Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Chemotherapy is the mainstay of treatment. Surgery does not play a role in the curative treatment of lymphoma.
An adequate biopsy is critical to render an accurate diagnosis and classify lymphoma. An excisional or incisional biopsy is the preferred procedure for confirming a new diagnosis.
Along with the patient's clinical history and differential diagnosis, specimens should be submitted to the pathologist in saline for appropriate testing, such as flow cytometry.
Highly aggressive lymphomas such as Burkitt or lymphoblastic lymphoma should be referred to a medical oncologist emergently.
Limited-stage Hodgkin lymphoma and diffuse large B-cell lymphoma of the head and neck are highly curable with chemotherapy or a combination of chemotherapy and involved-field radiotherapy.
Mucosa-associated lymphoid tissue lymphomas of the thyroid and salivary glands are rarely life threatening and should be treated with low-dose involved-field radiotherapy.
Diffuse large B-cell lymphoma of the paranasal sinuses is associated with a high risk of relapse in the central nervous system.
Natural killer/T-cell lymphoma of the nasal type has an aggressive clinical course and frequently causes marked tissue destruction and necrosis. A combination of chemotherapy and radiotherapy is the most effective treatment.
Lymphomas are malignant neoplasms of lymphocytes and their precursor cells. Historically, lymphomas were classified merely by their histologic appearance, specifically, by cell size (small, large, or mixed) and architecture (nodular or diffuse). The classification system from the World Health Organization (WHO) 2008 defines specific subcategories of lymphoma according to the immunologic and molecular characteristics of the lymphoma cells as well as the morphology. The updated 2016 WHO classification ( Box 116.1 ) of hematopoietic and lymphoid tumor uses morphologic, immunophenotypic, genetic, and clinical features aiming for distinct diagnostic approach, clinical expectations, and therapeutic strategies for the lymphoid neoplasms and is not based on the anatomic location of tumor cells. Several types noted in the 2008 classification are now considered distinct and are grouped together under single diagnostic categories. Lymphoma accounts for approximately 5% to 15% of head and neck malignancies. However, the number varies with different countries of study. They are the third most common cancer worldwide and constitute 3% of malignant tumors. It is the second most common primary malignancy occurring in the head and neck after epithelial malignancy. A steady increase in the incidence of lymphoma, particularly non-Hodgkin lymphomas (NHL), has been reported in recent decades. Most subtypes of lymphoma can potentially involve the head and neck, either as the only site of disease or as one of many sites of involvement. Cervical lymph nodes are estimated to be involved in 70% of lymphomas at initial presentation, and the head and neck is the second most common site of extranodal involvement by lymphoma, In a recent U.S. population-based study using the Surveillance, Epidemiology, and End Results (SEER) database in oropharyngeal lymphoma, the most common subsite of origin was the tonsil, comprising 71% of lymphomas. As a result, otolaryngologists are often the first physicians to evaluate these patients and obtain biopsies as well as the first to inform patients of their diagnosis. Understanding the pathology, clinical features, treatment, and prognosis for each of the nodal and extranodal lymphoma subtypes that can occur in the head and neck permits for a more accurate and efficient evaluation. In addition, a brief discussion of the diagnosis and prognosis by the head and neck specialist is extremely valuable to patients and their families, while they are awaiting an initial appointment with a medical oncologist.
Chronic lymphocytic leukemia/small lymphocytic lymphoma
Monoclonal B-cell lymphocytosis *
* Changes from the 2008 classification.
B-cell prolymphocytic leukemia
Splenic marginal zone lymphoma
Hairy cell leukemia
Splenic B-cell lymphoma/leukemia , unclassifiable
Splenic diffuse red pulp small B-cell lymphoma
Hairy cell leukemia-variant
Lymphoplasmacytic lymphoma
Waldenström macroglobulinemia
MGUS, IgM *
µ heavy-chain disease
γ heavy-chain disease
α heavy-chain disease
MGUS, IgG/A *
Plasma cell myeloma
Solitary plasmacytoma of bone
Extraosseous plasmacytoma
Monoclonal immunoglobulin deposition diseases *
Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma)
Nodal marginal zone lymphoma
Pediatric nodal marginal zone lymphoma
Follicular lymphoma
Pediatric-type follicular lymphoma *
Large B-cell lymphoma with IRF4 rearrangement *
Primary cutaneous follicle center lymphoma
Mantle cell lymphoma
In situ mantle cell neoplasia *
DLBCL, NOS
T-cell/histiocyte-rich large B-cell lymphoma
Primary DLBCL of the central nervous system
Primary cutaneous DLBCL, leg type
EBV + DLBCL, NOS *
EBV + mucocutaneous ulcer *
DLBCL associated with chronic inflammation
Lymphomatoid granulomatosis
Primary mediastinal (thymic) large B-cell lymphoma
Intravascular large B-cell lymphoma
ALK + large B-cell lymphoma
Plasmablastic lymphoma
Primary effusion lymphoma
HHV8 + DLBCL , NOS *
Burkitt lymphoma
Burkitt-like lymphoma with 11q aberration *
High-grade B-cell lymphoma, with MYC and BCL2 and/or BCL6 rearrangements *
High-grade B-cell lymphoma, NOS *
B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and classical Hodgkin lymphoma
T-cell prolymphocytic leukemia
T-cell large granular lymphocytic leukemia
Chronic lymphoproliferative disorder of NK cells
Aggressive NK-cell leukemia
Systemic EBV + T-cell lymphoma of childhood *
Hydroa vacciniforme–like lymphoproliferative disorder *
Adult T-cell leukemia/lymphoma
Extranodal NK-/T-cell lymphoma, nasal type
Enteropathy-associated T-cell lymphoma
Monomorphic epitheliotropic intestinal T-cell lymphoma *
Indolent T-cell lymphoproliferative disorder of the GI tract *
Hepatosplenic T-cell lymphoma
Subcutaneous panniculitis-like T-cell lymphoma
Mycosis fungoides
Sézary syndrome
Primary cutaneous CD30 + T-cell lymphoproliferative disorders
Lymphomatoid papulosis
Primary cutaneous anaplastic large cell lymphoma
Primary cutaneous γδ T-cell lymphoma
Primary cutaneous CD8 + aggressive epidermotropic cytotoxic T-cell lymphoma
Primary cutaneous acral CD8 + T-cell lymphoma *
Primary cutaneous CD4 + small/medium T-cell lymphoproliferative disorder *
Peripheral T-cell lymphoma, NOS
Angioimmunoblastic T-cell lymphoma
Follicular T-cell lymphoma *
Nodal peripheral T-cell lymphoma with TFH phenotype *
Anaplastic large-cell lymphoma, ALK +
Anaplastic large-cell lymphoma, ALK − *
Breast implant–associated anaplastic large-cell lymphoma *
Nodular lymphocyte predominant Hodgkin lymphoma
Classical Hodgkin lymphoma
Nodular sclerosis classical Hodgkin lymphoma
Lymphocyte-rich classical Hodgkin lymphoma
Mixed cellularity classical Hodgkin lymphoma
Lymphocyte-depleted classical Hodgkin lymphoma
Plasmacytic hyperplasia PTLD
Infectious mononucleosis PTLD
Florid follicular hyperplasia PTLD *
Polymorphic PTLD
Monomorphic PTLD (B- and T-/NK-cell types)
Classical Hodgkin lymphoma PTLD
Histiocytic sarcoma
Langerhans cell histiocytosis
Langerhans cell sarcoma
Indeterminate dendritic cell tumor
Interdigitating dendritic cell sarcoma
Follicular dendritic cell sarcoma
Fibroblastic reticular cell tumor
Disseminated juvenile xanthogranuloma
Erdheim-Chester disease *
Provisional entities are listed in italics .
ALK, Anaplastic lymphoma kinase; BCL, B-cell lymphoma; EBV , Epstein-Barr virus; DLBCL , diffuse large B-cell lymphoma; Ig, immunoglobulin; IRF4, interferon regulatory factor 4; MGUS, monoclonal gammopathy of undetermined significance; NK , natural killer; PTLD, posttransplant lymphoproliferative disorders.
The American Cancer Society has estimated an increase in new cases of lymphoma in the United States in 2020, including 77,240 cases of NHL and 8480 cases of Hodgkin lymphoma (HL). About 970 deaths from HL and 19,940 from NHL will be attributed in the same year. The incidence of NHL has risen dramatically since 1970. An average risk of developing NHL during lifetime is about 1 in 47. The cause of this rise is not completely understood. The human immunodeficiency virus (HIV) epidemic and the increase in NHL after solid organ transplants account for only a minority of the new lymphomas. The incidence of NHL is slightly higher in men than in women, and it increases exponentially with age. The most reproducible environmental risk factor is exposure to certain pesticides or herbicides, and inconsistent associations have been reported with hair dyes, ultraviolet radiation, certain occupations, smoking, consuming foods high in animal fat, and receiving blood transfusions. Obesity positively correlates with the incidence of diffuse large B-cell lymphoma (DLBCL) in several studies. Infectious agents that include Epstein-Barr virus (EBV), HIV, human T-cell leukemia virus 1, Helicobacter pylori, Chlamydia psittaci, hepatitis C, human herpesvirus 8, simian virus 40 (SV40), and Borrelia burgdorferi have been proposed as etiologic agents in the pathogenesis of some cases of NHL. Other factors associated with a significantly increased risk of NHL include autoimmune disorders, most commonly Sjögren syndrome and rheumatoid arthritis, although it is difficult to separate the effects of immunosuppressive drugs used to treat these diseases and the underlying autoimmune disease.
HL has a bimodal age distribution in developed countries; the first peak occurs in the third decade of life, and the second peak occurs after the age of 50 years. Men have a slightly higher incidence than women. An association exists between HL and factors that decrease exposure to infectious agents at an early age, including advanced maternal education, early birth order, decreased number of siblings, and living in a single-family residence. A history of infectious mononucleosis increases the risk of HL at least threefold and suggests EBV as an etiologic agent. The nearly 20-fold increased risk of HL reported in patients with HIV and other conditions associated with chronic immunosuppression is also likely related to chronic EBV infection. An increased incidence among first-degree relatives, a significant concordance rate among identical but not fraternal twins, and linkage with certain human leukocyte antigen types suggest a genetic predisposition for HL. Tobacco use may increase the risk of HL as shown in multiple studies. Some childhood infectious illnesses such as measles, mumps, rubella, chickenpox, and pertussis may have a negative association with the occurrence of HL ( P = .013). Furthermore, breastfeeding has been shown in multiple studies to provide the protective effect, but the possible role of maternal antibodies is not clear. A population-based case-control study of 565 case patients with HL has demonstrated that aspirin may protect against HL possibly through inhibition of transcription factor such as NF-κB, which has significant role in the survival of HL cells.
Lymphoma should be included in the differential diagnosis of any patient with adenopathy, salivary gland enlargement, or a mass in Waldeyer ring (WR), nasal cavity, paranasal sinuses, or thyroid. An accurate history and physical examination can provide important clues to the diagnosis.
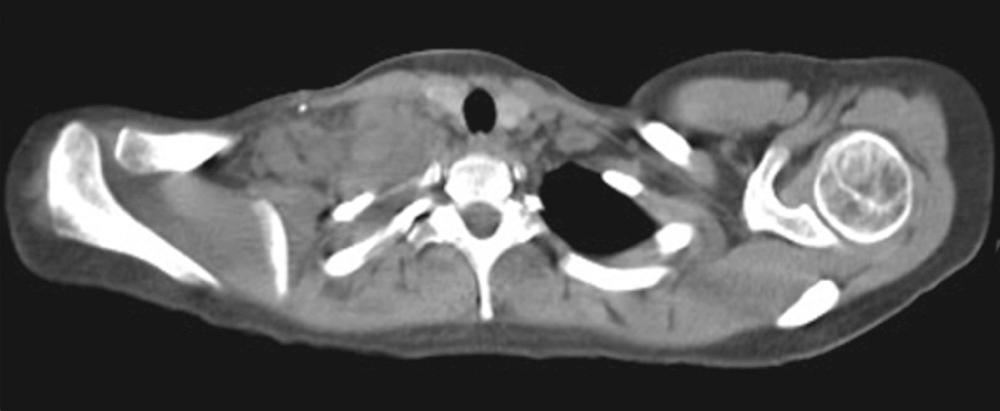
Classical HL occurs most commonly in young adults and usually manifests as painless lymphadenopathy in the cervical and/or supraclavicular regions. In contrast to NHL, HL spreads in a contiguous pattern, and it rarely involves the preauricular or occipital nodes or extranodal sites of the head and neck, such as the tonsil or sinus. Infraclavicular involvement in patients with bulky supraclavicular nodes is common in HL but is rarely seen in NHL. Bulky, matted nodes are not uncommon ( Fig. 116.1 ). Although staging studies reveal mediastinal adenopathy in more than 85% of patients with HL, symptoms of cough, chest pain, dyspnea, and superior vena cava (SVC) syndrome are uncommon, even in patients with bulky mediastinal disease. Systemic symptoms, or “B” symptoms, including fevers (temperature greater than 38°C), drenching night sweats, and weight loss, occur in 30% to 40% of patients with stage III or IV disease but in fewer than 10% of patients with stage I or II disease. A hallmark of HL—generalized, severe pruritus—occurs in approximately 25% of patients with HL. It often precedes the diagnosis by months, can be a presenting symptom of both early- and advanced-stage disease, and has no known prognostic significance. Alcohol-induced pain in involved lymph nodes is a rare symptom of HL (<1%). A rare subtype of HL, nodular lymphocyte–predominant HL (LPHL), usually is seen as a solitary cervical, axillary, or inguinal lymph node mass. In LPHL, the mediastinum is generally spared, and in contrast to the contiguous pattern of lymph node involvement in classic HL, the pattern of spread is not consistent.
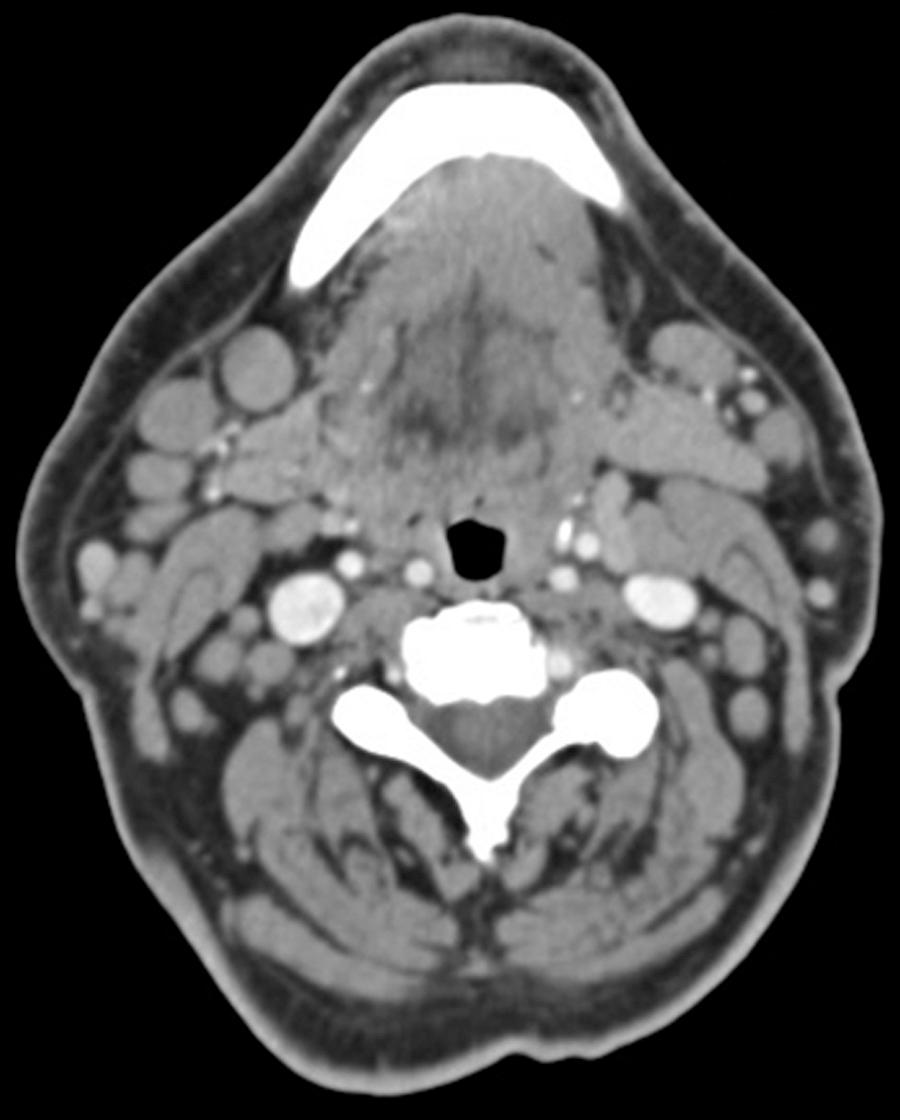
Presenting symptoms of NHLs vary substantially and depend on the pathologic subtype of NHL and the disease site. The asymmetric enlargement of tonsil and preauricular lymphadenopathy are common presentations of nodal and extranodal involvement of the head and neck lymphoma. The cervical region and lymphoid tissue of the WR (tonsils, base of the tongue, and nasopharynx) are commonly involved in NHL. Indolent lymphomas, such as follicular lymphoma (FL) or chronic lymphocytic leukemia/small lymphocytic lymphoma (SLL), often manifest with painless peripheral adenopathy. Multiple soft, mobile, bilateral cervical nodes that range in size from 1 to 2 cm are common with both FL and SLL ( Fig. 116.2 ); matted peripheral lymph nodes are uncommon. Isolated head and neck involvement is unusual with these subtypes of lymphoma, and examination of axillary and inguinal regions usually reveals additional enlarged nodes; SLL can also involve the tonsillar regions. Because spontaneous regressions occur in up to 20% of patients with FL, patients may describe a history of waxing and waning adenopathy, with swollen nodes present for years in some cases. Most patients with indolent lymphoma feel well at the initial visit, and B symptoms are unusual. Patients with SLL frequently have involvement of the peripheral blood, and a complete blood count may reveal a lymphocytosis. Peripheral blood flow cytometry may provide a diagnosis and may obviate the need for a tissue biopsy. Indolent lymphomas are uncommon before the age of 50 years.
Approximately one-third of mucosa-associated lymphoid tissue (MALT) lymphomas, indolent lymphomas that occur in extranodal sites, can be found in the head and neck. MALT lymphoma, currently incorporated as extranodal marginal zone lymphoma (MZL) of MALT, is a group of mature B-cell neoplasms, which occurs as an isolated swelling in the thyroid, or salivary gland, commonly the parotid gland, may also involve the ocular adenexa. The orbital structures (e.g., eyelid, extraocular muscles, lacrimal apparatus, and conjunctivae) are commonly involved in marginal zone and mantle cell lymphoma (MCL). Bilateral parotid involvement can occur, and occasionally a history of stable enlargement over months or years is elicited. Cases of MALT lymphoma have also been reported in the sinuses, oral cavity, nasal cavity, and tonsil. MALT lymphoma of the head and neck is often associated with autoimmune disorders such as Hashimoto thyroiditis, Sjögren syndrome, dermatomyositis, and circumscript sclerodermia, and it occasionally precedes the diagnosis of the autoimmune disorder.
Many aggressive NHLs, the most common being DLBCL, also often occur as painless cervical or supraclavicular adenopathy without other associated symptoms. Fevers, night sweats, or weight loss occurs in about 20% of patients with advanced-stage disease. Primary extranodal large cell lymphomas are common and account for 15% to 20% of all large cell lymphomas; these can occur in the tonsils, nasopharynx, oropharynx, thyroid, salivary glands, or sinuses. Primary central nervous system (CNS) lymphoma may also involve the eye. The presentation of extranodal lymphomas of the head and neck is discussed in more detail later in this chapter.
Two very aggressive NHLs, lymphoblastic and Burkitt lymphomas, are rare in the adult population but can occur with acute symptoms, and they can be life threatening without rapid intervention. In adults, lymphoblastic lymphomas occur most commonly in young men and frequently occur with acute respiratory compromise because of bulky mediastinal adenopathy and pleural or pericardial effusions. Occasionally, supraclavicular adenopathy is present, and the otolaryngologist will be called on to obtain diagnostic tissue emergently.
Because surgery does not play a role in the curative treatment of lymphoma, the goal of biopsy is to provide enough material for an accurate diagnosis while minimizing the cosmetic effect of the biopsy. If the biopsy involves a nodal site, sample the largest node or any node growing out of proportion to other nodes in order to exclude transformed lymphoma. Sampling a single site is usually adequate.
Tissue biopsy is essential in the diagnosis and management of patients with lymphoma. Recent advances in the understanding of the immunology and molecular biology of lymphoma, as well as new diagnostic reagents and methods, have resulted in more precise diagnoses. The most recent WHO classification includes mature B-cell neoplasms, which comprise more than 30 subtypes, mature T and natural killer (NK) neoplasms, HL, and histiocytic and dendritic cell neoplasms. A separate group has been designated for posttransplant lymphoproliferative disorders (PTLD) for lymphoma associated with solid organ transplantation and allogeneic hematopoietic stem cell transplantation, with B-cell neoplasms representing 80% to 90% of this group (see Box 116.1 ). When the clinical history is suggestive of lymphoma, but initial histologic review, immunohistochemistry (IHC), or flow cytometry is nondiagnostic, molecular testing for T-cell receptor and immunoglobulin heavy-chain gene rearrangements should be considered. Cases in which the pathologic diagnosis appears inconsistent with the clinical history should be reviewed by an expert hematopathologist.
The proper handling of specimens for adjunctive diagnostic tests is critical whenever lymphoma is suspected. Specimens should not be transported on dry towels or surgical sponges; rather, they should be submitted to the pathologist in saline along with the patient's clinical history and differential diagnosis. Specimens should not be held overnight or for extended periods prior to processing by the pathology laboratory. If there will be a delay in processing the specimen, preserve a portion of the specimen in formalin to maintain the architecture. Crushed specimens are extremely difficult to evaluate for lymphoma.
The pathologist usually reserves fresh cells or frozen tissue for immunophenotyping and molecular diagnostics as needed. Immunophenotyping is performed, by either flow cytometry or IHC staining or both, for nearly all new cases of lymphoma. Flow cytometry requires a fresh cell suspension, but it offers the advantage of preservation of antigens. IHC staining can be performed on slides prepared from frozen tissue or paraffin-embedded, formalin-fixed tissue. Although fewer antigens are preserved in fixed and embedded tissues, performing IHC staining on them allows analysis of archival specimens and offers the benefit of correlation with architectural and cellular details.
Obtaining an accurate diagnosis of lymphoma according to the WHO classification system requires the integration of clinical, morphologic, cytogenetic, molecular, and immunophenotypic features. Therefore, it is essential that all available clinical and diagnostic information related to a specimen be made available to the hematopathologist, including any prior diagnosis of lymphoma.
Because of the improved diagnostic methods previously discussed, a less-invasive procedure, such as fine-needle aspiration (FNA) or core needle biopsy (CNB), may lead to a precise diagnosis without the need for surgery in some cases of lymphoma. Although FNA is a rapid and cost-effective method, it provides only cytologic materials; cytology alone is less useful for the initial diagnosis of lymphomas, because the architectural pattern is often necessary for accurate subclassification. In addition, FNA often does not provide adequate tissue for immunophenotyping, especially when the lymphoma is associated with extensive fibrosis, which limits the ability to aspirate cells. However, if an adequate number of cells can be aspirated, many pathologists agree that FNA may be adequate in the setting of relapsed disease, because it is often easier to confirm a previous diagnosis than to render an initial diagnosis on the basis of limited materials.
Because of the lack of fibrosis and a unique cytologic appearance and immunophenotype, SLL and lymphoblastic lymphoma can often be accurately diagnosed solely on the basis of FNA. Lymphoblastic lymphoma, a high-grade lymphoma, often presents with SVC syndrome or severe dyspnea and progresses extremely rapidly, and the ability of pathologists to provide a preliminary diagnosis within hours on the basis of FNA of a supraclavicular or mediastinal node may permit earlier initiation of therapy. In one report of eight children with lymphoblastic lymphoma, FNA was used as the initial diagnostic procedure. Immunophenotyping established the T-cell derivation in all cases, and treatment was initiated based only on FNA results in six cases. Two patients had subsequent surgical biopsies that confirmed the FNA diagnosis of lymphoblastic lymphoma. In a separate retrospective study, nine of nine cases of lymphoblastic lymphoma were correctly identified on the basis of specimens obtained by FNA.
The value of FNA in the diagnosis of other lymphoma types is more controversial. Hehn and colleagues found that a specific and complete histologic diagnosis of lymphoma was obtained in only 27 of 93 FNA attempts (29%) at initial diagnosis and in only 9 of 22 FNA attempts (41%) done in the setting of recurrent disease. Importantly, these 115 needle aspirations were interpreted by 70 different pathologists in the community setting, and only 43% had concurrent ancillary studies such as flow cytometry. They concluded that FNA is not useful in the diagnosis of lymphoma. However, in several more recent reports, when ancillary studies such as flow cytometry were routinely combined with cytomorphology, the sensitivity and specificity in the differentiation of NHL from nonmalignant pathology reached 95% to 97%, with similarly impressive positive and negative predictive values. Nonetheless, the precision of NHL subclassification remains a concern, and studies consistently demonstrate an accuracy rate of only 50% to 70%. A large systematic review has analyzed the 42 studies on effectiveness of FNAC and CNB to diagnose and subclassify lymphoma. The study has reported that FNAC/CNB yields a definitive diagnosis in only about 65% to 75%. Therefore, the current recommendation is that FNA alone is not sufficient for the initial diagnosis of lymphoma.
An accurate diagnosis of lymphoma by FNA requires an experienced sampling team, an expert cytopathologist, and the facilities to perform and interpret appropriate ancillary tests. The continued identification of unique immunophenotypic and molecular changes associated with many subtypes of lymphoma and the addition of other ancillary techniques, such as polymerase chain reaction or fluorescence in situ hybridization, are likely to make this procedure more promising as the sole method of diagnosis in the future, although limitations remain in selected situations, such as tissues with necrosis, partial involvement, or fibrosis.
The use of percutaneous CNB can sometimes overcome the limitations of FNA by retaining the architecture of the tissue and providing serial sections for histochemical and immunocytochemical stains. If a CNB is technically feasible, use the largest gauge needle possible (12 to 16 gauge) and obtain multiple cores, when a lymph node is not easily accessible for open biopsy. In general, both the peripheral and central portion of the mass should be sampled to avoid obtaining only necrotic tissue.
Many studies to evaluate CNB for lymphoma diagnosis have been published. CNB procedures yielded a definitive lymphoma classification or sufficient material for formulation of a treatment plan in 78% to 95% of patients. Burke and colleagues reported their 9-year experience of CNB for the diagnosis of lymphoma of the head and neck in a single center. Of the 171 patients with lymphoma initially found in the head and neck, 83 underwent CNB as part of the workup, and 67 of these patients (81%) had adequate diagnostic tissue that resulted in treatment decisions from CNB only. Metzgeroth and colleagues compared results of FNA and CNB in 101 lymph nodes. Of the 46 lymph nodes with lymphoma, cytology alone achieved the definitive diagnosis only 30% of the time. When immunocytology was combined with cytology, the rate of diagnosis increased to 70% compared with a 96% diagnosis rate by CNB. Furthermore, the sensitivity of CNB in the diagnosis of lymphoma was reported to be 92% in a meta-analysis, in contrast to 74% reported in a meta-analysis of FNA.
The retrospective review on 70 patients with cervical lymphadenopathy who underwent core biopsy demonstrated that 63 (90%) were diagnostic for either lymphoma or other pathology, without requiring further tissue sampling. Overall, 19 patients were diagnosed with lymphoma, of whom only one required further biopsy owing to inconclusive initial core biopsy, suggesting that CNB could be an effective tool for initial investigation of lymphoma providing information comparable to excisional biopsies and involving less surgical risk to the patient at a lower cost to the hospital in comparison with excisional biopsy. But an incisional or excisional biopsy should be considered if the sample from CNB is nondiagnostic.
Despite encouraging results with limited needle biopsies, open biopsy remains the gold standard, and both oncologists and hematopathologists prefer an open (excisional or incisional) biopsy as initial diagnostic tissue in nearly all cases of lymphoma. Because biopsies can be obtained from head and neck masses with less invasive procedures than those for intrathoracic or intra-abdominal lymph nodes, there should be no reason to potentially compromise the diagnosis because of limited material. Histologic diagnosis obtained from excisional or incisional biopsy is usually confirmed with the result of flow cytometry and immunohistochemical stains of the biopsied material.
In summary, an incisional or excisional biopsy provides adequate tissue for diagnosis. Therefore it is the preferred modality of initial investigation. A CNB plays an important role when open biopsy is not possible to perform.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here