Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Amputation of the upper extremity takes its toll on both the patient and the surgeon. The patient is devastated at the prospect of life with a functional disability and laments the potential loss of the independence we all take for granted. For the surgeon, the toll is much less, but there remain feelings of sympathy and regret, as we wish we had another option. Nonetheless, it is important that surgeons who care for the hand and upper extremity have an appreciation of the finer points of amputations. In addition, they should have a comfortable understanding of the treatment goals in postoperative rehabilitation and functional restoration of the upper extremity to maximize outcomes.
While the amputation of a digit is by far more common, major upper extremity amputations comprise up to a quarter of all amputations. In the United States alone, the prevalence of transradial amputations was approximately 41,000 people in 2005. This has risen from previous estimates due to improved trauma and critical care medicine, which is preserving the life of severely injured patients; it is likely to continue to rise due to an aging population of patients with a higher incidence of comorbidities including diabetes and vascular disease. The human hand has 23 degrees of freedom and its utility is closely linked to our abilities to be gainfully employed or to perform simple activities of daily living. The effects of an upper extremity amputation are significant and greatly impact quality of life. Up to one-third of patients who undergo amputation of an upper extremity require a change in occupation, and almost two-thirds discontinue hobbies and vocations they participated in prior to their amputation. ,
The technical principles of upper extremity amputations are fairly constant, regardless of indication for surgery or level of amputation:
Preservation of functional length
Durable coverage of the residual limb to allow for long-term prosthetic use
Prevention of symptomatic neuromas
Prevention of adjacent joint contractures
Early prosthetic fitting (“golden period”)
Unlike in the lower extremity, the majority of upper extremity amputations are performed for acute trauma. , In fact, in a Scandinavian epidemiologic study, up to 90% of upper extremity amputations were trauma-related. Amputations may be performed acutely when the hand surgeon believes that the functional potential of the salvaged limb would be substantially worse than prosthetic limb rehabilitation. At times, the surgeon will elect to perform multiple operative procedures in an attempt to salvage a hand or extremity but are unsuccessful in these attempts. It is even possible that these attempts to salvage a severely damaged limb can be detrimental to the health of the patient. In these cases, there is often severe and irreparable damage to the neurovascular supply to the extremity or severe injuries to the skeleton, either of which may make meaningful recovery nearly impossible. It is also possible that amputations are performed in a delayed or staged fashion, such as when replantations and other reconstructive efforts ultimately fail.
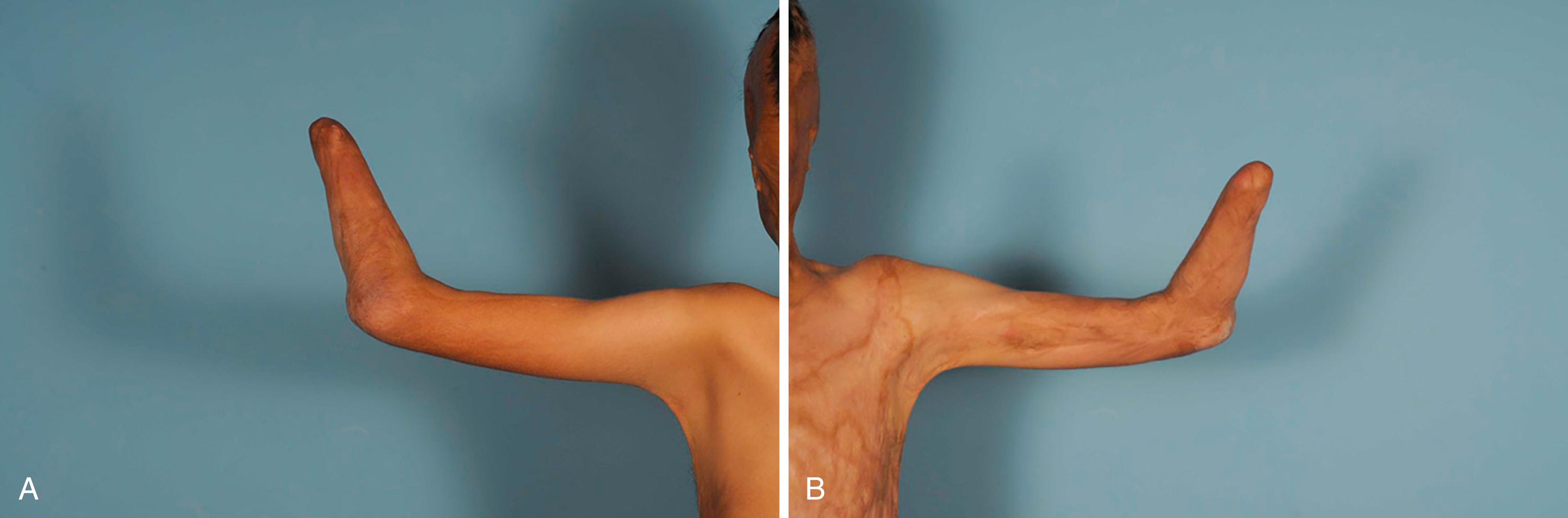
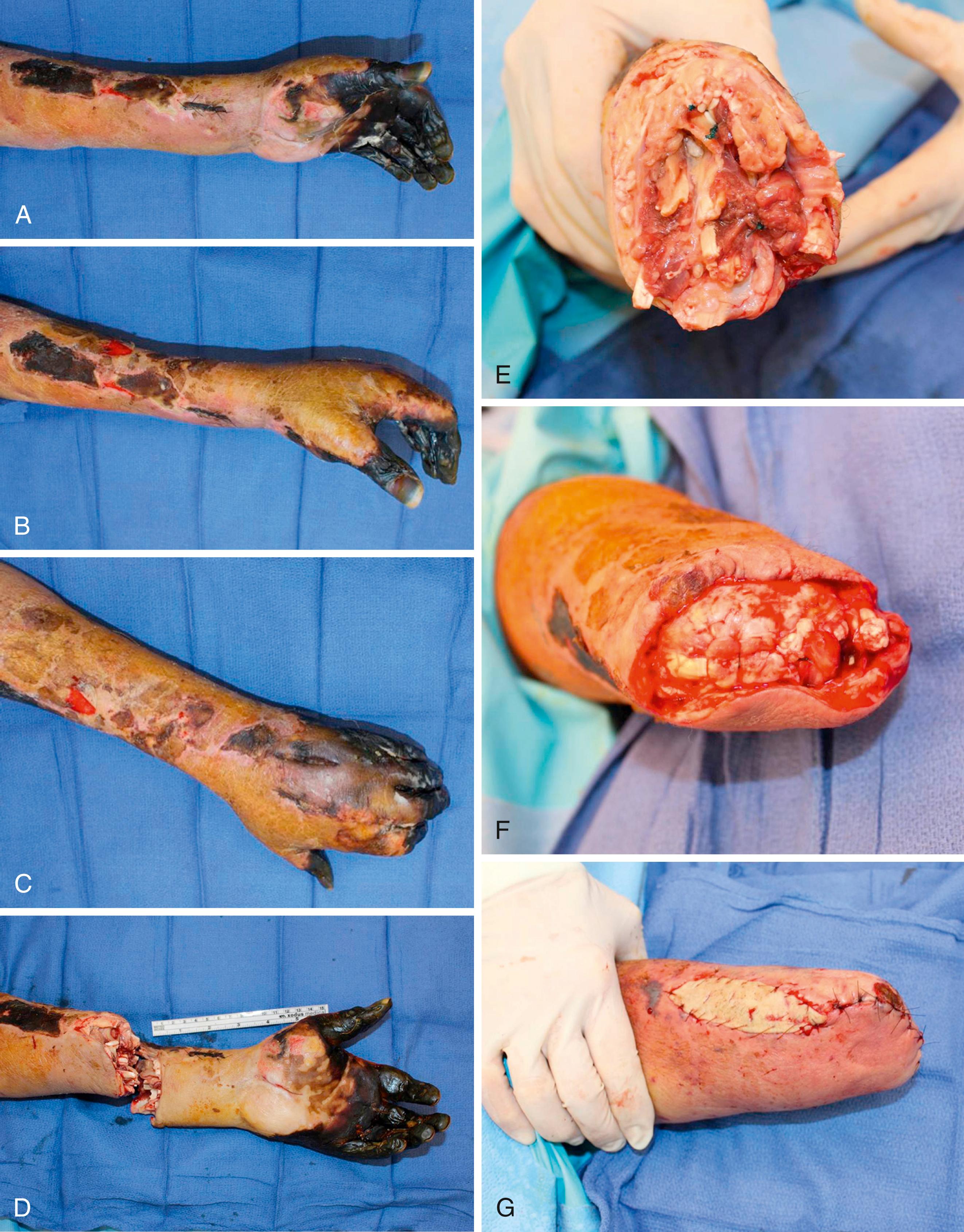
Major upper extremity amputations may also be required following burns or infections or as treatment for malignancies. Up to 26% of electrocution injuries require some form of major amputation. Deep thermal burns result in amputations approximately 3.8% of the time, usually due to nonviable tissues, but at times for control of a septic source ( Fig. 50.1 ). While most infections can be managed with antibiotics and surgical debridement, invasive fungal infections, like mucormycosis, almost uniformly result in amputation, particularly in the solid-organ transplant patient population. There has been only one case report published of a salvaged upper extremity in an immunocompromised patient with a mucormycosis infection. The mortality in this patient population has been reported as high as 92%. , Advances in radiation therapy, chemotherapy, and limb salvage surgical techniques have considerably reduced the need for upper extremity amputation in sarcoma patients over the past 40 years, yet radical amputation remains a mainstay of treatment in recurrent disease and large tumors. ,
After decades of research and clinical experience, controversy remains regarding the ideal level of amputation in patients that require removal of the hand. Wrist disarticulation preserves limb length, thus providing a longer lever arm with which to perform work. More importantly, the longer residual limb preserves the distal radioulnar joint (DRUJ), resulting in better pronation and supination. The metaphyseal flare of the distal radius also provides a contour that aides in suspension of a terminal device ( Fig. 50.2 ). However, these benefits come at a cost. The prominence of the distal radius and ulnar styloids can become pressure points, leading to breakdown of the soft tissues of the residual limb, usually along the incisional scar. Though the additional length in a wrist disarticulation provides a longer lever arm, it leads to a limb-length discrepancy with the uninvolved side when a prosthesis is worn. A myoelectric terminal device may add several centimeters of additional length to the end of a residual limb, making the limb length discrepancy even more prominent. This not only presents an esthetic concern but also makes it more difficult for a patient to reach the anatomic midline, requiring greater shoulder abduction and scapular retraction.

For these reasons, patients with wrist disarticulations are more likely to abandon their prostheses than patients with transradial amputations. , Ideally, the patient is afforded the opportunity to have a preoperative consultation with a physiatrist and a prosthetist so that they may make an educated decision between a wrist disarticulation and a transradial amputation. Given the usual indications for transradial amputation, however, this is unfortunately rarely the case. Amputation 8 to 10 cm proximal to the ulnar styloid provides the greatest variety of prosthetic options for functional restoration of the extremity. , This preserves an adequate arc of pronation and supination and a reasonable lever arm for flexion at the elbow. However, one form of amputation is not ideal for all patients, making the preoperative consultation critically important in the process. For instance, patients who perform heavy labor frequently prefer a wrist disarticulation due to the increased durability of a body-powered prosthetic, the increased lever arm length, and the preserved DRUJ.
As the transradial amputation becomes more proximal and approaches the elbow, the anticipated pronation and supination may be minimal. In fact, there is minimal pronation and supination once half of the original forearm length is removed. Yet preserving at least 5 cm of ulna is sufficient for successful prosthetic fitting. The addition of an elbow joint to the prosthesis greatly increases the amount of work required to use it and dramatically increases the likelihood of abandonment. As a result, preserving the elbow joint should remain a high priority, even when complex reconstructive efforts such as free flaps are required to maintain this joint.
The skin incisions are designed with equal-length flaps along the volar and dorsal aspects of the forearm, in what is often referred to as a “fish-mouth” pattern ( Case Study 50.1 ). The incisions are designed so that the osteotomies in the radius and ulna will lie at least 1 to 2 cm proximal to the level of skin incision ( Fig. 50.3 ). The arm is exsanguinated, and tourniquet control is used for hemostasis. The skin and subcutaneous tissues are elevated off of the underlying antebrachial fascia proximally past the level of proposed osteotomies. The antebrachial fascia is then incised at the level of skin incision, and all of the neurovascular structures are individually identified. The radial and ulnar arteries are ligated with suture ties or vascular clips, while the interosseous vessels are cauterized. The flexor and extensor musculature is divided 1 cm distal to the level of osteotomies. The periosteum is incised, and a small cuff is elevated proximally. An oscillating saw is used to make the osteotomies, and the edges of the bone are smoothed with a rasp.
AM is a 67-year-old right-handed, critically ill man who developed ischemia of the left hand secondary to a thrombosed radial artery resulting from an arterial line and vasopressors. The patient underwent radial artery thrombectomy, carpal tunnel release, and hand fasciotomies. Intrinsic muscles appeared nonviable. Continued vasopressor usage led to gangrene of all digits and the distal palm, even with Doppler signals in palmar arches ( eFig. 50.1 ).
What level of amputation would provide the most prosthetic options?
ANS: The patient could undergo a wrist disarticulation or a transradial amputation. The former preserves the distal radioulnar joint and maximum pronation and supination, and the latter offers the most options for prosthetic rehabilitation. The ideal level of amputation is 8 to 10 cm proximal from the styloids.
The surgical procedure is shown in eFig. 50.2 .

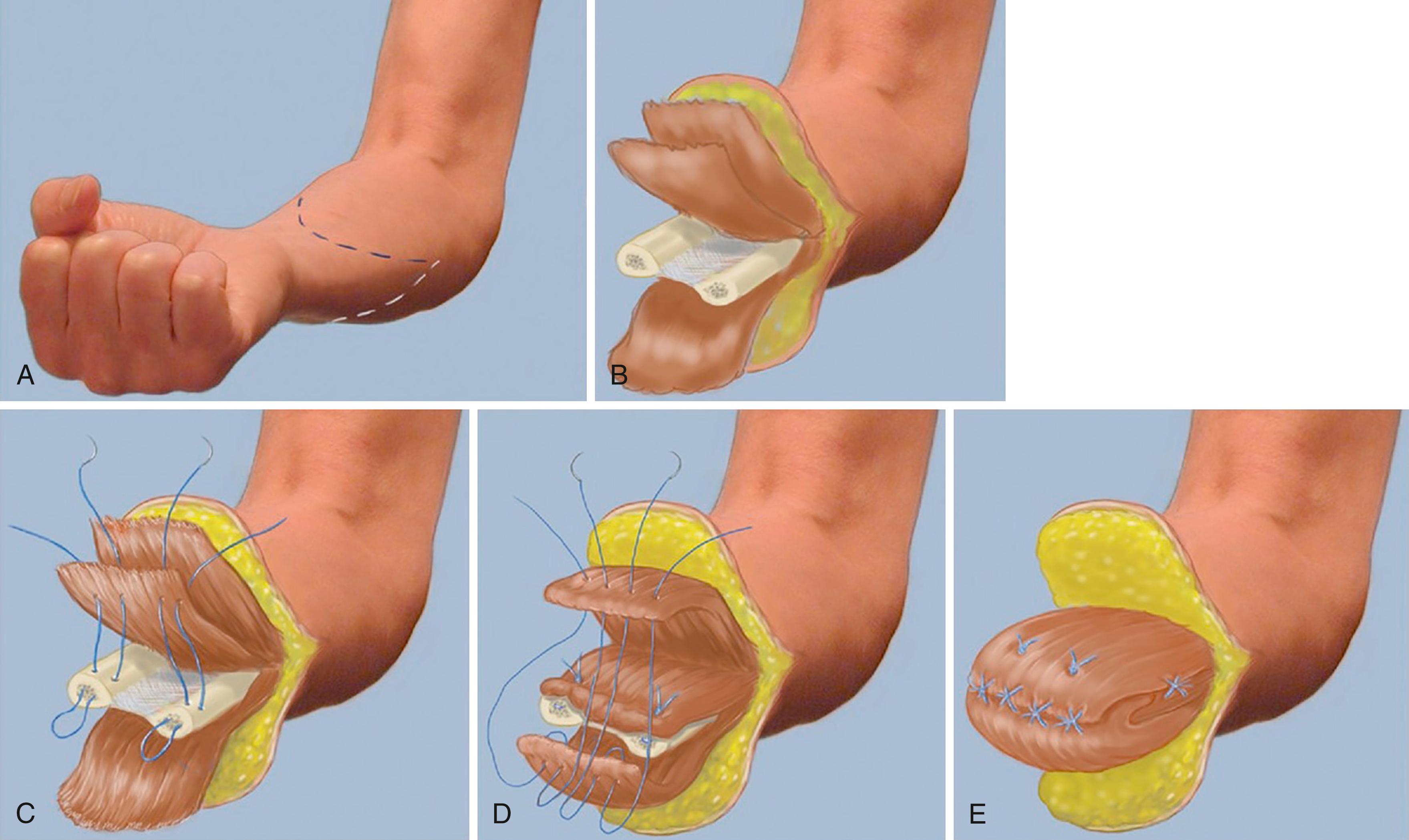
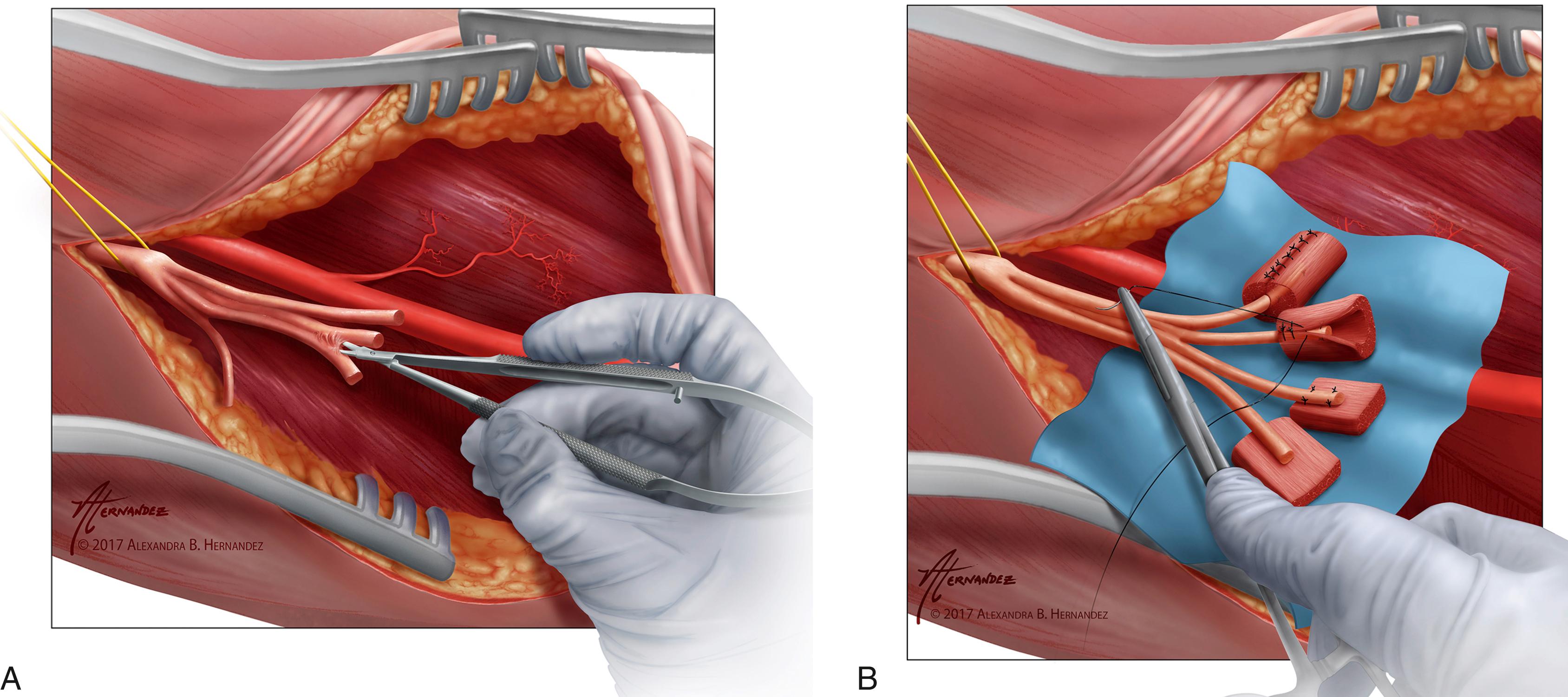
Regenerative peripheral nerve interfaces (RPNIs) or targeted-muscle reinnervation (TMR) should be performed at the time of amputation to reduce phantom pain and neuroma pain postoperatively (see Frontiers in Prosthetic Rehabilitation section). Each of the major mixed motor/sensory and pure sensory peripheral nerves should be controlled with either RPNIs or TMR. To create an RPNI, the peripheral nerve is sharply transected with a 15 blade at level of the bony cuts. A 30 × 15 × 5 mm muscle graft is harvested from the palmaris longus, flexor carpi radialis, or a distant site like the vastus lateralis. The muscle graft is harvested in the direction of the muscle fibers. All fatty tissue, fascia, and fibrous tissue are then removed from the muscle. The terminal end of the peripheral nerve is secured into the muscle graft with interrupted sutures of 6-0 nylon between the epineurium and epimysium ( Fig. 50.4 ). The edges of the muscle graft are then wrapped around the terminal end of the peripheral nerve and secured to itself similarly with epimysial sutures of 6-0 nylon. The RPNI construct is then placed deeper in the soft tissues away from the incision line. To perform TMR, a peripheral nerve stimulator is used to identify a motor branch to one of the residual innervated muscles of the forearm. The motor branch is then divided, and the terminal end of the peripheral nerve is coapted in an end-to-end fashion to the motor branch as it enters the muscle.
Once the peripheral nerves have been controlled with either RPNIs or TMR, a myodesis is then performed. The deeper muscle bellies are fixed firmly to the underlying skeleton to establish durable bony coverage and to prevent bursitis from excessive excursion of the muscles over the end of the bones. The superficial musculature is sutured with Ethibond in agonist/antagonist pairing over the end of the osteotomies. Care is taken to recreate physiologic tension to superficial muscle units to maximize postoperative contractions. The force of these contractions will ultimately be used to control a myoelectric prosthesis. The wound is closed in layers, and a bulky compressive dressing is applied.
The loss of the elbow joint has a significant adverse impact on the function of the residual limb and greatly diminishes a patient’s adaptation to meaningful use with a prosthetic. In these more proximal amputations, the elbow must be replaced with a prosthetic component that not only adds weight but also, more importantly, adds additional functional requirements that need to be replaced with fewer residual innervated muscles. Above-the-elbow prosthetics require the exertion of more energy to perform daily functions, and thus patients with transhumeral amputations are more likely to abandon their prosthetics than their transradial counterparts.
The discussion regarding elbow disarticulation versus transhumeral amputation is similar to the previous discussion regarding preservation of the distal forearm. There are advocates for either approach, as they each have their own benefits and drawbacks. Preservation of the distal humerus conserves the flare of the condyles, which not only aids in the suspension of the device but also allows for transmission of rotation. These benefits come at fairly high price, however. When an elbow disarticulation is performed, the greater length of the residual upper arm creates limb length discrepancy, which is particularly problematic when a patient utilizes a prosthetic device with an elbow articulation. In these situations, it is more difficult for the patient to reach the anatomic midline, and the asymmetry with the unaffected arm is fairly noticeable, unesthetic, and functionally limiting.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here