Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Management of patients with a breast abscess is an art, and each abscess has unique features that require familiarity by the treating physician. Breast abscesses can be frustrating for both the patient and the surgeon. Even for patients referred with chronic, recurring abscesses, the surgeon should initially repeat the breast conservative treatment that may have failed in the past, the purpose of which is to “get to know” the abscess and the patient. Knowing the personality of the patient is important because, on rare occasions, a simple mastectomy may be the last alternative to the patient’s ability to live without recurrent breast abscesses.
Mastitis is an inflammation of the breast tissue that may or may not be accompanied by infection . An infection of the breast parenchyma that goes unnoticed or untreated can eventually develop into an abscess. Patients with acute mastitis and abscess formation often represent a diagnostic and therapeutic challenge. Some abscesses drain spontaneously, and others require intervention that can include needle aspiration, incision and drainage, or excision. There is currently no consensus on optimal management strategies. The principles that guide successful diagnosis, evaluation, and management of various types of primary breast infections are discussed in this chapter.
Patients with acute breast infection typically present with one or more of the following symptoms: skin erythema, palpable mass, tenderness, fever, and/or pain. Breast abscesses may occur in both the lactational and nonlactational settings. Breast abscesses have been most commonly reported to occur in women between 20 and 50 years of age. However, breast infections have also been reported in men, postmenopausal women, and children. Postmenopausal patients with a breast abscess often have a more indolent presentation and may lack many of the classical findings of a traditional breast abscess. Abscesses may occur either centrally (subareolar or periareolar) or peripherally in the breast, usually in the upper outer quadrant where a majority of breast tissue is located. Breast infection can result from recent surgery, tattoos, or nipple piercing, but most causes are unknown. The incidence of breast infection associated with surgery is 5% to 10% and with nipple piercing is estimated to be as high as 10% to 20% in the months after the procedure.
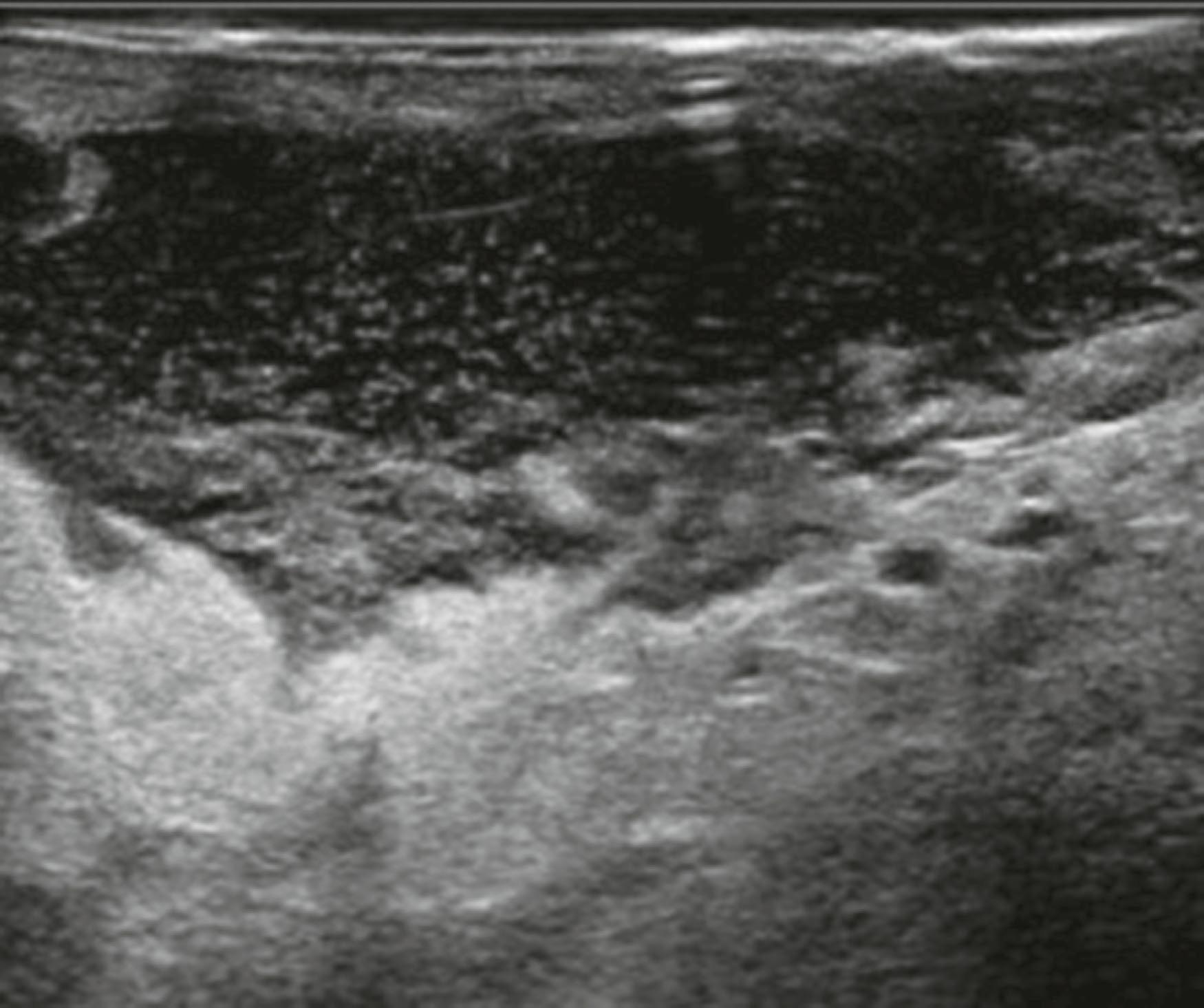
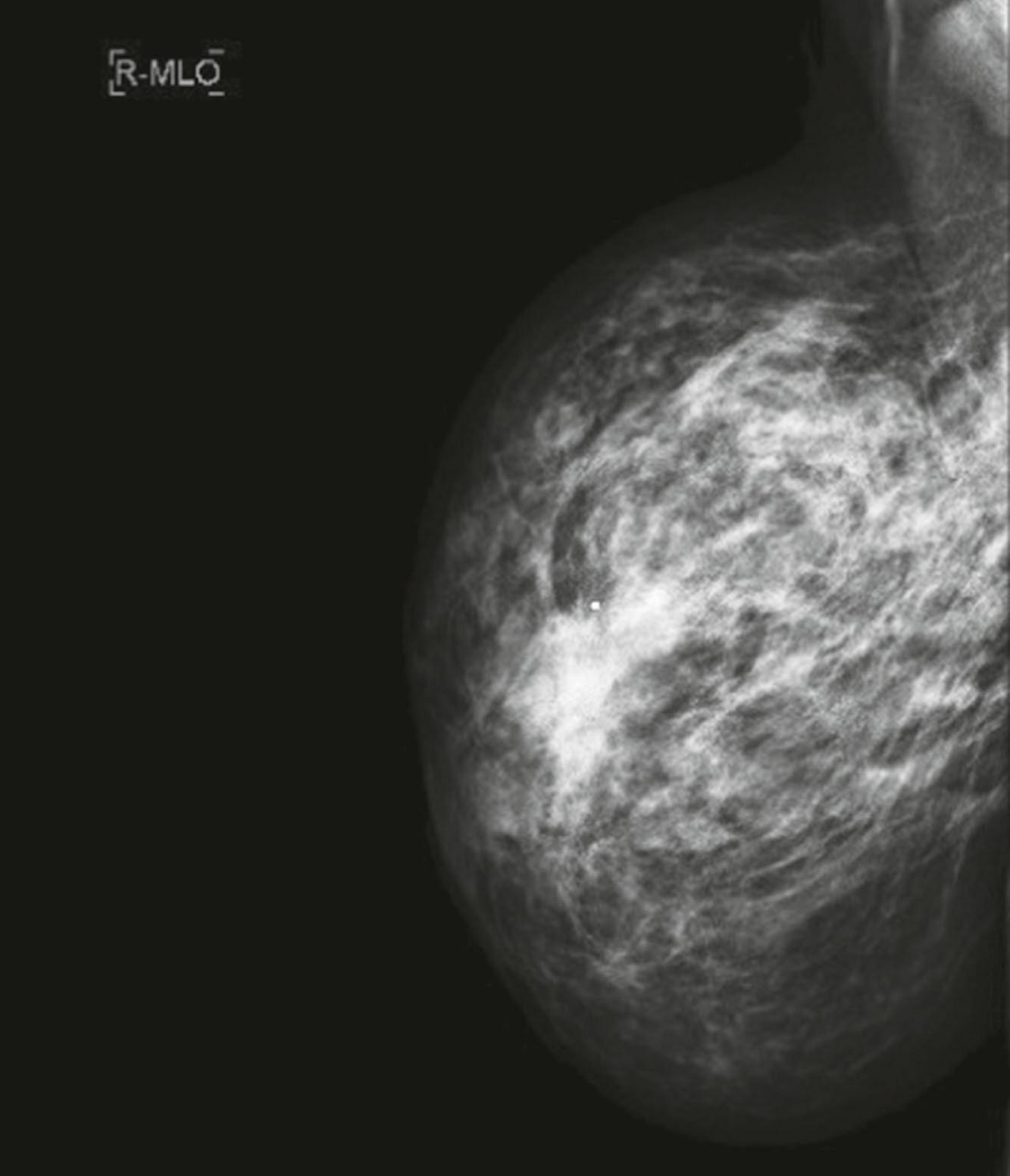
Careful clinical examination is the cornerstone of diagnosis for acute breast infection. Findings on examination can include a mass, erythema, skin warmth, skin thickening, and tenderness ( Fig. 15.1 ). Ultrasound is a useful modality as an adjunct to physical examination to evaluate for the presence or absence of an associated underlying abscess. Additionally, ultrasound can help to identify the size and depth of the abscess cavity, as well as the presence of multiple abscesses, which may not be appreciated on physical examination ( Fig. 15.2 ). Many patients with a breast abscess also have abnormal mammograms with nonspecific findings, including an irregular mass, focal asymmetry, diffuse asymmetric density, circumscribed mass, or architectural distortion ( Fig. 15.3 ). These findings in the acute setting may be difficult to differentiate from those findings associated with malignancy. In addition, in the acute setting of suspected breast infection, mammography is often not possible, secondary to breast pain and tenderness. Importantly, in cases of atypical presentation or patients with recurrent, nonimproving symptoms, a mammogram should be performed to rule out inflammatory breast cancer. After successful medical, percutaneous, or surgical management and resolution of an acute breast infection or abscess, mammography to exclude an underlying or associated malignancy and to ensure complete resolution is recommended.

In the management of breast abscess, particular attention should be given to obtaining cultures for specific pathogens to help guide treatment decisions. Staphylococcus aureus is the most common organism associated with breast abscess. Recently, an increase in methicillin-resistant S. aureus has been detected in community-acquired breast infections. Other commonly reported causative organisms include Pseudomonas aeruginosa , Staphylococcus epidermidis , Proteus , Serratia , Bacteroides , and Kelbsiella . Of note, 20% to 40% of breast abscesses are found to be sterile on culture. Cigarette smoking has been associated with increased rates of anaerobic breast infections and increased rates of recurrent breast abscess. Pathologic organisms that have been documented after nipple piercing include aerobic, anaerobic, and mycobacterial infections. A variety of unusual pathologic organisms have been documented in association with breast abscess, including Actinomyces species, Brucella , Mycobacterium tuberculosis , Fusarium solani , Echinococcus , and Cryptococcus . Many of these unusual infections are endemic to specific areas and specific patient populations, and they require special consideration in the appropriate clinical setting. Necrotizing soft tissue infections and gangrene of the breast have been reported in association with anticoagulant treatment and trauma, and in the postpartum period.
Ultrasound is useful for the detection of an intramammary fluid collection in patients who present with signs and symptoms of mastitis and are clinically suspected of having an underlying breast infection or abscess. For patients with no fluid or a small fluid collection seen on ultrasound, a trial of oral antibiotics is warranted. Initial choice of antibiotics is best directed by local antibiograms and to cover the most common pathogen, S. aureus . Antibiotic recommendations include cephalexin 500 mg four times daily, dicloxacillin 500 mg four times daily, and/or clindamycin 300 mg four times daily, with the optional addition of metronidazole 500 mg three times daily for 7 to 10 days’ duration. Failure to improve should prompt further evaluation with repeat ultrasound to evaluate for the development of an intramammary fluid collection requiring an alteration in the management strategy. In some cases, a tissue biopsy may be necessary to exclude malignancy. The patient should be scheduled for regular follow-up appointments until the infectious process has completely resolved.
The traditional initial treatment approach of surgical incision and drainage of a breast abscess has been replaced by needle aspiration. Aspirated material should always be sent for microbiological analysis to allow for adjustments of the antibiotic regimen accordingly. Warm compresses placed over the abscess are recommended for comfort.
Numerous authors have suggested aspiration of breast lactational and nonlactational abscesses as the primary management. Benefits of aspiration as an initial management strategy include improved cosmesis, lack of requirement for general anesthesia, no requirement for wound packing, and decreased cost. It has been reported to be successful in 54% to 85% of cases. The described aspiration technique of several authors involves use of a 16-gauge needle (or larger if necessary) with aspiration and irrigation of the cavity through an area where the skin is not thinned from inflammation. Use of ultrasound to guide aspiration may be helpful and is associated with higher rates of success, but this is not essential, especially in superficial lesions. The addition of oral antibiotics is a necessary component of initial therapy for breast abscess managed with aspiration. Cultures of aspirated fluid may be useful to guide antibiotic choice. Although some authors have suggested sending abscess fluid for cytology to exclude malignancy, the value of this practice is not well defined and not widely recommended. Some authors have advocated instillation of antibiotics or saline irrigation into the abscess cavity ; however, this practice is not widely accepted, and its benefit has not been clearly demonstrated. Some have advocated placement of an indwelling drain at the time of aspiration, but this is also not routinely recommended. After initial management, patients should undergo at minimum biweekly clinical reassessment to determine resolution of the abscess or subsequent requirement for additional treatment (repeat aspiration or surgical drainage). Median time to resolution of breast abscess with aspiration is approximately 2 weeks (range, 1–8 weeks). Reported success rates for the aspiration technique are highest with repeated, multiple aspirations. Successful treatment for single and multiple aspirations of breast abscess are 57% to 79% and 90% to 96%, respectively. Patients who fail to improve with multiple aspirations or whose clinical condition deteriorates require surgical incision and drainage. Factors that have been associated with failure of aspiration include large size (>3 cm) and the presence of multiple loculations.
Surgical intervention in the form of incision and drainage should be performed for an abscess that has failed repeat aspiration. As with needle aspiration, this technique can be performed in the outpatient setting with use of minimal conscious sedation or local anesthetic. Use of conventional local anesthetic agents (e.g., lidocaine) is seldom effective in providing adequate local analgesia for the incision because of the low tissue pH in the inflamed skin tissue fluid, but should still be used. Additional options to make the patient comfortable include oral sedation in the office, administration of intravenous/intramuscular conscious sedation in the emergency department, or performing the procedure under general anesthesia in the operating room.
To perform incision and drainage, the incision should be made over the site of maximum fluctuance and kept within Langer’s lines for optimal cosmesis. The abscess cavity should be explored and all the loculi and septations broken down using either finger fracture technique or a hemostat. The abscess may be extensive or multilocular and must be drained completely, taking care not to excise the surrounding indurated tissue so as not to destroy surrounding breast tissue or disfigure the breast. The purulent material should be cultured for both aerobic and anaerobic bacteria, and a Gram stain should be performed. In the appropriate age group, a biopsy specimen of the abscess wall should be taken to rule out carcinoma. The abscess cavity should then be irrigated with normal saline solution. After irrigation of the abscess cavity, a gauze wick packing is placed to assist drainage and prevent premature skin closure. Tight packing should be avoided because it can cause necrosis of the tissue and overlying skin. Postprocedurally, antibiotics should be continued. The patient should be scheduled for biweekly follow-up appointments until the process has resolved. Final follow-up should include an ultrasound to document complete resolution.
The traditional approach to the large, chronic, deep breast abscess involves taking the patient to the operating room for surgical incision and drainage with disruption of septae and open packing of the wound to heal by secondary intention ( Fig. 15.4 ). Options to consider include use of operative ultrasound to identify all subclinical abscess pockets in the breast, pulse lavage, antibiotic-impregnated irrigation (such as gentamycin), and finger fracture or a hemostat to break up intervening loculations in the abscess cavity, packing the wound open with normal saline or iodine-soaked gauze or placement of a temporary dwelling Penrose drain. Planned return trips to the operating room and frequent follow-up should also be considered.

Limitations to this approach include need for general anesthesia; high cost of performing surgery in an operating room; and the patient’s understanding of potential prolonged healing, need for frequent packing/dressing changes, close follow-up, and risk of cosmetic deformity and recurrence. In addition, surgical incision and drainage have been associated with recurrence rates of between 10% and 38% requiring additional procedures.
Principles of management of necrotizing soft tissue infection of the breast are similar to necrotizing soft tissue infections of other areas and include early diagnosis, early and aggressive surgical management, and systemic antibiotics. Because necrotizing soft tissue infections are most commonly polymicrobial in etiology, broad-spectrum antibiotics represent the best initial choice of antimicrobial coverage.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here