Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vascular anomalies are often poorly managed for a number of reasons: they are uncommon (other than the true infantile hemangioma), their mode of presentation is extremely variable, their classification has been very confusing and is still poorly understood by the majority of doctors, and their treatment is challenging. The interested interventional radiologist is in an ideal position to play a major, if not the lead, role in patient management. So many aspects of assessment and treatment require radiologic input, and it is essential that this involvement start at the time of referral and the patient’s first visit to the outpatient clinic. It is not good practice for a radiologist to accept a referral for endovascular treatment of a vascular malformation without first assessing the patient.
For a clinician familiar with these anomalies, the diagnosis is almost always straightforward. A thorough patient history and physical examination usually make it clear which patients require, and are likely to benefit from, treatment. Patients and referrers are invariably keen for definitive intervention to cure what are often highly disfiguring or lifestyle-limiting conditions, but most vascular malformations cannot be cured, and the aim of any intervention is usually long-term symptom control. The radiologist’s role is as much that of gatekeeper as interventionalist, stressing the current limitations of medical science, advising against heroic and often fruitless major intervention, and helping patients come to terms with their condition. A holistic approach is key, and the care of a patient with a vascular anomaly is ideally undertaken by a multidisciplinary team.
In 1982 Mulliken and Glowacki proposed what was at that time a very new way of classifying vascular anomalies. Their system has been modified very little since then, with only minor changes made by the International Society for the Study of Vascular Anomalies when it was established in 1992. This is now the most widely recognized system in use, encouraging management based on underlying histology and natural history of the lesion subtypes. The dichotomous Mulliken and Glowacki classification separates vascular tumors from vascular malformations. The vascular tumor arm includes the common infantile hemangiomas as well as rarer congenital hemangiomas and other vascular tumors, many of which are high flow. The vascular malformation arm comprises low-flow venous and lymphatic malformations and high-flow arteriovenous malformations (AVMs) ( Table 18.1 ).
| Type | Characteristics |
|---|---|
| Infantile hemangioma |
|
| Congenital hemangioma | Present at birth |
| Noninvoluting |
|
| Rapidly involuting |
|
| Other Types | |
| Tufted angioma | |
| Kaposiform hemangioendothelioma | |
| Pyogenic granuloma | |
Most vascular tumors are infantile hemangiomas, which occur in up to 12% of Caucasian infants by the age of 1 year. Congenital hemangiomas share some of the characteristics of the common infantile lesions but have different natural histories. Other tumors in this arm of the classification system are rare but are more likely to involve interventional radiology. These include tufted angiomas and kaposiform hemangioendotheliomas.
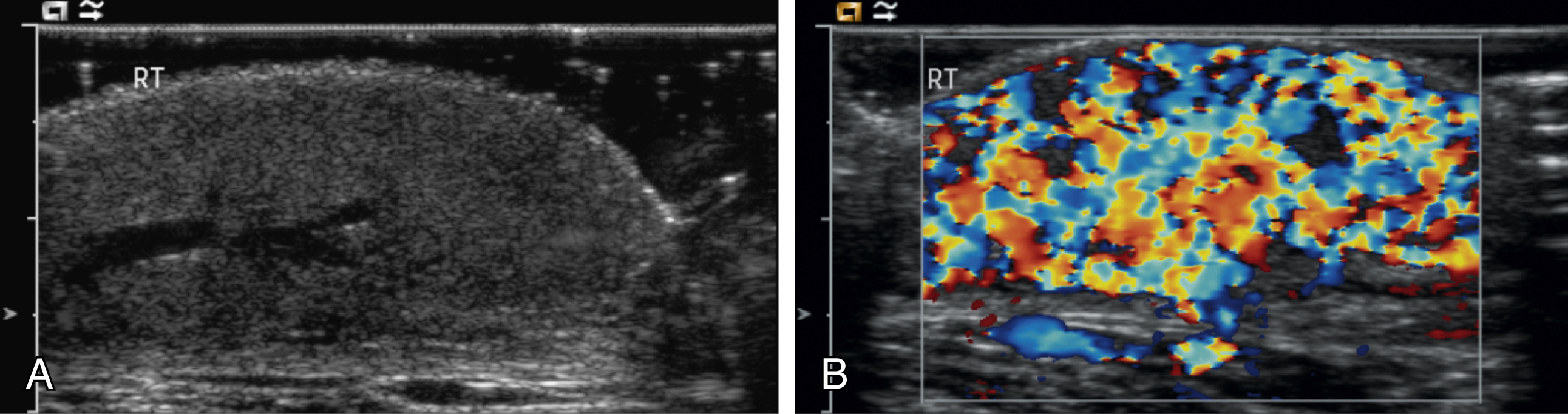
Infantile hemangiomas are by far the most common lesions in this subgroup. They are not present at birth, appearing at around 2 to 4 months of age. Typically they demonstrate a highly active period of growth and proliferation over several months and then slowly involute, disappearing during school age. It is this natural history that clearly separates them from vascular malformations that, in contrast, are present at birth and grow commensurately with the child. Infantile hemangiomas are usually superficial lesions with a characteristic bright red color and are easily diagnosed clinically, rarely troubling the radiologist. Deeper seated lesions will not exhibit skin staining. Such rapidly growing masses generate consternation and urgent referral. The diagnosis is simple because the imaging features are usually characteristic. Ultrasound demonstrates a well-defined echogenic lesion that is highly vascular with large central feeding arteries and draining veins ( Fig. 18.1 ). The highly arterialized nature of the lesion simply reflects its extremely active proliferation. Occasionally, biopsy may be required to allay concerns. Infantile hemangiomas express glucose transporter type 1 (GLUT1), a simple diagnostic marker. Core needle biopsy, when necessary to exclude more serious pathology, is usually straightforward under ultrasound guidance because lesions are typically superficial. A 16G coaxial technique is advocated in view of the highly vascular nature of these lesions, allowing a single pass through the tumor capsule and plugging of the biopsy track with Gelfoam pellets (Pfizer, New York, NY); complications, in the authors’ experience, are rare.
Perhaps surprisingly most of these highly vascular tumors do not cause vascular steal or cardiac compromise and can be managed conservatively. Intervention is indicated when lesions cause significant mass effect or disfigurement. Subglottic lesions and those that obstruct the visual axis are of particular concern. Pharmacologic management is now the mainstay of treatment in this group, with β-blockers the preferred first-line therapy. β-Blockers induce rapid shrinkage of infantile hemangiomas over a matter of weeks if administered in the proliferative phase. Although drug administration needs to be carefully managed, this provides a simple and noninvasive method of disease control and means that embolization is now almost never required for large, hypervascular lesions causing systemic effects.
This hemangioma subgroup merits brief mention because of significant differences in their natural history and prognosis when compared with infantile hemangiomas, which influences management decisions. Congenital hemangiomas are fully formed at birth and this feature alone distinguishes them from the infantile group. They are similar in appearance but have subtle differences in color and contour compared with the classic infantile lesions. Imaging features are not strikingly different from those of infantile hemangiomas, although the lesions are often more heterogeneous, and calcification can be seen.
Congenital hemangiomas form two distinct clinical subgroups defined by their natural history. Some involute very rapidly in the first few months of life and are termed rapidly involuting congenital hemangioma (RICH), and others never involute ( noninvoluting congenital hemangioma [NICH]). Both types are histologically and immunophenotypically distinct from infantile hemangiomas. Neither expresses GLUT1. Biopsy of such lesions is sometimes helpful to allow clinicians to predict outcome. NICHs are usually small and clinically inconsequential, RICHs can be extremely large and hypervascular at birth, causing cardiovascular instability and coagulopathy. Urgent embolization of very large congenital hemangiomas is often requested but should be avoided if possible, because these lesions will involute quickly without intervention.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here