grade III injuries conservatively. We believe that the treatment of grade III injury is dependent not only on the specific location of the MCL rupture but also the degree of laxity on physical examination, as well as the degree of the arthroscopic drive-through sign. The extent of injury and laxity of the injury to the POL and posterior capsule is instrumental in our decision-making.
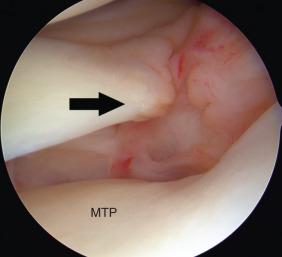
Diagnostic arthroscopy is performed initially to evaluate intra-articular injuries. A valgus force is placed on the knee while the knee is flexed at 30 degrees of flexion with the arthroscope viewing from the anterolateral portal. Tibiofemoral widening with valgus stress, which allows the arthroscope to be easily “driven through” to the posteromedial aspect of the knee, is called the “medial drive-through” sign. This indicates a medial sided injury. One can easily assess, when performing this maneuver, if the MCL injury is primarily based on the femur or tibia, and where it will be necessary to operate and perform a repair. For femoral-sided MCL injuries, the medial meniscus remains reduced with the tibia upon valgus opening (i.e., a gap forms above the medial meniscus). On the other hand, tibial-sided MCL injuries demonstrate that the medial meniscus remains reduced with the femur on valgus opening (i.e., a gap forms between medial meniscus and tibia, with the medial meniscus lifting off the tibia). If the medial meniscus elevates off the tibia, the coronary ligament, which attaches the meniscus to the tibia, is torn and should be repaired. An injury with extension to the POL and posterior capsule can also avulse the medial meniscus root from its attachment site. This also is critical to recognize and repair.
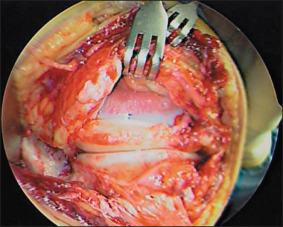
With valgus opening of the knee during arthroscopic examination, it may be observed whether the knee opens posteriorly to the medial meniscus, particularly as the knee is slowly extended with valgus load. If the capsule is exposed with this maneuver posteriorly, the patient has an injury of the POL and posterior medial capsule, which needs to be addressed at the time of surgical correction ( Fig. 101.5 ).
If the injury is acute, less than 14 days old, primary medial repair is attempted. In this setting particularly in the young athlete, repair is generally successful in the majority of cases with tibial based avulsions. For chronic injuries, the medial structures are repaired and augmented or can be primarily reconstructed.
For acute repair, the origins and insertions of the deep and superficial MCL are evaluated. Typically, the lesion is on the tibial side. Isolated femoral-sided lesions often heal reliably without surgical repair.
The surgical approach is a fairly easy one in that the incision is similar to a hamstring harvest incision, except the length of the incision is longer in the proximal direction. The surgical incision is longitudinal between the tibial tubercle and the medial aspect of the knee. This exposure is carried from the inferior margin of the superficial MCL and may be taken proximally to the femoral insertion if required. The sartorial fascia is incised to expose the MCL. The hamstrings are retracted for dissection to the distal MCL insertion on the tibia.
The initial approach is made from the inferior aspect of the lesion by placing grasping tension sutures in the entire MCL structure. Careful dissection is performed while lifting it off the tibia with a scalpel or periosteal elevator, following its course superiorly and posteriorly. Following the MCL structures superior to the medial joint line and exposing the insertion of the deep MCL results in further dissection.
Repair of the deep MCL and coronary ligament that attaches the medial meniscus to the tibia is performed by placing multiple suture anchors from posterior to anterior along the tibial joint line; four anchors with double-loaded nonabsorbable sutures are typically used.
Sutures are then passed through the deep and superficial MCL structures and tied down to the tibia while maintaining tension on the grasping sutures placed at the start of dissection. Tying of sutures to the tibial insertion is performed at 30 degrees of flexion with a varus load applied to the knee. The tibial insertion of the superficial MCL is often secured to the tibia with a large fragment screw and spiked-washer construct 6 cm distal to joint line with the grasping sutures.
Posteriorly to the repaired MCL structures, the POL and capsular tissue are reefed from multiple posterior to anterior directed sutures, typically figure of 8 sutures or horizontal mattress sutures. The objective is to take the laxity and slack out of the medial POL, which helps tighten the rotational instability caused from the injury.
Chronic medial-sided injuries are also initially assessed with arthroscopy. As previously described, the liftoff test is performed in a valgus maneuver to the knee. If the medial meniscus lifts off the tibia with valgus stress to the knee, we approach reconstruction of the tibial side. If the medial meniscus stays to the tibia with valgus stress to the knee, it is a more femoral-based injury. Surgical exposure and approach are the same as stated previously in the acute repair.
For chronic MCL injury reconstructions, if postoperative stiffness is not a concern or if the patient has an isolated MCL injury, an autograft hamstring tendon is harvested in the same surgical incision. Otherwise, the allograft tendon is used for reconstruction.
The deep MCL structures and capsule are repaired to the anatomic origin and insertion of the femur and tibia with suture anchors that are double-loaded with nonabsorbable sutures, as described previously for the acute injury repair. The tissue is reefed to remove laxity and slack in the injured structures. Augmentation with the autograft or allograft is performed once this maneuver is complete.
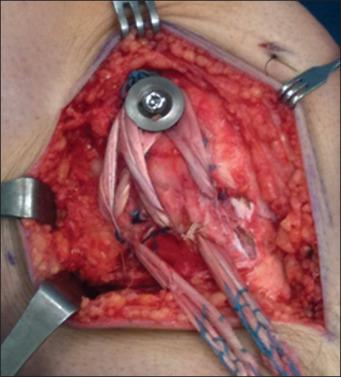
To augment the repair, autograft semitendinosus hamstring is harvested with an open-ended tendon stripper, leaving the distal attachment intact to the tibia at the pes anserine. The muscle tissue is cleaned from the semitendinosus tendon proximally with a large periosteal elevator, and a nonabsorbable whipstitch suture is placed in the free end of the tendon. All accessory attachments of the semitendinosus distally are carefully freed. A Kirschner wire is inserted at the medial epicondyle. The tendon is looped over the wire and the isometry of the tendon is evaluated with the knee in flexion and extension. If the excursion is more than 2 mm, the wire is moved to a position of isometry. Once isometry is confirmed, a large fragment screw and spiked washer are placed provisionally in the femur without fully setting the head at that isometric position of the medial femoral epicondyle. A bone trough is made around the screw shank. The tendon is looped around the screw. The screw is then tightened to the femur with the knee in 30 degrees of flexion, and varus stress is applied to the knee.
A right-angled hemostat is used to create a window in the direct head semimembranosus tendon attachment of the femur posteriorly. The free end of the semitendinosus tendon autograft is then directed posterior and obliquely and pulled through this window, recreating the central arm of the POL. The autograft is sutured to the semimembranosus tendon with use of a nonabsorbable suture.
If an allograft tendon is used, the aforementioned technique is modified, with attachment of the tibial limb of the allograft augment secured to the tibial insertion of the superficial MCL with another large fragment screw and spiked washer fixation.
A case example is that of a 16-year-old high school football player who sustained a contact MCL and ACL injury that was treated operatively in a staged fashion ( Figs. 101.6–101.8 ). After treatment, he was allowed full return to contact sports 1 year from injury. Although most femoral-sided tears can be treated successfully with conservative methods, complete tibial-sided avulsions of the deep and superficial MCL, although rare, often heal with residual laxity. In athletes who participate in level I sports, we frequently favor operative repair of these tibial-sided complete avulsions that display retraction of the deep or superficial MCL on MRI ( Fig. 101.9 ). Figs. 101.9 and 101.10 highlight a case example of a Division I football player with an isolated tibial-sided complete MCL avulsion with gross laxity and an impressive arthroscopic drive-through sign that was treated surgically.


Our rehabilitation protocol for grade III lesions is placement in a long-leg hinged knee brace locked in extension with weight bearing as tolerated on crutches for 2 weeks. After approximately 2 weeks we unlock the brace during weight bearing. In the first 4 weeks, our goal is to have the patient attain nearly full ROM and normal gait pattern with full weight bearing in a hinged knee brace, and begin quadriceps and hamstring strengthening.
In contrast, patients who undergo a repair of the MCL follow a different protocol. Postoperatively, a hinged knee brace is locked from 30 to 90 degrees for 3 weeks, followed by unlimited motion. Weight bearing is limited for 3 weeks with crutches and then progressed to full weight by 4 to 6 weeks. Bracing is discontinued at 6 weeks and nonimpact conditioning is allowed, with running started by 3 months.
Chronic laxity of the medial support structures after nonoperative management is difficult to treat. A firefighter we treated after nonoperative management of his grade III medial lesion had chronic medial instability, which for him was a significant safety issue for performance of his professional duties. Fig. 101.11 shows medial reconstruction of his POL and MCL using allograft tissue and performed anatomically as an isolated procedure for chronic medial stability.
The treatment of MCL injuries initially promotes nonoperative management; thus rehabilitation is pivotal and is the primary modality for treatment. No one perfect rehabilitation protocol exists that will work for every athlete. Upon reviewing the literature, no apparent consensus exists regarding the most efficacious rehabilitation protocol, and protocols are usually based on surgeon preference and experience. Steadman, Bergfeld, O'Connor, and Cox have had excellent success with their individual protocols for treatment of MCL injuries. To effectively treat MCL injuries, the grade of the injury must be determined because the parameters of rehabilitation are based on the degree of injury. Table 101.2 shows the general principles for rehabilitation of MCL injuries.
| Phase | Goals | Criteria for Progression |
|---|---|---|
| Maximal protection phase | Early protected ROM Decrease effusion and pain Prevent quadriceps atrophy |
No increase in instability No increase in swelling Minimal tenderness Passive ROM at least 10 to 100 degrees |
| Moderate protection phase | Full painless ROM Restore strength Ambulation without crutches |
No instability No swelling or tenderness Full painless ROM |
| Minimal protection phase | Increase strength and power |
Isolated grade I sprains are treated with rest, ice, compression, and elevation for the first couple of days to help reduce swelling. Patients are allowed weight bearing as tolerated with the use of an assistive device if pain is experienced with walking. The only exception is patients with significant valgus deformity, because they will place more stress on the MCL, affecting healing. In these patients, it may be safer to allow partial weight bearing for a couple of weeks. With grade I MCL tears, immobilization in a brace is rarely required, and if patient compliance is of concern, a short-leg hinged brace is used to control valgus and rotational stresses. ROM is begun immediately to prevent arthrofibrosis and stiffness. In addition, quadriceps strengthening and closed chain exercises are started. Once the patient regains full ROM, resistive exercises are begun along with sport-specific drills.
Isolated grade II injuries are treated similarly to grade I injuries with rest, ice, elevation, and compression. Because grade II injuries involve a greater degree of damage to the ligament with increased valgus instability, a long-leg hinged brace is usually needed. Patients are allowed to progressively bear weight as tolerated in the brace; however, if the patient is having significant pain, the brace can be locked in extension until the pain subsides, usually in 1 week. Assistive devices are used until the patient has a nonantalgic gait. Active ROM exercises are started immediately. During the early period, quadriceps strengthening is performed in a nonweight-bearing fashion with straight leg raises, quadriceps-setting exercises, and electrical stimulation. Once the patient has achieved full ROM and functional strength, proprioceptive and agility drills can be initiated.
Isolated grade III injuries usually involve disruption of both the superficial and the deep fibers. Therefore the rehabilitation process is slower, and a longer period of immobilization is required.
The treatment of grade III injuries can be divided into stages. In the first phase (for about 4 weeks), the patient should wear a brace locked in extension, and progressively increase weight bearing to attain a normal gait pattern. Also, the patient needs to perform ROM exercises with eccentric strengthening of the quadriceps and hamstrings. Failure to perform ROM exercises and prolonged immobilization results in increased ligament creep and poorer cellular metabolism. In phase II, which lasts 4 to 6 weeks, the patient continues to attain full ROM, unlocks the brace, and achieves quadriceps and hamstring strengthening. After 6 weeks, the brace can be discontinued if the patient has a nonantalgic gait and has regained quadriceps strength for daily ambulation. Phase III starts after 6 weeks and includes squatting, light jogging with agility drills, and continued strengthening to return to sports.
After surgical repair of an isolated MCL, the brace is locked at 30 degrees and the patient is allowed to perform toe-touch weight bearing for 3 weeks. The patient is encouraged to continue ROM from 30 to 90 degrees. The patient also continues strengthening of the quadriceps and hamstring while wearing a brace. If possible, we prefer to add a compression cryotherapy device (such as a Game Ready, Concord, Georgia, USA) as ACL studies have demonstrated improved knee ROM and functional scores with the use of compression cryotherapy compared to cryotherapy alone. After 3 weeks, the patient is allowed to progress to full weight bearing with full-time brace wear to continue to protect the repair. The brace can be worn unlocked to allow free ROM, as well as valgus and rotational stability. From 3 to 6 weeks, the goal is to restore full ROM along with continued strengthening with closed kinetic chain exercises. After 6 weeks, the patient continues to progressively increase activities with resistive and sport-specific exercises.
Combined injuries of the MCL and ACL require additional steps compared with the rehabilitation of isolated MCL tears. Upon reviewing the literature on ACL and MCL injuries, as stated previously, conservative treatment of MCL injuries followed by surgical reconstruction of the ACL is the favored management in most patients. Initially the protocol focuses on the severity of the MCL injury. For example, a grade I MCL injury with an ACL injury will proceed with the protocol presented earlier for grade I injuries. The patient will quickly regain ROM and functional strength, and then the surgeon can proceed with reconstruction of the ACL. Conversely, the patient with a grade III injury with an ACL injury will take much longer to heal because of the slower protocol for type III injuries. Regaining ROM and functional strength training may take 8 to 10 weeks, and therefore it will take longer to proceed with ACL reconstruction with a type III injury. The ACL is reconstructed accompanied by conservative treatment of the MCL, following the rehabilitation protocol for an ACL reconstruction. After a combined ACL reconstruction and medial-sided repair, the knee is braced in full extension, and a standard ACL protocol is followed with protected weight bearing. In a combined ACL and MCL injury, it is important to remember that ACL rehabilitation takes precedence over medial-sided repair.
For RTP guidelines, see Box 101.1 .
Full ROM
No instability
Muscle strength 85% of contralateral side
Proprioception ability is satisfactory
No tenderness over the medial collateral ligament
No effusion
Quadriceps strength; torque/body weight
Use of a lateral knee brace (if necessary)
ROM, Range of motion.
Numerous authors have shown excellent results with nonoperative treatment of grade I and II MCL tears. Ellsasser and associates looked at 74 knees in professional football players and achieved a 98% success rate with a nonoperative protocol. They had strict inclusion criteria to ensure an isolated MCL injury was present: (1) up to grade II laxity with a firm end point in flexion, (2) no instability to valgus stress in extension, (3) no significant rotatory or AP subluxation, (4) no significant effusion, and (5) normal stress radiograph findings. In this series, patients were treated with crutches, no brace, and progressive weight bearing. Based on their experience, Ellsasser and associates concluded that by 1 week, patients should progress to full extension, have no effusion, and perceive decreased tenderness. The players returned to football in 3 to 8 weeks. The only failure occurred in a patient with an osteochondral fracture that was found at later follow-up.
Derscheid and Garrick performed a prospective study that examined 51 grade I and grade II MCL injuries in college football players. They used a nonoperative rehabilitation protocol with a knee immobilizer initially. Players with a grade I injury returned to full participation at an average of 10.6 days, and players with a grade II injury returned at an average of 19.5 days. At long-term follow-up, these patients showed slight increases in medial instability. Injured knees had a higher incidence of reinjury than did control knees, but this finding was not statistically significant. Bassett and associates and Hastings studied the use of a cast brace in treating isolated MCL ruptures. In both studies, early return to athletics was found with the use of the cast brace. Nonoperative treatment varies from casting to functional bracing to no bracing, and good outcomes occur with all three forms of treatment.
Fetto and Marshall found an 80% incidence of concomitant ligamentous injuries with a grade III MCL tear, with 95% of the associated injuries being an ACL tear. Early authors recommend primary repair for grade III injuries. O'Donoghue stressed the importance of immediate repair of complete tears of the MCL. Hughston and Barrett supported primary repair of all medial structures, including the superficial MCL and POL. They believed that repair and advancement of the POL was key to restoring medial stability. Their results were good to excellent in 77% to 94% of patients. Muller reported 65% good and 31% excellent results in the repair of isolated grade III MCL injuries. He repaired the superficial MCL avulsion with screws and washers and intrasubstance tears with a combination of approximation and tension-relieving sutures. Hughston and Barrett, O'Donoghue, Muller, Collins, Kannus, LaPrade and Wijdicks have written that surgical intervention is necessary for complete ruptures of the MCL.
Although good results have been demonstrated with surgical repair of the MCL, many studies have focused on the nonoperative management of grade III MCL injuries. Fetto and Marshall were among the first to assess outcomes after nonoperative treatment of grade III MCL injuries. They studied 265 MCL injuries and found that patients with grade II injuries did much better than patients with grade III injuries (97% compared with 73%). Initially, in their study, all patients with grade III injuries underwent operative intervention. However, some patients with grade III injuries did not have an operation because of skin lesions and infection. At follow-up, patients with operative treatment of isolated MCL ruptures had no improved outcome compared with the nonsurgical group. This incidental finding led the way for more prospective studies to investigate the role of nonoperative treatment in patients with isolated grade III MCL injuries.
Indelicato prospectively compared operative and nonoperative treatment of isolated grade III ruptures. All patients underwent examination with the use of an anesthetic and arthroscopy to rule out any other pathology, such as ACL and meniscal tears. Indelicato found objectively stable knees in 15 of 16 patients treated operatively and in 17 of 20 patients treated nonoperatively. Both groups followed a rigid rehabilitation protocol including casting at 30 degrees of flexion for 2 weeks and then 4 weeks longer in a cast brace with hinges that allowed motion from 30 to 90 degrees. Subjective scores were higher in the nonsurgical group, with good to excellent results for 90% in the nonsurgical group and 88% in the surgically repaired group, suggesting that surgical intervention offered no benefit. Indelicato also showed that patients treated with early motion returned to football 3 weeks earlier than did immobilized patients. A subsequent study by Indelicato and associates showed that a conservative approach in patients with complete MCL ruptures was successful in collegiate football players. All players were managed with a functional rehabilitation program, and 71% had good to excellent results.
Similar to Indelicato, both Reider and colleagues and Jones and associates found excellent outcomes in athletes with isolated grade III medial ligament injuries who were treated conservatively and agreed that nonoperative treatment of these lesions is justified. Reider and colleagues studied 35 athletes who were treated with early functional rehabilitation for isolated grade III tears. Of these 35 athletes, 19 returned to full and unlimited activity in less than 8 weeks. At an average follow-up of 5.3 years, outcomes based on subjective and objective measurements were comparable with earlier investigations using a surgical repair. In 1986, Jones et al. reported results for 24 high school football players who returned to competition at an average of 34 days. Management consisted of 1 week of immobilization followed by gradual ROM and strengthening. The knee was tested weekly with valgus stress, and instability was reduced to grade 0 or 1 by 29 days. No increased incidence of reinjury was found the following spring.
Although Indelicato, Fetto and Marshall, Jones et al., and Reider et al. found excellent results with nonoperative treatment, Kannus studied 27 patients with grade III lesions at an average 9 years of follow-up. Patients were found to have poor outcomes (an average Lysholm score of 66) and degenerative changes on radiographs. Kannus concluded that early surgical repair would prevent deterioration. A careful review of the patients showed that 16 of 27 had greater than a 2+ Lachman score, and 10 of 27 had anterolateral instability. Thus this study did not show that nonoperative treatment has poor outcomes but that associated injuries, such as ACL injuries, need to be addressed to prevent poor long-term outcome.
In the last decade, anatomic restoration of the medial knee structures has been found to provide satisfactory outcomes. Lind et al. described a technique to reconstruct the MCL and POL. The clinical results they published showed that 98% of their patients treated with this technique had normal or near normal International Knee Documentation Committee (IKDC) measures at follow-up of more than 2 years.
LaPrade and associates reported their technique and follow-up at an average of 1.5 years for reconstruction of the MCL and POL. Their outcomes showed improved IKDC measures and decreased valgus opening on stress radiographs.
Several cadaveric studies of anatomic MCL reconstruction have been recently performed. Wijdicks and associates performed a cadaveric biomechanical study comparing augmented repair versus reconstruction of a completely transected superficial MCL. The MCL was reconstructed via the LaPrade method. Compared to the transected state, augmented repair and reconstruction both decreased medial gapping. However, the authors noted that neither technique reproduced the stability of the intact ligament. Gilmer et al. performed a cadaveric analysis comparing a repair of the MCL and POL versus a repair with internal bracing versus LaPrade's allograft reconstruction technique. They found that the mean moment to failure was highest in the intact ligament. Augmentation with internal bracing improved moment to failure and valgus angle at failure compared to repair alone, and was similar in comparison to allograft reconstruction. Finally, Omar and colleagues performed a biomechanical analysis of fixation techniques for use in augmented repair. Spiked polyetheretherketone washers (PEEK) reinforced with polyester sutures provided the best results with regard to elongation during cyclic loading and load to failure.
Combined injury to the MCL and ACL represents a completely different entity than an isolated MCL injury. The ACL is a primary restraint to anterior displacement and acts as a secondary stabilizer to valgus stress, especially in full extension. Conversely, the MCL is the primary restraint to valgus stress at 30 degrees of flexion. Therefore injury to the MCL and ACL results in both anterior and valgus instability and can significantly compromise knee function. Even though the apparent consensus is that a solitary MCL rupture can be treated nonoperatively, the optimal treatment for a concurrent ACL and MCL injury is debated. The extent of involvement of the posteromedial capsule and POL may help to guide treatment strategies.
The management of combined ACL and MCL injuries has been a controversial topic in the literature. The first issue pertains to the various surgical options available for managing these injuries. Three principal surgical options exist: (1) surgical reconstruction and repair of both ligaments; (2) ACL reconstruction and nonoperative MCL management; and (3) operative management of MCL with nonoperative ACL treatment. ACL reconstruction with nonoperative management of the MCL remains the most popular option. The second controversial issue regarding combined injuries is whether early or late ACL reconstruction provides better functional and long-term results.
In years past, authors recommended surgical intervention for both ligamentous structures in concomitant ACL and MCL ruptures. Fetto and Marshall had 79% unsatisfactory outcomes in patients treated operatively for ACL and MCL tears. Even though studies have shown that operative repair of all ligaments results in stable, functional knees, a high incidence of knee stiffness was found. Other authors have stated that isolated operative MCL repair and nonoperative ACL reconstruction leads to good results. Hughston and Barrett reported that 94% of their patients with combined ACL and MCL injury who were treated with only MCL reconstruction returned to their preinjury levels of athletic performance. They stated that the key to obtaining excellent results was reconstruction of the POL and posteromedial structures. Noyes and Barber-Westin criticized the method used by Hughston and Barrett to report results, and stated that the results may have been overly optimistic. However, Hughston continued to report good results at 22 years of follow-up. In addition to Hughston, Shirakura and associates reported excellent results in 14 patients with combined lesions but reconstruction of the MCL only; however, they did not report AP instability. Conversely, Frolke and coworkers reported poor results with solitary MCL repair. They performed arthroscopically guided repair of the MCL, which led to functional stability in 68% of knees, but clinical testing of all 22 knees showed abnormal or severe abnormal examination findings. More recently, Pandey and associates found higher IKDC scores, higher Lysholm scores, and fewer complaints of instability in patients with combined injuries who underwent repair of the MCL and POL as well as ACL reconstruction compared to patients who underwent repair of medial sided structures only.
Most authors suggest that nonoperative treatment of the MCL with reconstruction of the ACL provides good to excellent results. Shelbourne and Porter demonstrated good to excellent results in 68 patients with ACL reconstruction and nonsurgical management of an MCL tear. They also showed that these patients achieved a greater ROM and more rapid strength gains than did patients with surgical reconstruction and repair of both ligaments. Similarly, Noyes and Barber-Westin demonstrated a higher incidence of motion problems when MCL and ACL were treated operatively, and they recommend arthroscopic reconstruction of the ACL with nonoperative management of the MCL after recovery of ROM and muscle function. In a prospective randomized study, Halinen and associates treated 47 consecutive patients with combined ACL and grade III MCL injuries. All patients underwent early ACL reconstruction within 3 weeks of injury. The MCL was treated operatively in 23 patients and nonoperatively in 24 patients. All patients were available for follow-up at a mean of 27 months. The nonoperative treatment of the MCL led to results similar to those obtained with operative treatment with respect to subjective function, postoperative stability, ROM, muscle power, return to activities, and Lysholm score. Halinen and colleagues concluded that MCL ruptures did not need to be treated operatively when the ACL was reconstructed early.
In a retrospective study, Millett and colleagues reported on 19 patients with a complete ACL injury and a minimal grade II MCL tear who underwent early ACL reconstruction and nonoperative treatment of the MCL. At the 2-year follow-up, subjective evaluation showed a Lysholm score of 94.5 and a Tegner activity score of 8.4. Clinical examination revealed good ROM and strength. None of the patients experienced graft failure or required subsequent surgery.
More recently, there has been increased interest in anatomic repair or reconstruction of combined injuries. Piatkowski et al. examined the primary repair of grade III MCL injuries with delayed reconstruction of ACL tears. Good to very good outcomes were achieved in 63% based on IKDC scores, and good outcomes were achieved in 74% based on the Lysholm scale. They noted that patients over 40 years of age were less likely to have good outcomes. Blanke et al. presented a case series of patients who underwent screw and suture repair of grade II MCL injuries at the same time as ACL reconstruction. The chronicity of the injuries was not reported. At the 9-month follow-up, all five patients had grade A IKCD medial instability and postop instability scores. The average Lysholm score was 94.6. Zhang et al. also examined simultaneous ACL reconstruction and MCL reconstruction. The patients in their series had a mean time from injury to surgery of 7.6 months. At 40 months follow-up, they noted significant decreases in valgus laxity with normal to near normal mean gapping on stress radiographs. The presence of anteromedial rotatory instability decreased from 71% preoperatively to 0% postoperatively. Patients’ IKDC scores improved postoperatively to a mean of 87.7. One patient had loss of flexion over 15 degrees.
Dong and colleagues performed a randomized, controlled trial comparing anatomic ligament repair to triangular reconstruction in patients with acute grade III MCL injury and concomitant ACL tears. No significant differences in valgus instability, knee ROM, return to sport, functional scores, or flexion/extension deficit were noted between groups. The reconstruction group had significant decreases in anteromedial rotatory instability (9.4% vs. 34%). The primary repair group had a nonstatistically significant increase in medial knee pain, four ACL re-ruptures, and two patients undergoing revision for continued medial instability. One patient in the reconstruction group underwent revision reconstruction of the MCL secondary to hardware failure, and another patient underwent surgical release for arthrofibrosis.
Dong et al. also retrospectively reviewed outcomes of triangular ligament reconstruction in patients with isolated grade III MCL injuries and those with concomitant ACL injuries who had failed 6 months of nonoperative treatment. In both groups of patients, medial instability and the presence of anteromedial rotatory instability significantly improved. A total of 58.9% of patients had Grade A IKDC scores and 35.7% had grade B IKDC scores. However, patients with concomitant MCL and ACL reconstruction were more likely to have extension deficits at final follow-up.
Finally, in a systematic review of MCL and posteromedial corner techniques, Delong and associates report that 76% of MCL repair cases in the literature had a concomitant ACL reconstruction. A total of 75% of cases in the systematic review had medial laxity less than grade I at final follow-up, and the average Lysholm score was 91.6.
Another controversial issue regarding combined ACL and MCL injury is whether early or late ACL reconstruction provides optimal return of function and long-term results. Based on animal studies, MCL healing is adversely affected by ACL insufficiency, and therefore it has been proposed that early ACL reconstruction will improve healing of the MCL. Both Halinen and colleagues and Millett and associates showed good subjective scores and minimal loss of motion complications with early ACL reconstruction (within 3 weeks). Conversely, Petersen and Laprell demonstrated poorer results with early ACL reconstruction compared with late ACL reconstruction in combined injuries. All patients underwent nonoperative treatment of MCL injury, with early ACL reconstruction performed within 3 weeks of injury and late ACL reconstruction after a minimum of 10 weeks. The late reconstruction group had a lower rate of loss of motion and higher Lysholm scores compared with the early reconstruction group.
The literature supports nonoperative treatment of the MCL tear with surgical reconstruction of the ACL, and most surgeons are currently following this protocol. However, early versus late reconstruction continues to be a subject of debate, with studies supporting both points of view. Other factors, such as preoperative and postoperative rehabilitation protocol along with bracing, may need to be further analyzed to help assess whether early or late reconstruction is more beneficial.
Complications of MCL ruptures are rarely reported in the literature. Failure to diagnose associated ligament injuries, such as ACL, can lead to long-term instability and degenerative problems. Failure to recognize and repair all injured medial and posteromedial structures can also lead to residual instability. In addition, missed associated meniscal tears and articular cartilage defects can lead to continued pain. Atrophy and arthrofibrosis are rare complications given the aggressive rehabilitation protocols with early motion and strengthening. Infection is a rare complication with surgical reconstruction. Persistent pain and Pellegrini–Stieda lesions can occur after MCL sprains, usually near the femoral origin in the region of the medial epicondyle. Treatment consists of a local injection or antiinflammatory medication, and resection of the lesion may be required for relief. In addition to pain, patients with femoral-sided lesions are more prone to have loss of motion and associated stiffness.
As with most topics within orthopaedic surgery, basic science knowledge is ever increasing. The avenues for future research are vast in the areas of chemistry, biology, and biomechanics. Our understanding of cellular processes allows us to alter the progression of injury or speed up the restoration of health.
Collagen healing is currently being investigated for the ligaments of the knee. Enzymatic processes in the inflammatory process of ligament injury and healing are plentiful. Research into the MCL and ACL response to a procollagen growth factor and transforming growth factor-β1 is ongoing. In addition, newer research has explored different expressions of lysyl oxidases in ACL and MCL tissue in response to transforming growth factor-β1 and TNF alpha. This research is furthering the investigation into the role of procollagen processes of ligament healing.
The past decade has seen an increase in anatomic and biomechanical studies of the structures of the knee. Data from these and future studies will continue to influence surgical techniques. Finally, the majority of the literature consists of studies level 3 or below in evidence. Future level 2 and higher studies would help provide answers to many of the controversies regarding medial-sided knee injuries.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here