Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ulceration of the lower extremity is a relatively common condition that causes significant discomfort and disability. An ulcer is defined as a disruption of the skin with erosion of the underlying subcutaneous tissue. This breach may extend further to the contiguous muscle and bone. The pathophysiologic mechanisms underlying ulcer formation are multifactorial and include neuropathy, infection, ischemia, and abnormal foot structure and biomechanics. It is not surprising then that the management of the diabetic foot is a complex clinical problem requiring an interdisciplinary approach. Minor trauma, often footwear related, is a frequent inciting event. A chronic ulcer is defined as a full thickness skin defect with no significant re-epithelialization for more than 4 weeks.
Common causes of leg ulcerations are responsible for almost 95% of leg ulcers; about 40% to 80% of ulcers are a result of underlying venous disease, 10% to 20% are caused by arterial insufficiency, 15% to 25% are a consequence of diabetes mellitus, and in 10% to 15% of patients a combination of two or more causes exists. Prolonged pressure and local infection are common causes of leg ulcers with minimal vascular compromise. Rare causes are responsible for less than 5% of all leg ulcers ( Box 61.1 ). The disease entities that usually underlie leg ulceration, such as venous insufficiency, peripheral artery disease, and diabetes mellitus, are associated with significant patient morbidity and mortality. A detailed knowledge of the clinical picture, pathogenesis, relevant diagnostic tests, treatment modalities, and differential diagnosis of leg ulcerations is essential in planning the optimal treatment strategy ( Table 61.1 ). An incorrect or delayed initial diagnosis may harm the patient and increase the risk of serious complications, including permanent disability and amputations.
Venous insufficiency
Peripheral artery disease
Vasculitis
Autoimmune disease (scleroderma)
Hypertension (Martrell ulcer)
Thromboangiitis obliterans (TAO; Buerger disease)
Lymphedema
Hematologic disorders (sickle cell anemia)
Clotting disorders (antiphospholipid syndrome)
Diabetes mellitus
Uremia
Acquired immunodeficiency syndrome (AIDS)
Nutritional deficiencies
Charcot foot
Rheumatoid arthritis (Felty syndrome)
Fracture, dislocations
Infectious diseases
Physical or chemical injury (trauma, pressure ulcers, burns, frostbite)
Metabolic diseases (porphyria, calciphylaxis)
Neoplasms (melanoma, basal cell carcinoma, squamous cell carcinoma, sarcomas)
Drug reactions or side effects (steroids, warfarin)
Ulcerating skin diseases (pyoderma gangrenosum)
| Site | Skin Appearance | Ulcer Characteristics | Other Findings | |
|---|---|---|---|---|
| Venous | Lower third of leg; malleolar area | Edema, hemosiderin, dermatitis, eczema | “Weeping,” irregular borders, painful | Varicose veins, “bottle” leg, ABI normal |
| Arterial | Most distal areas, toes | Thin, atrophic, dry, “shiny,” hair loss | Round, regular borders, no bleeding, dry base, very painful | Weak/absent pulse, poor capillary refill, ABI < 0.8 |
| Neurotrophic (diabetes mellitus) |
Pressure sites; heel and metatarsal heads | Cellulitis | Round, deep, purulent discharge, painless | Sensory deficit; ABI often > 1.3 due to vascular calcification |
The exact prevalence of lower extremity ulcers in the United States is unknown. The prevalence of leg ulceration in the general population of Western nations has been reported to be from 1% to 3.5%, with the prevalence increasing to 5% in the geriatric population. The data from these studies most likely underestimate the true prevalence because they do not include patients with leg ulcers who are not known to the healthcare system.
The cost of treating leg ulceration is staggering. Epidemiologic studies from Sweden estimated annual costs of treatment of lower extremity ulcers at $25 million. In England, the estimated cost of care for patients with leg ulcers in a population of 250,000 was about $130,000 annually per patient. Items factored into the equation include physician visits, hospital admissions, home healthcare, wound care supplies, rehabilitation, time lost from work, and jobs lost. Adding to the cost is the chronic nature of these wounds, the high rate of recurrence, and the propensity for ulcers to become infected. It is also evident that a true accounting of the cost is difficult because of the unknown prevalence of disease.
The social cost of leg ulcers also becomes a factor as the disease affects a patient’s lifestyle and attitude. The ability to work may be temporarily or permanently affected by the condition. Reduction in working capacity adds to the total cost. An estimated 10 million workdays annually are lost in the United States from lower extremity ulcers, and this figure may be low. A report in 1994 focused on the financial, social, and psychological implications of lower extremity lesions in 73 patients. Among the study patients, 68% reported feelings of fear, social isolation, anger, depression, and negative self-image because of the ulcers. In addition, 81% of the patients felt that their mobility was adversely affected. Within the younger population that was still actively working, there was a correlation between lower extremity ulceration and adverse effect on finances, time lost from work, and job loss. In addition, there was a strong correlation between time spent on ulcer care and feelings of anger and resentment. These factors combined to have a negative emotional impact on their lives.
An appreciation of the biomechanics required for walking is essential in understanding the etiology of foot ulcers. The foot is a complicated biologic structure containing 26 bones, numerous joints, and a network of ligaments, muscles, and blood vessels. Gait is a complex set of events that requires triplanar foot motion and control of multiple axes for complete bipedal ambulation ( Fig. 61.1 A ). When the heel hits the ground, its outer edge touches first. The foot is in a supinated position, which makes it firm and rigid. The soft tissue structures (muscles, tendons, and ligaments) then relax, allowing the foot to pronate. The foot becomes less rigid and is able to flatten, absorb the shock of touchdown, and adapt to uneven surfaces. During midstance, the heel lies below the ankle joint complex, the front and back of the foot are aligned, and the foot easily bears weight. Toward the end of midstance, the soft tissue structures begin to tighten; the foot resupinates and regains its arch. The foot is again firm, acting as a rigid lever for propulsion. The heel lifts off the ground, it swings slightly to the inside, and the toes push weight off the ground.
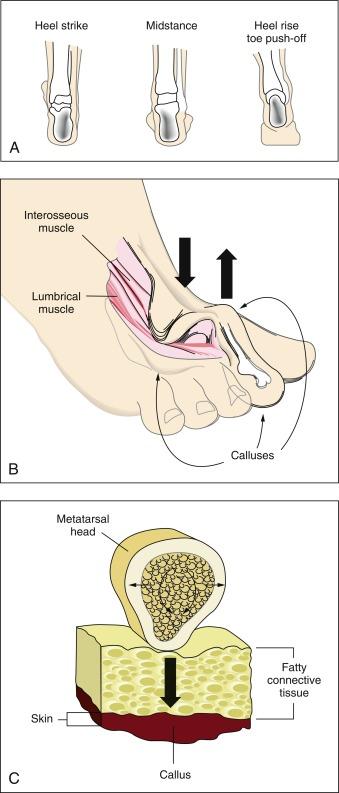
Sensory input from the visual and vestibular systems, as well as proprioceptive information from the lower extremities, is necessary to modify learned motor patterns and muscular output to execute the desired action. Various external and internal forces affect foot function. The combination of body weight pushing down and ground reactive force pushing up creates friction and compressive forces—shear results from the bones of the foot sliding parallel to their plane of contact during pronation and supination. Foot deformities or ill- fitting footwear enhance pressure points because they focus the forces on a smaller area. When the foot flattens too much or overpronates, the ankle and heel do not align during midstance and some bones are forced to support more weight. The foot strains under the body’s weight, causing the muscles to pull harder on these areas, making it more difficult for tendons and ligaments to hold bones and joints in proper alignment. Over time, swelling and pain on the bottom of the foot or near the heel may occur. Bunions can form at the great toe joint, and hammertoe deformities can form at the lesser toes. Abnormal foot biomechanics resulting from limited joint mobility and foot deformities magnify shearing forces, resulting in increased plantar pressure on the foot during ambulation (see Fig. 61.1 B and C). This can represent critical causes for tissue breakdown.
Venous leg ulcers are the most frequently occurring chronic lower extremity wounds ( Fig. 61.2 A ) (also see Chapter 54 ). The prevalence of lower extremity ulceration secondary to chronic venous disease in European and Western populations is estimated to be 0.5% to 1%. In the United States, it is estimated that between 600,000 and 2.5 million patients have venous ulcerations. Treatment costs in the United States are between $2.5 and $3 billion dollars, with a corresponding loss of 2 million workdays per year. Ten years ago, the annual cost of treatment for venous ulcer patients was almost $40,000 per patient. This cost has risen since then.

The physiology of venous blood flow is straightforward. Blood returns from the lower extremities against gravity to the inferior vena cava, through the deep and superficial venous systems. The deep veins are located within the muscles and deep fascia of the legs. The superficial system consists of the great saphenous vein and the small saphenous vein, and is located within the subcutaneous fat. Valves are present within both systems and prevent retrograde flow of the blood. A portion of blood from the superficial system is directed to the deep system through the communicating perforators. While standing, about 22% of the total blood volume is localized to the lower extremities, and hydrostatic pressure in the foot veins can reach 80 mm Hg. In healthy individuals with competent venous valves, the efficient calf muscle pump can reduce venous pressure by two-thirds during exercise. Venous insufficiency occurs when any of these elements do not function adequately. The pressure in the venous system increases, and most importantly, the ambulatory venous pressure rises during leg exercise. The primary cause of venous hypertension is insufficiency of the valves of the deep venous system and the perforating veins of the leg.
The exact mechanism by which ulcerations develop in patients with venous insufficiency is not clear. One theory is that ulceration results as a consequence of increased intraluminal pressure within the capillary system of the leg. The capillaries become dilated and elongated. Blood flow is sluggish, resulting in microthrombi formation and frequently leading to occlusion of the capillaries. Fibrin, albumin, and various macromolecules leak into the dermis, where they bind to and trap growth factors, making them unavailable for the tissue repair process. Leakage of fibrinogen through capillary walls results in deposition of pericapillary fibrin cuffs, which has been suggested as a physical barrier impeding the passage of oxygen. Iron deposition, white blood cell accumulation, decreased fibrinolytic activity, and a myriad of inflammatory responses to the vascular damage are all postulated to be the pathways leading to venous ulceration, but it is still not clear whether they are causative factors.
Tissue hypoxia appears to be a major underlying factor for venous ulceration. Unlike ulcers associated with arterial insufficiency, this hypoxic state is not caused by decreased blood flow to the legs; patients with venous insufficiency usually have adequate blood flow to their lower extremities. Direct measurements of transcutaneous oxygen levels on the lower portion of the leg have demonstrated that exercise produces a marked rise in skin oxygen tension in normal legs, but not in those affected by venous insufficiency. Exercise reduces venous pressure in patients with competent valves, thus removing the stimulus for reflex vasoconstriction. In patients with compromised valves, the venous pressure remains high during exercise and reflex vasoconstriction persists.
On the basis of these findings, it is clear that management of lower extremity ulcers caused by venous insufficiency must include measures that improve the abnormal venous blood return from the affected extremity. Leg elevation, compression therapy, local wound care, and surgical correction of selected underlying pathology are all important components of the treatment plan.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here