Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Squamous cell carcinoma (SCC) accounts for 85% to 95% of malignant laryngeal tumors.
Tobacco and alcohol are the two most important risk factors for the development of laryngeal SCC.
In the United States, laryngeal SCC occurs in the glottis more frequently than in the supraglottis. Subglottic SCC is rare.
Laryngeal preservation may be achieved in properly selected cases by the use of conservation laryngeal surgery (partial laryngectomy), radiotherapy, or chemoradiotherapy.
Early (stage I and II) laryngeal SCC is generally treated with single-modality therapy, either surgery or radiotherapy.
Advanced (stage III and IV) laryngeal SCC is generally treated with combined-modality therapy.
Endoscopic partial laryngectomy (transoral laser microsurgery) has oncologic outcomes similar to open partial laryngectomy with less functional morbidity.
Total laryngectomy is the gold standard surgical procedure for the treatment of advanced laryngeal SCC.
Concurrent chemoradiotherapy in a properly executed organ-preservation protocol is the most effective nonsurgical treatment for appropriately selected advanced laryngeal SCC.
The stage of disease is the most important factor predictive of prognosis, with nodal stage more significant than tumor stage.
Cancer of the larynx is the second most common malignancy of the upper aerodigestive tract (UADT), and over 13,150 cases are reported annually in the United States alone. Although a large variety of malignancies may occur in the larynx, 85% to 95% of laryngeal malignancies are squamous cell carcinoma (SCC) that arises from the epithelial lining of the larynx. The successful management of laryngeal malignancy requires accurate diagnosis, staging, assessment of patient wishes, and selection of the most appropriate treatment for the individual patient with close posttreatment surveillance. Treatment options have expanded and become more complex as new surgical procedures have been developed, advanced radiation therapy (RT) modalities have evolved, and new chemotherapeutic drugs have become available. These treatments still have significant morbidity and pose risks of adverse impact on voice quality, airway integrity, and swallowing. In recent decades, major efforts have been made to develop therapeutic strategies to preserve the larynx anatomically and functionally using RT, conservation laryngeal surgery, and chemoradiotherapy (CRT). These techniques are now important tools in the armamentarium of the head and neck oncologist. This chapter focuses on the principles of the diagnosis, evaluation, and treatment of SCC of the larynx. Nonsquamous cell malignancies form a small but important subset of laryngeal malignancies and are also covered in detail. More specific details of surgical techniques are discussed in subsequent chapters.
A detailed knowledge of laryngeal embryology and anatomy is necessary to understand patterns of spread of laryngeal cancer and its clinical behavior. The pattern of spread of tumors within the larynx is guided by the ligaments, connective tissue membranes, and major cartilages of the larynx that contain the spread of tumors, as well as by the soft tissue spaces within the larynx that act as pathways for the spread of tumors both within and outside the larynx. The lymphatic drainage of the three regions of the larynx differs, and, therefore the risk of metastasis to regional lymph nodes, the likelihood for contralateral metastasis, and the first echelon nodes vary according to the site of the primary tumor. This characteristic of tumor behavior can be explained by the embryologic development of the larynx.
The embryologic development of the larynx influences the pattern of metastatic spread of laryngeal cancer. The supraglottic larynx is derived from the buccopharyngeal primordium, which develops from the third and fourth branchial arches. The glottis and subglottis are derived from the tracheobronchial primordium from the sixth branchial arch and are formed by the union of lateral furrows that develop on each side of the tracheobronchial primordium. Analogous to the embryology, the larynx has a dual blood supply and lymphatic drainage. The supraglottis is supplied by the superior laryngeal arteries from the superior thyroid artery, and its lymphatic drainage follows these vessels to the carotid sheath to drain into deep cervical chain nodes in Levels II and III. The glottis and subglottis are supplied by the inferior laryngeal arteries emanating from the inferior thyroid artery, and similarly, lymphatic drainage from these two regions follows these arteries to drain into prelaryngeal and pretracheal nodes (Level VI) before it reaches the deep cervical chain nodes in Level IV.
The glottis is formed by paired structures that fuse in the midline. The lymphatics drain unilaterally and the vocal folds have sparse lymphatics; therefore glottic cancers must invade deeply before they gain access to lymphatic channels. These factors explain the lower incidence of lymphatic metastasis in glottic SCC and the propensity for unilateral metastases. Because the supraglottis is formed without a midline union, its lymphatics drain bilaterally. The increased likelihood of bilateral lymphatic metastases from supraglottic carcinoma is ascribed to this embryologic factor. Pressman and colleagues noted that the inferior extent of supraglottic injection was the inferior false vocal cord; the ventricle defines an anatomic barrier that halts further inferior flow of the dye.
A complete description of the anatomy of the larynx is beyond the scope of this chapter, so the following discussion is limited to a description of the boundaries of the larynx, its compartments, and its lymphatic drainage. The laryngeal framework is formed by three unpaired cartilages—the epiglottis, thyroid, and cricoid—and the paired arytenoid cartilages. The superior boundary of the larynx consists of the tip and lateral margin of the epiglottis and the superior edge of the aryepiglottic folds. The anterosuperior limit is formed by the lingual surface of the suprahyoid epiglottis and the hyoepiglottic ligament, which forms the superior boundary of the preepiglottic space. The anterior boundary of the larynx is formed by the thyrohyoid membrane and thyroid cartilage in the supraglottis, thyroid cartilage in the glottis, and cricothyroid membrane and anterior arch of the cricoid cartilage in the subglottis. The inferior limit of the larynx is defined by the horizontal plane, which passes through the inferior edge of the cricoid cartilage. The posterior and lateral borders of the larynx are composed of the laryngeal surface of the aryepiglottic folds, arytenoid cartilages, interarytenoid space, and the posterior surface of the subglottic space, defined as the mucosa that covers the surface of the cricoid cartilage.
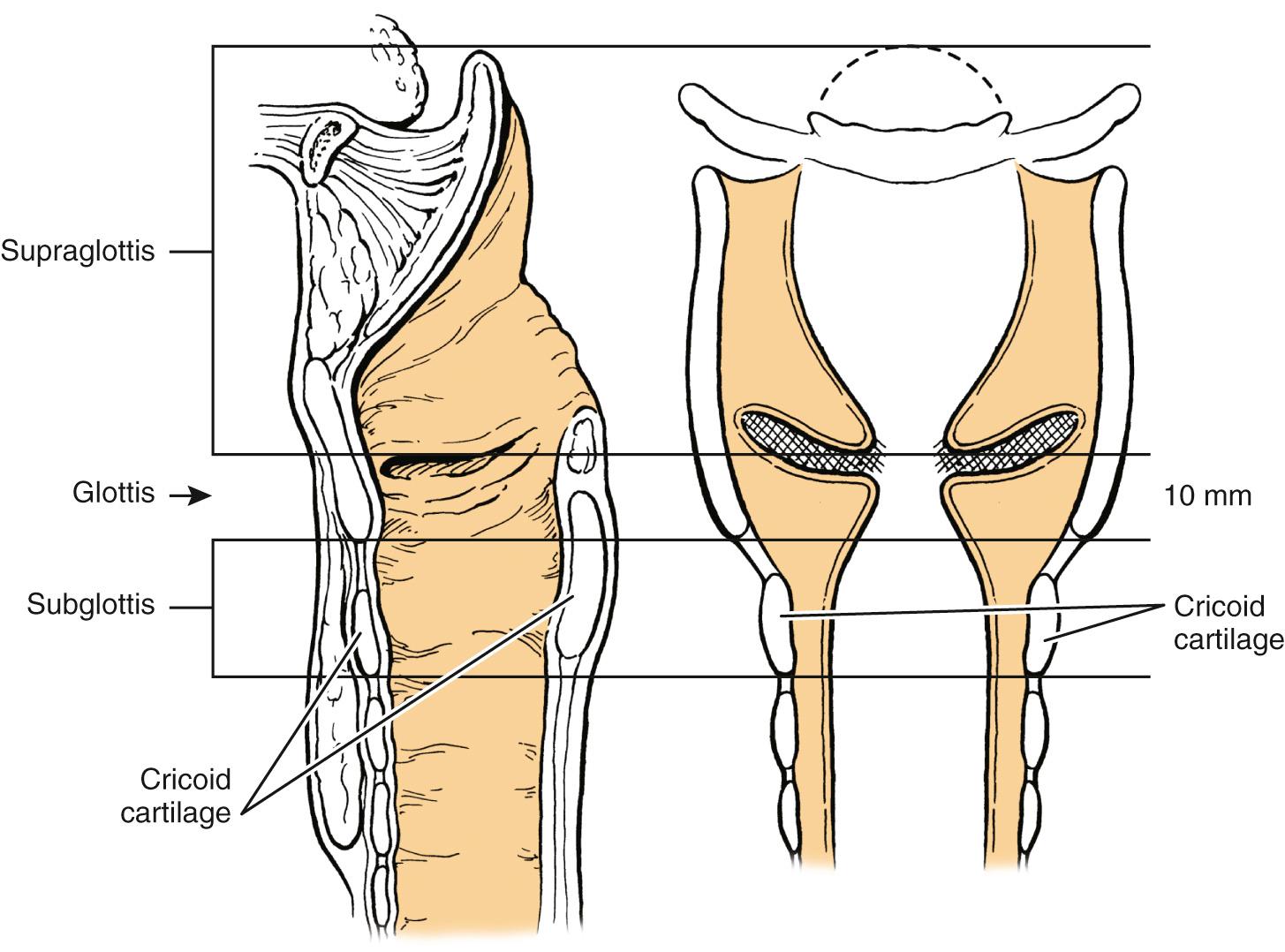
The larynx is divided into three regions: the supraglottis, the glottis, and the subglottis ( Fig. 105.1 ). This division reflects the embryologic structure of the larynx and the anatomic barriers to spread of laryngeal cancer outlined earlier. The tumor/node/metastasis (TNM) staging system further subdivides the supraglottis and glottis of the larynx into multiple subsites, which are used to define the T stage ( Box 105.1 ). The supraglottis is composed of the suprahyoid and infrahyoid epiglottis, both the lingual and the laryngeal surfaces; laryngeal surfaces of the aryepiglottic folds; the arytenoids; and the false vocal cords. The boundary between the suprahyoid and infrahyoid epiglottis is a horizontal plane that passes through the hyoid bone. This separation is important because the infrahyoid epiglottis communicates anteriorly with the preepiglottic space (PES), whereas the suprahyoid epiglottis does not. The inferior limit of the supraglottis is a horizontal plane through the lateral margin of the ventricle at its junction with the superior surface of the true vocal cord. The glottis is composed of the true vocal cords, both the superior and inferior surfaces, and includes the anterior and posterior commissures. The inferior boundary of the glottis is a horizontal plane 1 cm inferior to the inferior limit of the supraglottis, defined as the lateral margin of the ventricle at its junction with the superior surface of the vocal cord. The subglottis extends from the inferior limit of the glottis to the inferior edge of the cricoid cartilage; it is not divided further into any subsites.
| Primary Tumor (T) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| TIS | Carcinoma in situ |
| Supraglottis | |
| T1 | Tumor limited to one subsite of supraglottis with normal vocal cord mobility |
| T2 | Tumor invades mucosa of more than one adjacent subsite of supraglottis or glottis or region outside the supraglottis (e.g., mucosa of base of tongue, vallecula, and medial wall of piriform sinus) without fixation of the larynx |
| T3 | Tumor limited to larynx with vocal cord fixation and/or invades any of the following: postcricoid area, preepiglottic space, paraglottic space, and/or inner cortex of thyroid cartilage |
| T4a | Moderately advanced local disease |
| Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) | |
| T4b | Very advanced local disease |
| Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures | |
| Glottis | |
| T1 | Tumor limited to the vocal cord(s) with normal mobility; may involve anterior or posterior commissure |
| T1a | Tumor limited to one vocal cord |
| T1b | Tumor involves both vocal cords |
| T2 | Tumor extends to supraglottis and/or subglottis and/or with impaired vocal cord mobility |
| T3 | Tumor limited to the larynx with vocal cord fixation and/or invasion of paraglottic space and/or inner cortex of the thyroid cartilage |
| T4a | Moderately advanced local disease |
| Tumor invades through the outer cortex of the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, cricoid cartilage, soft tissues of neck including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) | |
| T4b | Very advanced local disease |
| Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures | |
| Subglottis | |
| T1 | Tumor limited to the subglottis |
| T2 | Tumor extends to vocal cord(s) with normal or impaired mobility |
| T3 | Tumor limited to larynx with vocal cord fixation and/or invasion of paraglottic space and/or inner cortex of the thyroid cartilage |
| T4a | Moderately advanced local disease |
| Tumor invades cricoid or thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck including deep extrinsic muscles of the tongue, strap muscles, thyroid, or esophagus) | |
| T4b | Very advanced local disease |
| Tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures | |
| Regional Lymph Nodes (N) | |
| cNX | Regional lymph nodes cannot be assessed |
| cN0 | No regional lymph node metastasis |
| cN1 | Metastasis in a single ipsilateral lymph node, ≤3 cm in greatest dimension |
| cN2 | Metastasis in a single ipsilateral lymph node, >3 cm but not >6 cm in greatest dimension, or in multiple ipsilateral lymph nodes, none >6 cm and ENE(−); or metastasis in multiple ipsilateral lymph nodes, none larger than 6 cm and ENE(−); or bilateral or contralateral lymph nodes, none >6 cm and ENE(−) |
| cN2a | Metastasis in a single ipsilateral lymph node, >3 cm but not >6 cm and ENE(−) |
| cN2b | Metastasis in multiple ipsilateral lymph nodes, none >6 cm and ENE(−) |
| cN2c | Metastasis in bilateral or contralateral lymph nodes, none >6 cm and ENE(−) |
| cN3 | Metastasis in a lymph node >6 cm and ENE(−); or metastasis in any lymph node(s) with clinically overt ENE(+) |
| cN3a | Metastasis in a lymph node, >6 cm and ENE(−) |
| cN3b | Metastasis in any lymph node(s) with clinically overt ENE(+) |
| pNX | Regional lymph nodes cannot be assessed |
| pN0 | No regional lymph node metastasis |
| pN1 | Metastasis in a single ipsilateral lymph node, ≤3 cm and ENE(−) |
| pN2 | Metastasis in a single ipsilateral lymph node, ≤3 cm and ENE(+); or >3 cm but not >6 cm and ENE(−); or multiple ipsilateral nodes, ≤6 cm and ENE(−); or bilateral or contralateral lymph node(s) ≤6 cm and ENE(−) |
| pN2a | Metastasis in a single ipsilateral lymph node, ≤3 cm and ENE(+) |
| pN2b | Metastasis in multiple ipsilateral lymph nodes, none >6 cm and ENE(−) |
| pN2c | Metastasis in bilateral or contralateral lymph nodes, none >6 cm in greatest dimension and ENE(−) |
| pN3 | Metastasis in a lymph node >6 cm in greatest dimension and ENE(−); or metastasis in a single ipsilateral node, >3 cm and ENE(+); or multiple ipsilateral, contralateral or bilateral lymph nodes any with ENE(+); or a single contralateral node of any size and ENE (+) |
| pN3a | Metastasis in a lymph node, >6 cm in greatest dimension and ENE(−) |
| pN3b | Metastasis in a single ipsilateral node >3 cm and ENE(+); or multiple ipsilateral, contralateral or bilateral lymph nodes any with ENE(+); or a single contralateral node of any size and ENE(+) |
Note: nodal sizes are all for the greatest dimension of the lymph node.
The mucosal lining of the larynx differs in the three regions. The epithelium of the supraglottis is predominantly of the pseudostratified columnar type, except at the edges of the aryepiglottic folds and the lateral borders of the epiglottis, which are stratified squamous epithelium. The supraglottic mucosa has an abundance of mucous glands and lymphatic vessels. The true vocal cords have a unique structure: stratified squamous epithelium covers a three-layered lamina propria composed of superficial, intermediate, and deep layers. The intermediate and deep layers of the lamina propria make up the vocal ligament, which forms the superior border of the conus elasticus and interdigitates with the vocalis muscle. The glottis has few lymphatic vessels. The subglottis is lined by pseudostratified columnar epithelium, which is in close approximation to the cricoid cartilage and cricothyroid membrane.
The laryngeal cartilages, hyoepiglottic ligament, thyrohyoid membrane, quadrangular membrane, conus elasticus, anterior commissure, and cricothyroid membrane form natural barriers to the spread of tumor. Within the larynx, the PES and the paraglottic space (PGS) provide pathways for spread of laryngeal tumors ( Fig. 105.2 ). The boundaries of the PES are anteriorly, the thyroid cartilage and thyrohyoid membrane; superiorly, the hyoid bone, hyoepiglottic ligament, and valleculae; and posteriorly, the anterior surface of the epiglottic cartilage and the thyroepiglottic ligament; laterally, the PES is open and continuous with each of the two paraglottic spaces. The PES contains fat and areolar tissue and is frequently invaded by tumors, because the cartilage of the epiglottis has multiple small fenestrations through which cancers that arise from the infrahyoid epiglottis may pass. Superiorly, the hyoepiglottic ligament provides a barrier to spread of tumor to the tongue base ( Fig. 105.3 ). The lymphatics of the PES drain through the thyrohyoid membrane and spread to lymph nodes on both sides of the neck, primarily in Levels II and III ( Fig. 105.4 ). Supraglottic tumors with PES involvement are staged as T3 lesions.
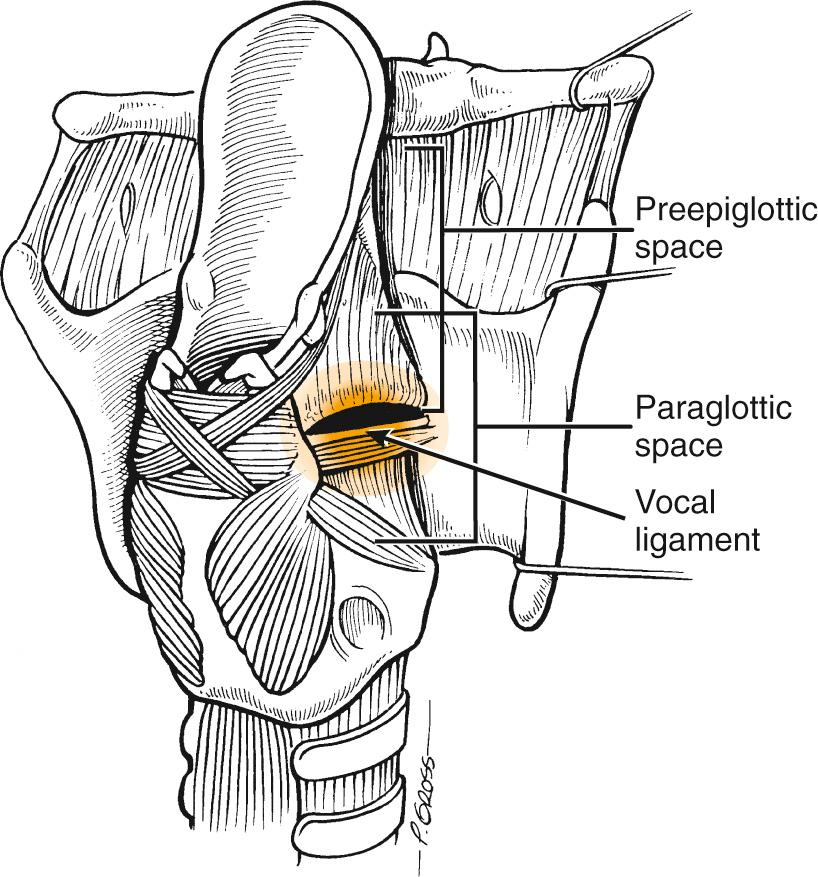
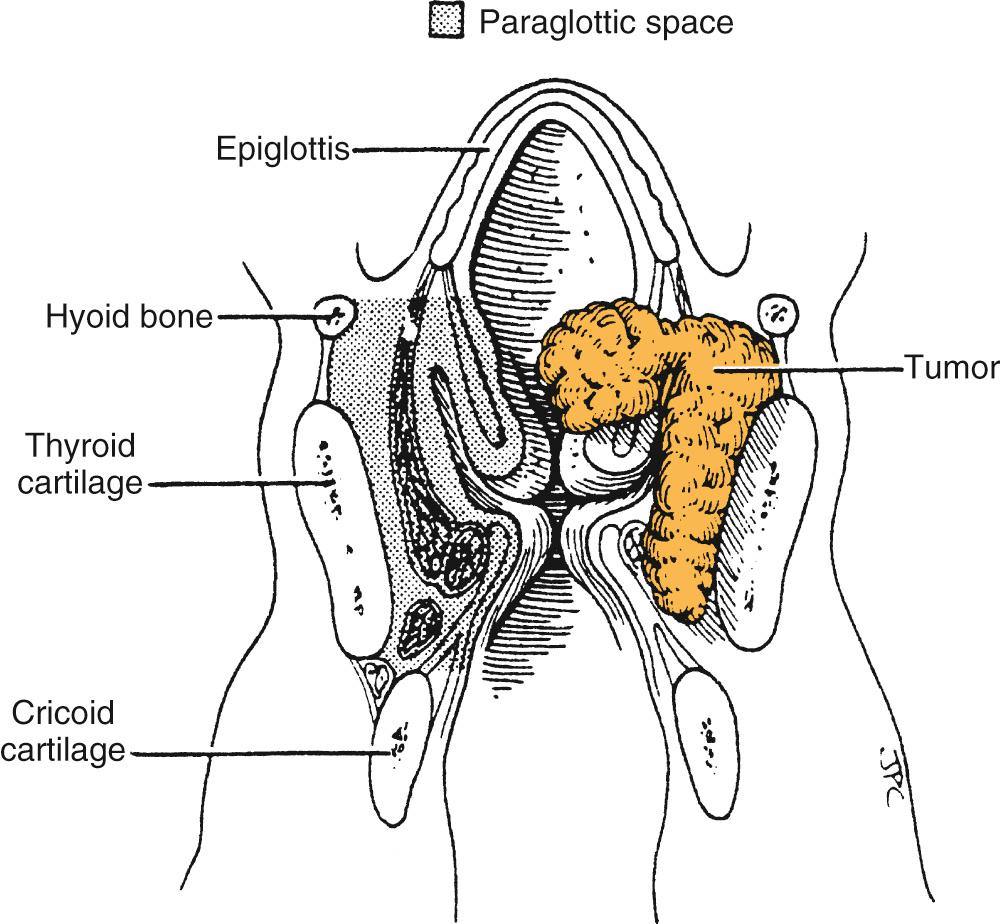
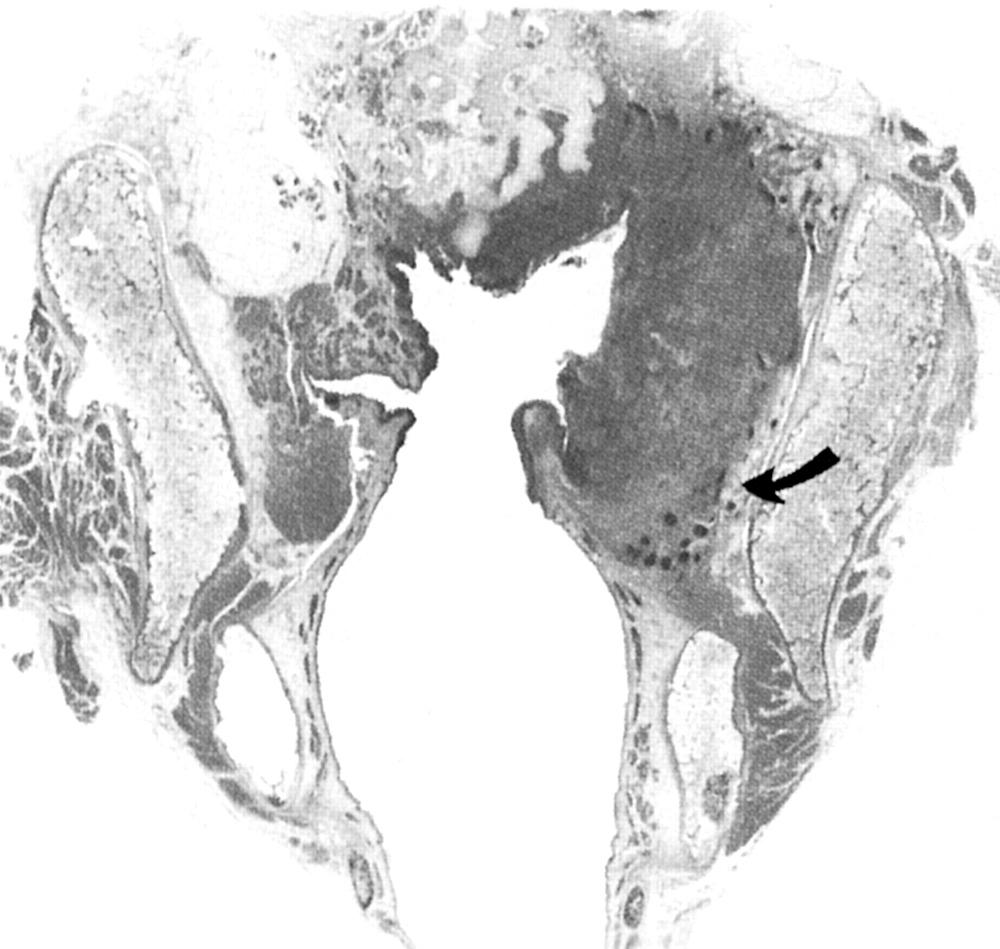
The PGS lies lateral to the true and false vocal folds and extends laterally to the thyroid cartilage ( Fig. 105.5 ). The boundaries of each PGS are medially (from superior to inferior), the quadrangular membrane, laryngeal ventricle, and conus elasticus; laterally, the thyroid cartilage anteriorly and the mucosa of the medial wall of the piriform sinus posteriorly; and inferolaterally, the cricothyroid membrane. Anteriorly, each PGS is continuous with the PES, and tumors may spread along this pathway (see Fig. 105.2 ). PGS involvement in either a glottic or supraglottic tumor is staged as T3 and is significant, because the extent of the PGS means that tumors in this space may spread to involve any or all of the three regions of the larynx ( Fig. 105.6 ).
Conservation laryngeal surgery is undertaken on the basis of the theory of compartmentalization of the larynx, which evolved from the work of Frazer, Pressman and colleagues, and Tucker and Smith. Pressman and colleagues found that this separate embryologic derivation explained why supraglottic tumors of substantial bulk do not spread across the laryngeal ventricle to the vocal cord. In experiments using submucosal vital dyes and radioisotopes, they also noted that the inferior extent of supraglottic injection was the inferior false vocal cord; the ventricle was an anatomic barrier to the inferior flow of the dye and thus was confirmed as a barrier to tumor spread. Using animals, cadavers, and whole-organ serial sections of human tumor specimens, Tucker and Smith confirmed that elastic tissue barriers within the larynx explain the findings of the dye studies. Although these studies confirm compartmentalization of the larynx, and clinically, supraglottic tumors are uncommonly observed to invade the glottis (and vice versa), no true anatomic barrier separates the supraglottis from the glottis.
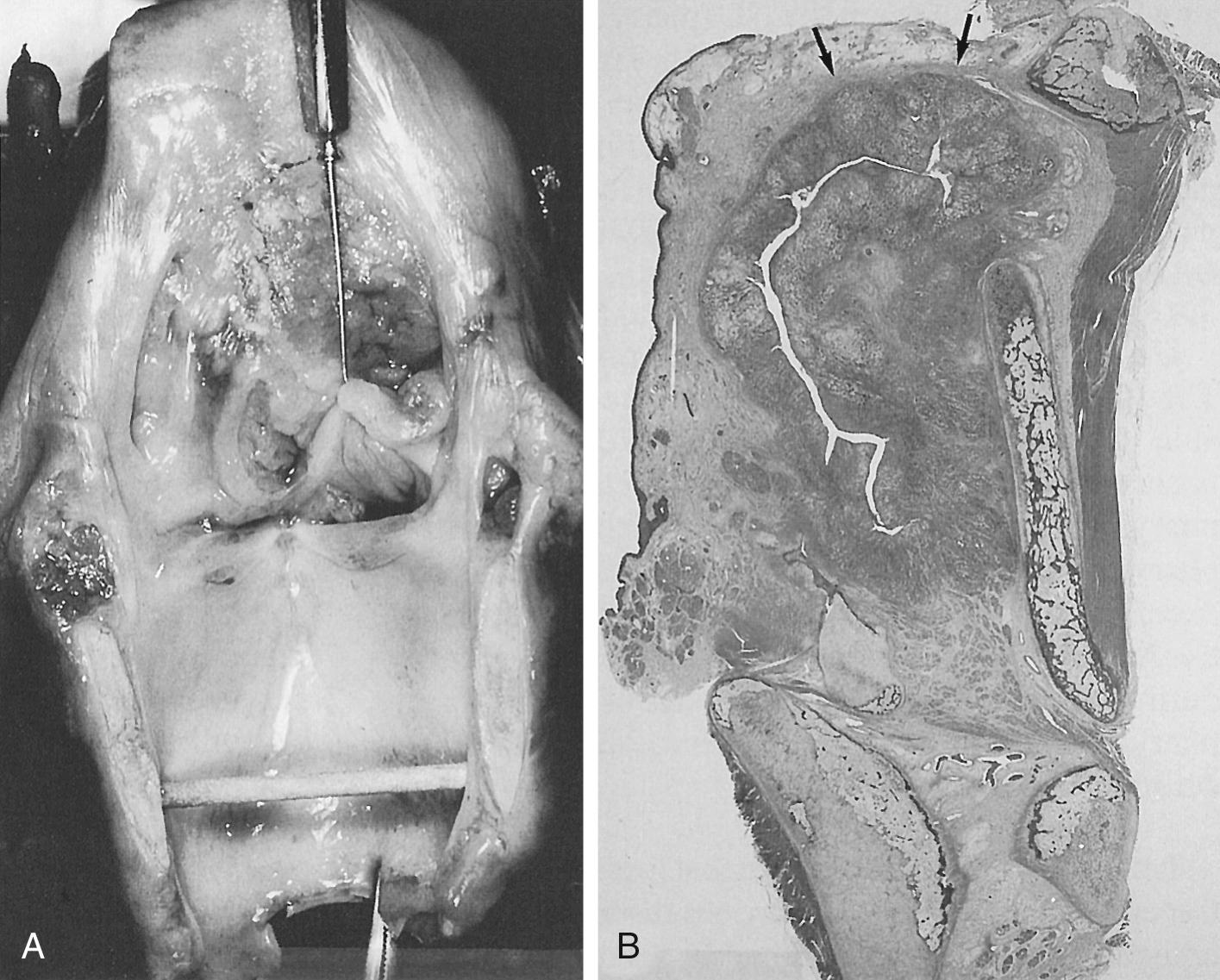
Transglottic tumors are an important subset of laryngeal tumors with aggressive behavior and high risk of lymphatic metastasis. The term transglottic was first used by McGavran and associates in 1961. It is not used in the American Joint Commission on Cancer (AJCC) staging system and is defined by Kirchner and colleagues as a tumor that crosses the ventricle in a vertical direction. LeRoux-Robert probably first described this type of cancer, proposing that the site of origin was the ventricle and that this was the only tumor that invaded supraglottic and subglottic areas. Kirchner and colleagues have shown that transglottic tumors do not necessarily arise from the ventricle. Tumors can become transglottic in four ways: (1) by crossing the ventricle directly, (2) by crossing at the anterior commissure, (3) by spreading through the paraglottic space, or (4) by spreading along the arytenoid cartilage posterior to the ventricle. The latter form of spread does not predict deep invasion; in Kirchner's series of 50 transglottic tumors studied in whole-organ preparations, none of the eight tumors with transglottic spread along the arytenoid demonstrated laryngeal cartilage invasion. In the same series, invasion of the laryngeal framework was seen in over half of transglottic tumors over 2 cm. Cervical metastases were seen in 30% of cases; and in primary tumors greater than 4 cm in diameter, 55% of tumors had nodal metastases.
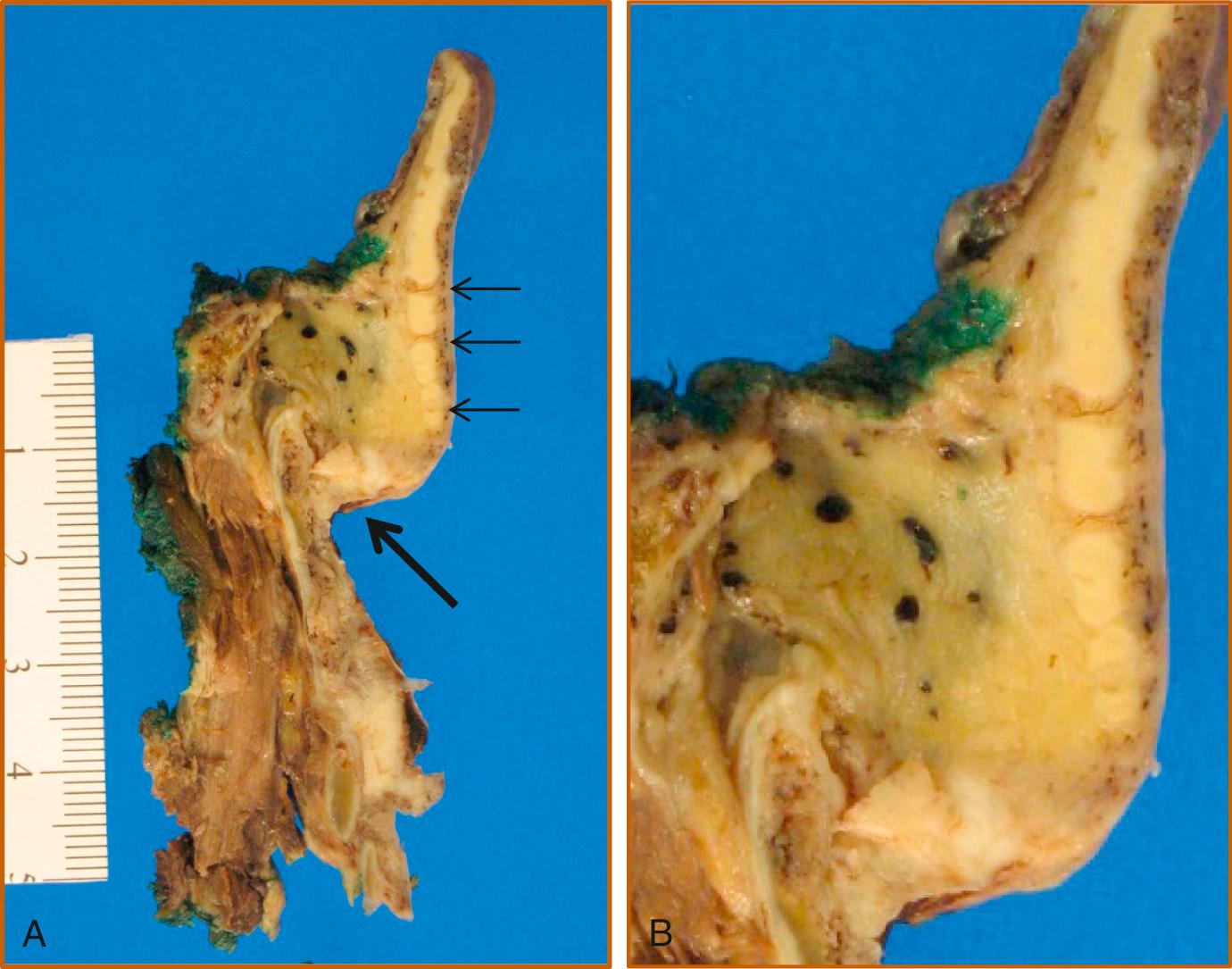
The anterior commissure is the part of the glottis where the true vocal cords meet anteriorly. The anterior commissure tendon is a 1-mm wide, 10-mm long band of fibrous tissue that extends from the vocal ligaments to the midline of the inner surface of the thyroid cartilage. At this insertion, the thyroid cartilage is devoid of perichondrium. Therefore in this area, the true vocal cords are in close approximation to the thyroid cartilage. Kirchner has studied factors associated with spread of tumors along the anterior commissure, and the anterior commissure tendon forms a strong barrier to spread of cancer. Tumors that cross from one true vocal cord to the opposite cord do not necessarily have deep invasion. Thyroid cartilage invasion or extralaryngeal spread of cancer at the anterior commissure requires significant supraglottic or infraglottic extension. Superiorly, tumors have access to the petiole of the epiglottis and preepiglottic space, whereas inferiorly, they have access to subglottic lymphatics, the thyroid cartilage, and the cricothyroid membrane. The thyroid cartilage is more likely to be ossified inferiorly, and ossified cartilage is not as strong a barrier to invasion as is cartilage.
Although the vast majority of malignant tumors of the larynx originate from squamous epithelium, a small number arise from other tissues within the larynx. Because of the differing clinical behavior of these tumors, an accurate histologic diagnosis is crucial. Recognizing the importance of this issue and the need for standardization in the histologic nomenclature of laryngeal tumors, the World Health Organization (WHO) has published a histologic classification of laryngeal tumors, the 4th edition of which was released in 2017. This classification system is outlined in Box 105.2 . Non–squamous cell laryngeal malignancies are described individually later in the chapter.
Mucous retention cyst
Laryngocele/saccular cyst
Heterotopic thyroid tissue
Vocal fold polyp
Vocal process granuloma
Infectious
Tuberculosis
Candidiasis
Histoplasmosis
Inflammatory
Wegener granulomatosis
Foreign body (e.g., Teflon) granuloma
Relapsing polychondritis
Pseudoepitheliomatous hyperplasia
Squamous cell hyperplasia
Keratosis
Necrotizing sialometaplasia
Chondrometaplasia
Amyloidosis
Langerhans cell histiocytosis
Rosai-Dorfman disease
Epithelial
Papilloma
Pleomorphic adenoma
Oncocytic papillary cystadenoma
Nonepithelial
Soft tissue
Lipoma
Schwannoma
Neurofibroma
Leiomyoma
Rhabdomyoma
Hemangioma
Lymphangioma
Granular cell tumor
Paraganglioma
Inflammatory myofibroblastic tumor
Bone and cartilage
Chondroma
Giant cell tumor
Low-grade dysplasia (low-grade SIL)
High-grade dysplasia (high-grade SIL)
Carcinoma in situ
Epithelial
Squamous cell carcinoma (SCC)
Conventional SCC
Verrucous SCC
Spindle cell carcinoma
Acantholytic (adenoid) SCC
Papillary SCC
Lymphoepithelial carcinoma
Clear cell carcinoma
Malignant salivary gland tumors
Adenocarcinoma
Acinic cell carcinoma
Mucoepidermoid carcinoma
Adenoid cystic carcinoma
Carcinoma ex pleomorphic adenoma
Epithelial-myoepithelial cell carcinoma
Salivary duct carcinoma
Neuroendocrine carcinoma
Well-differentiated NEC (carcinoid tumor)
Moderately differentiated NEC (atypical carcinoid tumor)
Poorly differentiated NEC
Small-cell NEC
Large-cell NEC
Malignant soft tissue tumors
Malignant paraganglioma
Fibrosarcoma
Malignant fibrous histiocytoma
Liposarcoma
Leiomyosarcoma
Rhabdomyosarcoma
Angiosarcoma
Kaposi sarcoma
Malignant hemangiopericytoma
Malignant nerve sheath tumor
Alveolar soft part sarcoma
Synovial sarcoma
Ewing sarcoma
Malignant tumors of bone and cartilage
Chondrosarcoma
Osteosarcoma
Hematolymphoid tumors
Lymphoma
Extramedullary plasmacytoma
Contiguous primary site
Hypopharynx
Oropharynx
Thyroid
Distant primary site
Kidney
Skin (melanoma)
Breast
Lung
Prostate
Gastrointestinal tract
For the staging of malignant tumors, the AJCC and the Union for International Cancer Control (UICC) use the TNM classification system, developed in 1943 by Pierre Denoix. The TNM system takes into account the extent of the primary tumor (T), the absence or presence and extent of regional lymph node metastasis (N), and the absence or presence of distant metastases (M). The 2017 AJCC/UICC TNM definitions for epithelial laryngeal malignancies are given in Box 105.1 .
Using this system, tumors with varying combinations of T, N, and M are grouped into stages; these are described in Table 105.1 . A tumor may be classified clinically, designated cTNM, or pathologically, designated pTNM. The clinical classification is based on the evaluation of the patient before treatment commences and includes information obtained from physical examination, which includes laryngoscopy, radiologic imaging, endoscopy, and biopsy.
| Stage | T | N | M |
|---|---|---|---|
| 0 | TIS | N0 | M0 |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III | T3 | N0 | M0 |
| T1 | N1 | M0 | |
| T2 | N1 | M0 | |
| T3 | N1 | M0 | |
| IVA | T4a | N0 | M0 |
| T4a | N1 | M0 | |
| T1 | N2 | M0 | |
| T2 | N2 | M0 | |
| T3 | N2 | M0 | |
| T4a | N2 | M0 | |
| IVB | T4b | Any N | M0 |
| Any T | N3 | M0 | |
| IVC | Any T | Any N | M1 |
The TNM classification system for the larynx is used for epithelial malignancies of the larynx only—nonepithelial tumors such as those of lymphoid tissue, soft tissue, cartilage, or bone are not included, although such lesions may be staged according to the system relevant to their histopathology (e.g., lymphomas of the larynx are staged according to the TNM system for lymphoid neoplasms).
An additional comment regarding the T staging of glottic tumors should be made. The T2 classification for glottic tumors encompasses a wide variety of lesions, including those with normal and impaired vocal cord mobility. Because the local control rate of RT for T2 glottic tumors with impaired vocal cord mobility has been observed to be lower than that of T2 tumors with normal vocal cord mobility, many authors distinguish between these two subsets of the T2 group by using T2a to denote those tumors with normal vocal cord mobility and T2b for those with impaired mobility. This division of the T2 stage has not been incorporated into the AJCC/UICC TNM system.
In 2017, the WHO reclassified lesions that were previously termed “premalignant”, carcinoma in situ (CIS) and varying degrees of dysplasia to a new category of precursor lesions. Precursor lesions were categorized into a two-tier system, including low-grade dysplasia and high-grade dysplasia. This was based on the amended Ljubljana classification. Clinically dysplastic lesions are noted on the vocal folds as leukoplakia (white patches), erythroplakias (red patches), or erythroleukoplakias (red and white patches). Low-grade dysplasia has a relatively low malignant potential, while high-grade dysplasia is considered a high-risk premalignant lesion. Morphologic criteria of low-grade dysplasia versus high-grade dysplasia is listed in Table 105.2 . A three-tier system can be used for treatment purposes in which the high-grade category can be further separated into high-grade dysplasia and carcinoma in situ. CIS should be reserved for “rare” cases with pronounced architectural disorder, severe atypia and increased mitosis. Previous classification systems were plagued with problems of widespread variability found in pathologic interpretation and diagnosis, which was noted to be inherently subjective.
| Low-grade dysplasia Low malignant potential with changes ranging from squamous hyperplasia to an augmentation of basal and parabasal cells occupying up to the lower half of the epithelium, with normal upper half epithelial maturation. |
|
| Architectural criteria |
|
| Cytologic criteria |
|
| High-grade dysplasia Premalignant lesion with immature epithelial cells occupying the lower half to full epithelial thickness. |
|
| Architectural criteria a |
|
| Cytologic criteria a |
|
a Complete loss of stratification and polarity and/or severe cytologic atypia and atypical mitoses qualify as carcinoma in situ if a three-tiered system is used.
The primary clinical concern is the likelihood of a precursor lesion progressing to malignancy. Malignant transformation rates progressively increase as lesions become more dysplastic. A recent review noted that 30% of patients with dysplastic lesions that progressed to invasive cancer eventually underwent total laryngectomy. Because some lesions that show mild dysplasia, and even those without dysplasia, may progress to invasive cancer, long-term follow-up of all premalignant laryngeal lesions is warranted. A comprehensive review of laryngeal leukoplakia by Isenberg and colleagues estimated malignant transformation rates of lesions without dysplasia, with mild to moderate dysplasia, and severe dysplasia/CIS of 3.8%, 10.1%, and 18.1%, respectively. A meta-analysis of laryngeal dysplasia demonstrated an overall malignant transformation rate of 14%, with a mean time of malignant transformation being 5.8 years. Blackwell and colleagues observed a 3.9-year interval between initial biopsy and progression to invasive cancer. In a large series of over 1000 keratotic laryngeal lesions, the mean interval to malignant transformation was 3.1 years. The latency was longer for earlier lesions, and 7% of lesions transformed to invasive carcinoma more than 10 years after the initial biopsy.
The visual appearance of a precursor laryngeal lesion does not predict its histologic nature, nor does laryngeal videostroboscopy reliably differentiate precursor lesions. Biopsy is the gold standard for diagnosis, and adequate sampling is important because an insufficient biopsy will result in sampling error.
The treatment of a precursor lesion should aim to eradicate the lesion while preserving voice quality and laryngeal function. Accurate diagnosis is critical for proper decision making, and a number of factors related to the characteristics of the lesion, as well as patient factors, affect the treatment decision-making process ( Table 105.3 ).
| Patient Factors | Tumor Factors |
|---|---|
| General health/comorbidities | Extent of lesion |
| Unilateral vs. bilateral | |
| Anterior commissure involvement | |
| Extension beyond the glottis | |
| Focal vs. diffuse lesion | |
| Vocal demands (e.g., professional singer) | Previous treatment |
| Prior surgical excision | |
| Prior radiation therapy | |
| Compliance with tobacco cessation, alcohol cessation, reflux treatment | |
| Patient choice |
Patients with concerning vocal fold lesions should undergo microdirect laryngoscopy with directed biopsies. Critical to this is the use of high-power magnification, fine microsurgical instruments, and meticulous surgical techniques to remove the entire lesion and preserve the underlying lamina propria. Treatment options include microflap and full-thickness excision, ablation with carbon dioxide laser and excision with photoangiolytic lasers such as the 585-nm pulsed dye laser (PDL) and the 532 nm pulsed potassium-titanyl-phosphate (KTP) laser. Historically, vocal fold stripping was performed, in which the mucosa and underlying lamina propria were removed. This, however, causes vocal fold scarring and poor voice outcomes; hence this technique is no longer advocated and has been abandoned. After treatment, patients should be followed closely in the office to monitor for recurrence. Lesions that recur should be treated again, with the understanding that some patients may have lesions that recur more than once.
Lesions that are high-grade dysplasia and CIS have an increased risk of progressing to malignancy. Close follow-up is required because of the risk of recurrence of the lesion and possible malignant transformation. CIS may be treated with surgery or by RT. The recurrence rate for CIS treated with surgery is greater than that for neoplasms treated with RT and is reported to be approximately 20% after initial excision. With repeated surgical excision, the ultimate local control rate is excellent and is at least equivalent to that of RT. Surgical treatment is preferred for focal lesions in patients who are reliable and will attend routine follow-up.
RT is also an effective treatment for CIS; a recent review of 16 studies of CIS treated with RT determined that the local control rate was 93.5%. RT is particularly useful for multiple recurrences following surgical excision; for diffuse lesions that extend beyond the vocal cords that cannot be excised without inducing significant morbidity; for patients who are unlikely or unable to attend follow-up; and for medically infirm patients unfit for general anesthesia. Voice quality is well preserved following RT. The primary disadvantage of RT is that it cannot be repeated if there is a recurrence or second tumor in the irradiated field. Long-term side effects of RT should be considered as well. Successful management of premalignant laryngeal lesions also requires the implementation of tobacco and alcohol cessation strategies and treatment of laryngopharyngeal reflux when present.
Over the past two decades, in-office management of precursor lesions has become more common. Initially this was performed with the 585-nm PDL, but more recently, the 532-nm pulsed KTP laser has been used more commonly. In a pilot study, Franco and colleagues used PDL for the treatment of dysplasia in the operating room under general anesthesia. In most cases, the treated lesions were then excised and sent for histologic examination. This treatment was effective: 81% of patients had greater than 70% regression of their lesions. The authors also noted that regression occurred in treated lesions that were not excised. A subsequent report from the same group demonstrated the efficacy of PDL delivered via a flexible endoscope in the office for the treatment of dysplasia. Koufman and colleagues found that 64% (16/25) of their patients with dysplasia required no further treatment during the follow-up period of their study. Franco has also described favorable experience with the use of PDL for dysplasia. Zeitels and colleagues subsequently adopted the pulsed KTP laser for in-office use, citing smaller fiber diameter, greater reliability, improved intralesional energy absorption, and improved hemostasis as advantages of the pulsed KTP system over PDL.
The energy from these lasers is preferentially absorbed by oxyhemoglobin; the absorption of energy from the pulsed KTP is superior to that of PDL and causes photoangiolysis of the sublesional blood vessels. Preferential destruction of intraepithelial desmosome junctions and separation of the treated epithelial cells from the basement membrane have also been observed microscopically. Apart from the obvious advantages of in-office procedures—avoidance of general anesthesia, lower cost, improved efficiency, and patient preference—these lasers have minimal effect on the surrounding tissue, and scarring is uncommon. The bilateral simultaneous treatment of lesions in and around the anterior commissure is possible, with minimal risk of web formation.
While performing in-office biopsy at the time of laser surgery is possible, specimens are often small and difficult to analyze and, as such, biopsy is rarely performed. This being the case, a concern of office-based surgery is that no specimen is obtained for pathologic examination, and therefore a definitive assessment of the tumor extent and margin status is not possible. In the reports published to date, a biopsy was obtained in all patients before the commencement of treatment. It bears repeating that all patients should first be taken to the operating room for microdirect laryngoscopy, and subsequent recurrences can be treated in the office if desired. Potential limitations of in-office treatment include poor exposure of the lesion, difficulty treating medial edge of infraglottic lesions, and decreased freedom in fiber positioning compared to suspension laryngoscopy. Serial, outpatient office-based laser treatment has been shown to be effective in management of these lesions in study with long follow-up. Treatment in the operating room should always be reserved for patients with concern of progression of disease.
SCC is the most common malignant tumor of the larynx and is responsible for between 85% and 95% of all laryngeal malignancies. This tumor arises from stratified squamous epithelium or from respiratory epithelium that has undergone squamous metaplasia. The incidence of SCC in each of the three regions of the larynx—the supraglottis, glottis, and subglottis—varies according to the patient population. In the United States, Canada, England, and Sweden, glottic SCC is more common than supraglottic SCC, whereas the reverse is true in France, Italy, Spain, Finland, and the Netherlands. In Japan, glottic and supraglottic SCC have similar incidence rates, and primary subglottic SCC is rare in all populations. In a large review of nearly 160,000 cases of laryngeal SCC in the United States, the site of origin was the glottis in 51%, the supraglottis in 33%, and the subglottis in 2%; lesions could not be categorized accurately in 14%.
In the United States, approximately 13,150 cases of laryngeal cancer were diagnosed in 2018, resulting in approximately 3710 deaths. The male-to-female incidence ratio is 3.9:1 for laryngeal cancer. While no racial predilection is apparent, race has been shown to be an independent prognostic factor, with African American patients presenting at a younger age and lower overall survival compared with Caucasians, Hispanics, and Asian patients. The epidemiology and risk factors largely parallel those for head and neck cancer overall; over 90% of cancers occur in people over 40 years of age, and 85% to 95% of these cancers are SCC. Worldwide, the overall burden of laryngeal cancer has decreased between 1990 and 2015, due largely to the significant reduction in smoking behavior in developed countries. A 7:1 male-to-female ratio exists, representing the highest gender disparity among all head and neck cancers. The higher incidence in males is due to an increased exposure to risk factors, rather than to an inherent gender predilection.
Tobacco and alcohol use are the two primary risk factors for cancer of the larynx. The International Agency for Research on Cancer has concluded that evidence is sufficient to state that there is a causal link between tobacco and alcohol use with development of head and neck cancer. The risk is proportional to the intensity and duration of tobacco or alcohol consumption, and the risk decreases slowly after cessation but does not return to the baseline rate for at least 15 years. There are variations in risk with the type of tobacco exposure (e.g., cigar vs. cigarette, filtered vs. nonfiltered cigarettes), but the most important factors are the amount of tobacco consumed and the duration of exposure. While alcohol independently increases the risk of head and neck cancer, with a twofold increase in odds of cancer in nonsmokers who drink, tobacco and alcohol act synergistically to increase the risk of cancer. The relative contribution of alcohol and tobacco varies by site. Alcohol consumption is a more important risk factor for supraglottic carcinoma, whereas tobacco use is strongly associated with glottic carcinoma.
Chronic irritation of the larynx has been proposed as a risk factor for laryngeal cancer and may be a contributing factor for those who do not smoke or drink. Gastroesophageal reflux disease affects between 20% and 40% of the US population, and up to 70% of these patients also have laryngopharyngeal reflux (LPR). While concern that LPR could cause cancer was raised in the 1980s, it has been difficult to determine whether the relationship is causal or merely an association. A large case-control study of U.S. veterans concluded that the risk is moderately increased for laryngeal or pharyngeal cancer associated with LPR independent of tobacco and alcohol use, though a more recent study within the same population revealed no relationship between reflux and laryngeal cancer. Alkaline bile reflux may also be a causative factor. One study identified a significantly higher incidence of laryngeal carcinoma in patients who underwent gastrectomy compared with controls. However, there is currently a lack of definitive evidence for a causal relationship of reflux with cancer.
Occupational exposure to toxins is another risk factor for laryngeal cancer. The incidence of laryngeal cancer is higher in unskilled manual workers who have both a high alcohol and tobacco intake and are exposed to disproportionate levels of potential toxins. Numerous agents have been implicated as risk factors for laryngeal cancer; these include diesel exhaust, asbestos, organic solvents, sulfuric acid, mustard gas, certain mineral oils, metal dust, asphalt, wood dust, stone dust, mineral wool, and cement dust. Establishing a link between any one toxin and larynx cancer has been difficult, because the studies have been underpowered and plagued with confounding variables. The significance of asbestos exposure is controversial. A meta-analysis published in 1999 concluded that a weak association exists between asbestos exposure and laryngeal cancer, though a recent systematic review that included 162 studies did not find evidence to support a correlation between asbestos exposure and laryngeal cancer.
Human papillomavirus (HPV) has long been recognized as a causative factor for cervical cancer in women and is now known to be causative in oropharyngeal SCC. The association of HPV and other subtypes of head and neck SCC, including the larynx, is not as well established. A recent meta-analysis identified 54 publications in which laryngeal SCC was examined for the presence of HPV DNA and found the prevalence of HPV DNA in 2739 cases of laryngeal SCC to be 22.1%, about half that of cancers of the oropharynx. However, the mere presence of HPV DNA in cancer specimens is not sufficient to prove viral causation. Using more accurate biomarkers of the viral oncogenic activity such as E6/E7 mRNA (markers of HPV oncogene transcriptional activity), the attributable fraction of laryngeal SCC to the HPV virus was found to be 8.6%. In a separate large case series, including 1042 cases of laryngeal SCC, the rate of HPV-attributable laryngeal SCCs was found to be 3.5%. Additionally, while HPV has been found to be a strong independent prognostic factor for survival among oropharyngeal cancer patients (Ang 2010), no such association between HPV status and patient outcomes in laryngeal SCC has been identified. Because of both the lack of definitive causal association between HPV and laryngeal SCC and the lack of prognostic significance of p16 positivity, routine testing of HPV in laryngeal cancer specimens is not currently recommended.
Mounting evidence supports the idea of a genetic susceptibility to laryngeal SCC. While most smokers die prematurely as a result of tobacco use, only a minority will develop cancer. Additionally, a historical cohort study showed a relative risk of 3.79 for SCC of the head and neck in association with a family history of squamous cell carcinoma of the head and neck. Moreover, second primary tumors are a common feature of head and neck SCC, affecting 10% to 30% of patients, and representing the leading long-term cause of mortality in these patients. Genetic polymorphism variants in tobacco carcinogen and alcohol metabolism genes may increase SCCHN risk. Polymorphisms of Phase I and Phase II detoxifying enzymes, as well as polymorphisms of DNA repair enzymes, are also associated with risk of developing head and neck cancer. Particular gene mutations and chromosomal alterations may be associated with malignancy as well, with mutations in p53 being found in 56.7% of laryngeal carcinomas. Epidemiologic studies can stratify risk for developing head and neck cancer and other cancers, and biomarkers are under development to identify molecular changes associated with cancer development. These assays provide markers for genetic susceptibility to cancer (e.g., mutagen sensitivity) and have the potential to provide prognostic information about response to treatment. These studies are useful for understanding the pathogenesis of cancer but currently do not provide assistance to guide the clinician managing individual patients.
The discovery of familial cancer syndromes drew attention to the role of genetic susceptibility to developing cancer. Only a small proportion of head and neck cancers arise from familial syndromes (e.g., xeroderma pigmentosum); however, studies of head and neck cancer demonstrate an elevated risk in family members. Copper and colleagues found a relative risk of 14.6 for respiratory tract cancers in the siblings of cancer patients and an overall relative risk of 3.5 for first-degree relatives. The host ability to tolerate exposure to carcinogens is highly variable and is related to the ability to prevent activation of procarcinogens, inactivate active carcinogens, repair DNA damage, and maintain immune surveillance. These factors are highly variable among individuals and are still poorly understood.
Evidence links dietary factors to the risk of head and neck cancer. An increased intake of fruits and vegetables and a decreased intake of meat and fat have a protective effect and are associated with a reduced incidence of head and neck cancer, colon cancer, and cardiovascular disease. However, these benefits may take 20 years or longer to accrue, and at present, these epidemiologic observations have not led to the successful development of a cancer reduction program.
The single greatest risk factor for head and neck SCC is prior head and neck SCC. The annual risk of a second primary tumor (SPT) following an index head and neck SCC is 1% to 7%, and this risk persists for at least 10 years. The cumulative risk of developing an SPT is at least 20% and is greater for those who continue to use tobacco and alcohol. An individual with stage I or II head and neck SCC is more likely to die of an SPT than from the index tumor. The majority of SPTs develop in the head and neck, but a significant proportion occur in the esophagus or lung. Second primary tumors may be synchronous, identified within 6 months of the index tumor, or metachronous, diagnosed more than 6 months after the index tumor. In a study of 875 patients with SCC of the head and neck, SPTs had developed in 207 patients within 5 years of the index tumor. Of these patients, 31% developed a third primary malignancy, and 10% had a fourth primary malignancy. For laryngeal cancer, the lung is a significant site for synchronous and metachronous SPTs. An isolated lung malignancy in a patient with larynx cancer is more likely to be an SPT than a metastasis from the laryngeal cancer; therefore an isolated pulmonary nodule should be considered an SPT until proven otherwise. Prior RT is associated with SPTs in a small number of cases. Slaughter and associates examined clinically normal tissue adjacent to head and neck cancers and identified many histologic changes seen in the malignant cells in the adjacent normal-appearing tissue, which led to the proposal of the concept of “field cancerization.” Improved understanding of head and neck carcinogenesis has provided a molecular explanation for these observations. Bedi and colleagues examined X-chromosome inactivation and performed microsatellite analysis to evaluate allelic loss at chromosomes 3p and 9p in females with multiple primary head and neck cancers. Both the original cancer and the second malignancy arose from a single clone. Califano and coworkers similarly observed that tissues adjacent to malignant and premalignant lesions shared common genetic changes. Multiple tumors generally do not arise from multiple transforming events; rather, a single transforming event produces a cell with a growth advantage that spreads throughout the mucosal surface. The tumor may accumulate further genetic damage and ultimately result in additional malignancies that are geographically distinct but genetically related to the original cancer.
The molecular biology of laryngeal SCC is similar to that of SCC in other sites of the head and neck. Carcinogenesis is a long process that occurs over many years preceding the development of cancer. Disruption of multiple genes is required to induce malignant transformation, with 6 to 12 distinct mutations generally necessary to produce malignancy. Understanding the molecular biology of head and neck cancer is useful to predict who will likely develop cancer, measure response to preventive agents, identify novel targets for treatment, and predict a patient's response to RT or chemotherapy. The molecular biology of head and neck cancer is discussed in Chapter 72 .
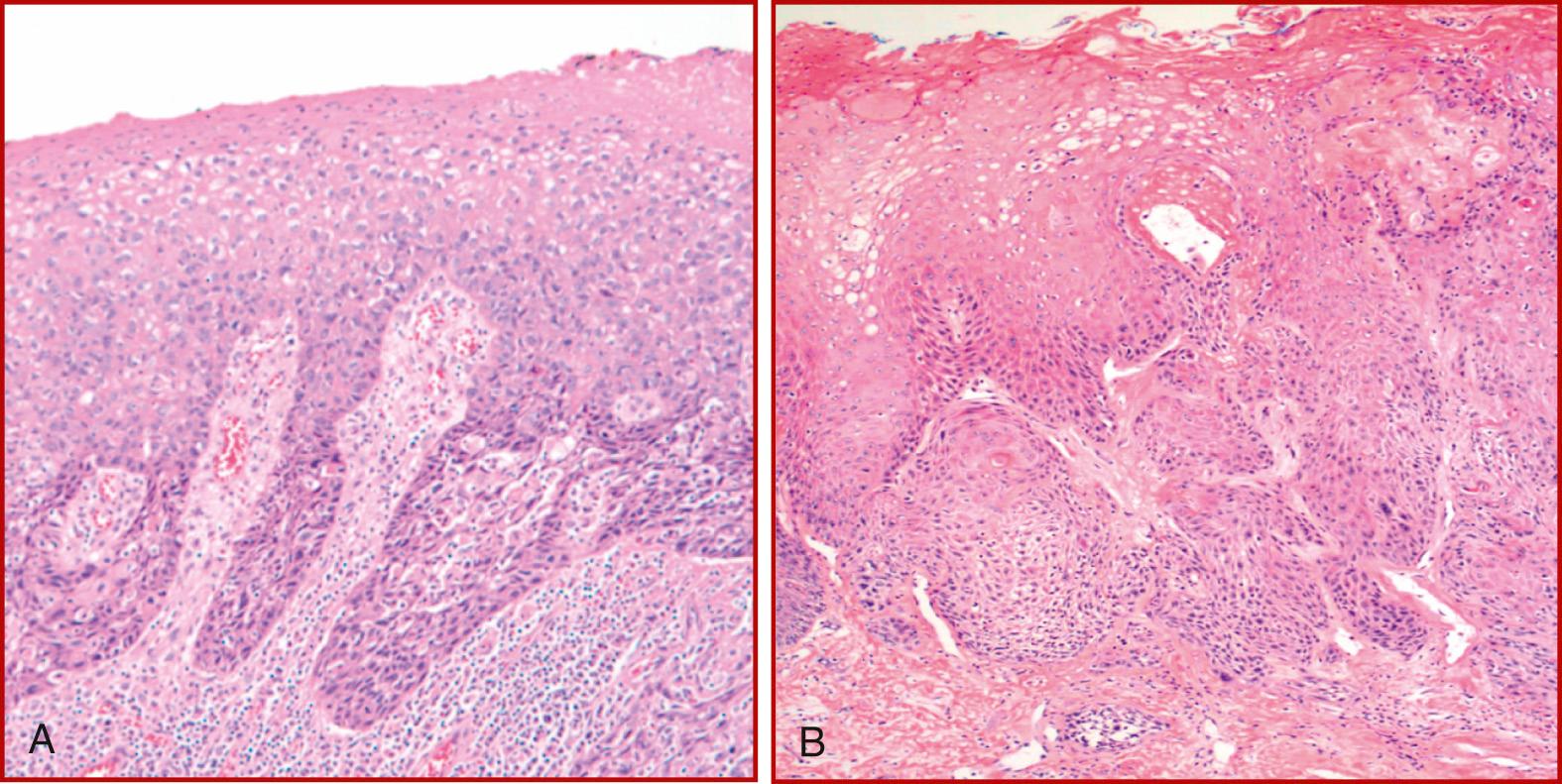
Squamous differentiation is the hallmark of SCC, which is characterized by the formation of keratin and/or the presence of intercellular bridges. SCC is graded by its histologic appearance and can be divided into three categories. Well-differentiated SCC resembles normal squamous epithelium and contains basal-type cells and squamous cells with keratinization and intercellular bridges; the nuclei are hyperchromatic and irregular in size and shape (pleomorphic); the nuclear/cytoplasmic ratio is reduced, and atypical mitoses are rare. Moderately differentiated SCC has less keratinization, more atypical mitoses, and more nuclear pleomorphism; intercellular bridges are also present. Poorly differentiated SCC has minimal, if any, keratinization, minimal intercellular bridges, and numerous atypical mitoses. The histologic grade has been reported as having prognostic value; however, grading is subjective, and sampling error may influence the grade assigned.
SCC breaches the basement membrane of the epithelium to invade the underlying tissue ( Fig. 105.7 ). The interface between the tumor and the adjacent normal tissue varies according to the pattern of invasion, which may be expansive, characterized by well-defined pushing margins, or infiltrative, characterized by poorly defined margins with occasional cells or “tongues” of tumor found in the tissue adjacent to the tumor. The latter pattern of invasion is associated with a worse prognosis. A lesion in which the entire thickness of the epithelium shows the cellular features of carcinoma without invasion of the underlying stroma is termed SCC in situ, and the term microinvasive SCC refers to SCC in which limited tumor invasion is confined to the area just deep to the basement membrane.
SCC expresses epithelial markers such as cytokeratin and epithelial membrane antigen. These markers are detected by immunohistochemistry (IHC), which is used to differentiate between SCC and malignant tumors of similar histologic appearance.
The pathologic diagnosis of SCC is usually straightforward; however, two entities in particular can be difficult to distinguish from SCC. The first, pseudoepitheliomatous hyperplasia (PEH), is characterized by an overgrowth of squamous epithelium that histologically mimics carcinoma. It can be a primary process or a secondary histologic finding associated with chronic irritation, trauma, infection, or giant cell tumor (GCT). The epithelium does not demonstrate cytologic evidence of malignancy; however, elongation of the rete ridges may simulate invasion when specimens are cut tangentially. Properly oriented specimens and careful examination will usually distinguish PEH from SCC, but immunostaining may aid differentiation.
The second entity, necrotizing sialometaplasia, is thought to be the result of infarction of salivary tissue. It is extremely uncommon in the larynx, but a few cases have been reported. It may develop in the larynx after ischemia or trauma and is characterized by squamous metaplasia of the ducts and acini of seromucinous glands, which may be confused with SCC or mucoepidermoid carcinoma (MEC). This lesion resolves spontaneously. IHC may be required to differentiate necrotizing sialometaplasia from SCC and certain nonsquamous malignancies such as MEC, neuroendocrine carcinoma, malignant melanoma, or lymphoma; these may have a similar appearance when examined histologically.
The symptoms of laryngeal SCC depend on the site from which the primary tumor originates. The cardinal symptom of glottic SCC is dysphonia, which develops early in the course of the disease because the normal vibratory characteristics of the vocal cord are altered by even a small lesion. Therefore patients with glottic SCC usually come to medical attention with earlier stages of disease, although if the early symptoms are ignored or attributed to other diagnoses, symptoms of advanced disease, such as dyspnea and stridor, may arise. Glottic tumors remain localized in the glottis for prolonged periods, owing to the natural barriers to tumor spread—ligaments, membranes, and cartilages—and to the relative paucity of glottic lymphatics. Supraglottic tumors may cause dysphonia, which often manifests as an alteration in vocal resonance, and they may also cause dysphagia, odynophagia, otalgia, stridor, dyspnea, and hemoptysis. Patients with supraglottic SCC may also be seen initially with metastatic cervical adenopathy without obvious laryngopharyngeal symptoms. Supraglottic cancers must grow large enough to cause obstructive symptoms, and at that point, they have often spread via the rich lymphatics to both sets of cervical lymph nodes. SCC of the subglottis often is seen with advanced stage disease, and dyspnea and stridor are the most common symptoms of subglottic SCC. Because onset is usually gradual and insidious, subglottic SCC may be misdiagnosed as asthma or some other pulmonary disease.
On examination of the larynx, SCC may appear as an ulcerative, exophytic, sessile, or polypoid lesion. However, in cases of ventriculosaccular SCC, which is uncommon, an epithelial lesion may not be seen in the early stages, because the carcinoma arises from the ventriculosaccular system, which lies within the paraglottic space. Fullness of the vestibular fold may be the only obvious examination finding. In this scenario, deep biopsies of the vestibular fold are necessary to confirm or exclude the diagnosis of malignancy. A second clinical presentation in which occult laryngeal SCC may be the underlying etiology is that of the laryngocele. An association between laryngoceles and SCC has been recognized for some time. In patients with laryngoceles, direct laryngoscopy with careful inspection of the ventricle using angled endoscopes is mandated to exclude SCC of the ventricle.
The incidence of cervical metastases from SCC of the larynx, as well as the nodal groups involved, varies according to the site of the primary tumor ( Fig. 105.8 ). Because of its rich network of lymphatics, supraglottic SCC has the highest incidence of regional metastases, both clinically apparent and occult metastases. Cervical metastasis has been confirmed pathologically in 10% of T1, 29% of T2, 38% of T3, and 57% of T4 supraglottic lesions. The incidence of occult metastases (cN0, pN+) in supraglottic SCC varies from 12% to 40% for all T stages. The incidence of occult metastases is greater in tumors with a higher T stage; the rate for T1 staging is 0% to 14%; for T2, the rate is 20% to 21%; for T3, it is 28% to 35%; and for T4 lesions, it is 40% to 75%. Supraglottic SCC usually metastasizes to Levels II, III, and IV. Levels I and V are involved by metastases rarely and only when other nodal levels are also involved. Bilateral metastases, both palpable and occult, occur frequently in supraglottic SCC and are more common in midline or bilateral tumors. Therefore in cases of supraglottic SCC, surgical treatment of the N0 and N1 neck is usually with a bilateral selective neck dissection (Levels II through IV). For N2 or N3 disease, a comprehensive neck dissection (Levels I through V) is indicated.
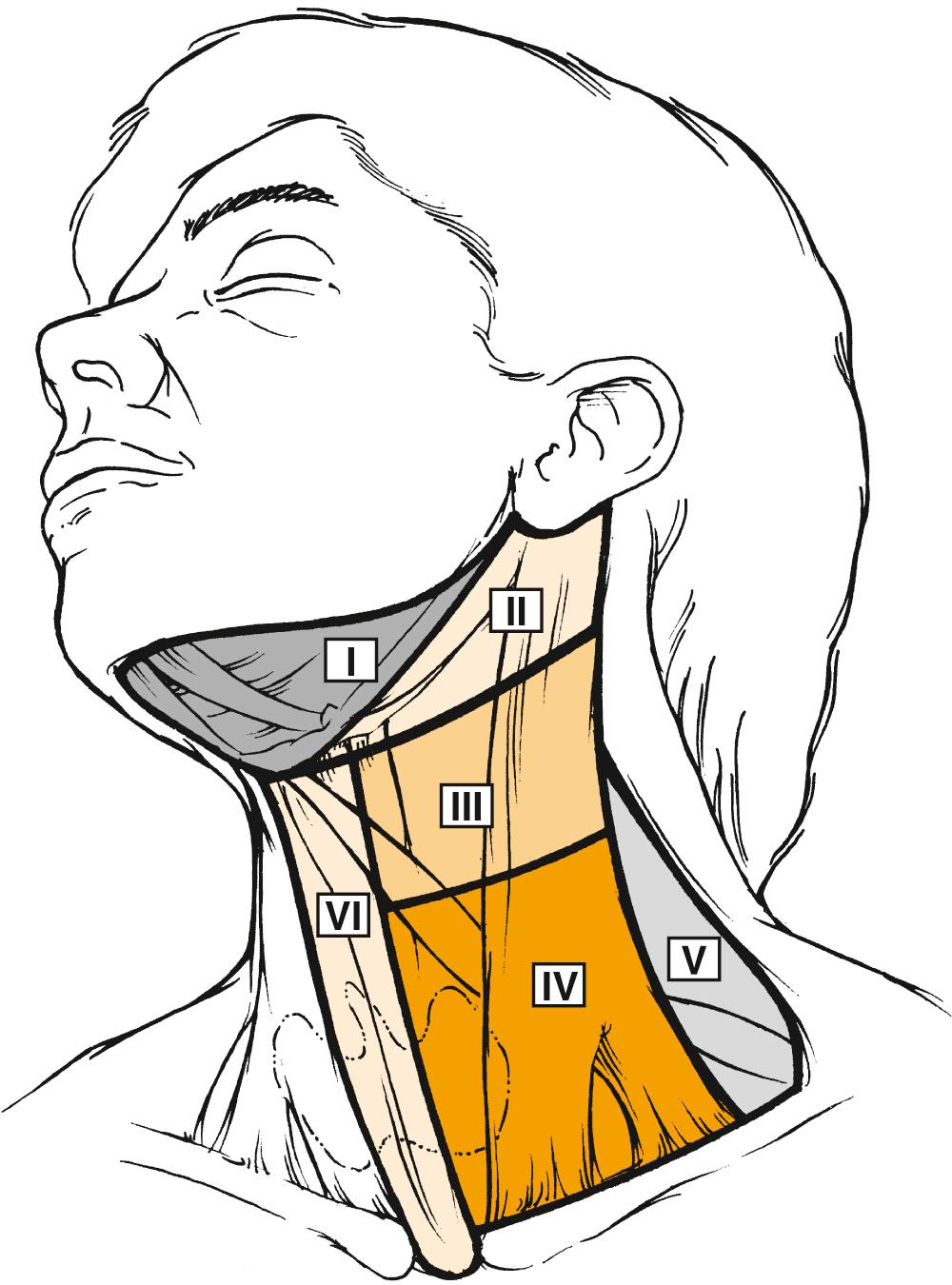
Glottic SCC has a low risk of cervical metastasis. In a series of 910 patients, the overall incidence of pathologically confirmed nodal metastasis was 5.9%, with an incidence of occult metastasis of 18%. Similar to supraglottic SCC, the incidence of regional metastasis correlates with T stage. In the same series, nodal metastases were found in 0.1% of T1 (one patient only), 5% of T2, 18% of T3, and 32% of T4 tumors. The nodes at risk of metastasis from glottic SCC are those in Levels II, III, IV, and VI—the prelaryngeal, pretracheal, and paratracheal nodes. Bilateral or contralateral metastases are rare.
Primary subglottic carcinoma is rare, and descriptions of the clinical behavior of these tumors are based on a small number of patients. The paratracheal nodes (Level VI) are most frequently involved with metastases, including contralateral or bilateral metastases. Metastases to Levels III, IV, and V are uncommon. Although these tumors are aggressive and have a poor prognosis, the incidence of cervical metastasis is generally reported to be low, with a range of 4% to 27%. However, Harrison detected metastatic tumor in approximately 50% of serially sectioned paratracheal nodes. Metastases to mediastinal lymph nodes are common (up to 46%), but they are classified as distant metastases.
Distant metastases from laryngeal SCC include not only hematogenous metastases to distant organs but also lymphatic metastases to nodal groups outside the neck. The most common site for distant hematogenous metastasis is the lung. The liver and skeletal system (ribs, vertebrae, and skull) are affected less often. The mediastinum is the most common site for distant lymphatic metastases, which are uncommon at initial presentation. Patients who develop distant metastases have almost always had regional metastases diagnosed at some stage in the course of their disease. The incidence of distant metastasis varies according to the site of the primary tumor: the rate is 3.1% to 8.8% in glottic SCC and 3.7% to 15% in supraglottic SCC. Supraglottic SCC usually has a higher incidence of distant metastases compared with glottic SCC. The frequency of distant metastases from subglottic SCC is less certain, because primary tumors in this site are rare; however, Spector and colleagues observed that 14.3% of subglottic SCCs developed distant metastases. Clinical and pathologic factors associated with an increased risk of distant metastases include an advanced-stage primary tumor, especially stage T4; the presence of cervical metastases, especially N2 and N3 disease; the duration, level, and extracapsular spread of cervical metastases; and locoregional recurrence. Lymphatic metastasis to the skin is also a sign of advanced disease and, similar to distant metastases, portends a grave prognosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here