Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgments: The authors would like to acknowledge Marybeth Ezaki, MD, and Scott Kozin, MD, for providing additional radiographs and photos that have enhanced our chapter.
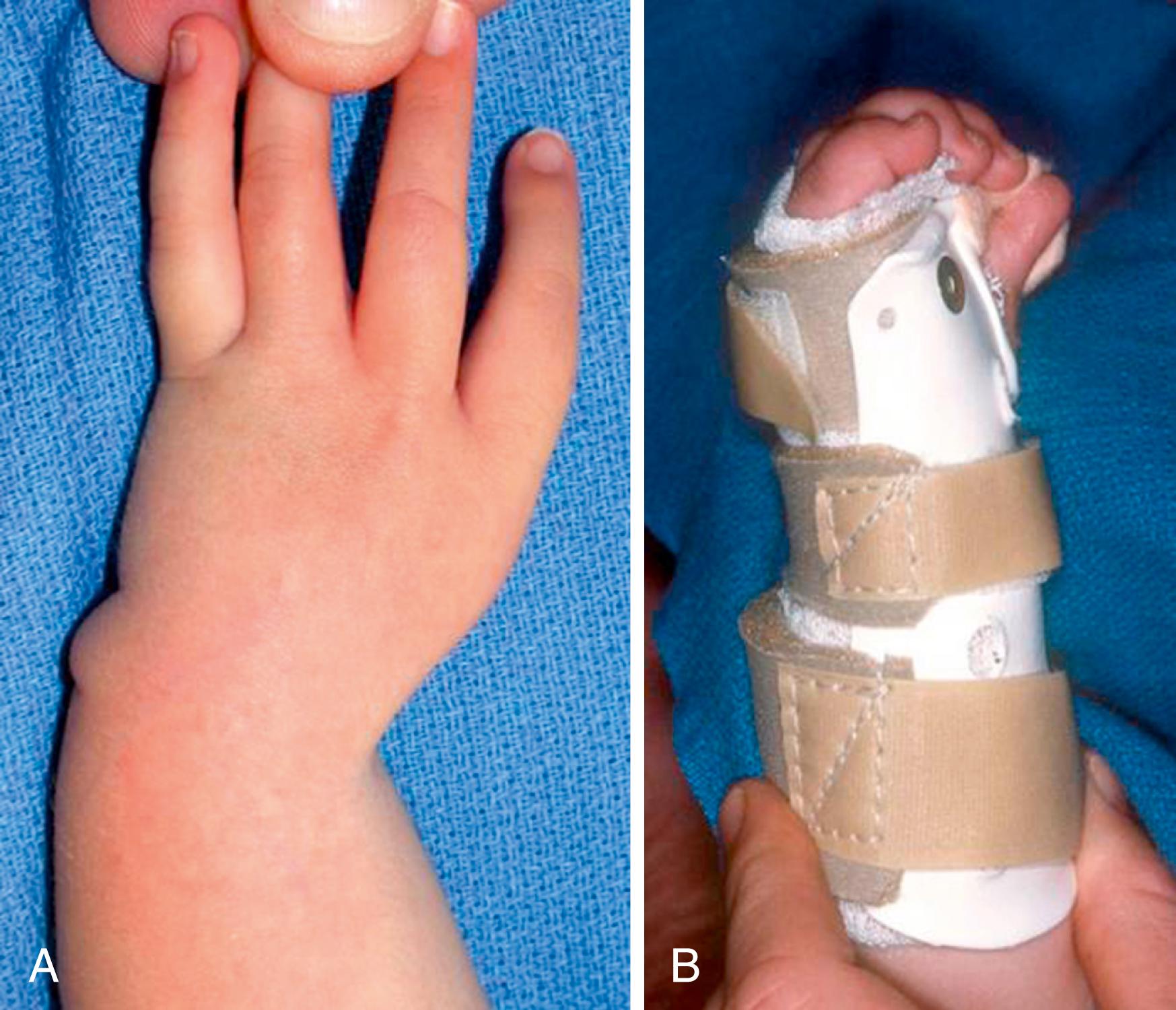
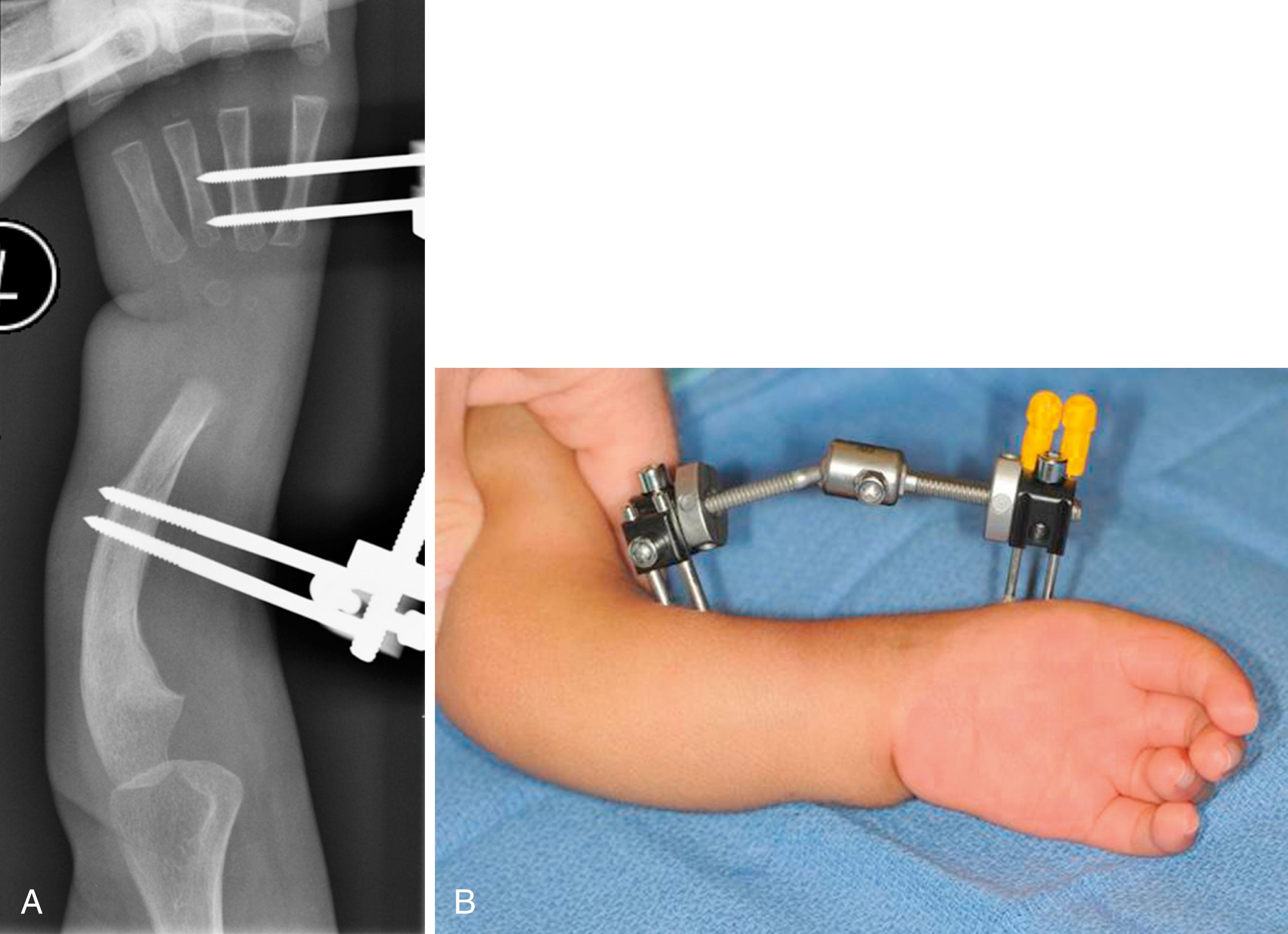
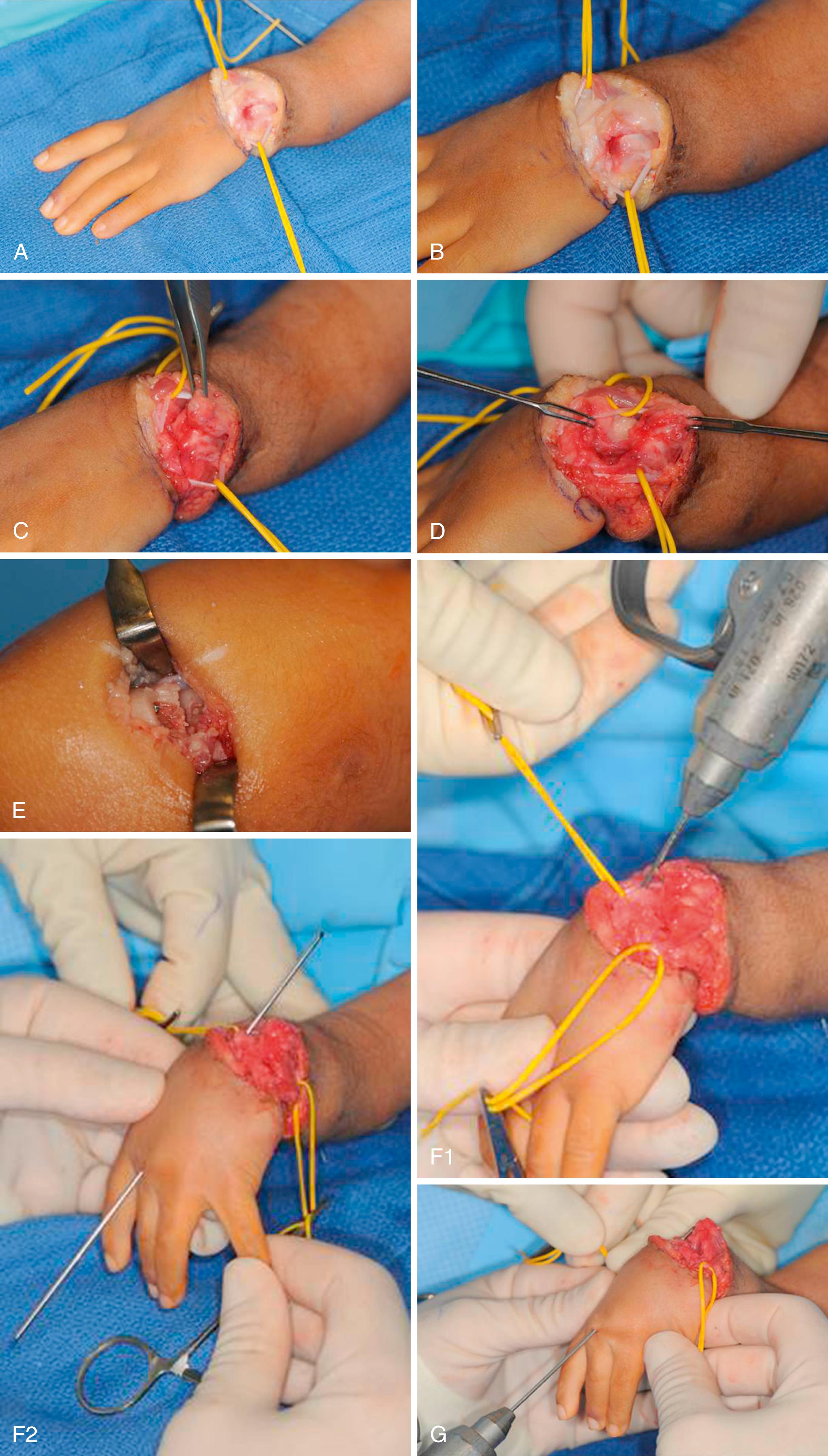
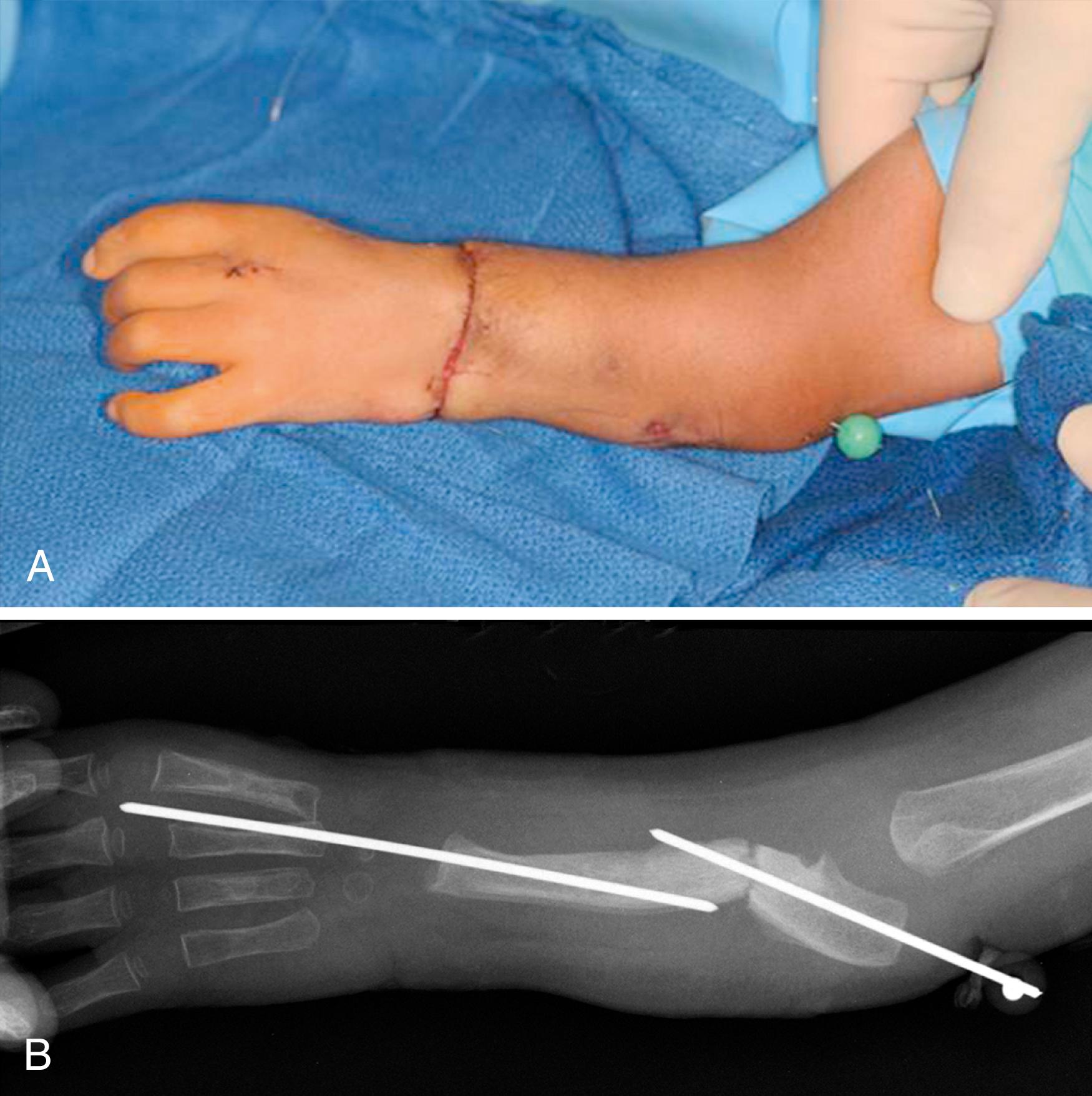
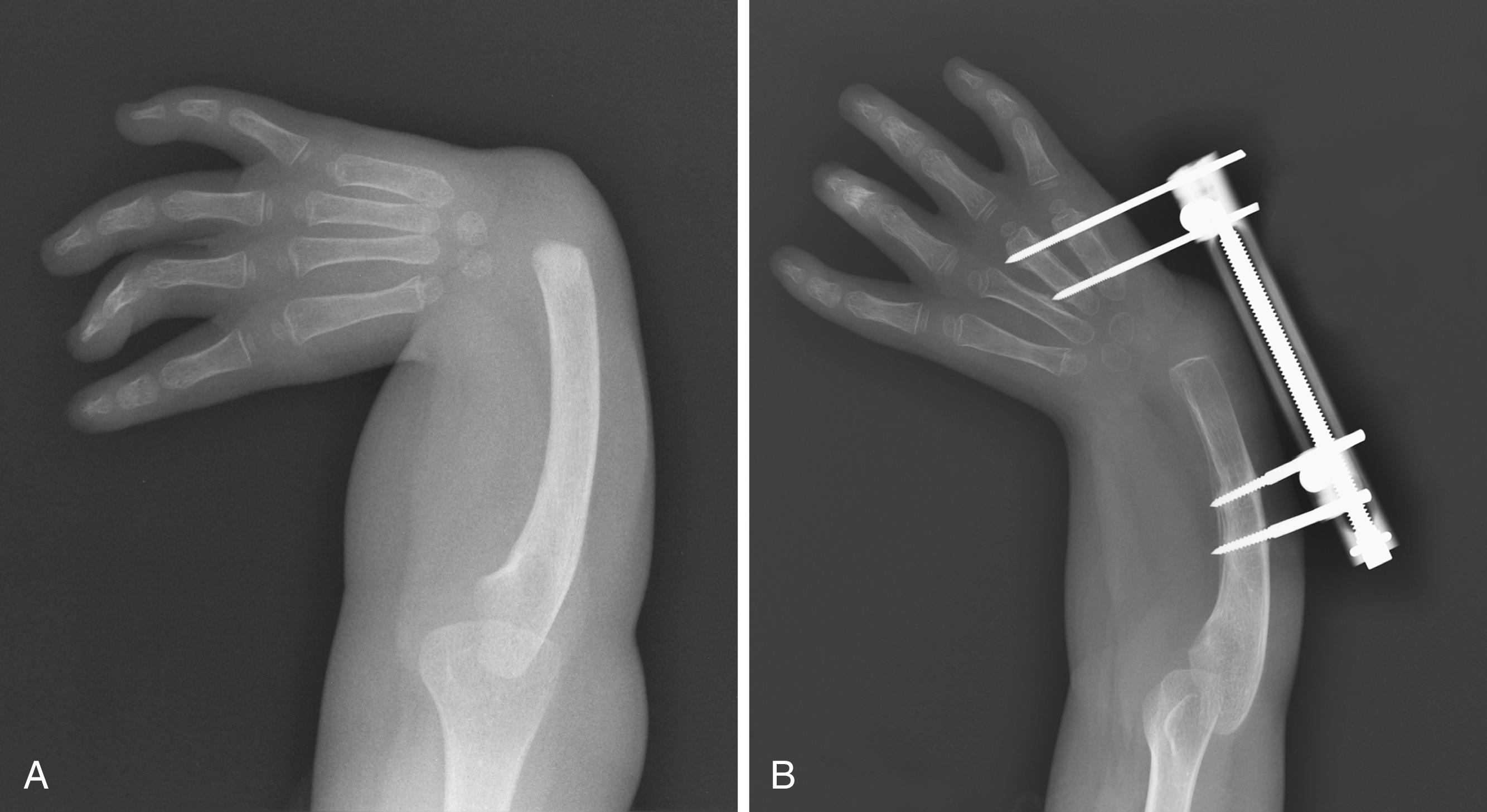
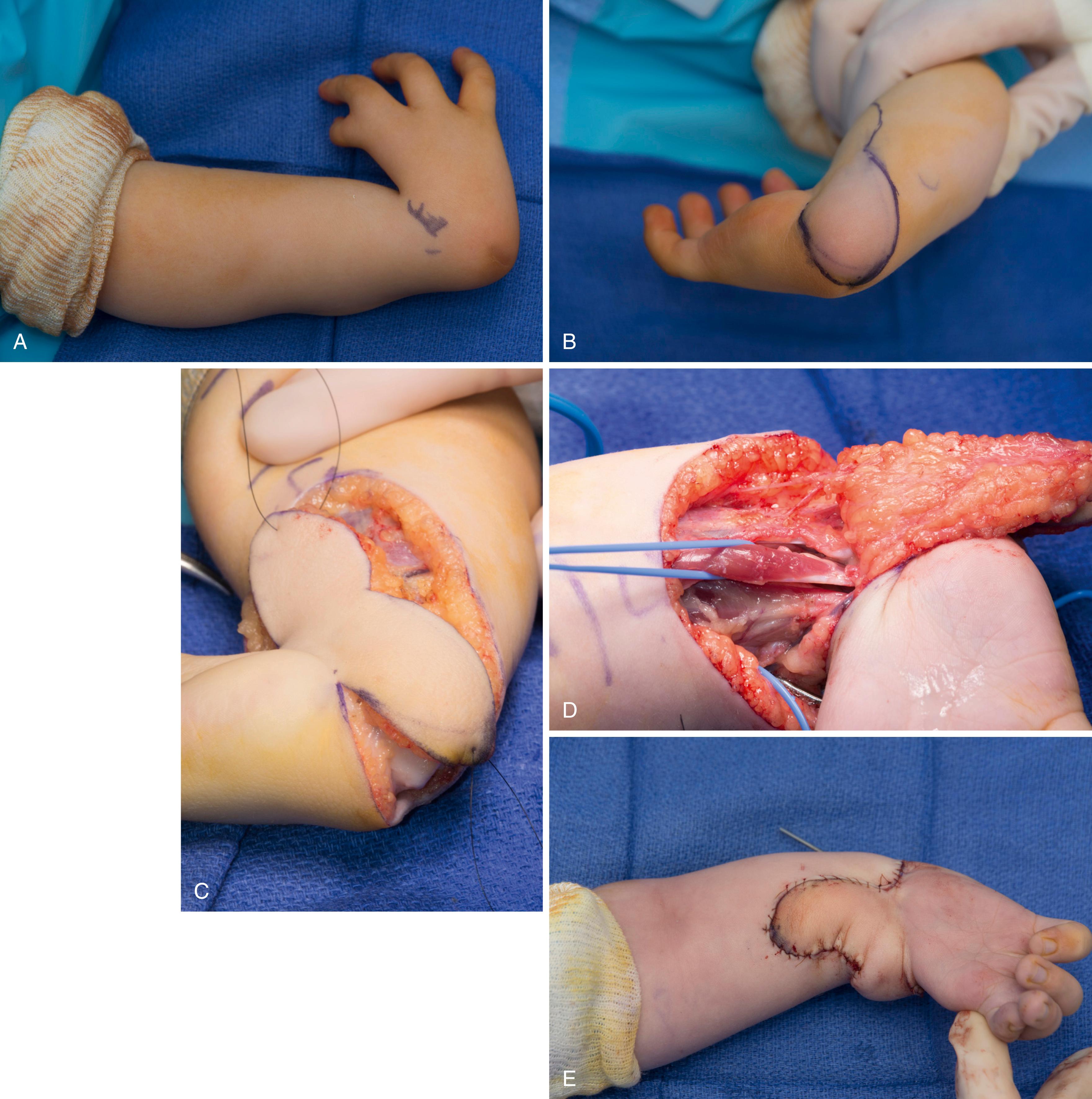
A boy with left type 4 radial deficiency was initially seen at 2 months of age. Stretching and splinting were instituted when he was 1½ years old ( eFig. 38.1 ), and radiographs were taken at that time ( eFig. 38.2 ). Treatment began with preliminary distraction ( eFig. 38.3 ). Next, centralization was performed ( eFig. 38.4 ). The final result is shown in eFig. 38.5 . Pollicization was then performed ( eFig. 38.6 ). The 2-year outcome is shown in eFig. 38.7 .



Radial longitudinal deficiency (RLD) is a spectrum of malformations affecting the structures of the radial side of the forearm (radius, radial carpus, and thumb), including hypoplasia of the bones and joints, muscles and tendons, ligaments, nerves, and blood vessels. In the Oberg, Manske, Tonkin classification of congenital hand differences, RLD is categorized as a malformation of the radial-ulnar axis. RLD is an uncommon condition, although it is the most common type of congenital longitudinal deficiency. A population-based study in Finland found RLD in nearly 1:5000 live births.
Children with RLD should undergo thorough and serial examinations of both upper extremities. RLD is frequently bilateral and asymmetric, and manifestations may be subtle. Because the radius and many organ systems develop at the same time, a systemic workup is also required. RLD is commonly associated with several congenital syndromes, such that only a third of patients with RLD present with an isolated upper extremity malformation ( Table 38.1 ). Therefore, a complete physical examination must be performed, and consultation with a clinical geneticist is recommended. In addition, radiographic and serologic tests are required as described below.
| Syndrome | Other Anomalies | Inheritance |
|---|---|---|
| VACTERL | Spinal, renal, gastrointestinal, cardiac | Sporadic |
| Holt-Oram | Cardiac (septal defects); other upper extremity malformations | Autosomal dominant |
| TAR | Thrombocytopenia, anemia; radius absent but thumb present | Autosomal recessive |
| Fanconi anemia | Pancytopenia | Autosomal recessive |
| Chromosome aberrations (trisomies 13 and 18) | Multiple | Sporadic |
| Nager, Rothmund-Thomson, IVIC | Craniofacial | Varies with the syndrome |
Although children with bilateral and severe RLD have functional impairment as a result of thumb dysfunction, wrist instability, and short upper extremities, there is no difference in long-term activity and participation levels between those with mild versus severe RLD. For some children with RLD, independent performance of activities of daily living, such as fastening buttons and zippers or accomplishing personal hygiene, may be difficult, prompting consideration for surgery.
Radiographs tend show the degree of involvement of the radius, thumb, and carpus dependent on the degree of ossification and/or previous surgical intervention. Classification of the RLD is based on radiographic studies. Spine x-rays, renal ultrasound, and echocardiography are required to assess for associated anomalies.
Persons with RLD have a high incidence of medical and musculoskeletal anomalies, which escalate with increasing severity of the deficiency. In addition to genetic counseling, testing for Fanconi anemia is recommended. Although there are several known genes responsible for Fanconi anemia, the gold standard for testing remains the chemical chromosomal breakage test. We recommend testing for Fanconi anemia for all children with deficiencies of the thumb and radial border of the forearm. Additional findings, such as abnormal skin pigmentation (café-au-lait spots) , kidney abnormalities, growth retardation, and microcephaly, add to the suspicion of Fanconi anemia. Failure to ascertain the diagnosis of Fanconi anemia will have lifelong ramifications for the child, family, and physician. Early testing allows Fanconi anemia to be diagnosed before the onset of bone marrow failure. Timely diagnosis allows for years of preparation to search for an appropriate bone marrow match that may prevent the child from dying from aplastic anemia. Innovative techniques, such as preimplantation genetic determination, allow the parents to have another child with matching blood characteristics and without Fanconi anemia. At birth, the cord blood can be harvested and used as a donor for the affected Fanconi anemia child. When hand surgeons and pediatricians fail to consider the diagnosis of Fanconi anemia in children with RLD, the child and the family are left to suffer the consequences of a painful terminal illness that could otherwise have been treated. For this reason, the association of Fanconi anemia and RLD is often tested on orthopedic in-training and board examinations.
RLD is associated with other upper extremity anomalies, including humeral hypoplasia, proximal radioulnar synostosis, congenital radial head dislocation, and finger stiffness. Less common associations include metacarpal synostoses and syndactyly. Infrequent findings are contralateral radial polydactyly and phocomelia.
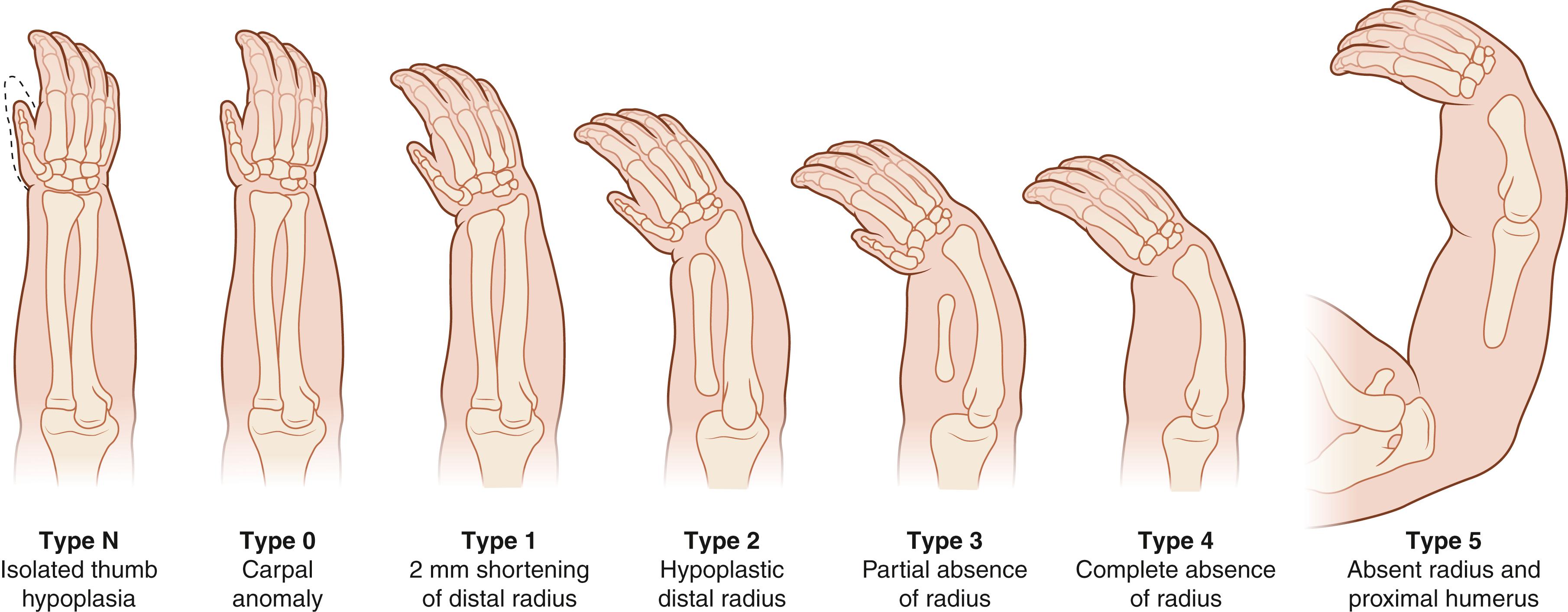
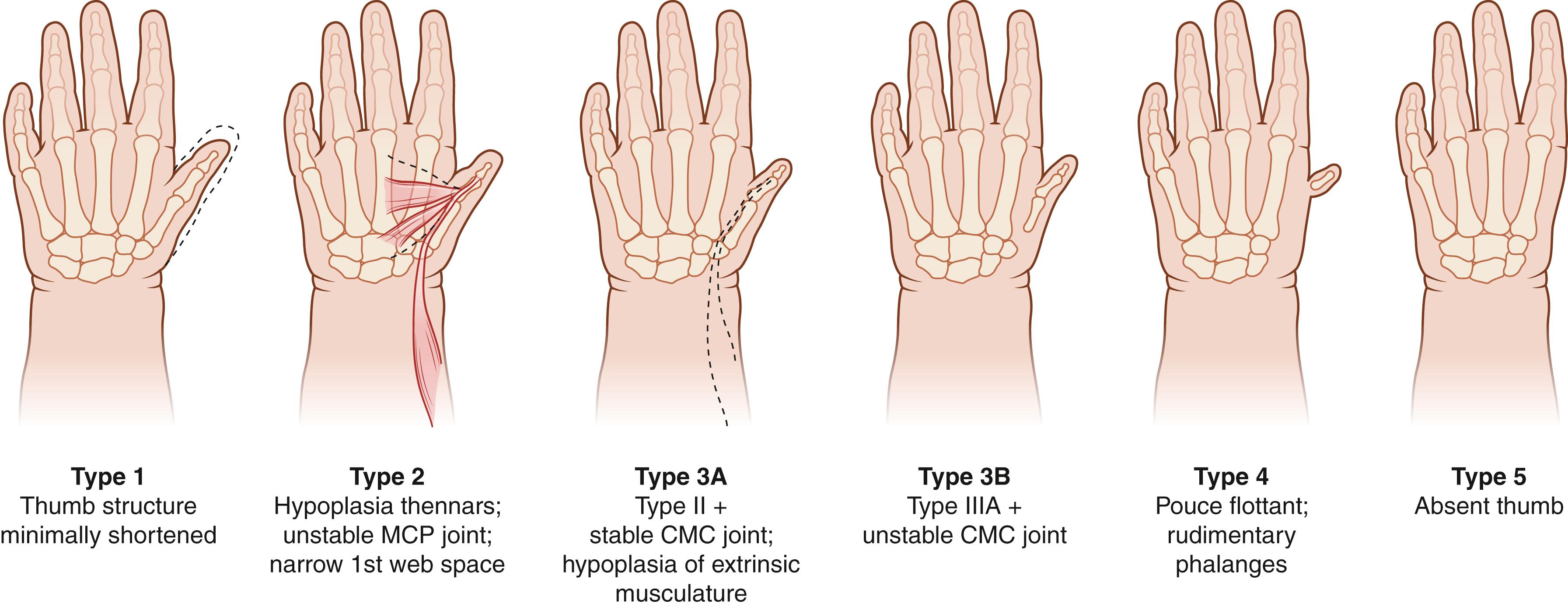
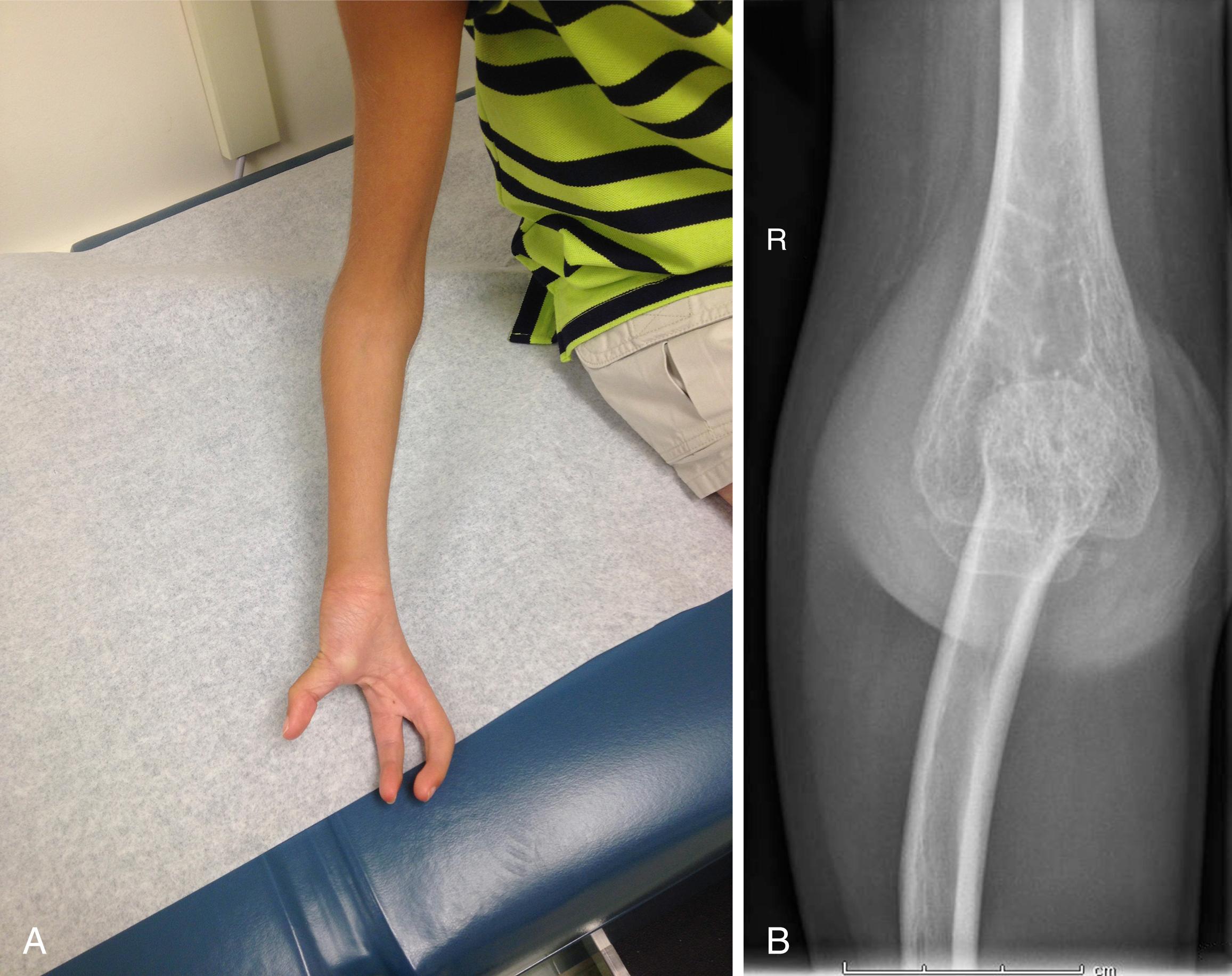
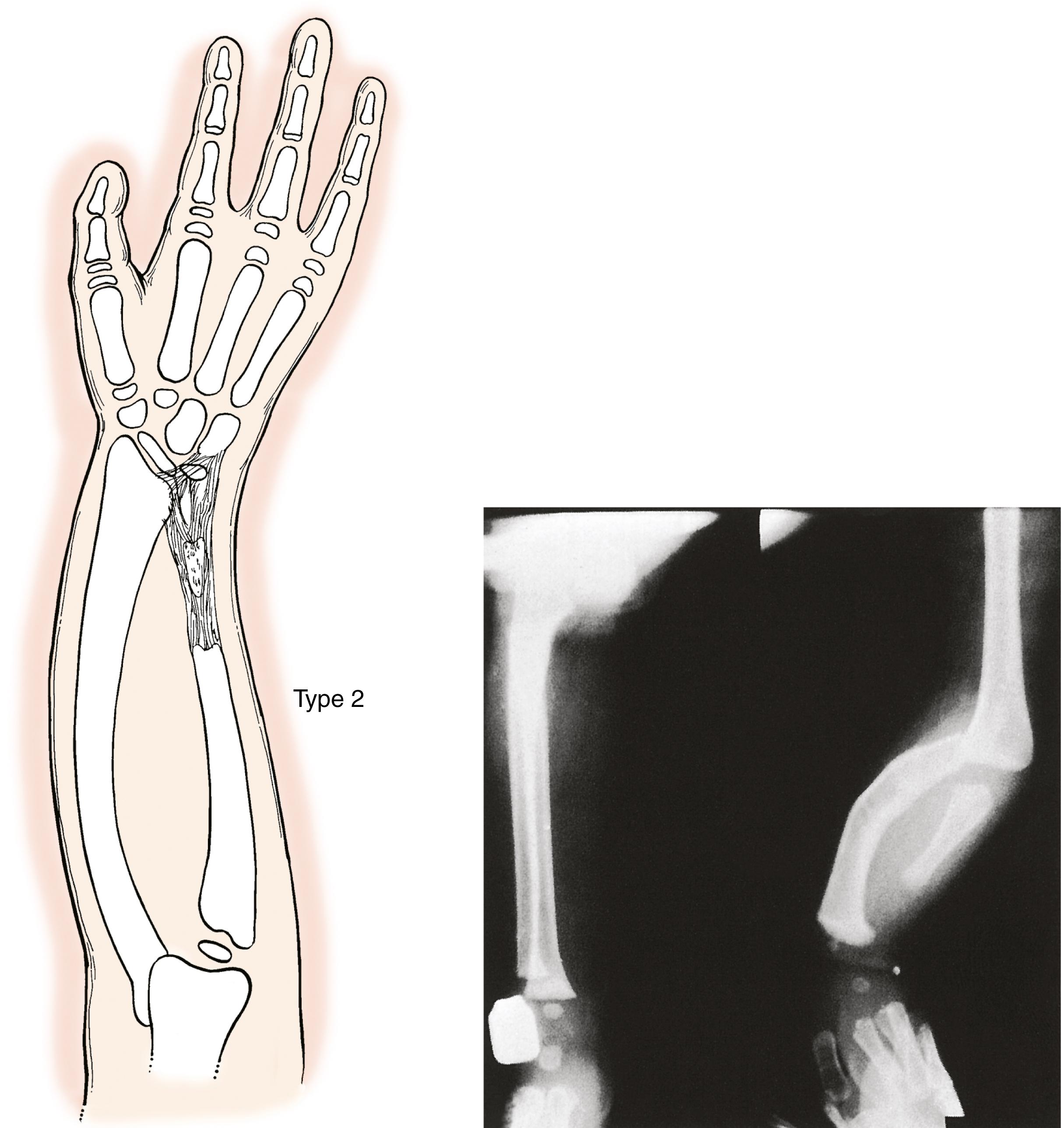
Bayne and Klug classified RLD into four types based on the radiographic severity of the radial deficiency ( Table 38.2 ). James and associates modified this classification to include patients with deficiency of the thumb or carpus in the presence of a radius of normal length ( Fig. 38.1 ). This classification is used in combination with the modified Blauth scheme for classifying thumb hypoplasia ( Fig. 38.2 ).
| Type | Thumb | Carpus | Distal Radius | Proximal Radius |
|---|---|---|---|---|
| N | Hypoplastic or absent | Normal | Normal | Normal |
| 0 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Normal | Normal, radioulnar synostosis, or congenital dislocation of the radial head |
| 1 | Hypoplastic or absent | Absence, hypoplasia, or coalition | >2 mm shorter than the ulna | Normal, radioulnar synostosis, or congenital dislocation of the radial head |
| 2 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Hypoplasia | Hypoplasia |
| 3 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Physis absent | Variable hypoplasia |
| 4 | Hypoplastic or absent | Absence, hypoplasia, or coalition | Absent | Absent |
Indications for treatment vary with the severity of the deformity and the age of the patient. Children with type 0 or 1 or mild type 2 radial deficiencies may require only stretching and splinting. When considerable radial deviation is present, tendon transfers and soft tissue releases may be indicated. Severe type 2 radial deficiency is difficult to treat. Lengthening of the radius may be possible, or centralization of the carpus on the end of the ulna may be performed to achieve stability and correct the radial deviation. A well-aligned forearm improves the likelihood that the child will use a reconstructed thumb.
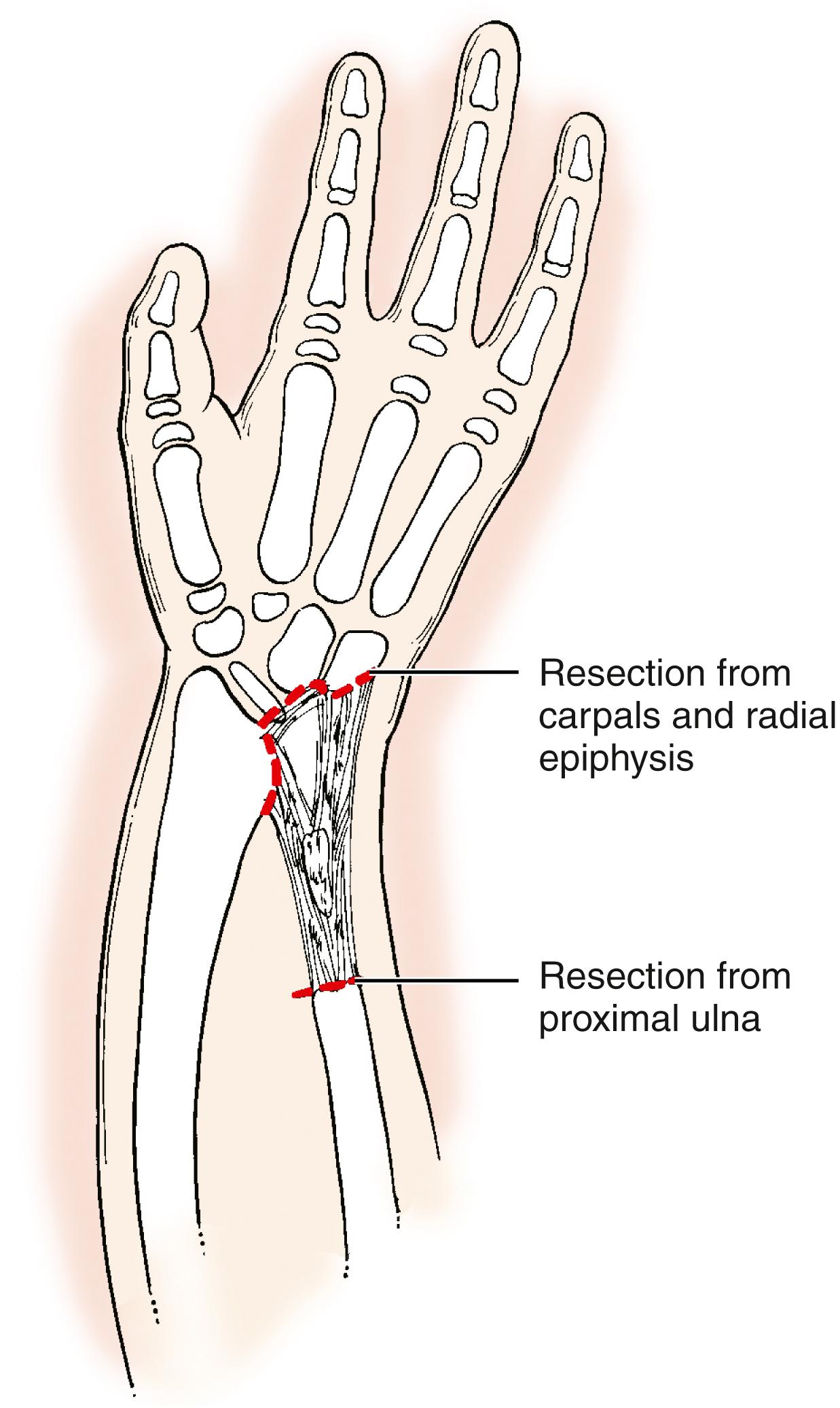
We have previously recommended bony centralization, including (if necessary) carpal resection and ulnar epiphyseal shaving, to correct the wrist instability and radial deviation in types 3 and 4 RLD. Although bony centralization is still performed by some surgeons, others prefer not to resect the carpus or shave the distal ulna because of the high rate of recurrent deformity and complications such as wrist stiffness and forearm growth impairment secondary to iatrogenic damage to the ulnar physis.
The best results of centralization are obtained when aberrant radial wrist extensors can be transferred to help maintain the new position and when the centralization is done before 1 year of age (as long as general anesthesia is not precluded by other manifestations of the child’s syndrome such as cardiac problems or thrombocytopenia). Before centralization, serial casting and/or application of a distraction device facilitates stretching of the taut radial soft tissue structures. This preliminary stretching diminishes the soft tissue tension and the likelihood that bony resection will be required during centralization. , Preliminary external distraction is most helpful for older children with untreated type 3 or 4 radial deficiency. A bilobed skin flap or dorsal rotation flap may redistribute excess tissue from the ulnar to the radial side of the wrist. ,
With unilateral type 3 or 4 involvement, the affected forearm is usually only half as long as the unaffected forearm. This deficit in length has been surgically addressed by ulnar lengthening via distraction osteogenesis. Lengthening can be performed in older children after centralization. However, lengthening procedures may deter the growth of the ulna, such that repeated lengthenings will be required to maintain the relative gain in length.
Vilkki described the combination of soft tissue distraction and microvascular epiphyseal transfer for the treatment of type 4 radial deficiency ( Fig. 38.3 ). Historically, attempts to treat radial deficiency by surgical transfer of nonvascularized growing bone were unsuccessful because the graft failed to grow. Although Vilkki’s early and midterm results are promising, the technique is technically demanding and the outcome at skeletal maturity is unknown.
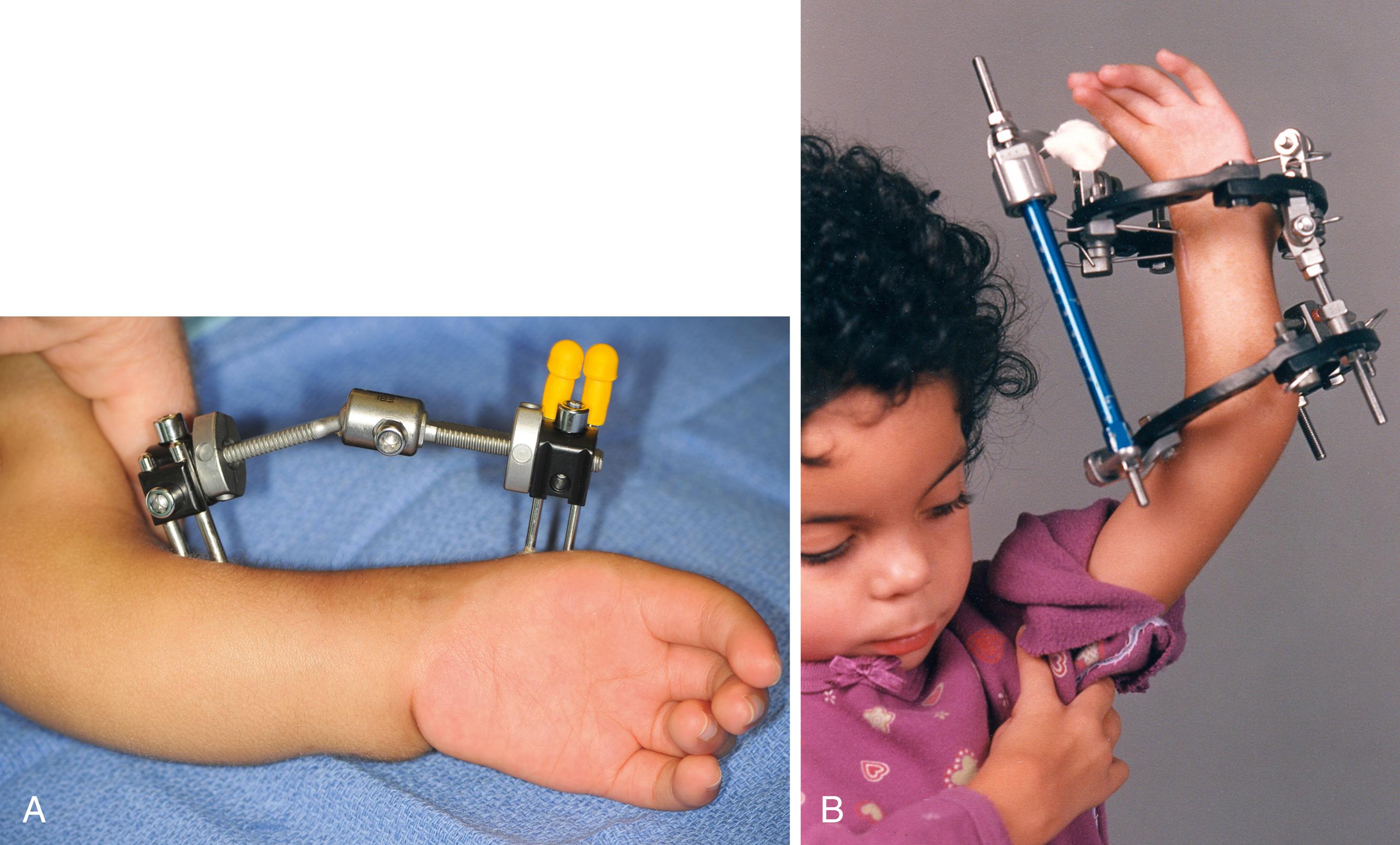
Unilateral and circumferential fixators have been used successfully to distract the radial soft tissues before centralization ( Fig. 38.4 ). , The fixator is applied across the wrist via an open technique for pin placement to protect the anomalous anatomy and gradually distracted until the wrist can be centralized without residual radial deviation after the external fixator is loosened or removed ( Fig. 38.5 ).
Although the wrist and forearm are profoundly abnormal in a radially deficient limb, the anomalies are predictable. All the radial forearm structures are deficient to varying degrees. The radial wrist extensors and extrinsic thumb motors are usually absent or aberrant. The radial nerve is generally absent below the elbow. The median nerve is always present and is frequently the most prominent structure on the radial side of the wrist. The radial artery is usually absent. Occasionally, a child with RLD has an elbow extension contracture. In this case centralization is contraindicated, as wrist radial deviation is needed for the child’s hand to reach the face.
The incision for centralization begins at the level of the distal end of the ulna just radial to the midline, extends toward the ulna in a transverse direction, and then forms an ellipse to excise excess skin and subcutaneous tissue. Alternately, excess tissue from the ulnar aspect of the wrist is rotated to the radial side. The dorsoulnar sensory nerve is preserved, and the extensor retinaculum is exposed. The extensor carpi ulnaris is isolated at its insertion into the base of the fifth metacarpal. The extensor retinaculum is raised as a radially based flap and the finger extensor tendons are retracted radially. The radial wrist extensors are generally absent or adherent to the dorsal capsule and devoid of proximal musculature. Their remnants are isolated and elevated with a piece of dorsal capsule.
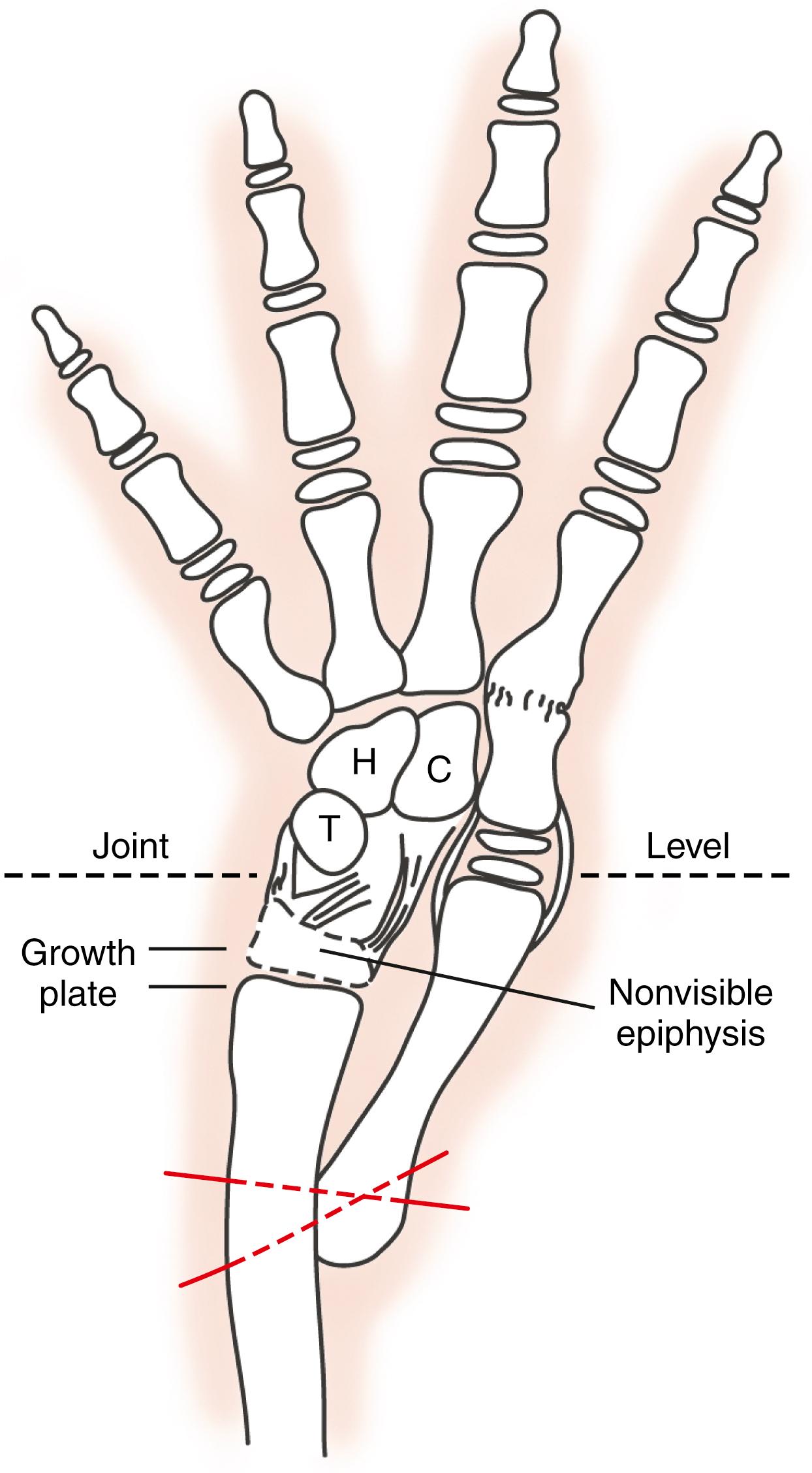
The wrist capsule is incised in a transverse direction over the ulnocarpal joint to expose the distal end of the ulna ( Fig. 38.6 ). The carpal bones are often palmar and radial to the distal ulna. The ulna is freed from its soft tissue attachments distal to the physis, and the carpal bones are detached from the palmar capsule. The carpus is then reduced onto the distal ulna. If reduction cannot be achieved, the radial structures are examined for any persistent taut tissue. In severe cases without preliminary distraction, adequate reduction cannot be achieved and alternative measures are necessary. Surgical options include carpectomy or limited shaving of the distal ulnar epiphysis while avoiding injury to the growth plate or the application of an external fixator, postoperative distraction, and delayed formal centralization.
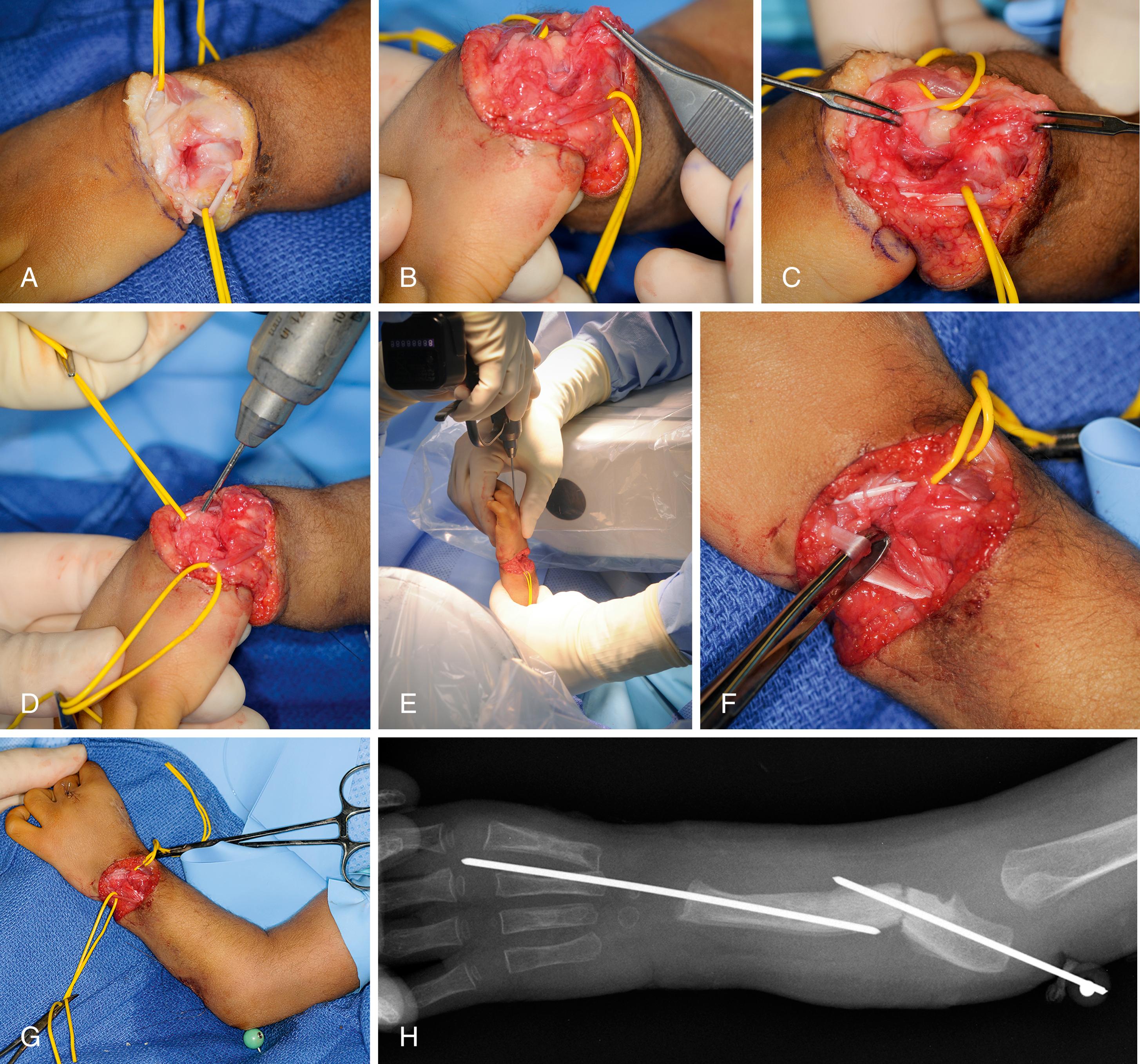
The reduction is maintained by placing a Kirschner wire through the carpus and third metacarpal into the ulnar shaft. If the ulnar angulation is greater than 30 degrees, a closing wedge osteotomy is performed at the apex of the deformity and secured with the same Kirschner wire. In severe deformity, separate Kirschner wires are often necessary. The wrist capsule is imbricated, and, if present, the radial wrist extensors are transferred into the extensor carpi ulnaris tendon. The extensor carpi ulnaris is tightened by detaching and advancing the tendon or imbrication to increase soft tissue tension on the ulnar side. The retinacular flap is passed underneath the finger extensors to reinforce the wrist capsule. Excess skin and subcutaneous tissue are excised, and the wound is closed with absorbable suture. A long-arm bulky compressive dressing is applied and covered with a long-arm fiberglass splint or cast.
The complications of formal centralizations, particularly when the carpus cannot be passively reduced onto the end of the ulna, have shifted many surgeons toward performing a soft tissue release and balancing procedure instead of a formal centralization ( Fig. 38.7 ). The major difference between these two operations is that in the soft tissue rebalancing, the joint capsule is not opened. Carpectomy and shaving of the distal ulnar epiphysis are also not performed. Tendon releases and transfers are performed in the same manner as for a formal centralization, and the hand and carpus are then pinned in the best position possible, accepting some translocation and/or deviation.
This procedure is rarely indicated. When lengthening is performed, the principles of distraction lengthening are followed. A uniplane or multiplane fixator is used, depending on any concomitant angular bony correction needed. For application of a circumferential frame, two half-pins and one transfixion wire are used proximal to the osteotomy. One half-pin and two transfixion wires (one in the ulna and one in the metacarpals) are placed distal to the osteotomy. For a uniplane fixator, two pins each are placed proximal and distal to the osteotomy. We prefer a uniplane fixator with a hinge at the midpoint to allow correction of the radial bow at the time of fixator application. Any residual radial deviation is corrected at the time of fixator application or during the distraction. Acute bony correction can be achieved with a closing wedge osteotomy followed by distraction osteogenesis. Distraction is initiated approximately 1 week after application of the fixator and is continued at 1 mm/day divided into two to three increments. Radiographic progress of bone regeneration is monitored weekly. The rate of lengthening is slowed if regeneration is lagging. The child and family are taught lengthening techniques and exercises to maintain elbow and digit motion. The ulna can usually be lengthened by 30% to 50%. The fixator is maintained during consolidation of the bony regenerate, which generally takes twice as long as the lengthening phase. The fixator is not removed until a total of three cortices are visualized on the anteroposterior and lateral x-rays. Occasionally, supplemental bone grafting is necessary to augment union.
Range-of-motion exercises for soft tissue stretching are started shortly after birth. The parents are instructed in stretching exercises to be performed with each diaper change or feeding. Once the child’s arm is large enough for splinting, generally around 3 months of age, a custom-fabricated long-arm Orthoplast splint (North Coast Medical, Gilroy, CA) is made for nighttime use in addition to the daytime stretches ( Fig. 38.8 ). The parents are instructed to continue stretching the wrist several times each day for at least the child’s first year. In certain children, neither pollicization nor centralization is indicated ( ![]() ). These children typically have a mobile and dexterous small finger along with a stiff index finger. Pinch and grasp are accomplished using the ulnar side of the hand (ulnar prehension), and straightening the wrist would put the ulnar digits in an unfavorable position for approaching and interacting with objects. This shift in position may be detrimental to the child’s overall function and independence.
). These children typically have a mobile and dexterous small finger along with a stiff index finger. Pinch and grasp are accomplished using the ulnar side of the hand (ulnar prehension), and straightening the wrist would put the ulnar digits in an unfavorable position for approaching and interacting with objects. This shift in position may be detrimental to the child’s overall function and independence.

Soft-tissue balancing and formal centralization have overlapping indications, and to date neither has proven superior in long-term function or esthetics. If the child is a candidate for centralization and is safe to undergo general anesthesia around age 1 year, surgical correction is planned. If the wrist can be passively reduced prior to surgery, formal centralization is performed. If not reducible, the parents are offered a choice between a soft tissue release and balancing procedure versus preliminary distraction followed by centralization. In the case of formal centralization, prolonged pin fixation followed by long-term splinting is necessary to minimize recurrence. Ulnar lengthening is reserved for mature older children or teenagers. Lengthening requires realistic expectations and emotional stamina on the part of the patient and family. Preoperative counseling and psychological assessment are helpful. The support of a limb-lengthening team, including a nurse, social worker, and occupational therapist, is also essential.
The basic goals of treatment are to (1) correct the radial deviation of the wrist, (2) balance the wrist on the forearm, (3) maintain wrist and finger motion, (4) promote growth of the forearm, (5) reconstruct the thumb deficiency, and (6) improve the function of the extremity.
Passive stretching and splinting of the taut radial structures are initiated during infancy.
Centralization and/or soft tissue release combined with tendon transfer is indicated in children with radial wrist deviation and insufficient support of the carpus.
Thumb hypoplasia is addressed at a second stage after wrist centralization.
The incision for centralization is planned to allow excision or rotation of the excessive ulnar tissue.
The extensor carpi ulnaris is tightened and the extensor retinaculum is preserved.
After releasing the taut structures, the carpus is pinned to the end of the distal ulna, avoiding removal of the carpal bones or shaving of the ulnar epiphysis.
If the surgeon elects to remove carpal bones or shave the ulnar epiphysis, great care must be taken to avoid damaging the ulnar physis.
Despite numerous technical modifications to preserve alignment, some recurrence of the radial deficiency is universal. Currently, long-term maintenance of the carpus on the end of the ulna without sacrificing wrist mobility or stunting forearm growth remains a daunting task.
In the treatment of RLD, the surgeon and family must choose between a wrist that is flexible and deviated or a wrist that is stiff and straight. Long-term follow-up studies of bony centralization report problems with recurrence and stiffness, as well as significantly worse ulnar growth than would be expected from natural history ( Fig. 38.9 ). , Despite these difficulties, Kotwal and colleagues did report that patients with RLD who underwent centralization showed improvements in both subjective measurements (such as appearance) and objective measurements (such as alignment, grip strength, and finger and wrist range of motion) compared with patients who did not undergo surgery.
The numerous long-term complications of centralization have resulted in some experienced pediatric hand surgeons abandoning formal centralization in favor of soft tissue reconstruction, such as a bilobed skin flap combined with musculotendinous releases and tendon transfers. , The soft tissue reconstruction has been shown to not limit ulnar growth.
After soft tissue balancing, the extremity is placed in a cast for at least 8 weeks. Subsequently, a long-arm splint, custom-fabricated to maintain the wrist position, is worn full time for 3 to 6 months and then at night until skeletal maturity is reached.
Complications of ulnar lengthening are common, especially pin tract infections, which usually resolve with local care and antibiotics. Finger stiffness may occur during the lengthening process and is treated by slowing the distraction rate and therapy. A second procedure to place bone graft at the osteotomy site is occasionally necessary to achieve union.
Ulnar deficiency occurs approximately once in 25,000 live births and is 4 to 10 times less common than radial deficiency. Ulnar deficiency occurs sporadically and is not associated with systemic conditions as occurs in children with radial deficiency. Ulnar deficiency is associated with other musculoskeletal abnormalities that warrant careful physical examination supplemented by radiographs.
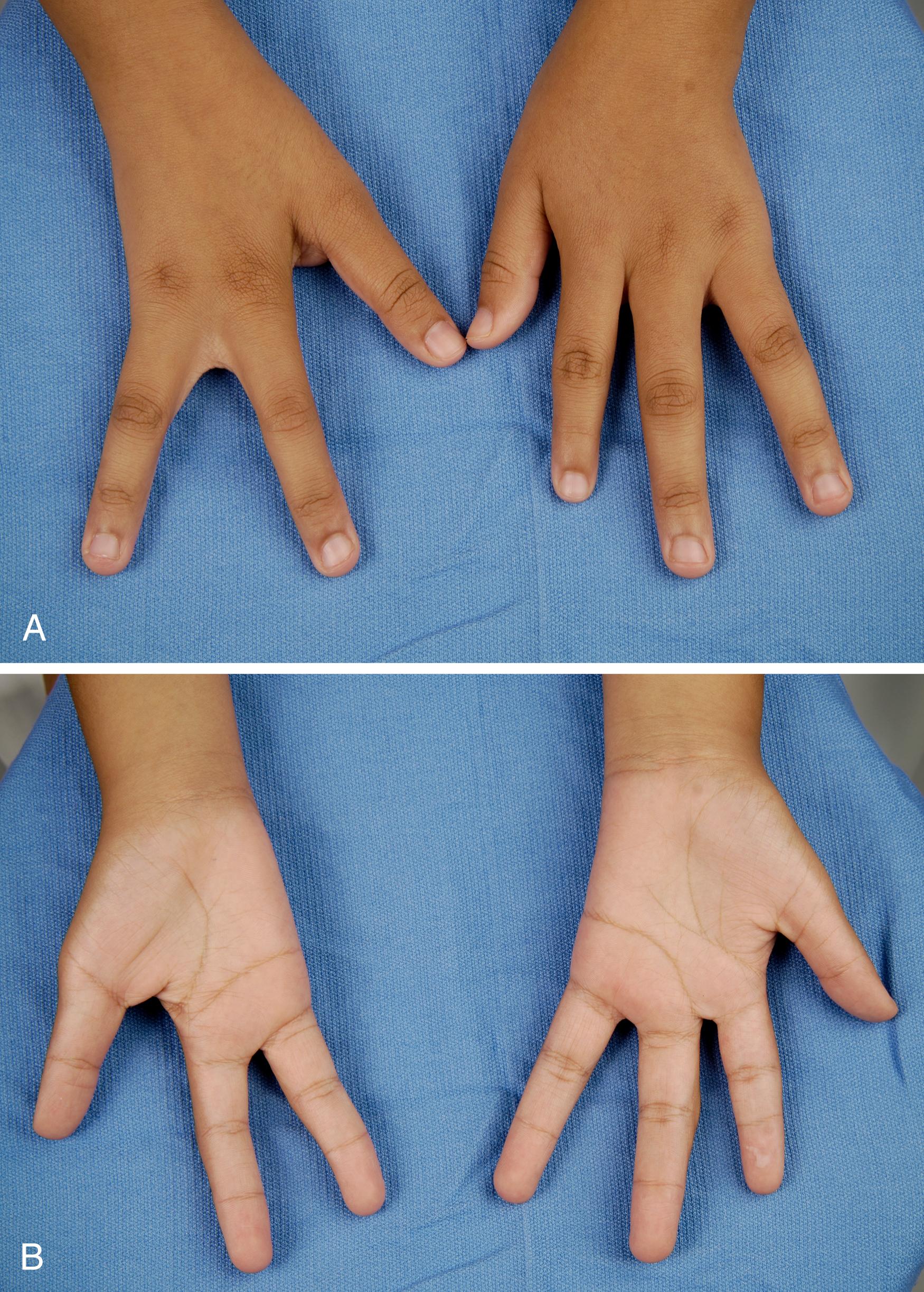
Unilateral ulnar deficiency is more common than bilateral deficiency. Children with ulnar deficiency have hypoplasia of the entire upper extremity. The elbow is malformed or fused (i.e., radiohumeral synostosis) in the majority of cases ( Fig. 38.10 ). The ulna may be partially or completely absent, and a cartilaginous ulnar “anlage” may be present. The hand and carpus are always affected, and occasionally isolated hand involvement is seen. About 90% of hands are missing digits, 30% have syndactyly, and 70% have thumb abnormalities ( Fig. 38.11 ). ,
The other musculoskeletal anomalies that may accompany ulnar deficiency include proximal femoral focal deficiency, fibular deficiency, phocomelia, and congenital scoliosis. Radiographs should be taken of both upper extremities, both lower extremities, and the spine. Ulnar deficiency is rarely associated with anomalies of other organ systems.
Most classification systems are based on elbow and forearm anomalies ( Table 38.3 ). , To supplement these systems, Cole and Manske described a classification system based on thumb and first web anomalies ( Table 38.4 ). Havenhill and colleagues included ulnar hand and carpal deficiencies without forearm or elbow involvement.
| Characteristics | Kummel (1895) | Ogden et al. (1976) | Riordan (1986) | Bayne (Dobyns, 1993) | Swanson et al. (1984) | Miller et al. (1986) |
|---|---|---|---|---|---|---|
| Elbow | ||||||
| Normal/near-normal humeroradial joint | I | |||||
| Humeroradial synostosis | II | III | IV | III | D | |
| Radial head dislocation | III | A, B a | ||||
| Ulnar Length | ||||||
| Normal-length ulna | ||||||
| Ulnar hypoplasia | I | I | I | |||
| Partial ulnar aplasia | II | II | II | |||
| Complete ulnar aplasia | III | I | III | II | ||
| Other Upper Extremity Characteristics | ||||||
| Congenital wrist amputation | IV | |||||
| Internal rotation deformity below the shoulder | C b | |||||
a B, radial head dislocation with complete absence of the ulna and cubital webbing.
b Humeroradial synostosis with variable absence of the ulna and associated internal rotation deformity.
| Type | Characteristics |
|---|---|
| A | Normal first web space and thumb |
| B | Mild first web and thumb deficiency |
| C | Moderate to severe first web and thumb deficiency; possible loss of opposition; malrotation of the thumb into the plane of the fingers; thumb/index finger syndactyly; absent extrinsic tendon function |
| D | Absent thumb |
Surgery for patients with ulnar deficiency is mainly focused on the associated hand differences. Surgical indications for many of the hand anomalies associated with ulnar deficiency are well established. Hand function is improved by release of the syndactyly and reconstruction of the thumb and first web deficiencies. Procedures that may be indicated include deepening of the first web space, opponensplasty, rotational osteotomy of the thumb metacarpal, and pollicization.
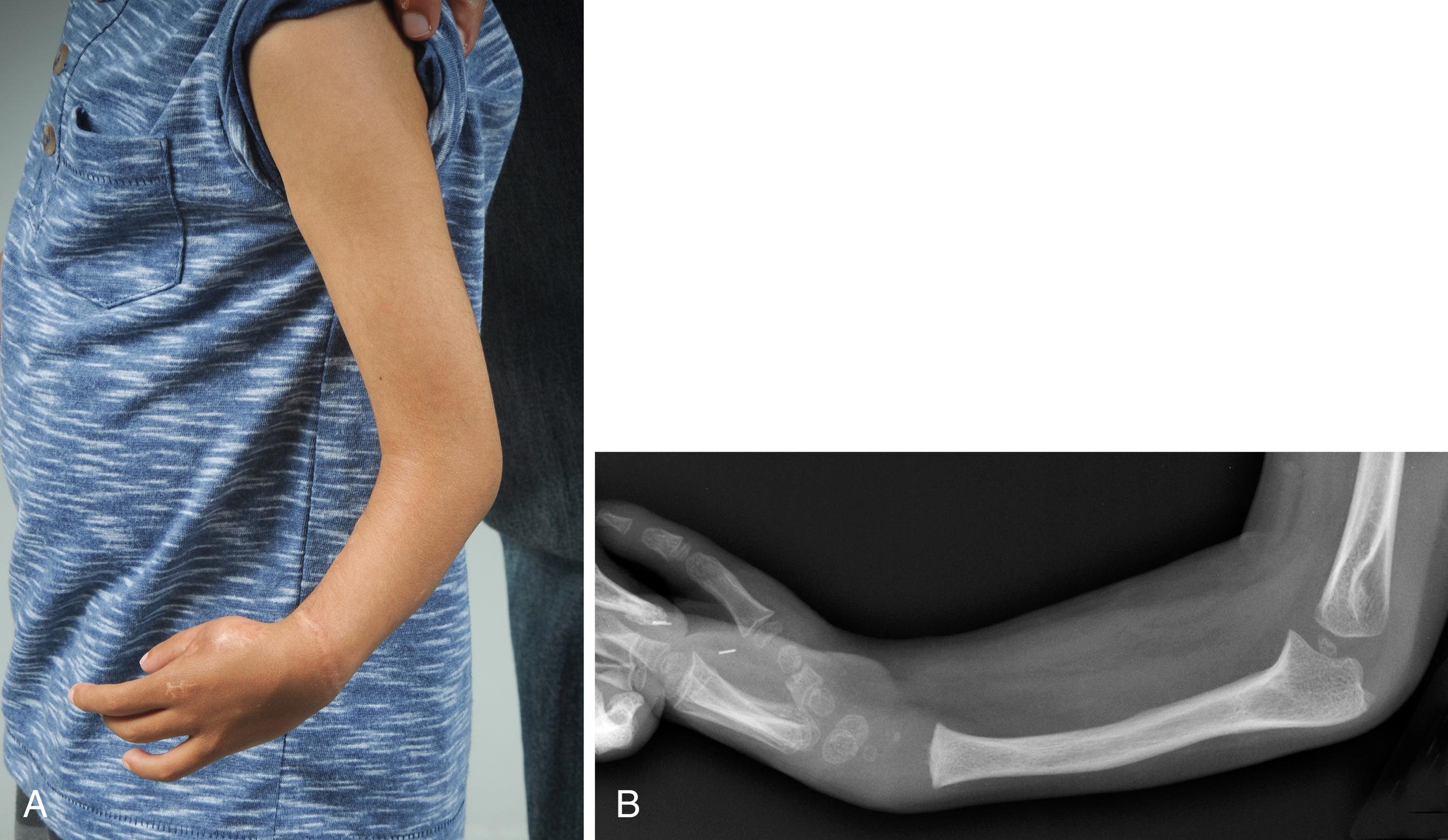
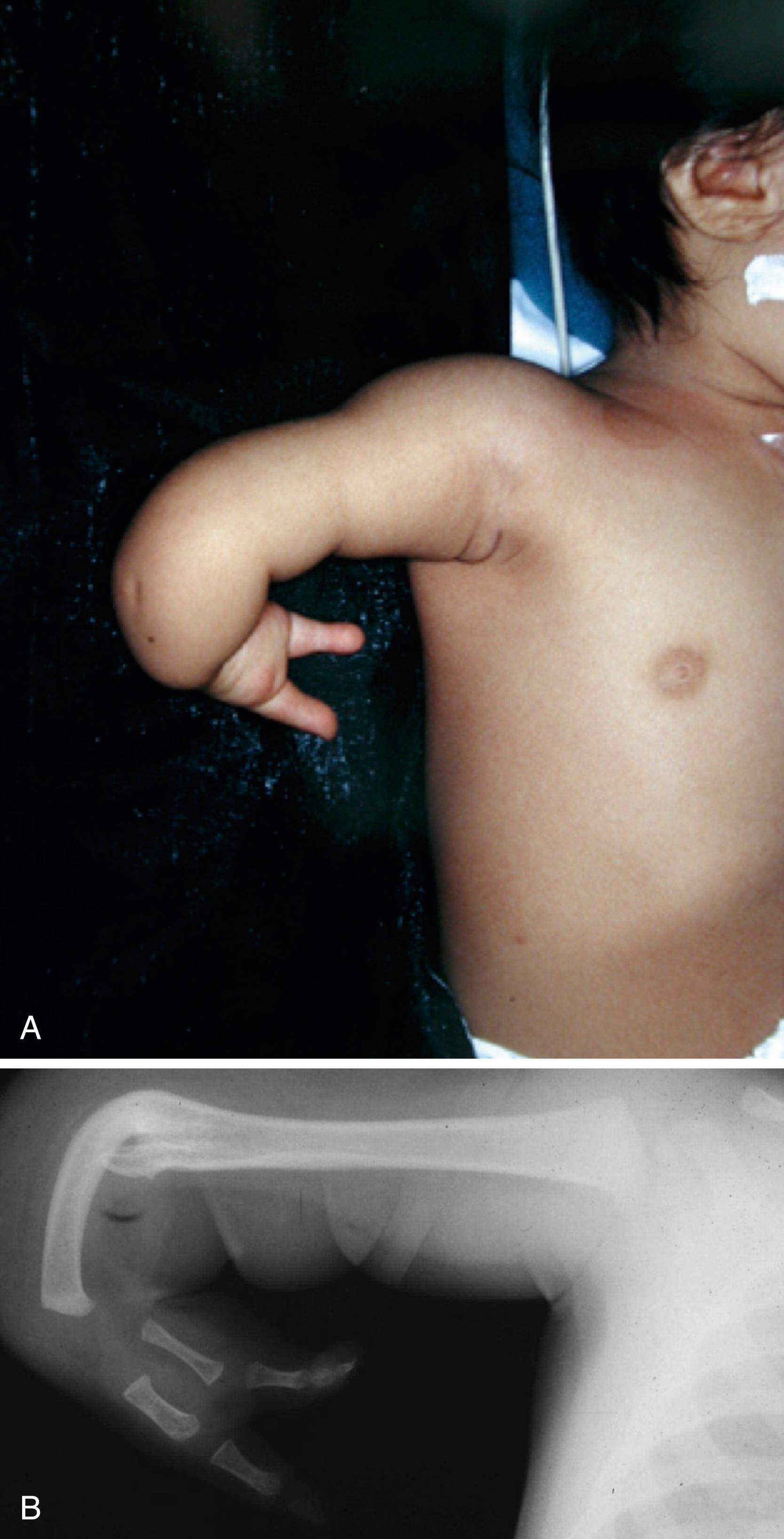
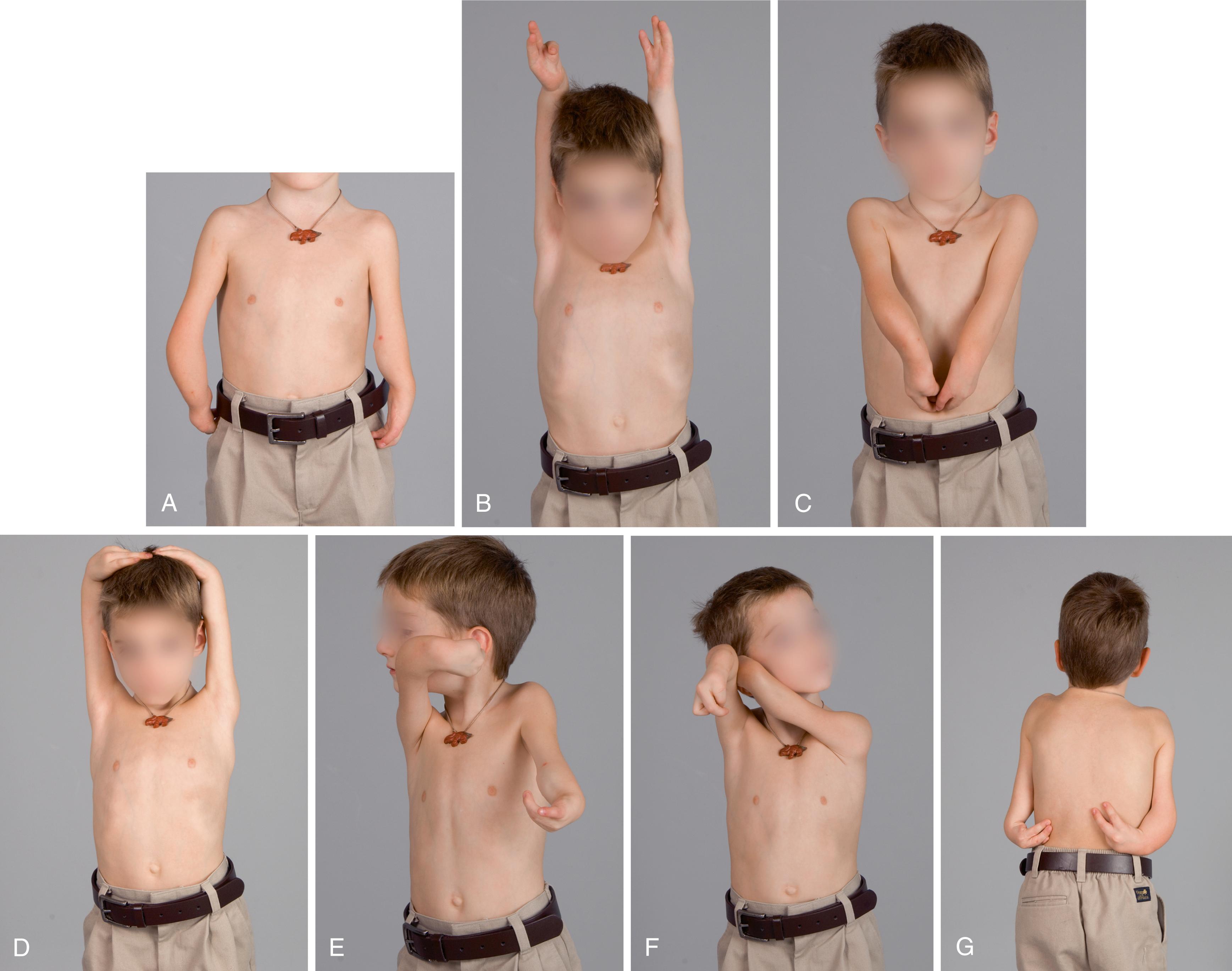
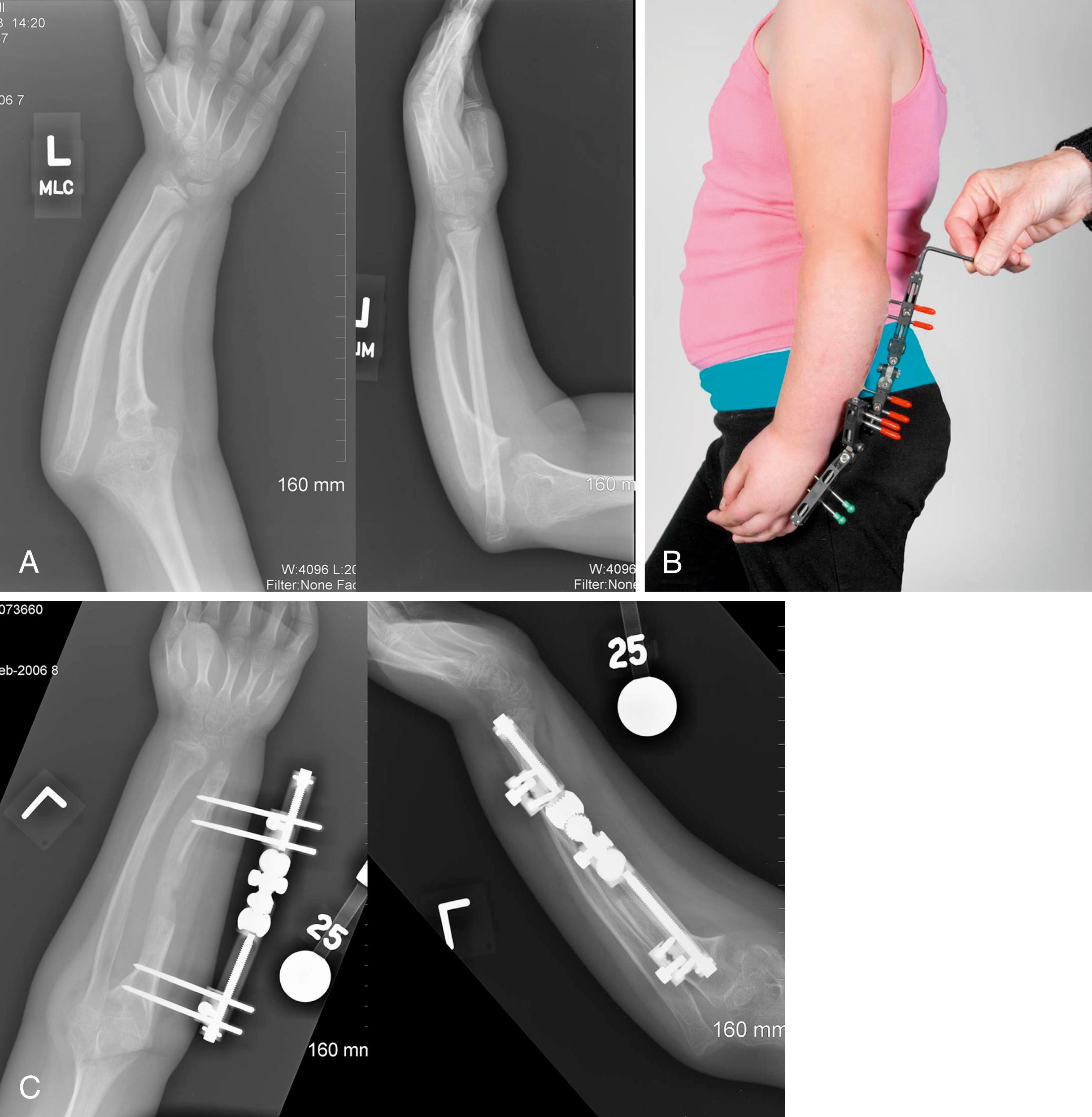
In cases of radiohumeral synostosis, the forearm is hyperextended relative to the humerus such that the hand rests on the buttock or flank ( Fig. 38.12 ). With this awkward positioning, children may be unable to reach their mouth or place their hand on top of their head. Over time, children may compensate for this position and obtain adequate function ( Fig. 38.13 ). In recalcitrant cases, a flexion osteotomy of the distal humerus improves the position of the hand and the overall function of the limb ( Fig. 38.14 ). Forearm rotational osteotomy is rarely necessary, even though the forearm is usually supinated. Rarely, the deformity may recur with growth, necessitating a repeat osteotomy at skeletal maturity.

The indications for surgical treatment of ulnar deviation of the wrist and instability of the forearm are less certain. Several authors have reported that ulnar deviation at the wrist is due to tethering by the ulnar anlage, a fibrocartilaginous structure occasionally found in the forearm of children with ulnar deficiency ( Fig. 38.15 ), hypothesizing that the ulnar anlage fails to grow with the radius and causes increasing ulnar deviation. Proponents of this theory have advocated early excision of the ulnar anlage to prevent progressive deformity. Others, however, have shown that increasing ulnar deviation is uncommon, and therefore resection of the anlage should be reserved for documented progression. The indications for surgical treatment of the forearm are even less defined. Some authors advocate surgical construction of a one-bone forearm to enhance forearm stability ; however, complete loss of forearm rotation may be detrimental to function. The surgeon must remember that despite substantial differences, these children are adaptive and ingenious, especially with parental support and therapy guidance.
See Chapter 48 .
See Chapter 36 .
The ulnar remnant is approached via a longitudinal incision along the ulnar border of the forearm ( Fig. 38.16 ). The ulnar extrinsic flexor muscles are often absent. The anlage will be adjacent to the ulnar neurovascular bundle, which must be protected. The anlage is dissected from its carpal attachment. The entire anlage need not be removed; removal of the distal third is adequate to release the tether. The subcutaneous tissue and skin are closed with absorbable suture and a long-arm cast is applied. The wrist is positioned as close to neutral as possible. Casting is maintained for 6 weeks and followed by a short-arm splint that is worn at night until skeletal maturity.
The distal end of the humerus is approached via a lateral incision. The course of the brachial artery should be marked preoperatively with a Doppler ( Fig. 38.17 ). Careful dissection is performed through the subcutaneous tissue, with care taken to visualize the radial nerve, which may be anomalous. The alignment of the humerus is marked by electrocautery or by inserting parallel Kirschner wires above and below the planned osteotomy site. A transverse osteotomy is performed, and the distal fragment is flexed and rotated until the hand can be placed in front of the trunk. Tight soft tissues may require bone shortening to prevent a traction injury to the neurovascular structures. The osteotomy is fixed with crossed Kirschner wires or a small plate. The subcutaneous tissue and skin are closed with absorbable suture. A well-fitted long-arm cast is applied and attached to the body with a Velpeau-type dressing.

This operation is rarely indicated but can help restore ulnar length in more mild cases of ulnar deficiency ( Fig. 38.18 ).
This operation is rarely indicated for patients with ulnar deficiency.
Excision of the ulnar anlage is reserved for children with progressive ulnar deviation of the wrist. The anlage may be resected at the same time as hand reconstruction, usually at around 1 year of age. Humeral rotational osteotomy is reserved for children who are impaired by inability to reach their hand to the midline or to their face and head. Surgery is performed after children are old enough to evaluate their ability to perform activities of daily living. This age allows additional determination of the optimal limb position for function.
Ulnar deficiencies are associated with other musculoskeletal abnormalities that warrant careful physical examination supplemented by radiographs (e.g., congenital scoliosis).
The forearm is difficult to manage and treatment should be individualized. Treatment is dependent on forearm stability, available elbow motion, and function. Surgery to restore motion for synostosis across the elbow or forearm (or both) is unsuccessful.
Ulnar deficiencies may be accompanied by thumb anomalies ranging from a narrow web space to an absent thumb, which are a major predictor of function. The thumb deficiency limits prehensile activity and is treated by principles similar to those for isolated thumb hypoplasia.
Children with unilateral ulnar deficiency generally function well, but those with radiohumeral synostosis, absent or stiff fingers, and/or bilateral deficiencies are more impaired.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here