Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Thyroid gland malignancies account for about 3% of all cancers (13.5/100,000 population), while representing the most common malignancy of the endocrine system. In general, thyroid cancer afflicts young to middle-aged adults with environmental, genetic, and hormonal factors often playing an etiologic role. Iodine is essential for normal thyroid function and consequently, radioactive iodine can be used in treatment. Women are affected by thyroid diseases nearly four times as frequently as men. Fine needle aspiration (FNA) has contributed significantly to the assessment of thyroid nodules, especially ultrasound-detected masses, with a corresponding decline in use of nuclear scintigraphy. FNA is satisfactory or unsatisfactory, making certain to meet the adequacy criteria as established by the Bethesda system. Satisfactory lesions are then separated into benign, follicular lesion of undetermined significance, neoplasms, suspicious for malignancy, and malignant. There is a sensitivity for cancer of 65% to 98%, specificity of 72% to 100%, and a positive predictive value of 90% to 96%. The false negative rate is from 1% to 11%, while the false positive rate is less than 1%. Most of the tumors are of thyroid follicular cell derivation and, for the most part, carry an excellent long-term prognosis.
Adequacy of tumor sampling is frequently a question. It is my practice to submit at least one section per centimeter of tumor diameter, but with an attempt to submit the whole periphery of the tumor. If the tumor looks macroscopically homogeneous after being bivalved, then the center of the tumor is not as critical to examine. The tumor is serially sectioned at 2 to 3 mm. Then, only the very periphery of the tumor to capsule to parenchymal interface is embedded. As many as five sections, 3 mm thick and up to 2.5 cm long, can be placed side by side in the 2.5 cm wide cassette. With this technique, the periphery of most tumors can be entirely embedded in 4 to 8 blocks, allowing for complete evaluation of the capsule.
“A malignant epithelial tumor showing evidence of follicular cell differentiation and a set of distinctive nuclear features. Either papillae or invasion are required” is a somewhat vague World Health Organization (WHO) definition of papillary thyroid carcinoma (PTC). However, with a constellation of architectural and cytomorphologic features, accurate diagnosis of papillary carcinoma is achievable.
Papillary carcinoma represents about 80% to 85% of all malignant thyroid neoplasms and occurs largely in middle-aged adults with a 3 : 1 female-to-male ratio, and a median age at presentation of 50 years. Even though rare in children, papillary carcinoma is still the most common pediatric thyroid malignancy. Whites are affected more commonly than blacks. Curiously, there is about a 20% prevalence of PTC (autopsy studies), supporting the overall excellent long-term prognosis and highlighting the difficulty in deciding appropriate patient management. There is a close link with radiation exposure, an association much more highly developed in children (especially for the solid variant of PTC). There is also a higher incidence of carcinoma in regions with high dietary iodine intake, in patients who have preexisting benign thyroid disease, and in some inherited disorders (Carney complex; familial adenomatous polyposis [FAP]). Patients present with a solitary, painless otherwise asymptomatic thyroid gland mass ( Fig. 25.1 ) or with cervical lymphadenopathy (metastatic disease in about 30%). Dysphagia, stridor, and cough are usually seen in patients with large tumors due to compression. There are many “incidental” papillary carcinomas (discussed later), which are frequently discovered during routine radiographic studies for unrelated reasons or in patients with other thyroid diseases. FNA is the initial study of choice for a thyroid nodule, with excellent positive predictive value. Thyroid function studies are not useful in the initial evaluation of patients as there is rarely functional compromise. However, serum thyroglobulin levels can be used to monitor disease status (if elevated).
A malignant epithelial tumor showing evidence of follicular cell differentiation and a set of distinctive nuclear features
Thyroid malignancies represent about 3% of all carcinomas
80%-85% of thyroid malignancies are papillary thyroid carcinoma
Recurrent laryngeal nerve damage and hypoparathyroidism
Excellent long term outcome (> 90% 20-year survival)
Females > > Males (3 : 1)
Age: 20-60 years; median: 50 years
Associated with radiation exposure
Usually a palpable painless (asymptomatic) mass lesion, often with neck lymph nodes
Uncommonly, dysphagia or hoarseness
Ultrasound shows a solid or cystic mass and guides FNA
Computed tomography is useful to determine extent of the mass and lymph node disease
Nuclear scintigraphy seldom used
Excellent long term prognosis (> 90 % 20-year survival)
Surgery (lobectomy or thyroidectomy) with follow-up radioactive iodine (in total thyroidectomy patients)
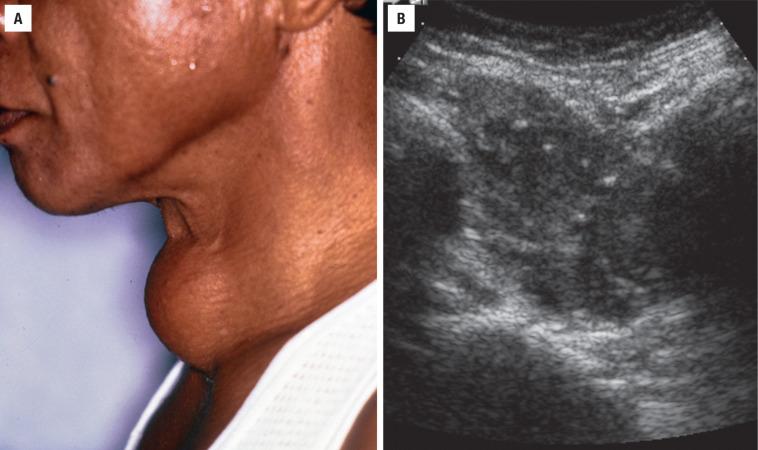
Ultrasound will usually establish the size and whether the lesion is solid or cystic, while also being a valuable adjunct for guiding FNA. Punctate microcalcifications are frequently present ( Fig. 25.1 ), with high central blood flow on color Doppler. While nuclear scintigraphy was widely used to demonstrate functionality (“cold” without uptake; “hot” increased uptake) in comparison to the uninvolved thyroid parenchyma, it has been almost completely replaced by ultrasound and FNA as the techniques of choice in initial evaluation of a thyroid nodule. CT or MRI scans are valuable in highlighting enlarged, cystic lymph nodes, which may suggest metastatic disease, showing increased signal intensity on T1-weighted images, and may reveal punctate calcifications.
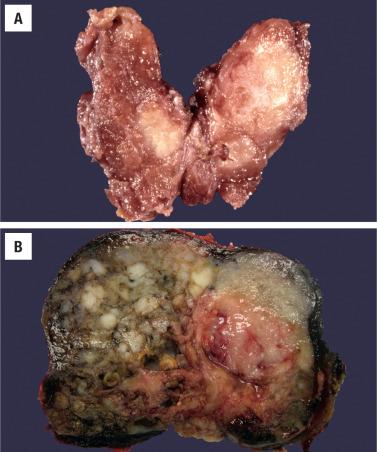
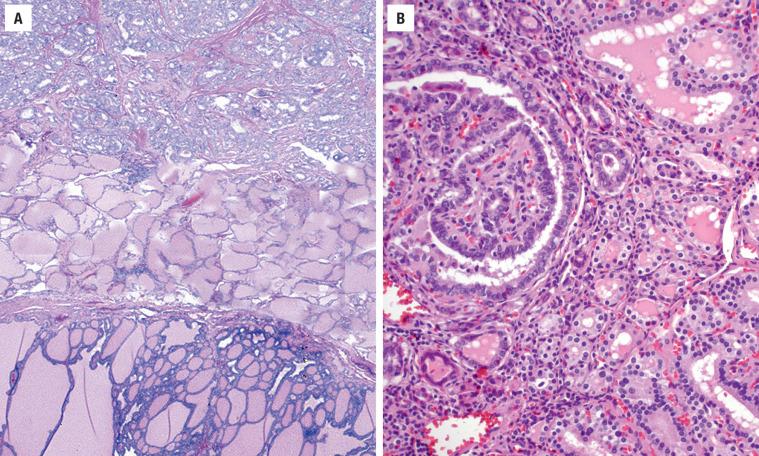
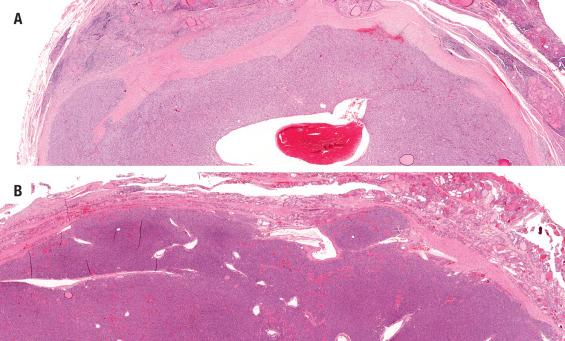
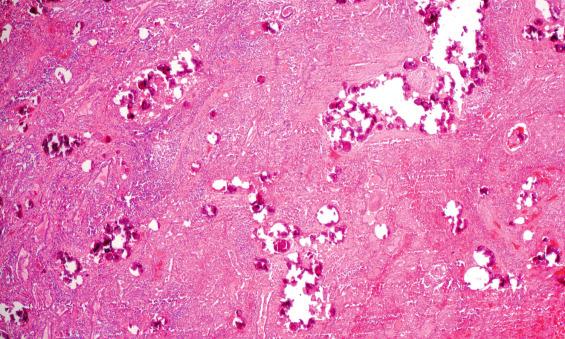
Most clinical tumors are discrete, ill-defined but circumscribed, often with an irregular and infiltrative border ( Fig. 25.2 ). Ranging from microscopic to 20 cm, infiltration into the surrounding thyroid parenchyma is frequently noted, along with extension beyond the thyroid gland periphery. Gritty, dystrophic calcification is common, while cystic change and hemorrhage may also be present. Multifocality is occasionally identified macroscopically. The cut surface can be shaggy to papillary, with irregular areas of fibrosis. The best sections to submit capture the “tumor-to-capsule-to-parenchyma” interface.
Discrete, grey-white, firm mass with irregular borders, although often circumscribed
Calcifications give a “gritty” cut surface
Extrathyroidal extension may be seen
Up to 20 cm; average about 3 cm
Architecture: Variable growth patterns, complex papillae, elongated and twisted follicles, invasive growth, psammoma bodies, “bright eosinophilic” colloid, crystals, and giant cells in colloid
Cytology: Enlarged cells, increased nuclear to cytoplasmic ratio; nuclear enlargement, nuclear overlapping and crowding, loss of polarity; nuclear contour irregularities, grooves, folds or “crescent moons,” nuclear chromatin is cleared, pale, fine delicate to even, with intranuclear cytoplasmic inclusions
Intratumoral fibrosis, psammoma bodies, colloid scalloping
TTF1, thyroglobulin, PAX8, CK7, CK19
Panel: HBME-1, galectin-3, CITED1 positive
Cellular aspirate with papillary and monolayered sheets, cuboidal cells with enlarged and overlapped nuclei, powdery nuclear chromatin with nuclear grooves and intranuclear cytoplasmic inclusions, and ropy, “bubble-gum” colloid
Adenomatoid nodules, diffuse hyperplasia (Graves' disease), dyshormonogenetic goiter, follicular adenoma, papillary carcinoma variants, follicular carcinoma, medullary carcinoma, metastatic tumors
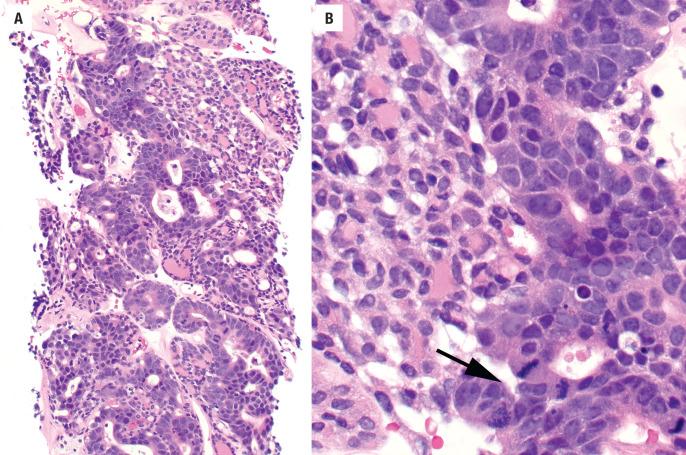
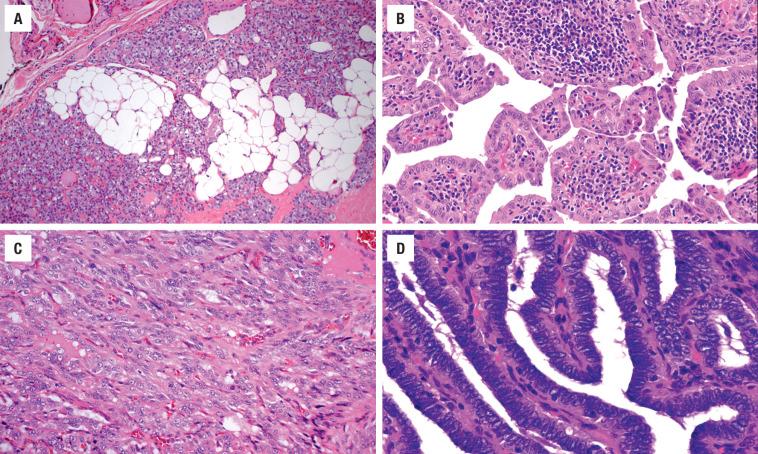
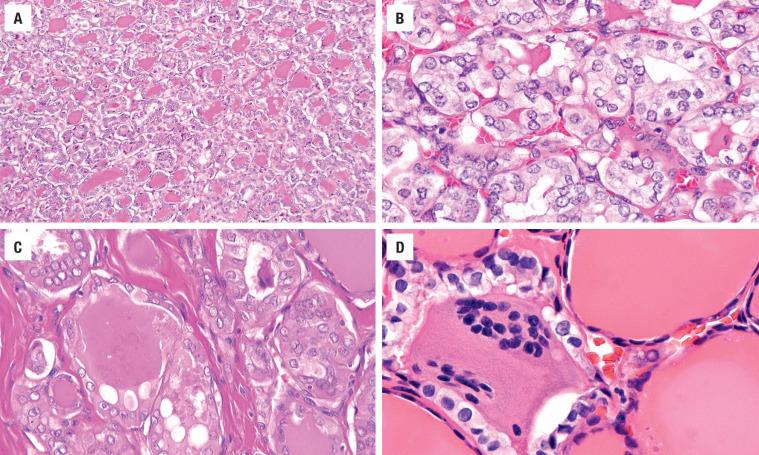
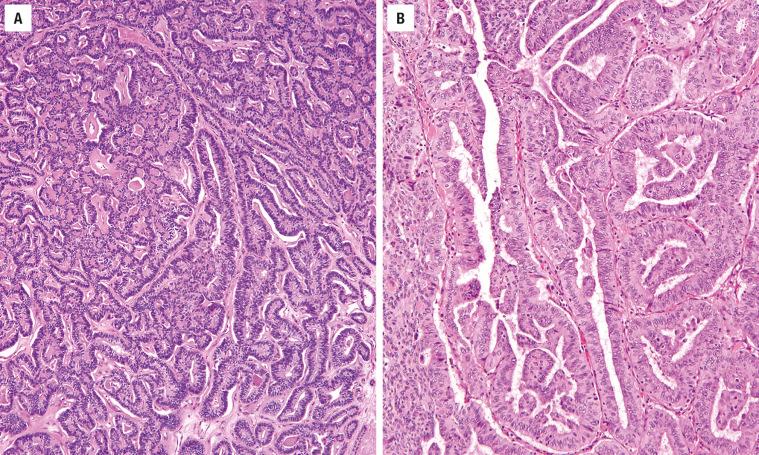
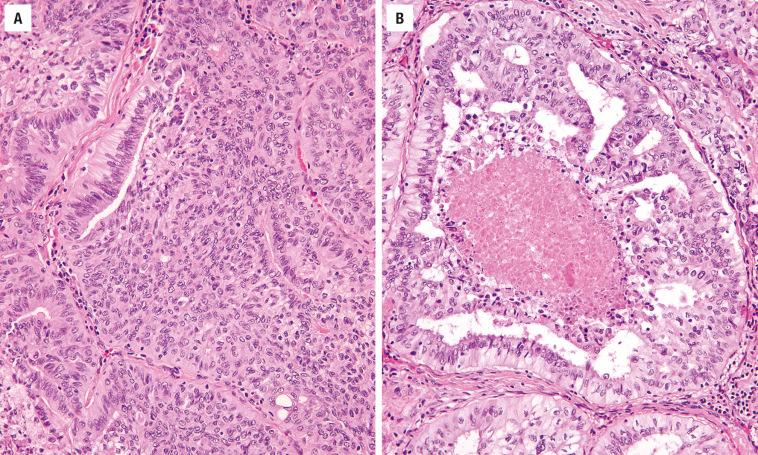
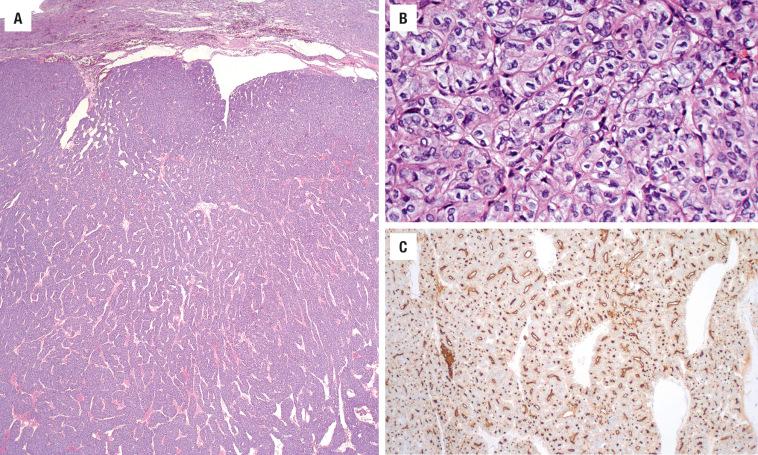
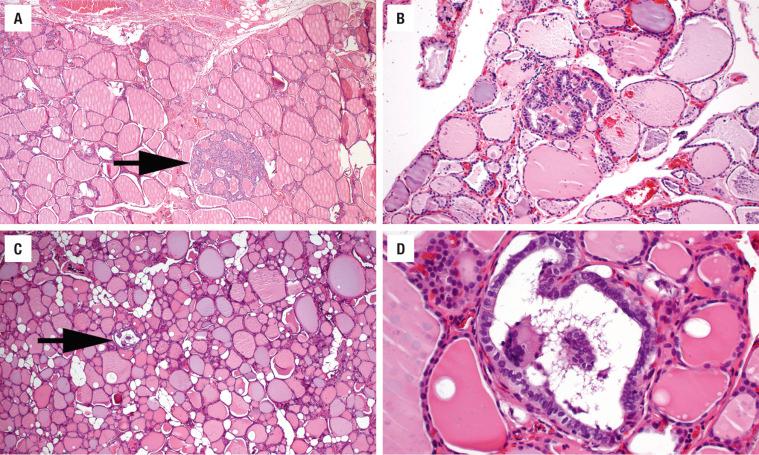
The diagnosis of papillary carcinoma is made by using an aggregate of architectural and cytologic features, with no one single feature being diagnostic. The exact number of features necessary for the diagnosis is undefined, but the nuclear features must be present to be diagnostic. Multinodular and multifocal tumors are common ( Fig. 25.3 ), seen in about 50% of cases. An irregular and invasive border is common, with both capsular and lymphovascular invasion ( Fig. 25.3 ). Extrathyroidal extension involves expansion of tumor into skeletal muscle ( Fig. 25.4 ), adipose tissue, around nerves, and adjacent to large perithyroidal vessels. Only macroscopic evidence of extrathyroidal extension, however, is evaluated in staging. The architectural features in PTC include variable growth patterns (papillary, solid, trabecular, micro- or macrofollicular, cystic); elongated and/or twisted follicles; complex, arborizing, delicate, narrow papillae; intratumoral dense acellular fibrosis; “bright,” hypereosinophilic, intense colloid (distinct from surrounding thyroid parenchyma); and psammoma bodies (concentrically laminated calcific bodies; Figs. 25.5–25.10 ). If a single tumor has many different growth patterns, suspicion for papillary carcinoma should be raised.
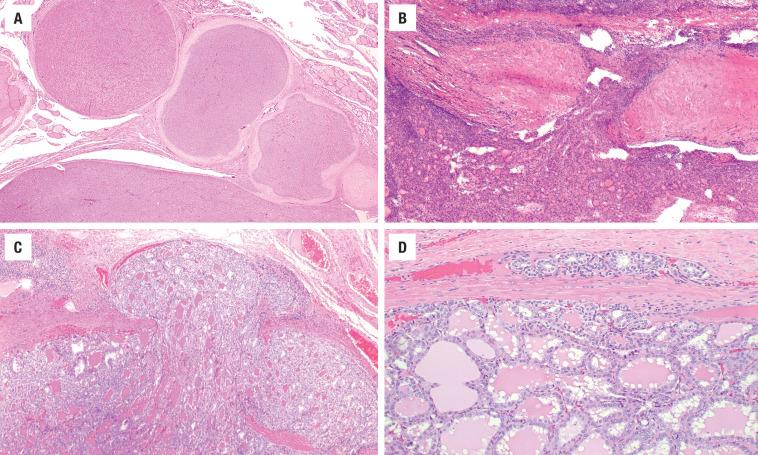
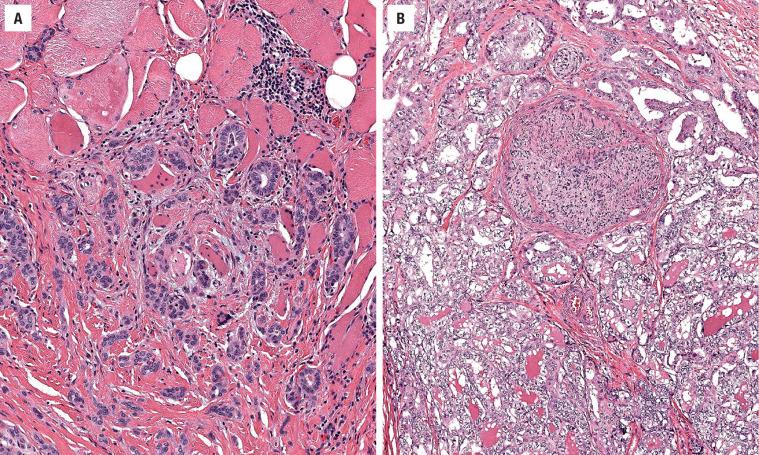
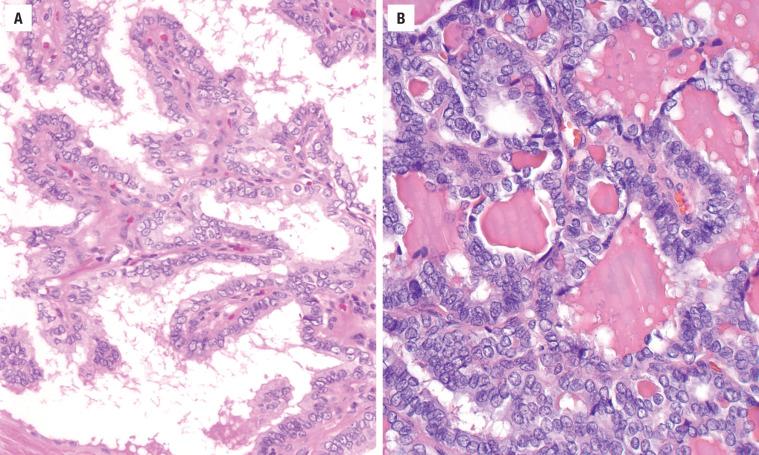
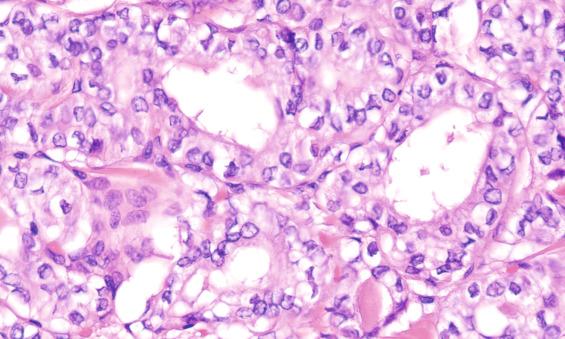
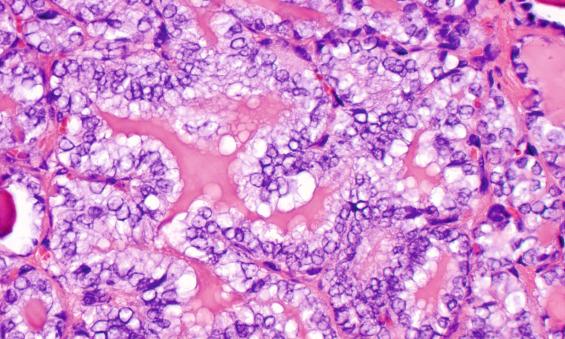
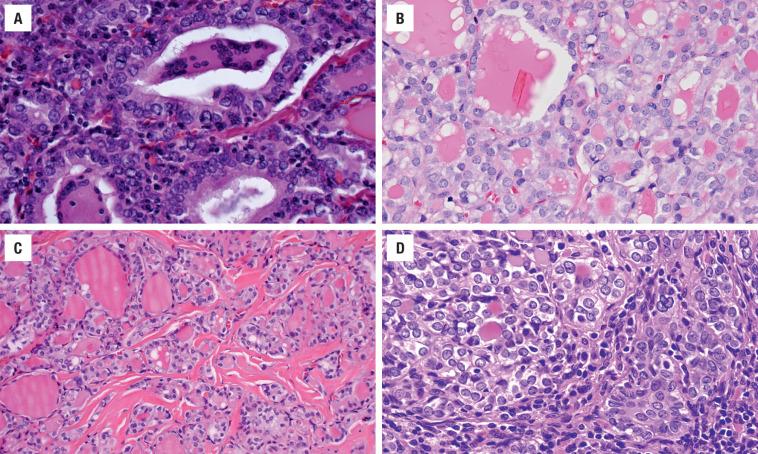
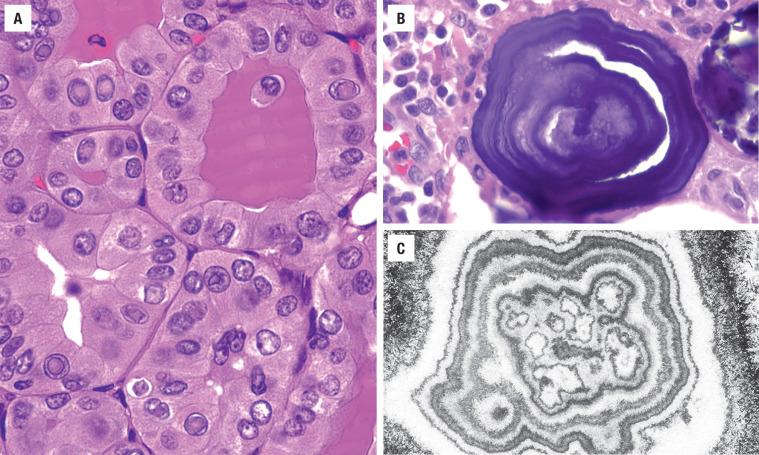
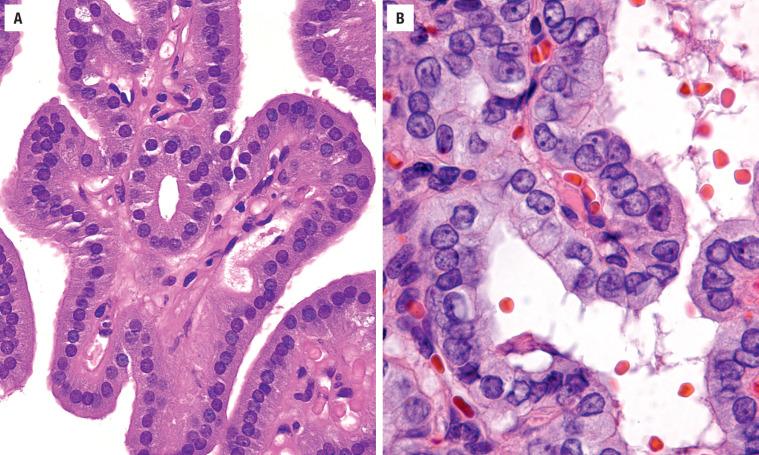
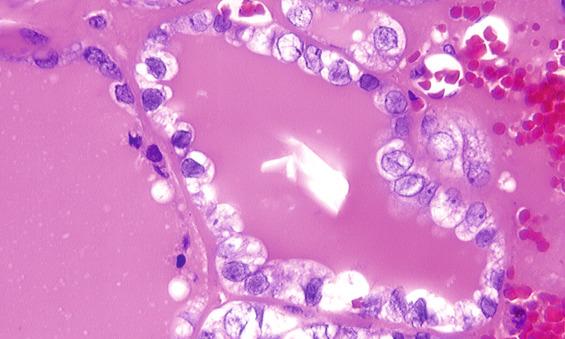
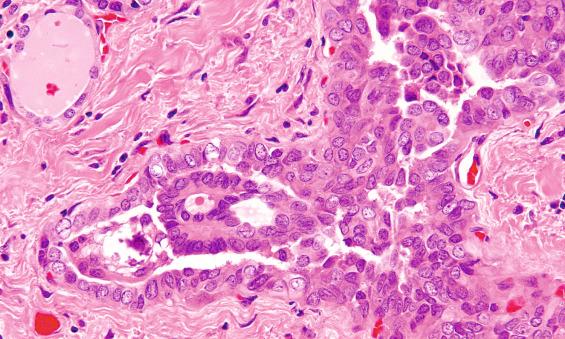
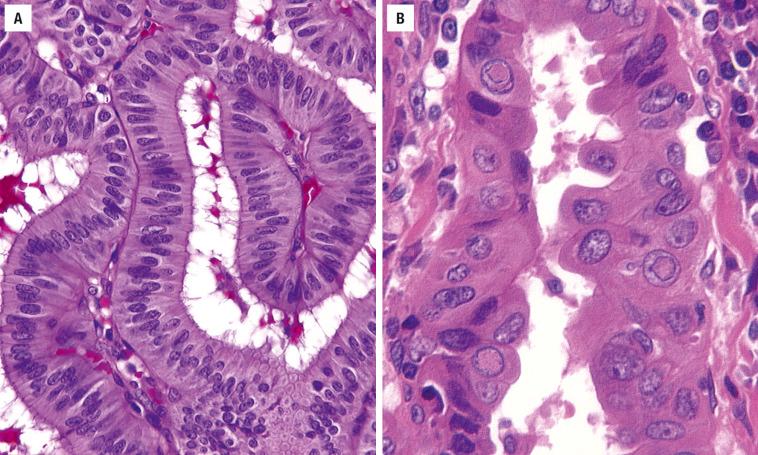
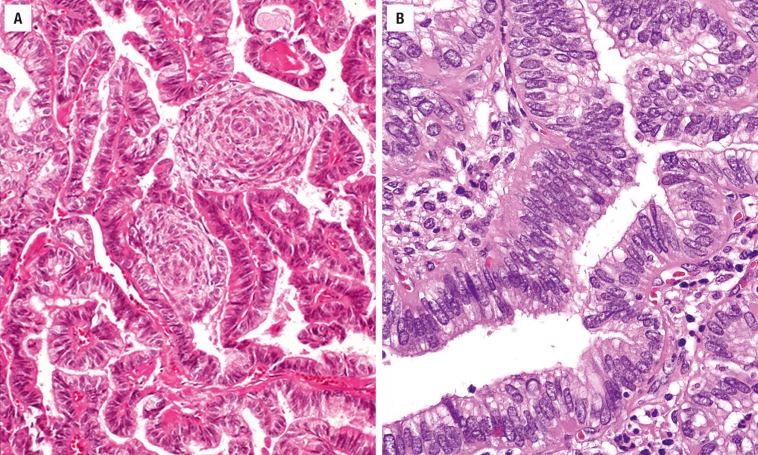
The cytomorphologic and nuclear features are vital in the diagnosis of papillary carcinoma and are usually constant even between the variants. These features are best assessed at the periphery of the tumor, where comparison can be made to the adjacent, uninvolved normal thyroid tissue. These features include enlarged cells with a high nuclear-to-cytoplasmic ratio; nuclear enlargement of oval to elongated nuclei; variability in size and shape, with nuclear overlapping and crowding; and loss of polarity and disorganized nuclear placement within the cell ( Figs. 25.5–25.9 ). The nuclear crowding creates a “herd,” “lake,” or “egg-basket” appearance ( Figs. 25.5 and 25.7 ). The nuclear chromatin is fine, delicate, even, and pale (“ground glass”) with chromatin margination or condensation (thick membranes) and clearing (“Orphan Annie” nuclei; Figs. 25.7 and 25.8 ). If slides are left on the heating block for too long or in an aqueous solution during processing, “false” intranuclear bubbles are created. Formalin fixation creates the clearing, since it is not seen in frozen section material nor in alcohol fixatives (SafeFix, HistoChoice). Nuclear grooves and longitudinal folds creating a “crescent moon,” triangular, angulated, or convoluted shape (“coffee bean,” “popcorn”) are characteristic ( Figs. 25.6 and 25.9 ). Nuclear envelope irregularities are more difficult to assess on frozen section material. Intranuclear cytoplasmic inclusions (pseudoinclusions) are recognized by the contents of the inclusion having an appearance similar to the cytoplasm—and not an artifactual “vacuole” formed secondary to fixation ( Fig. 25.10 ). Nucleoli, if present, are usually small and inconspicuous and seem to touch the nuclear membrane rather than being centrally located ( Fig. 25.9 ). The cytoplasm is variable and usually not helpful in the diagnosis, although variants are named according to the cytoplasm (clear, oncocytic, hobnail, columnar). Giant cells in the colloid and the presence of crystals are “soft” criteria, also seen in other lesions ( Fig. 25.9 ). Squamous metaplasia, cyst formation, and degeneration are not uncommon, with infarction induced by FNA ( Figs. 25.9 and 25.11 ). Psammoma bodies are not the same as dystrophic calcification of colloid in the center of a follicle. Psammoma bodies (Greek for “salt-like”) represent apoptotic cells that form the nidus for concentric lamellation of calcium ( Fig. 25.10 ). Present in up to 50% of cases, they are often identified within lymphovascular channels, diagnostic of intraglandular spread. Likewise, their presence in lymph nodes is pathognomonic for metastatic disease (any papillary pattern tumor may cause psammoma bodies), although potentially excluded in staging systems.
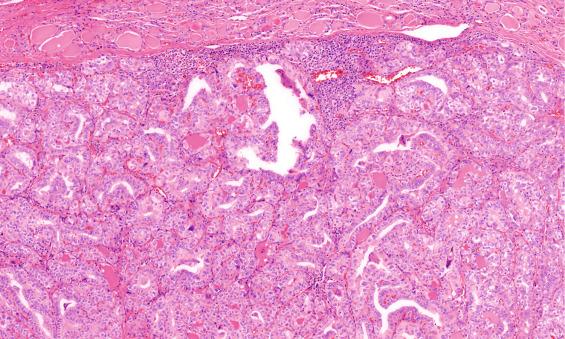
Mummification (peripheral cell death) is infrequently seen, but quite characteristic for papillary carcinoma ( Fig. 25.11 ). Separation of multifocal versus intraglandular spread of PTC can be difficult. Intraglandular spread is suggested when there are psammoma bodies within the septa or when there is viable tumor within a lymphovascular channel and has no stellate fibrosis at the periphery ( Fig. 25.12 ). Intratumoral fibrosis is an acellular, sclerotic, dense, eosinophilic fibrosis found in up to 90% of cases. The fibrosis is often irregular to stellate, a feature that is useful during gross examination to select areas for microscopic examination. Papillary carcinoma is not routinely graded, as nearly all are considered well differentiated. However, when there are increased mitoses (> 3/10 high power fields; Fig. 25.13 ) and tumor necrosis, then the tumor would be considered a poorly differentiated carcinoma. Tumor necrosis is uncommon in PTC, with its detection away from an FNA tract suggesting a more aggressive (poorly differentiated or undifferentiated) component within the tumor. A heavy lymphocytic response is frequently seen both adjacent to and within the tumor ( Fig. 25.14 ). Fatty metaplasia, spindled tumor cells and limited colloid may be seen ( Fig. 25.14 ). Variants are described in the next section.
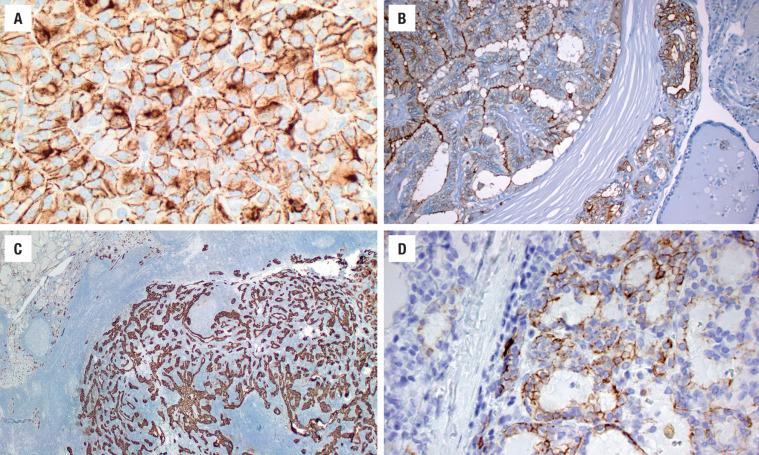
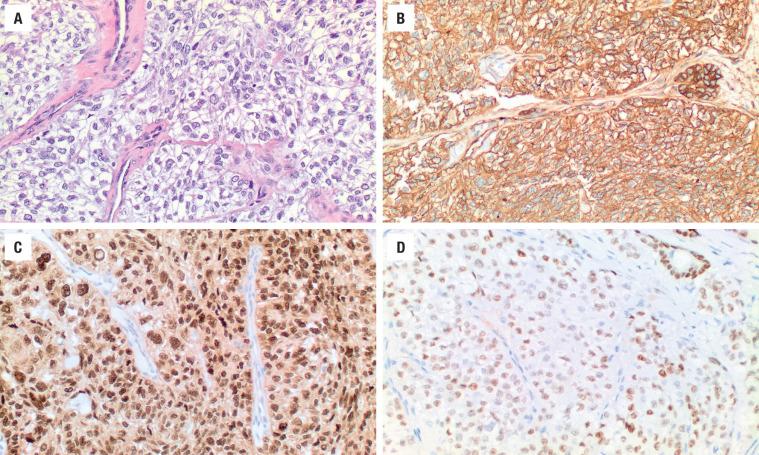
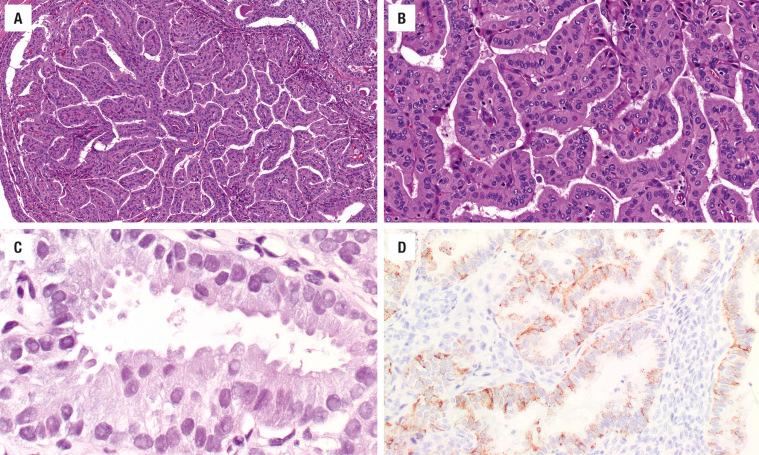
Immunohistochemistry is seldom of value in diagnosing PTC, although it may play a role in metastatic disease. The neoplastic cells are strongly and diffusely immunoreactive with keratin, CK7, thyroglobulin, TTF1, and PAX8, while other markers (HBME-1 [ Fig. 25.15 ], galectin-3, S100 protein, CITED1, CK19 [ Fig. 25.15 ]) yield variable results. In challenging cases, there is good sensitivity and specificity when using a panel approach: HBME-1 (membranous), galectin-3 (nuclear and cytoplasmic), and CITED1. However, for more than 98% of cases, immunohistochemistry is unnecessary. p27 (lost) and cyclin D1 (up regulation) shows differential staining in tumors that are more likely to metastasize.
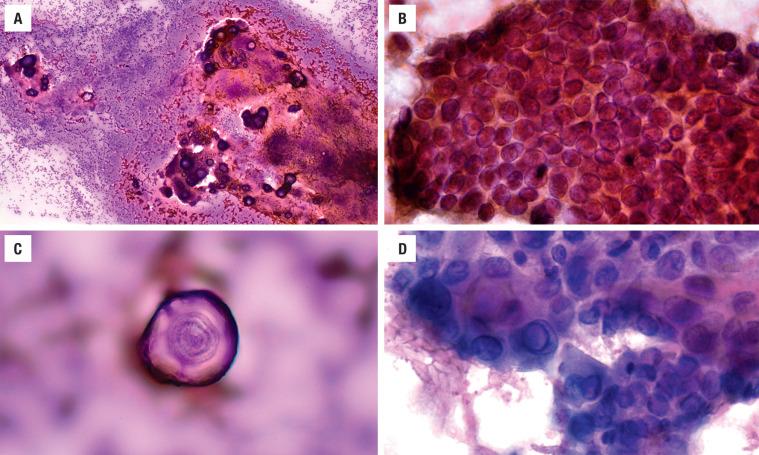
FNA is considered the test of choice for the diagnosis and management of thyroid nodules, having an excellent sensitivity, specificity, and positive predictive value. An initial pass using a 25-gauge needle—without suction—yields excellent material uncontaminated by blood. In general practice, about 70% of thyroid FNAs are benign, 10% are indeterminate, 15% are unsatisfactory, and 5% are malignant.
Aspirates from papillary carcinomas are usually diagnostic, meeting the adequacy criteria (at least 6 follicular groups with greater than 10 follicular cells per group) and are characteristically cellular, with monolayered sheets (syncytium) and three-dimensional clusters of enlarged cells ( Fig. 25.16 ). The nuclei are enlarged and overlapped with irregular borders, but with a powdery/dusty, delicate nuclear chromatin on alcohol fixed preparations. Nuclear folds or grooves and intranuclear cytoplasmic inclusions are also common. The cytoplasm is often pale or foamy, but not distinctive on FNA. Colloid is often scant and thickened (“chewing gum” or ropy), with occasional multinucleate giant cells and, rarely, psammoma bodies. The features of papillary carcinoma are best appreciated with alcohol-preserved Papanicolaou preparations rather than with air-dried material. With noninvasive follicular pattern tumors now recognized separately, they may show the nuclear features of papillary carcinoma. Thus, the definitive diagnosis of PTC on FNA material should be limited to those smears that show three-dimensional papillary structures and/or psammoma bodies.
Results are quite dependent on technique and the specific histologic variant. Most genetic alterations are mutually exclusive, with a majority of cases activating the mitogen-activated protein kinase (MAPK) pathway. In general, point mutations (such as BRAF V600E, NRAS ), gene fusions, or gene copy number variations account for the usual molecular findings. Point mutations in the BRAF gene are identified in up to 60% of papillary carcinomas (valine-to-glutamate substitution at residue 600: V600E), while other BRAF mutations (K601E) account for a minority of lesions. RAS gene ( NRAS , HRAS , KRAS ) mutations are seen in up to 15% of tumors, but almost exclusively in follicular patterned tumors. EIF1AX is also seen in follicular patterned tumors. Fusion genes often involve RET gene, while NTRK3 , NTRK1 , ALK , and others are also recognized. TERT mutations seem to be associated with higher risk of recurrence, distant metastases, and tumor-related mortality. Each mutation/fusion/rearrangement has distinct phenotypic and biologic properties. While not necessary for diagnosis, there may be value in inherited papillary carcinoma syndromes, such as FAP coli or Cowden syndrome, for genetic studies to help in patient management.
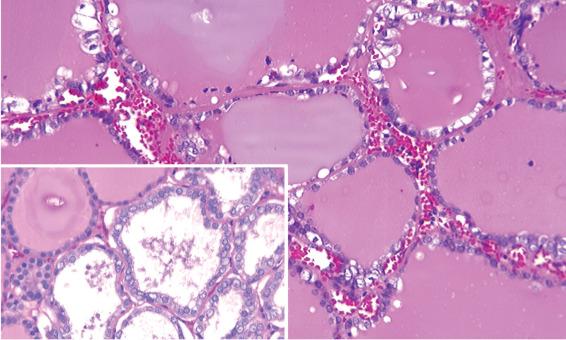
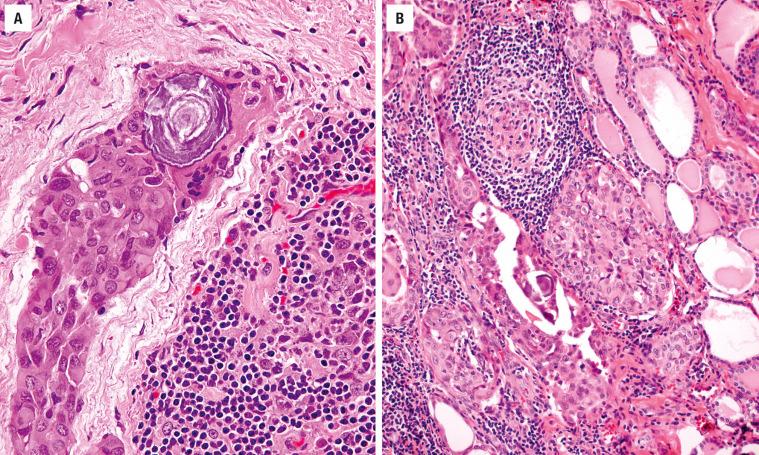
The principal differential diagnosis includes a number of disorders with papillae, including adenomatoid nodules ( Figs. 25.17 and 25.18 ), diffuse hyperplasia (Graves disease, Fig. 25.17 ), and dyshormonogenetic goiter, while follicular adenoma (FA), follicular thyroid carcinoma (FTC), medullary thyroid carcinoma (MTC), and metastatic tumors are also considered. In general, the papillae of all of these other lesions are short, simple, nonbranching, and often “thick.” The nuclei are round, regular, basally located, and hyperchromatic. Intracytoplasmic hemosiderin pigment is nearly always lacking in PTC. Although a nuclear feature or two may be present in these other lesions, there is both a qualitative and quantitative difference in their appearance. Many lesions that have oncocytic cytoplasm may induce nuclear enlargement, but other features of PTC are lacking. It is worth noting that noninvasive follicular thyroid neoplasm with papillary-like nuclear features is included in the differential diagnosis of follicular patterned tumors, and will be further discussed in the chapter on benign neoplasms.
Papillary carcinoma spreads preferentially by lymphatic channels, with the regional lymph nodes affected most commonly, and in a significant proportion of cases ( Fig. 25.19 ). Intraglandular spread, including the contralateral lobe, is common. However, the prognosis is excellent, with greater than 90% 20-year survival rate and a less than 0.2% mortality rate. Macroscopic extrathyroidal extension into the adjacent fat or skeletal muscle places the tumor in the American Joint Committee on Cancer (AJCC) stage pT3b (2017 criteria), but microscopic extension does not change stage. Age (<55 years) and sex (female) are the most important prognostic factors, although tumor size (> 4 cm), gross extrathyroidal extension, and metastasis are significant for patients ≥55 years. Surgery is the treatment of choice, although the extent of surgery (lobectomy, subtotal, or total thyroidectomy) remains controversial. Recurrent laryngeal nerve damage and hypoparathyroidism are known surgical complications. Radioablative iodine therapy is incorporated after a total thyroidectomy. However, the tumor needs to show uptake of the radiolabeled iodine to be therapeutically sensitive. Lymph node sampling is advocated only if there is clinical or radiographic enlargement.
Variants of papillary carcinoma have specific features that may be associated with a different patient outcome or cause difficulty with the differential diagnosis. In general, the changes should be the dominant finding to qualify as a histologic variant.
Classical histologic and architecture features of papillary carcinoma but in an entirely encapsulated tumor with only limited invasion
Most are encapsulated or very well circumscribed
Almost exclusively small follicles with scant, bright colloid
Classic nuclear features of papillary carcinoma
No tumor necrosis, increased mitoses, or dominant solid or other pattern
Invasion used to separate from noninvasive follicular thyroid neoplasm with papillary-like nuclei
Enlarged follicles with remaining features similar to follicular variant although nuclei are often flattened
Abortive, rigid papillae may be seen
Separation from adenomatoid nodule is imperative
30%–70% papillary architecture (criteria vary by study)
Enlarged cells with abundant oncocytic, glassy cytoplasm, apically-oriented enlarged nuclei with papillary features, increased number of intranuclear cytoplasmic inclusions
Degenerative changes common
Clear cytoplasm, although occasionally oncocytic and clear cells are combined
Must be separated from medullary and metastatic renal cell carcinoma
Focal to diffuse tumor cells spindling of proven epithelial cells (keratin and/or TTF1) that lack pleomorphism increased mitoses and necrosis
Follicular adenoma, follicular carcinoma, papillary carcinoma, paraganglioma, hyalinizing trabecular tumor, amyloid goiter, undifferentiated carcinoma, metastatic tumor, lymphoma
Diffuse, bilateral involvement, extensive fibrosis, innumerable psammoma bodies, extensive intravascular growth and extrathyroidal extension, florid squamous metaplasia, dense lymphocytic thyroiditis, solid or papillary growth of papillary carcinoma cells
Nearly all have extensive lymph node metastases
30%–70% of tumor area composed of cells that are at least three times as tall as they are wide, usually oncocytic cytoplasm, sharply defined cellular borders, increased intranuclear cytoplasmic inclusions, centrally placed nuclei within the cell
Papillary structures and parallel elongated follicles with limited colloid
Prominent papillary growth, parallel follicles (“railroad tracks”), scant colloid, syncytial architecture with prominent nuclear stratification, coarse nuclear chromatin, subnuclear cytoplasmic vacuolization, squamous metaplasia as “morules,” and increased mitotic figures
CDX2 and TTF1 reactive
Solid or insular pattern with nuclear features of papillary carcinoma
More common in children
Must lack features of another variant
Lacks increased mitoses and necrosis
Almost exclusively in female patients with FAP
Multiple encapsulated tumors, mixed patterns, cribriform dominant
Morules or whorls of squamous cells without keratinization, showing optical clearing
Columnar cells often have grooves and folds
Nuclear ß-catenin strong and diffuse; TTF1 and thyroglobulin: weak, focal and patchy
At least 30% of cells must have hobnail appearance, with protrusion into the colloid, apically placed nuclei with prominent nucleoli
Higher association with extrathyroidal extension, lymphovascular invasion, necrosis, and increased mitoses
Incidentally found, ≤ 1 cm papillary carcinoma with a proclivity for thyroid subcapsular location—designated “microcarcinoma” when not the reason for the surgery
Classical architecture and nuclear features of papillary carcinoma in a tumor that is totally encapsulated ( Fig. 25.20 ) with only limited evidence of invasion. In these cases, “encapsulated variant with invasion” is used to qualify the type of invasion. This tumor is separated from FA with papillary hyperplasia by the presence of classical papillary nuclear features. The papillary structures exclude a noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP).
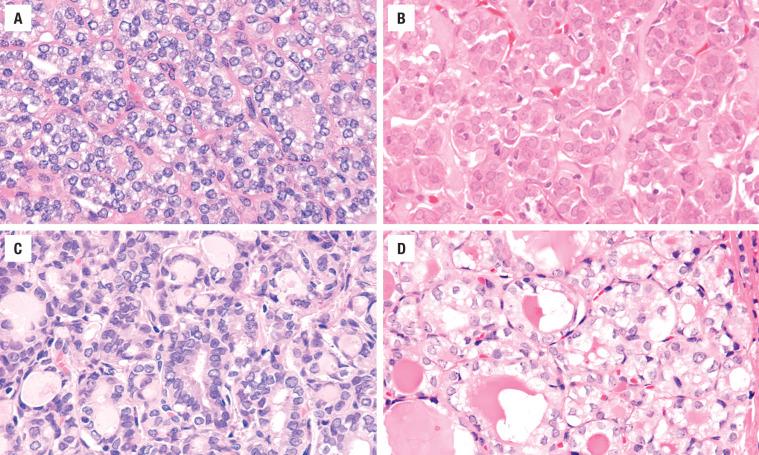
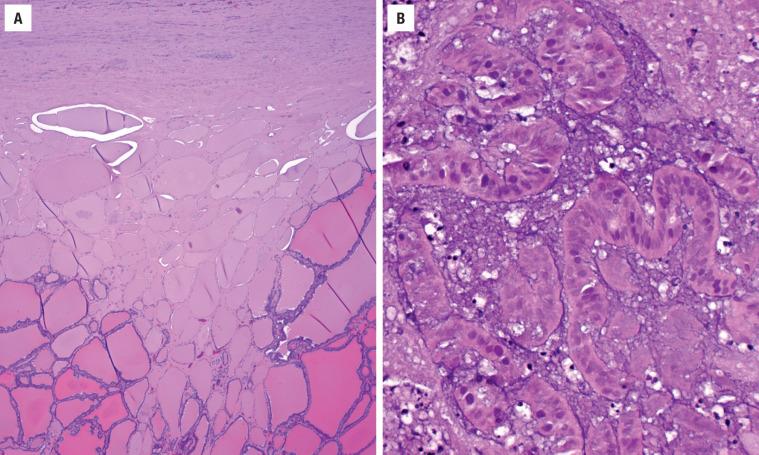
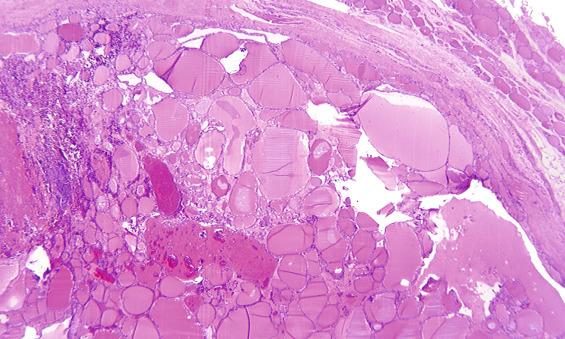
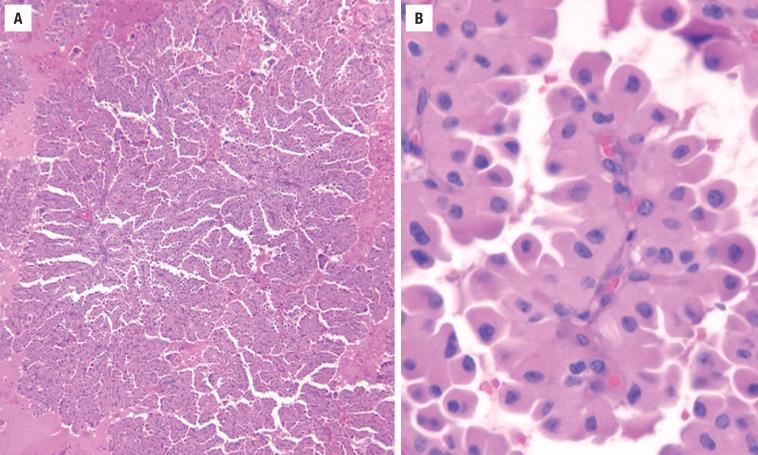
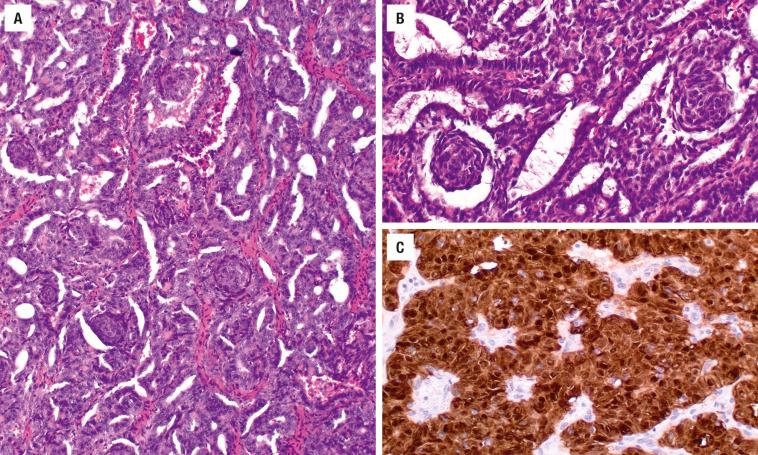
Usually encapsulated, the tumor must be predominantly composed of small, tight follicles with scant, hypereosinophilic colloid. Papillae are absent or less than 1% of the tumor volume ( Figs. 25.21 and 25.22 ). There are two types: encapsulated with invasion and infiltrative . By definition, invasion is present, otherwise the tumor would be considered as a NIFTP. The infiltrative form is sclerotic with easily identified invasion. The encapsulated with invasion type shows either capsular or lymphovascular invasion. The nuclear features determine the diagnosis in this variant. Specifically, the nuclei are large with pale to powdery to cleared nuclear chromatin and an increased number of nuclear grooves and folds ( Fig. 25.22 ). Internal sclerosis or fibrosis is seen ( Fig. 25.49 ). This variant has a similar outcome to conventional PTC.
This is an uncommon variant that is difficult to recognize as it has an architectural resemblance to adenomatoid nodules or hyperplastic nodules ( Fig. 25.23 ). The tumor is composed of predominantly large/macrofollicles with a subtle increased cellularity, often accentuated at the periphery ( Fig. 25.24 ). The colloid is often scalloped or vacuolated. The nuclei are often flattened and hyperchromatic, although classic papillary nuclei are scattered throughout the tumor ( Fig. 25.25 ). Abortive, “rigid” or straight papillary structures will extend into the center of the colloid-filled follicle, usually lined by the atypical cells. This variant seems to metastasize less frequently than classic papillary carcinoma, but otherwise is similar in treatment and outcome.
The macroscopic appearance is of a deep brown (“mahogany”) encapsulated neoplasm, which tends to be large and has cystic change. Lymphocytic infiltrate is common. More than 70% of the tumor should have complex, arborizing papillary structures ( Fig. 25.26 ), with fibrovascular stromal cores lined by enlarged cells with abundant oncocytic (oxyphilic, Askanazy, Hürthle) cytoplasm. Some authors use a lower cutoff, but this tends to dilute the category, with a few even suggesting a follicular oncocytic variant. The oncocytic cytoplasm is compact and “glassy” with a fine granularity, representing an increased number of mitochondria. The enlarged nuclei tend to be apically oriented and slightly more hyperchromatic than classic papillary carcinoma ( Fig. 25.27 ), with numerous intranuclear cytoplasmic inclusions (the latter a common finding in any tumor with abundant cytoplasm). Psammoma bodies are occasionally present. Degenerative changes are common. The cells are frequently immunoreactive with CK19, but this finding is nonspecific ( Fig. 25.27 ). The diagnosis by FNA is very difficult, but clear nuclei with grooves and inclusions may help to separate it from a follicular neoplasm. Oncocytic cells can be seen in the tall cell variant of papillary carcinoma, from which it should be separated. The patient outcome and management for the oncocytic variant is identical to classical papillary carcinoma.
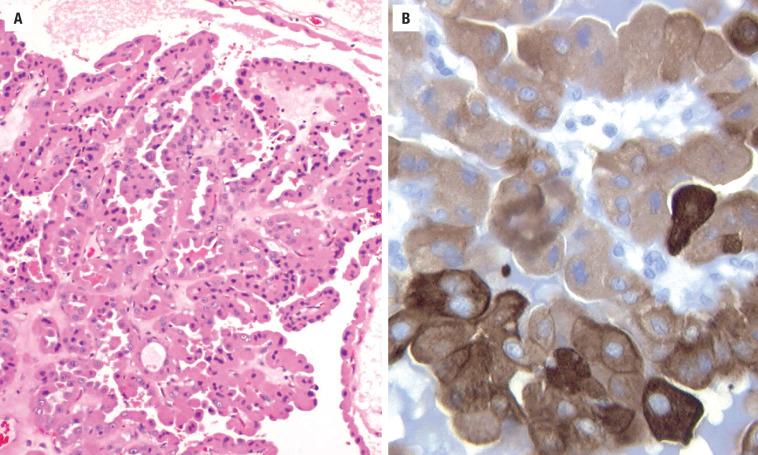
This is a very uncommon variant that is predominantly composed of cells with clear cytoplasm ( Fig. 25.28 ). Papillary or follicular patterns may predominate. Occasionally, a mixture of oncocytic and clear cells may be seen, as clearing results from degeneration of the oncocytic cells. Separation from metastatic renal cell carcinoma or medullary thyroid carcinoma can be made by the presence of colloid, but may require the use of TTF1, thyroglobulin ( Fig. 25.28 ), calcitonin, and CAIX. The treatment and prognosis are identical to classic papillary carcinoma.
Exceedingly rare, this variant shows focal to diffuse spindle cell proliferation not adjacent to a previous FNA site. The cells must be proven to be epithelial by cytokeratin and TTF1. The cells are bland, lacking increased mitoses and necrosis ( Fig. 25.14 ). This allows for separation from an undifferentiated carcinoma where there is profound pleomorphism, necrosis, and increased mitoses.
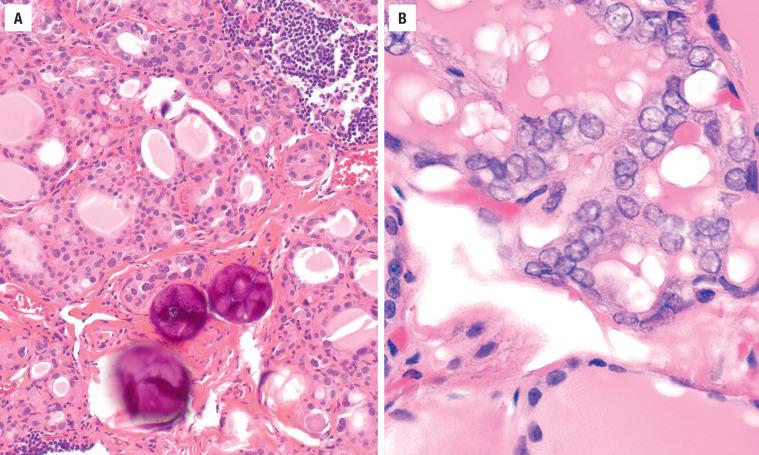
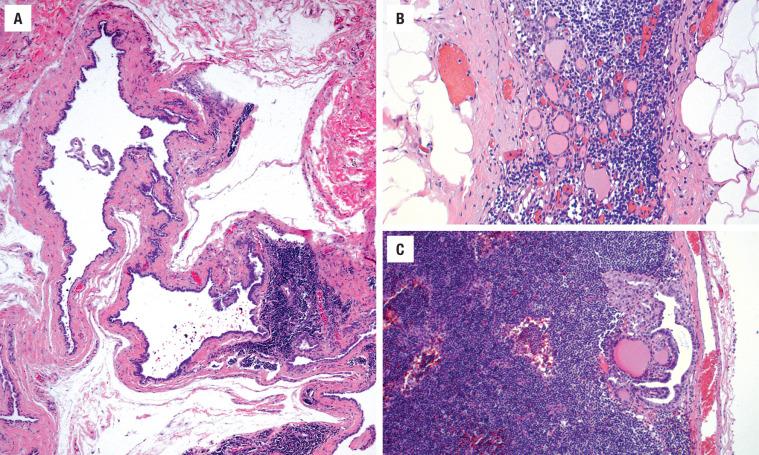
Usually developing in young patients (mean, 18 years), the tumor is characterized by diffuse involvement of one or both lobes with nearly 100% of patients demonstrating cervical lymph node metastasis at the time of presentation, while up to 25% develop distant metastases. The gland is firm, with white streaks and a gritty cut consistency, and an ill-defined border, if a dominant mass is noted. The histology shows an exaggeration of features of PTC, with extensive fibrosis, innumerable psammoma bodies, extensive intravascular and extrathyroidal extension, florid squamous metaplasia, and a background of dense lymphocytic thyroiditis (LT) ( Figs. 25.29 and 25.30 ). Nuclear features of papillary carcinoma are present, often identified in papillary or solid groups of cells within vascular spaces ( Fig. 25.31 ). Total thyroidectomy, lymph node dissection, and radioablative therapy will yield an excellent long-term prognosis despite the “biologically” aggressive clinical presentation. Lung metastases occur in up to 25% of patients, necessitating close and careful patient follow-up.
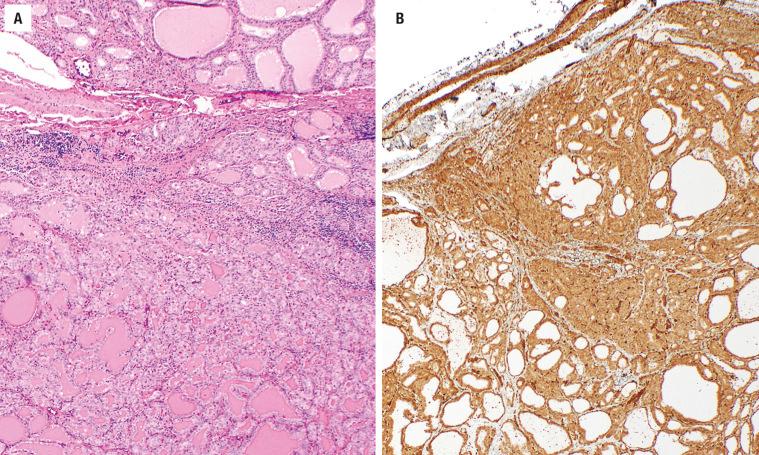
There is controversy as to whether the “tall cell” is a variant or just a pattern of growth within papillary carcinoma. When this cell type is the dominant finding in the neoplasm (range from 30% to 70%, but greater than 30% of the tumor area yields the most consistent correlation with outcome), the patients tend to be older (> 60 years), with an increased proportion of men, and the tumor tends to be large (> 5 cm), showing extrathyroidal extension. However, microscopic tumors may occur. Papillary structures and elongated parallel follicles with scant or no colloid are common ( Fig. 25.32 ), along with intratumoral fibrosis. By definition, a tall cell is at least three times as tall as it is wide (plane of section must be taken into consideration). There is usually abundant, granular cytoplasm, resulting in an increased number of intranuclear cytoplasmic inclusions and nuclear grooves ( Fig. 25.32 ). Intercellular borders are sharply demarcated. The nuclei are enlarged with a central position of the nucleus rather than at the luminal aspect as seen in the oncocytic variant ( Fig. 25.33 ). This variant stains positive with napsin, confounding when metastatic lung tumors are considered in the differential diagnosis ( Fig. 25.32 ). There is a high association with BRAF and TERT mutations, and also a high de-differentiation rate to undifferentiated carcinoma. There is an increased incidence of lymph node metastasis and hematogenous spread to bone and lung, with a tendency for local recurrence and invasion into adjacent structures. Surgery and adjuvant therapy are necessary, with a worse prognosis than classic papillary carcinoma.
Men and women are equally affected by this rare variant. Tumors are usually large (> 5 cm) and encapsulated, but have intra- and extrathyroidal spread. There is prominent papillary growth with markedly elongated, parallel follicles (“railroad tracks”), which are separated by scant colloid ( Fig. 25.34 ). The cells are tall with a syncytial arrangement. There is prominent nuclear stratification of elongated nuclei with coarse and heavy chromatin deposition, distinctly different from classic papillary carcinoma. Subnuclear or supranuclear vacuolization of the cytoplasm is common ( Fig. 25.35 ). Squamous metaplasia is common (“endometrioid pattern”; Fig. 25.36 ). Mitotic figures may be present, along with necrosis in a few cases. There is often CDX2 immunoreactivity, but TTF1 is also seen. If the patient is older with a large tumor that has extrathyroidal extension, more aggressive surgery and radioablative therapy may be necessary. The prognosis is worse than for classic papillary carcinoma, although it may be more a feature of infiltration than cytologic variant. Some examples of columnar variant histologically overlap with the more indolent cribriform-morular variant (discussed below). In these very uncommon and unusual histologic variants, performing selected immunohistochemistry studies (such as β-catenin in cases with squamous metaplasia) may be of value.
Papillary carcinoma may have a solid or insular pattern, with oval nests or islands with scant colloid, and cells with a high nuclear-to-cytoplasmic ratio ( Fig. 25.37 ). It is seen more often in children. This term is applied when the tumor is predominantly solid, trabecular, or nested, and does not show features of another variant. Sometimes the pattern is classified as poorly differentiated, but if the nuclear features of papillary carcinoma are present, then this pattern does not influence the management or the outcome. It is only when increased mitoses and necrosis are present that the tumor moves to the poorly differentiated category ( Fig. 25.13 ).
Seen almost exclusively in females, there is a high association with FAP, with a diagnosis of this variant prompting colonic examination and possibly genetic testing for germline APC mutation. In syndrome cases, there are often multiple encapsulated tumor nodules, showing a mixed pattern of growth: cribriform, trabecular, solid, papillary, and follicular ( Fig. 25.38 ). Colloid is scant to absent. There are often whorls or morules composed of spindle cells without keratinization, showing an optically clear nucleus. The nuclear features of papillary carcinoma are rare, taking more of a columnar shape, but still containing grooves and folds ( Fig. 25.38 ). TTF1 and thyroglobulin staining is weak, patchy, and focal, while a strong nuclear β-catenin accumulation ( Fig. 25.38 ) and immunoreactivity to ER and PR are characteristic.
This is an uncommon variant, requiring at least 30% of the cells to have hobnail features although this percentage is a source of debate. The variant shows complex papillary and micropapillary structures. These structures are lined by follicular cells that have a hobnail appearance, with apically placed nuclei showing prominent nucleoli. The cells tend to be dyscohesive. This variant has necrosis, mitoses, and frequent extrathyroidal extension and lymphovascular invasion.
Any of the papillary carcinoma variants may be less than 1 cm in size, which is referred to as microscopic papillary carcinoma, or occult, incidental, or microcarcinoma ( Fig. 25.39 ). This qualification should only be applied when the tumor is found incidentally in a thyroid gland removed for other reasons. The tumor has a proclivity to develop in the subcapsular region and is frequently sclerotic with a radiating “scar-like” infiltration into the surrounding parenchyma. The term “microcarcinoma” should be used for adult patients, since children with small tumors may still have biologically aggressive neoplasms. Separation from intraglandular metastasis may be difficult, although the intravascular location, lack of capsule and sclerosis, and lack of “stellate” growth supports intraglandular metastasis. Most of these tumors are less than 2 mm in size and are of limited clinical consequence, with an outcome indistinguishable from the general population. Therefore, no additional therapy is necessary for tumors of this size. The noninvasive tumors may qualify as the newly recognized noninvasive follicular thyroid tumor with papillary-like nuclear features, but by definition, they are tumors > 1.0 cm.
Follicular carcinoma (FC) is the second most common malignant neoplasm of the thyroid gland, defined by invasive growth of an encapsulated follicular epithelial-derived cell that lacks the nuclear features of papillary carcinoma. There is a familial association in up to 4% of FC in the U.S., with PTEN hamartoma tumor syndrome (Cowden disease, Werner syndrome) and Carney complex the most common ( Fig. 25.40 ). Iodine deficiency, radiation exposure (5.2 times relative risk), and pre-existing thyroid disease are known risk factors. Specifically, FA may be a direct precursor (similar genetic mutations may be seen, although lower frequency) since the histology is identical except for invasion, and patients with FC are about a decade older than patients with adenoma.
A malignant epithelial neoplasm with follicular cell differentiation, invasive growth, and lacking the nuclear features of papillary carcinoma
Up to 10% of thyroid malignancies
Increased in iodine-deficient areas and in patients with pre-existing thyroid disease or syndrome association (PTEN hamartoma tumor syndrome, Carney)
Recurrent laryngeal nerve damage and hypoparathyroidism
Excellent long-term outcome (~90% 20-year survival depending on type)
Females > males (2 : 1)
Usually in the 5th-6th decades
Oncocytic tumors occur in patients about a decade older
Usually an asymptomatic, palpable mass
Rarely dysphagia or hoarseness
Ultrasound shows a solid or cystic mass, a capsule, and is used to guide fine needle aspiration
Computed tomography is useful to determine extent of the mass and lymph node disease
Nuclear scintigraphy rarely used
Excellent long-term prognosis (~90% 20-year survival)
Surgery (lobectomy or thyroidectomy) with radioactive iodine
Up to 10% of thyroid carcinomas are FCs, reflecting a downward trend as the recognition of the follicular variant of papillary carcinoma has increased. FC is more common in women than men (about 2 : 1), with a peak incidence in the 5th and 6th decades, although recently the sex difference is not as distinct. The oncocytic type tends to occur in patients about a decade older. Patients usually present with an asymptomatic solitary, painless thyroid mass, which is usually solid on radiographic imaging. Hoarseness, dysphagia, dyspnea, and stridor are rare. FC tends to be larger than papillary carcinoma. Thyroid function tests are almost always normal. Lymph node metastasis is uncommon, although slightly more common in the oncocytic variant, as hematogenous spread is more common than lymphatic spread. Distant metastasis is seen in up to 20% of patients (lung and bone). Imaging cannot reliably distinguish between benign and malignant lesions. Iodinated contrast is to be avoided as it delays 131 I therapy. Ultrasound may demonstrate a solid versus cystic lesion, and show a nonechogenic halo (capsule). Turbulent intratumoral blood flow is seen more often in carcinoma.
Solitary, encapsulated mass
Invasion usually difficult to see on gross examination
Usually < 5 cm
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here