Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
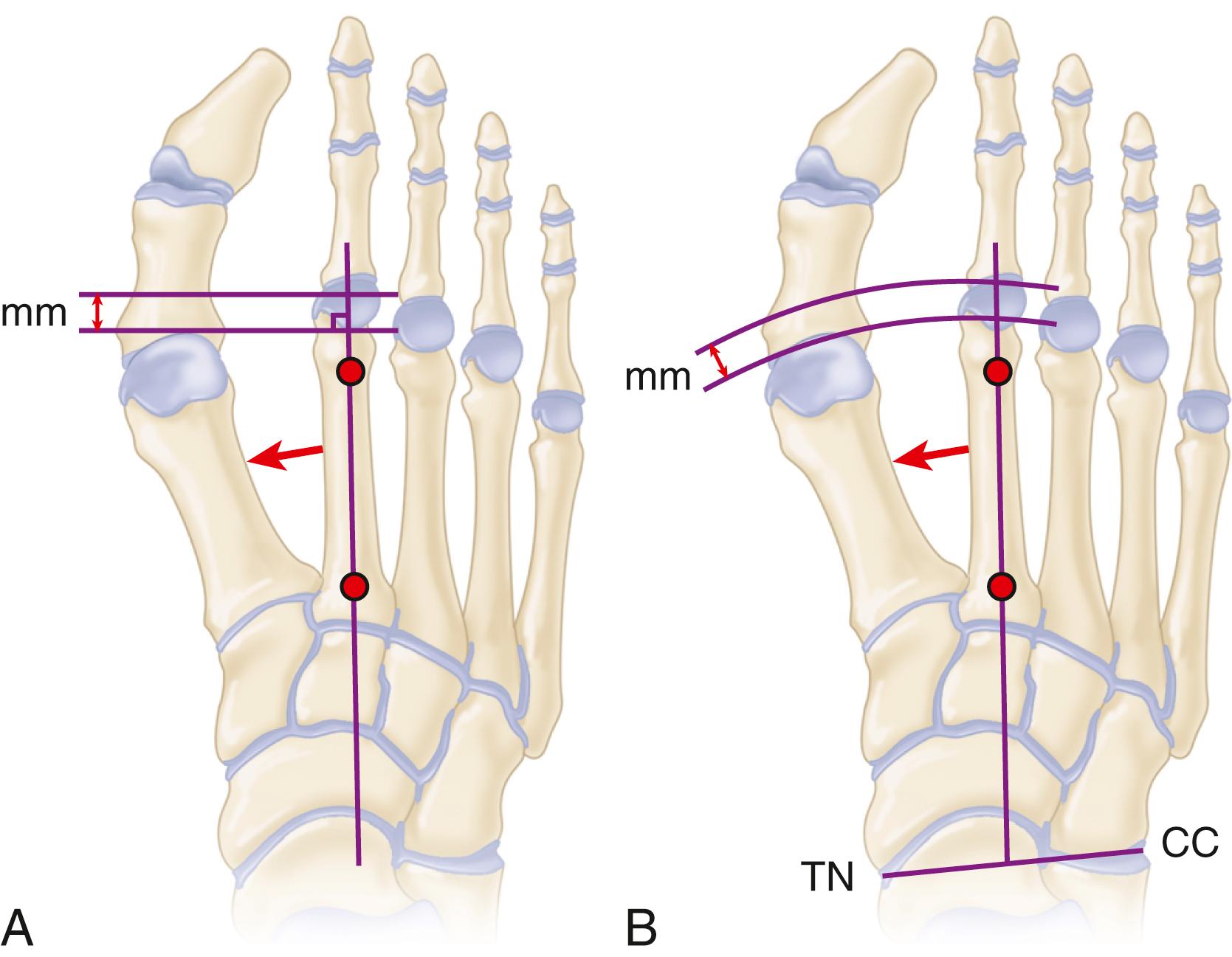
Deformity of the lesser toes, particularly of the second toe, sometimes is related to instability of the metatarsophalangeal joint. This disorder, which ranges in severity from synovitis of the metatarsophalangeal joint to dislocation and chronic deformity (hammer toe, claw toe, or crossover toe), has become a well-recognized problem. Lesser toe deformities are frequent in women older than the age of 50 years who wear constrictive high-heeled shoes and in athletes with chronic overuse and hyperextension of the toes. Coughlin’s extensive review of crossover toe deformity (which commonly involves some element of metatarsophalangeal synovitis) found the following associative factors: women older than age 50 years, hallux valgus, and degenerative changes in the first metatarsophalangeal joint. The most consistent physical finding was the presence of a positive drawer sign or Lachman test ( Fig. 84.1 ). Although the commonly held belief is that instability and synovitis are associated with an excessively long second metatarsal, this has been called into question. The traditional technique of measurement of second metatarsal length described by Morton involves a line drawn across the articular surfaces of metatarsals 1 and 3 ( Fig. 84.2A ). The Hardy and Clapham method ( Fig. 84.2B ) gives a different analysis of second metatarsal length. Weber et al., in a cadaver study evaluating the length of the second metatarsal, found a significant correlation between increased forefoot pressure and medial deviation of the second toe. Bhutta et al. found that a correlation between second metatarsal length as a causative factor and a metatarsophalangeal pathologic process depends largely on the method of measurement. This question is not a trivial one because the treatment decision often involves whether to shorten the metatarsal. Hallux valgus often is associated with metatarsophalangeal joint instability, but the most likely causes of instability are attritional changes in the lateral collateral ligament, capsule, and plantar plate. These changes more likely are caused by chronic synovitis and not by pressure from the deformity of the hallux. Other causes of instability include chronic synovitis from systemic arthritis, neuromuscular disease causing muscular imbalance, and acute traumatic disruptions of the plantar plate and collateral ligaments.

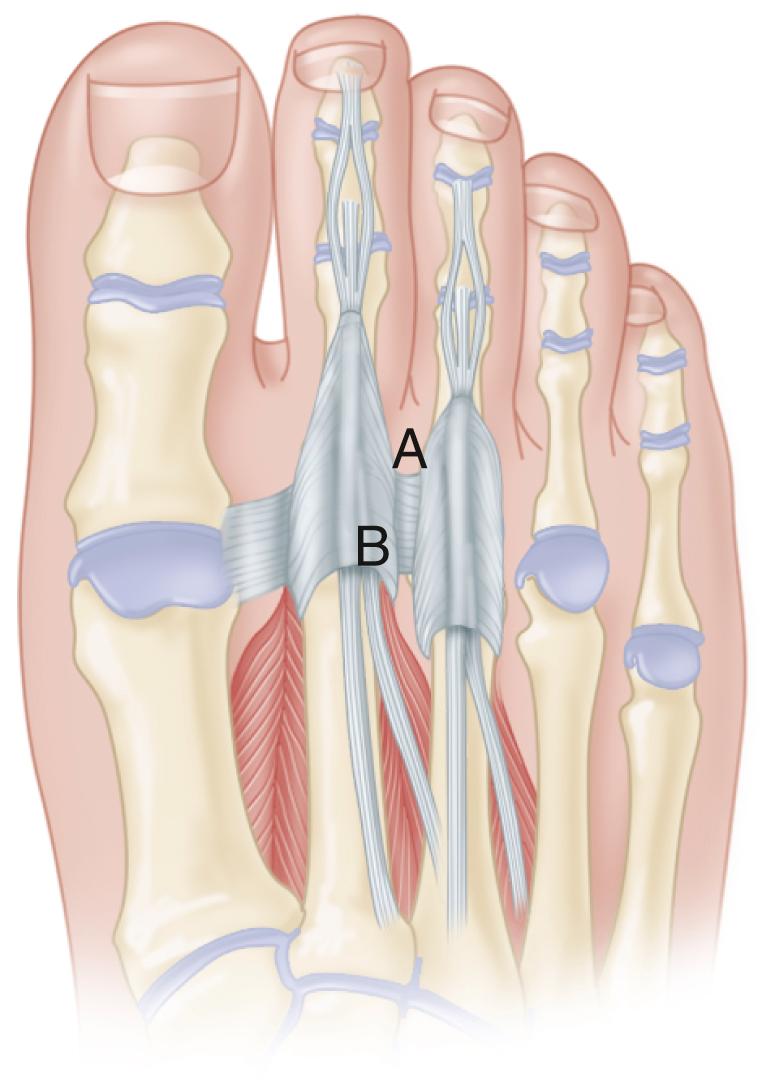
The most common site of synovitis, instability, and development of fixed toe deformity is the second metatarsophalangeal joint. Normal toe position depends on dynamic and static restraints. The most powerful extension force on the joint is delivered by the extensor digitorum longus tendon, which extends the metatarsophalangeal joint through a fibroaponeurotic sling that attaches plantarly to the plantar plate and capsule and suspends the phalanx ( Fig. 84.3 ). The extensor digitorum longus tendon is able to extend the interphalangeal joints of the toe only when the metatarsophalangeal joint is in a neutral or flexed position. If a toe is held in an extended position, such as in a high-heeled shoe, the extensor digitorum longus becomes a deforming force on the metatarsophalangeal joint.
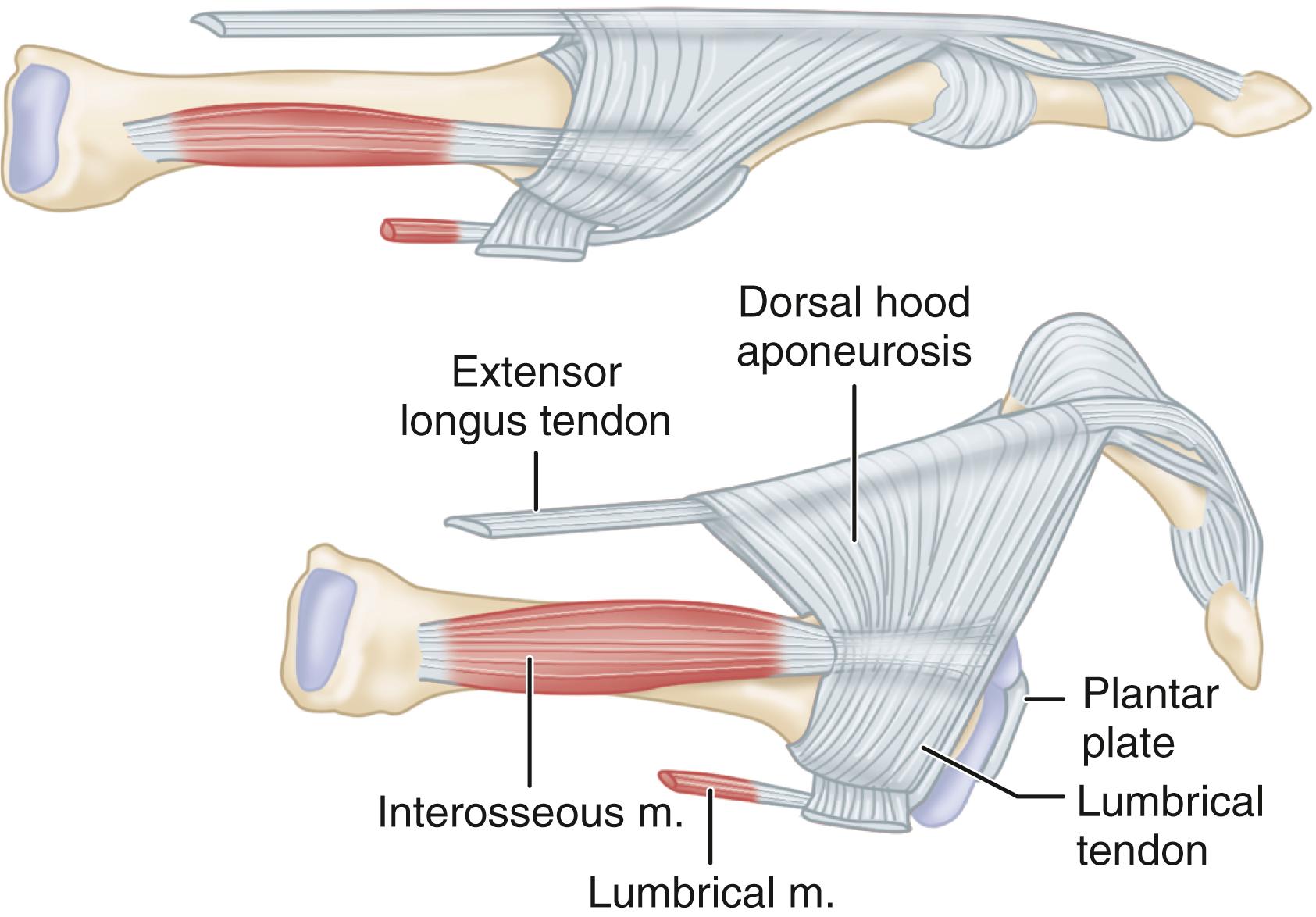
Flexion of the metatarsophalangeal joint primarily is a function of the intrinsic muscles. The second toe is unique in that there are two dorsal interossei and no plantar interossei. Normally, the axis of the pull of these muscles is plantar to the center of rotation of the metatarsophalangeal joint. As the metatarsophalangeal joint becomes chronically extended, however, the line of action moves dorsal to the center of rotation of the metatarsophalangeal joint, and these tendons become a deforming force for dorsal subluxation.
The lumbrical muscle is located on the medial side of the joint and axis and acts as an unopposed adductor of the toe. Although the lumbrical muscle normally passes plantar to the transverse intermetatarsal ligament and acts as a plantar flexor of the metatarsophalangeal joint, with chronic extension deformity it becomes ineffective as a plantar flexor.
Static restraints for joint stability include the collateral ligaments and the plantar plate, coupled with dynamic pull from the intrinsic muscles. The plantar plate, which originates partially as a thin synovial attachment in continuity with the periosteum of the metatarsal metaphysis, provides most of the stabilizing force. A firm fibrocartilaginous attachment inserts onto the base of the proximal phalanx adjacent to the articular cartilage. A cadaver study determined that the plantar plate is approximately 2 cm long, 1 cm wide, and 2 to 5 mm thick. The medial and lateral borders of the plate are thicker than the central portion, except for a broad thickened portion directly plantar to the metatarsal head.
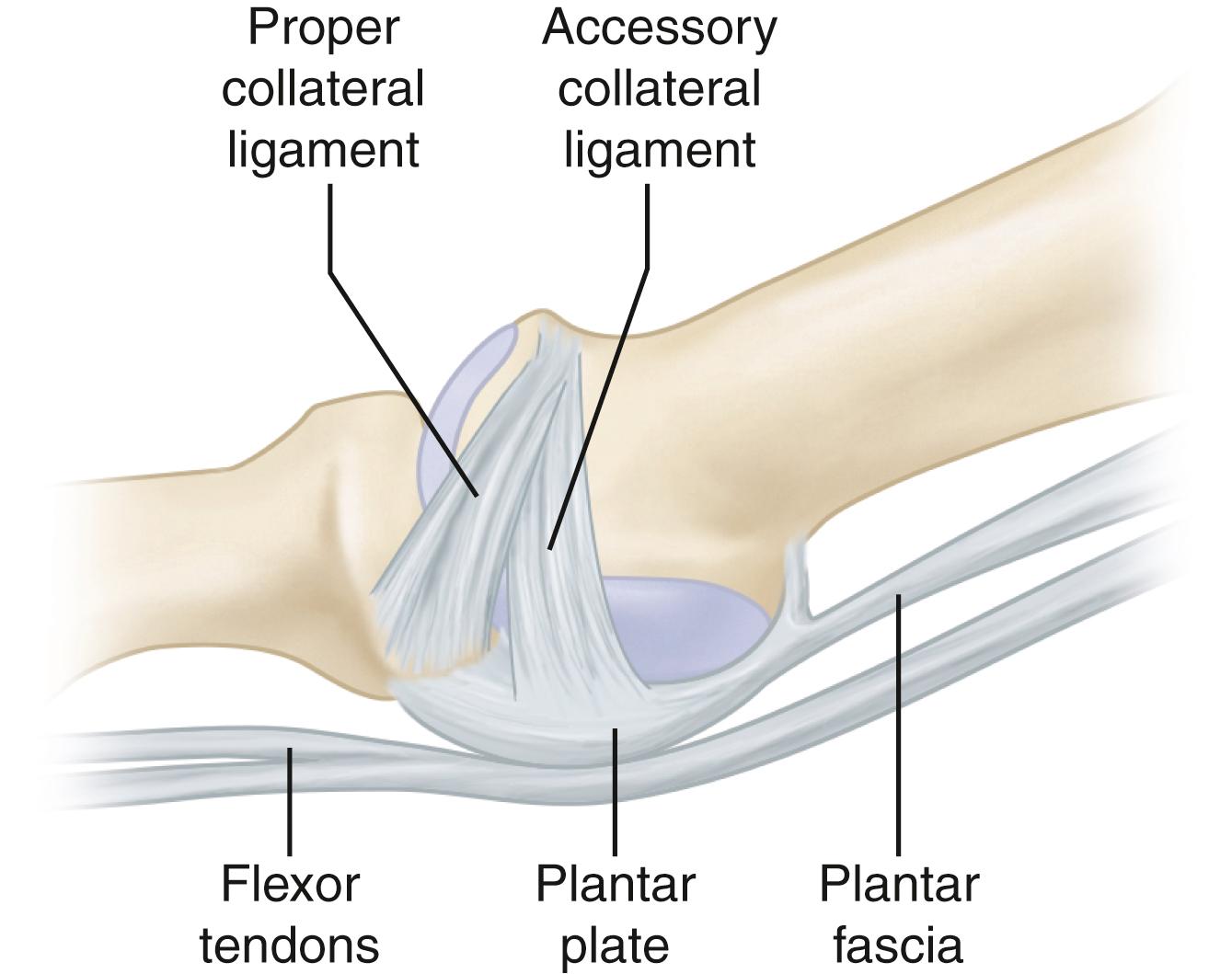
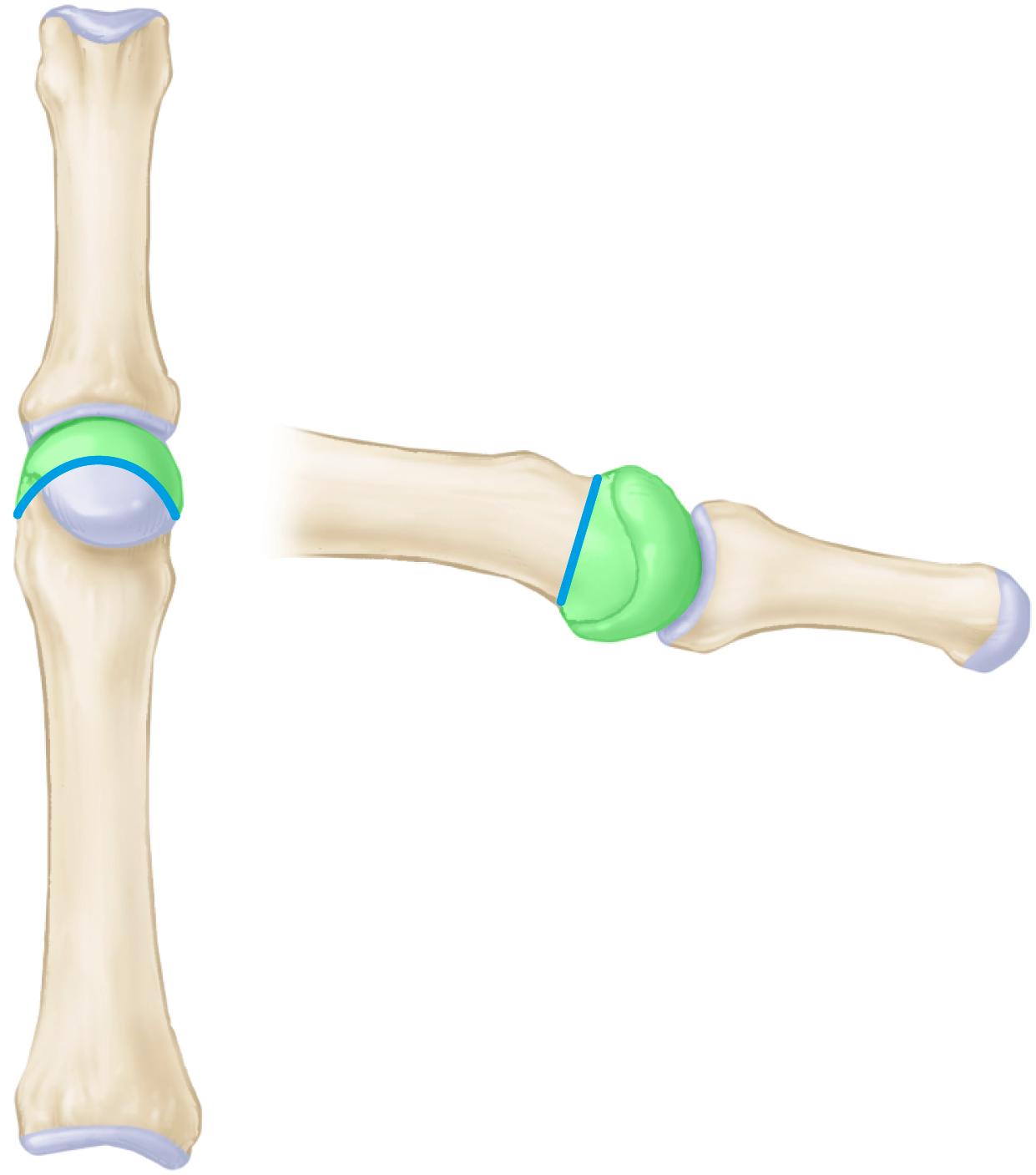
The plantar plate has a number of important attachments, including the collateral ligaments, the plantar fascia, the fibrous sheath of the flexor tendons, the interossei tendons, and the deep transverse metatarsal ligament. Several cadaver studies have evaluated the effects on joint stability of sectioning various structures around the lesser metatarsophalangeal joints. Reported contributions to dorsal translation stability for the plantar plate have ranged from 19% to 34% and for the collateral ligaments, 37% to 46%. Wang et al. found that bilateral sectioning of the deep transverse metatarsal ligament produced significant instability of the lesser metatarsophalangeal joints. Each of the collateral ligaments that insert onto the plantar plate has two distinct portions: the proper collateral ligament, which inserts at the base of the proximal phalanx, and the accessory collateral ligament, which inserts onto the plantar plate ( Fig. 84.4 ). Barg et al. found that insufficiency of the accessory collateral ligament leads to the most severe instability.
Chronic irritation of the joint and subsequent synovitis and joint effusion cause attritional degeneration, lengthening, and eventual rupture of these structures, especially the lateral collateral ligament and plantar plate, and subsequent instability. On the basis of their research and the research of other authors, Doty and Coughlin concluded that the plantar plate is the primary stabilizing structure that is the first to fail. The collateral ligaments also may fail in time, contributing to the transverse and sagittal plane malalignment of the toe.
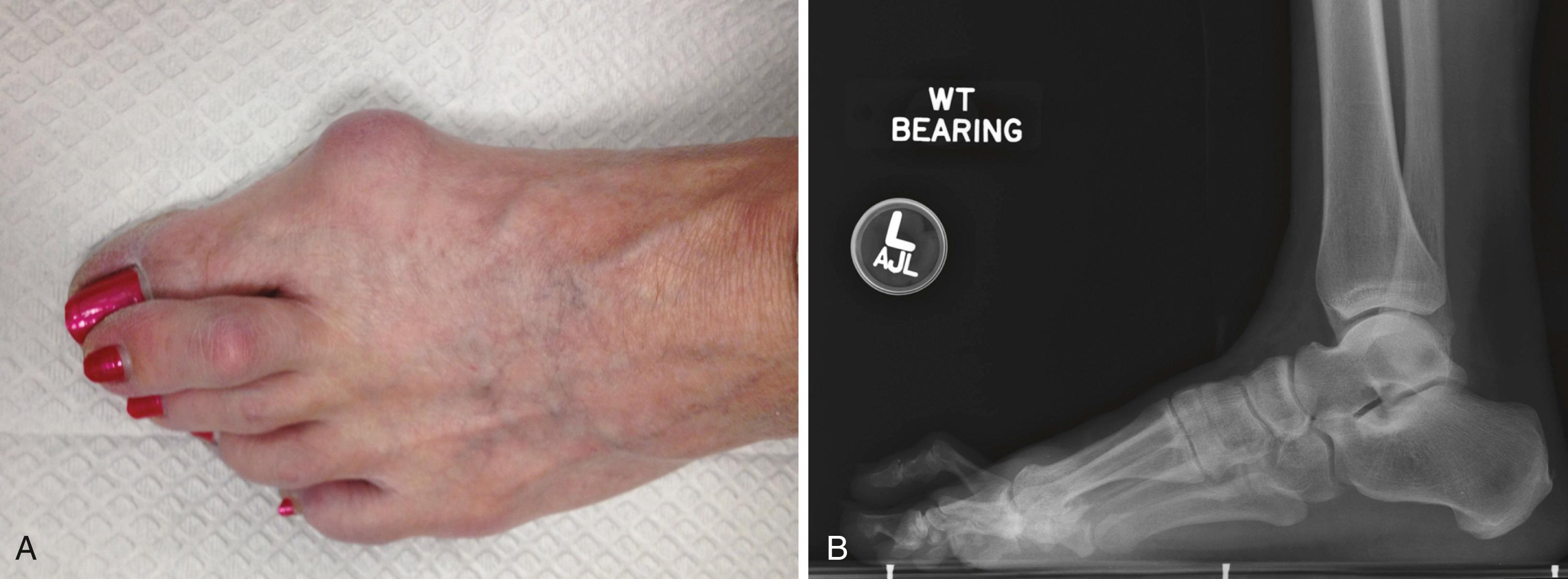
Patients with synovitis and instability of the metatarsophalangeal joint usually have an insidious, slowly progressive course of metatarsalgia, especially when wearing high-heeled shoes. Occasionally, neuritic symptoms may be present in the second web space, with radiation into the second and third toes. It must be emphasized that pain in this area is far more likely to be from the metatarsophalangeal joint than from an associated interdigital neuroma. Some patients, especially athletes, may remember an acute hyperextension injury to the foot that began the cycle of pain. Initially, pain occurs with weight bearing, but as the problem progresses, some patients have pain with rest. In the later stages of deformity, patients may have an antalgic gait pattern and compensate by shifting weight to the lateral column of the foot.
On examination, a hammer toe or crossover toe may or may not be present. Usually, some swelling of the joint manifests by the loss of contour of the long extensor tendon compared with the adjacent toes. Often a palpable effusion is present in the joint ( Fig. 84.5 ). Tenderness may be present in the dorsofibular side of the joint or the plantar plate directly beneath and just proximal to the metatarsal head. The Lachman (drawer) test is helpful in assessing dorsal-plantar instability (see Fig. 84.1 ). Limited motion of the joint usually is apparent, especially in flexion, compared with the contralateral toe. Clinical staging of instability defines the severity of the subluxation and is rated on a scale of 0 to 4 ( Table 84.1 ). Interestingly, Klein et al. found that a positive drawer test and deviation of the third metatarsophalangeal joint suggested a high-grade tear of the second metatarsophalangeal joint plantar plate ( Fig. 84.6 ).
| Stage | Alignment | Physical Examination |
|---|---|---|
| 0 | No malalignment, prodromal phase with pain | Joint pain, swelling, diminished toe purchase, negative drawer test |
| 1 | Mild malalignment, widening of the web space, medial deviation | Joint pain, swelling, diminished toe purchase, mildly positive drawer test (<50% subluxation) |
| 2 | Moderate malalignment; medial, lateral, or dorsal deformity; hyperextension | Joint pain, diminished swelling, no toe purchase, moderately positive drawer test (>50% subluxation) |
| 3 | Severe malalignment, dorsal deformity, toes may overlap, possible hammer toe | Joint and toe pain, little swelling, no toe purchase, dislocatable on drawer test |
| 4 | Severe malalignment, dislocation, fixed hammer toe | No toe purchase, dislocated toe |

The paper pull-out test can be used to evaluate toe strength and dynamic digital purchase on the ground. A narrow strip of paper is placed between the affected toe and the ground. The patient grasps the paper by plantarflexing the toe, resisting the examiner’s attempts to pull the paper from beneath the toe. The test is positive when the patient is unable to resist this pull.
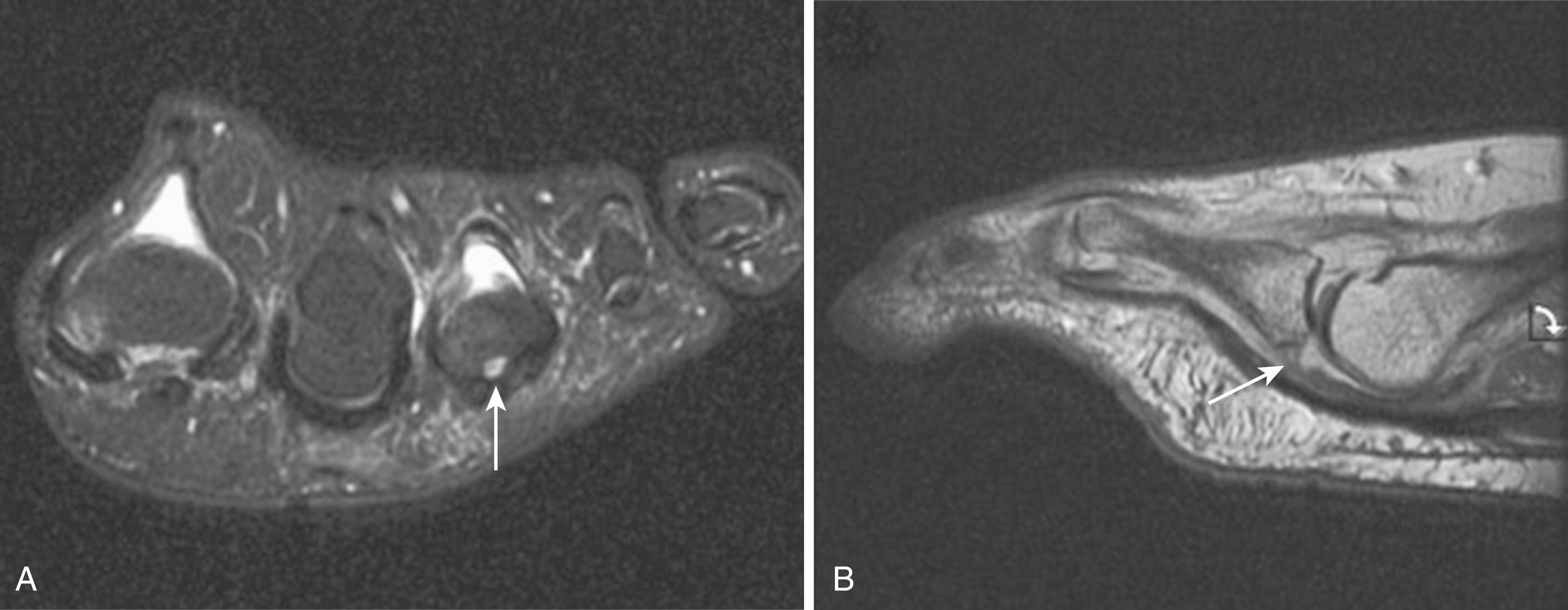
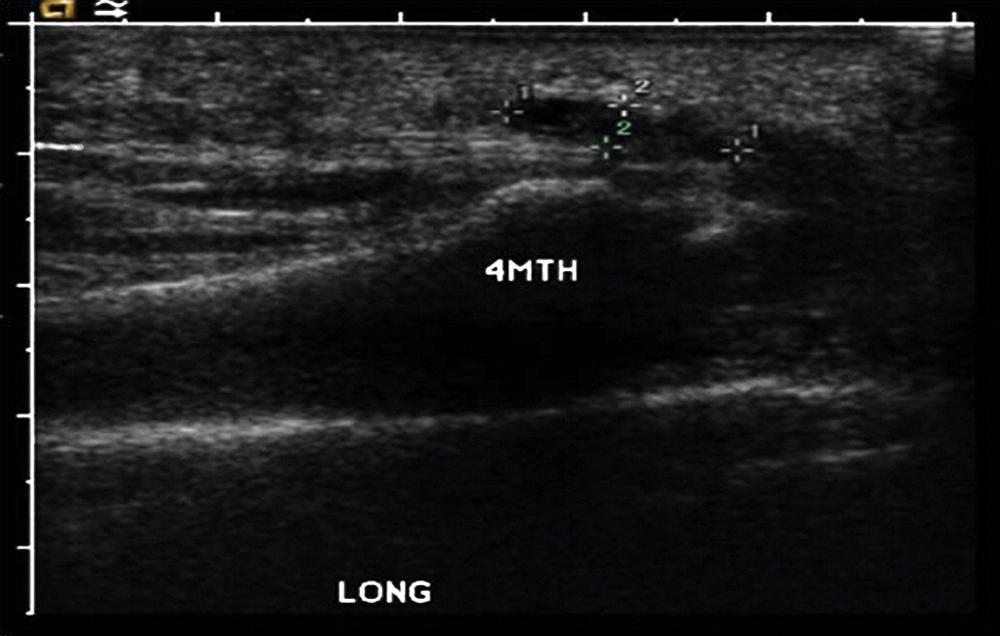
As deformity progresses, a plantar callus may develop. Although the diagnoses of metatarsophalangeal joint instability and plantar plate rupture are made primarily by clinical examination, MRI using a small receiver coil, as described by Yao et al., can be used for evaluation ( Fig. 84.7 ). Yamada et al. assessed direct and indirect MRI features related to plantar plate tears. They noted that when classic signs of a plantar plate tear could not be detected on MRI, indirect signs such as a pseudoneuroma sign, changes at the interosseous tendon-collateral ligament complex, and distance between the plantar plate and proximal phalanx were strongly associated with a tear. Ultrasound imaging has been found to have comparable sensitivity to MRI in the identification of lesser metatarsophalangeal joint plantar plate tears ( Fig. 84.8 ). Gregg et al. prospectively evaluated 160 patients with symptoms of plantar plate tears using ultrasonography and MRI; the sensitivity of MRI with surgical correlation was 87%, and ultrasound demonstrated a sensitivity of 96%. Feuerstein et al. found that, although both static and dynamic ultrasound techniques were highly sensitive, the sensitivity and accuracy of ultrasound examination were better with dynamic techniques.
In the early stages of synovitis when minimal deformity is present, a single intraarticular cortisone injection, oral antiinflammatory agents, metatarsal supports, taping of the toe in a neutral position, and use of stiff-soled shoes may eliminate pain and prevent deformity. The addition of a spring steel plate to the orthosis or directly to the sole of the shoe may help to eliminate extension forces on the toe. Peck et al., in a study of 154 patients with lesser metatarsophalangeal joint instability, found that 64% were managed nonoperatively with these methods and 36% were managed operatively with a combination of a flexor-to-extensor transfer, a Weil osteotomy, and a Stainsby procedure (which involved removal of the base of the proximal phalanx). They reported no significant difference in improvement between patients treated operatively and those treated nonoperatively. When significant deformity or instability is present, however, conservative treatment may be insufficient.
For chronic synovitis of the joint that is unresponsive to conservative treatment when no significant instability is present, extensor longus lengthening, dorsal capsulotomy, and synovectomy are indicated. Very occasionally, a second web space neuroma is present and should be resected if preoperative symptoms suggest neuritic pain.
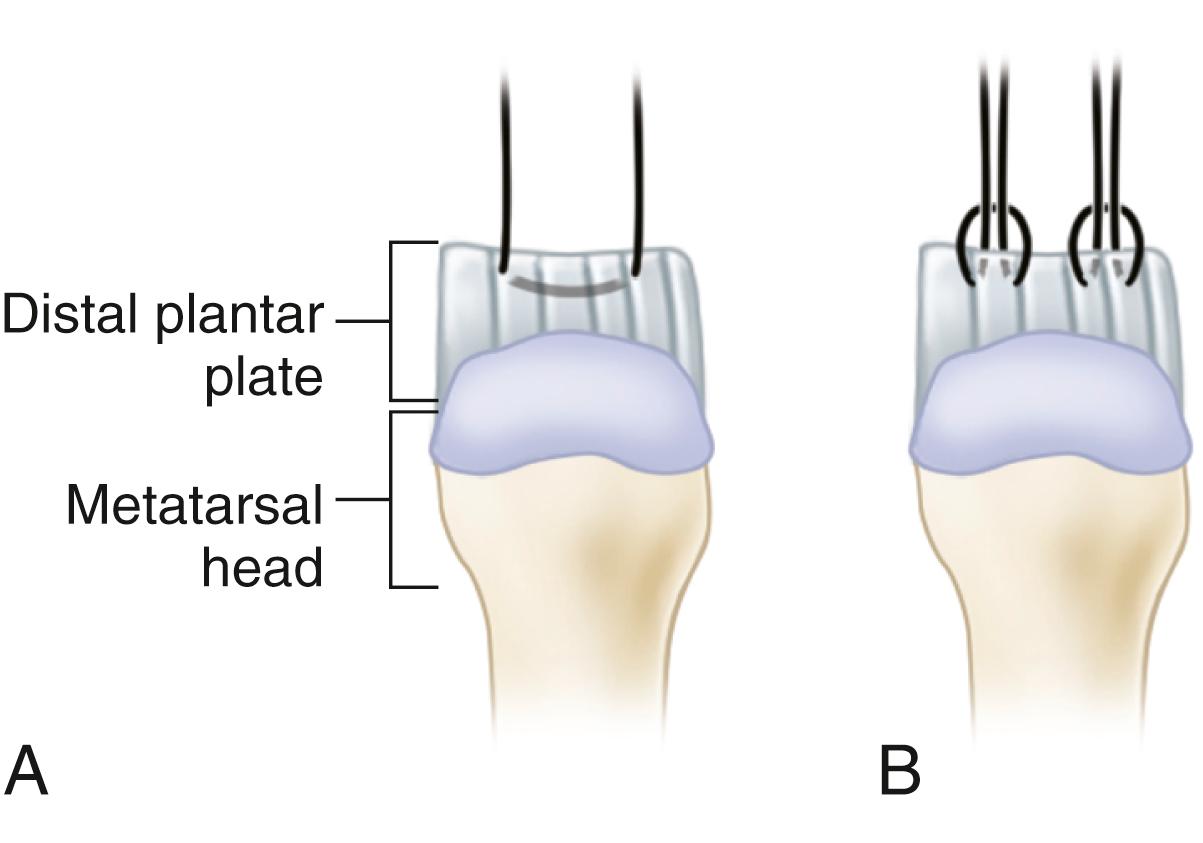
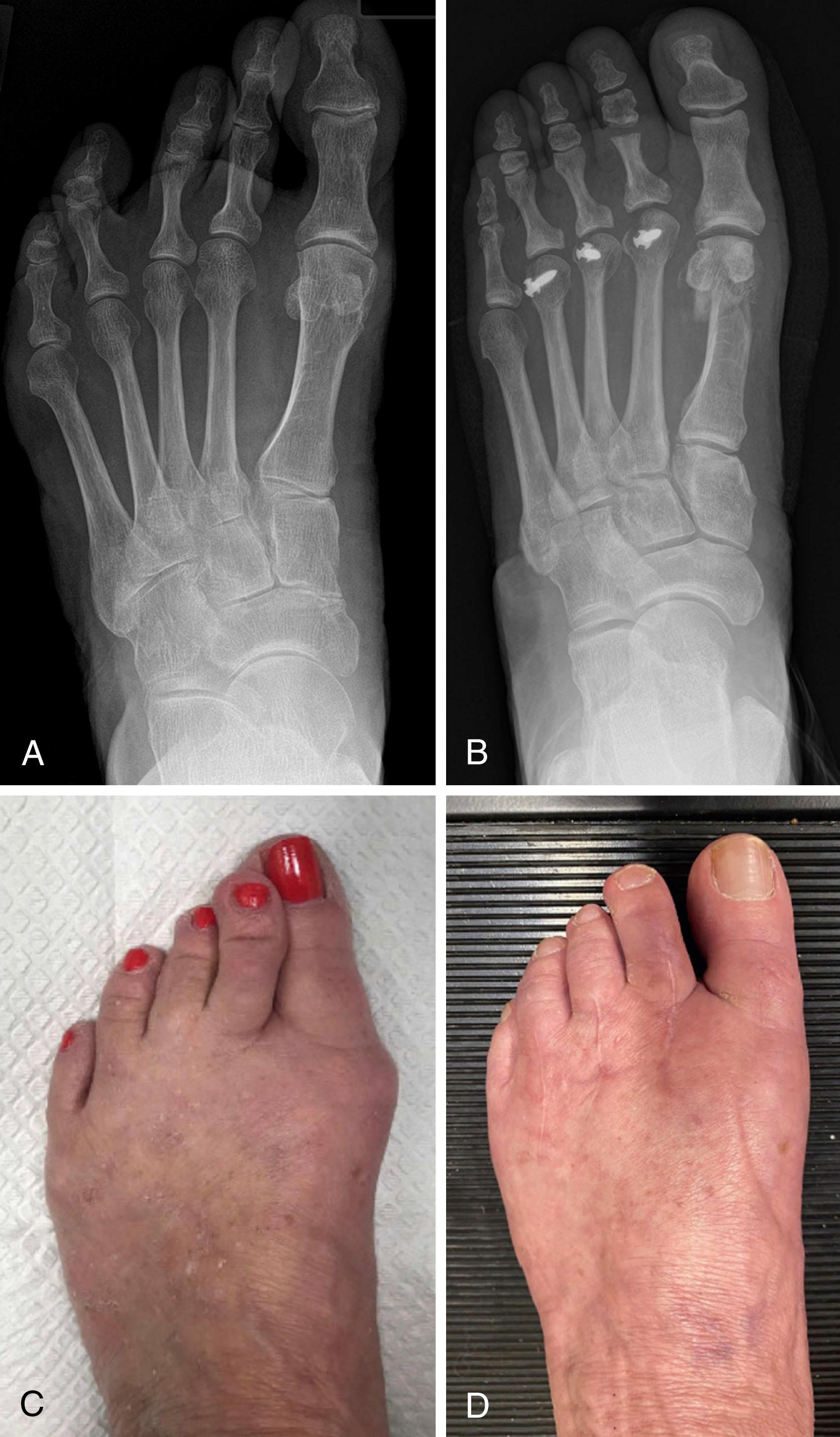
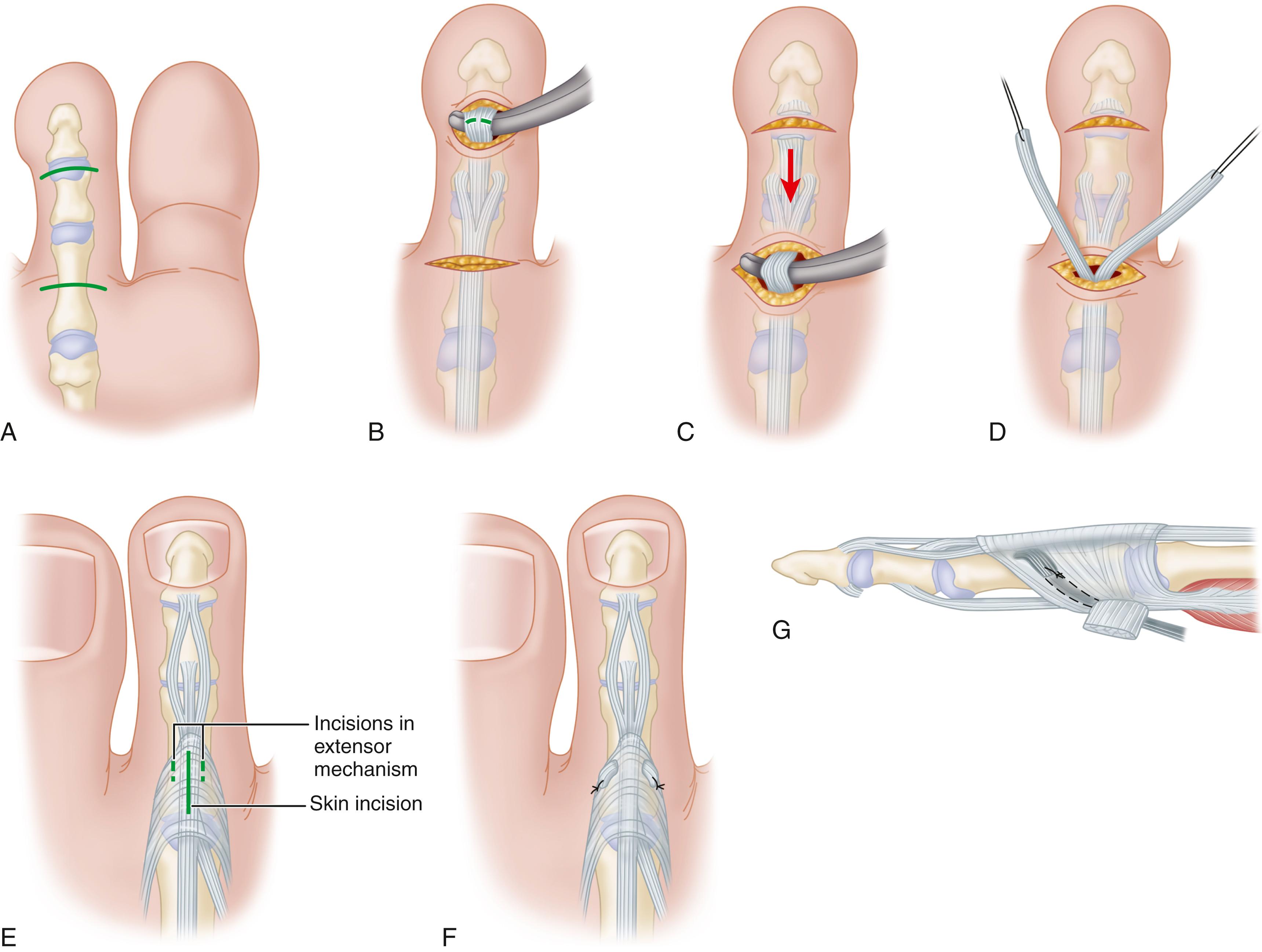
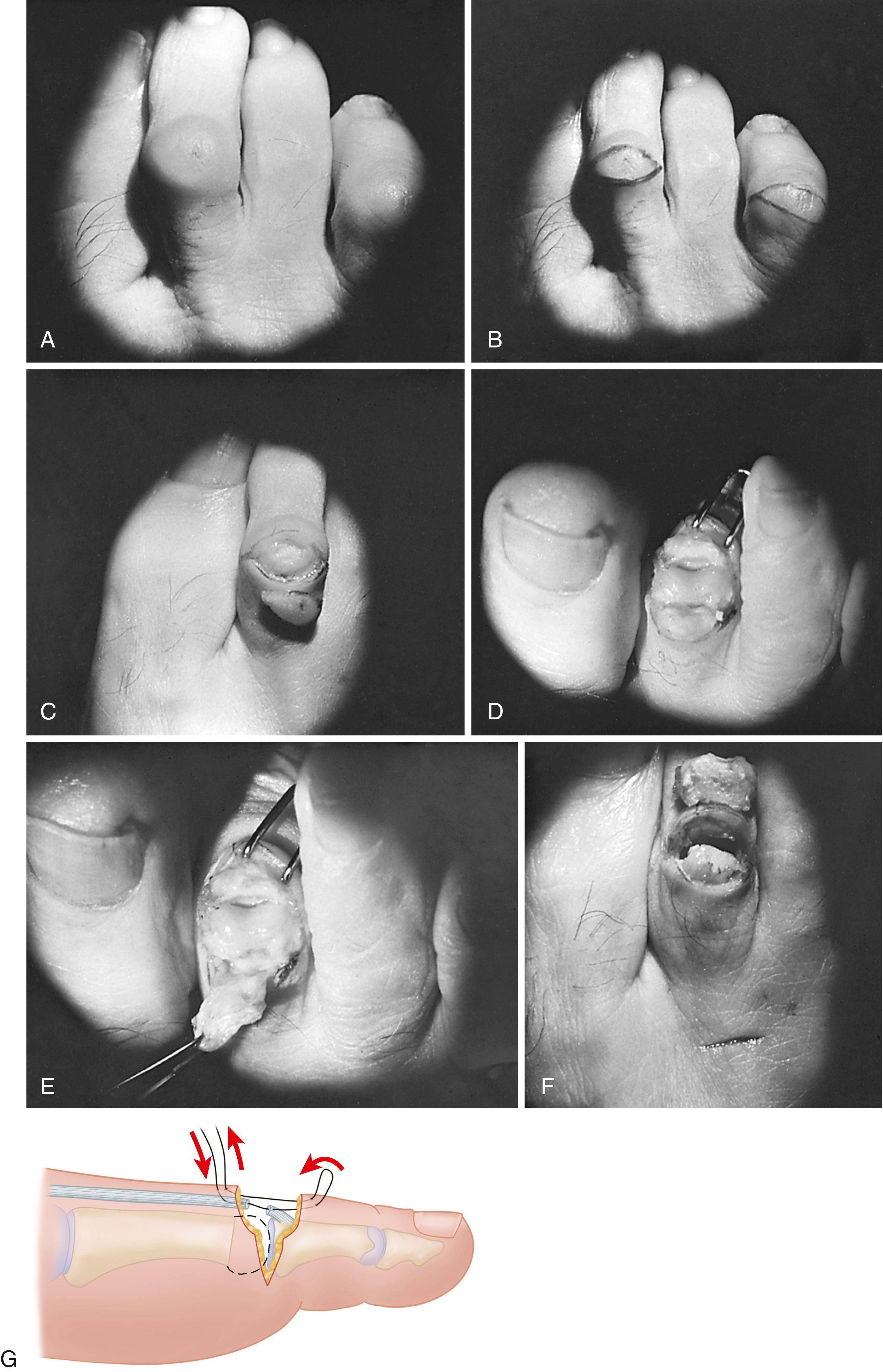
If the joint subluxates more than 50%, a stabilizing procedure should be added to the synovectomy. Attritional rupture of the plantar plate has been reported to occur primarily at the attachment on the plantar aspect of the proximal phalanx. Direct repair of the plantar plate to the base of the proximal phalanx using a plantar approach to the metatarsophalangeal joint has been reported, but no long-term outcome studies are available. Plantar plate repair through a dorsal approach is now our preferred treatment method for this condition, as it has been found to anatomically restore ligamentous support in the lesser metatarsophalangeal joints. Although tedious, it can be accomplished with correction of the primary problem: disruption of all or a portion of the plantar plate. Flint et al. in a prospective case series of 138 plantar plate tears reported 80% good to excellent satisfaction scores after dorsal plantar plate repair. Devices are now available that significantly improve the technique, making it faster and easier to perform. Two suture configurations generally are used in the dorsal approach, the horizontal mattress stitch or a luggage-tag stitch ( Fig. 84.9 ). In a biomechanical cadaver study, Finney et al. found the horizontal mattress stitch to be a superior configuration to the luggage-tag stitch, trending toward a higher load-to-failure force.
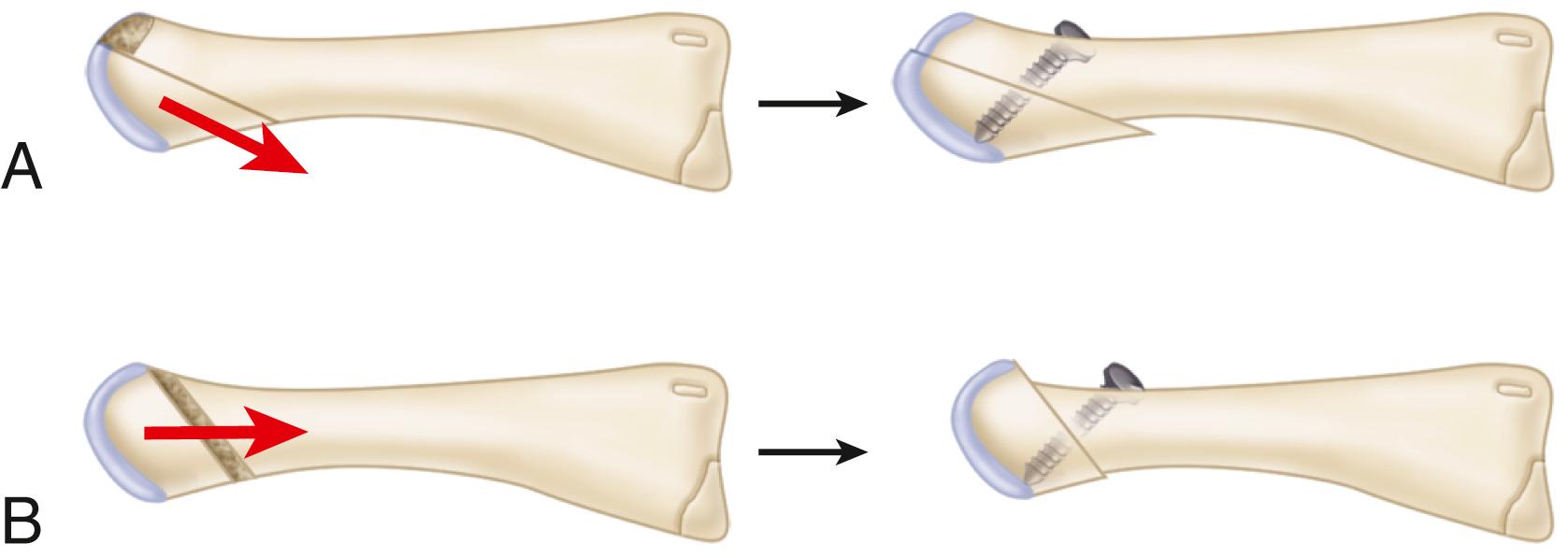
Although we believe that in most patients a Weil osteotomy is important, Saltzman has described a technique that does not call for the routine use of the osteotomy. The Weil shortening osteotomy corrects what is often the underlying problem, excessive metatarsal length, but also significantly improves visualization of the plantar plate. It is important not to overshorten the second metatarsal, because this will limit the ability to obtain tension on the repair. Removing a small slice of bone from the osteotomy and then restoring most of the length usually is sufficient to decompress the joint. Flexor-to-extensor transfer is still a very useful technique, especially in severe dislocations where there is little remaining plantar plate for repair. Garg et al. described a modification of the Weil osteotomy, a “segmental” osteotomy ( Fig. 84.10 ), that effectively shortens the metatarsal and reduces the plantar load under the metatarsal head. Although technically easier than the Weil osteotomy, the segmental osteotomy had frequent complications, including transfer metatarsalgia, floating toe, infection, and wound healing problems.
Flexor-to-extensor transfer or rerouting of the extensor digitorum brevis tendon underneath the second intermetatarsal ligament has been reported to be effective in the treatment of crossover second toe deformity, as has transfer of the flexor digitorum longus. Myerson and Jung reported combining flexor digitorum longus tendon transfer with proximal interphalangeal resection arthroplasty, proximal interphalangeal fusion, and/or Weil osteotomy of the metatarsal. Although many patients were pleased with the pain relief obtained, frequent complications, such as residual extension contractures at the metatarsophalangeal joint, medial deviation of the joint, and stiffness of the toe, resulted in 14% of patients being dissatisfied with the procedure. It cannot be emphasized enough that with lesser toe surgery, preoperative counseling regarding patient expectations is mandatory.
Percutaneous distal metatarsal osteotomies without soft-tissue procedures have been described for treatment of mild to moderate metatarsophalangeal joint instability with comparable results to open procedures. Authors cite as advantages reduced operating times and lower rates of complications (2.9% metatarsalgia) compared with traditional open techniques. However, delayed and nonunions have been reported, as well as the potential for injury to the metatarsal epiphyseal blood supply.
Although direct repair of a plantar plate detachment can be technically challenging, it can provide stability to the joint. Cooper and Coughlin described an approach for adequate exposure of the plantar plate, and Gregg et al. reported the results of plantar plate repair combined with Weil osteotomy.
Make a dorsal incision over the related interspace and a longitudinal capsulotomy at the affected metatarsophalangeal joint.
Divide the extensor digitorum brevis and make a Z-tenotomy of the extensor digitorum longus.
After full collateral release of the metatarsophalangeal joint, use a microsagittal saw to remove a small wedge of bone.
Provisionally fix the toe in a maximally shortened position with a 1.2-mm Kirschner wire.
Pull on the toe to expose the plantar plate.
If the plantar plate is partially or completely detached from the base of the proximal phalanx, freshen the plantar rim of the proximal phalanx.
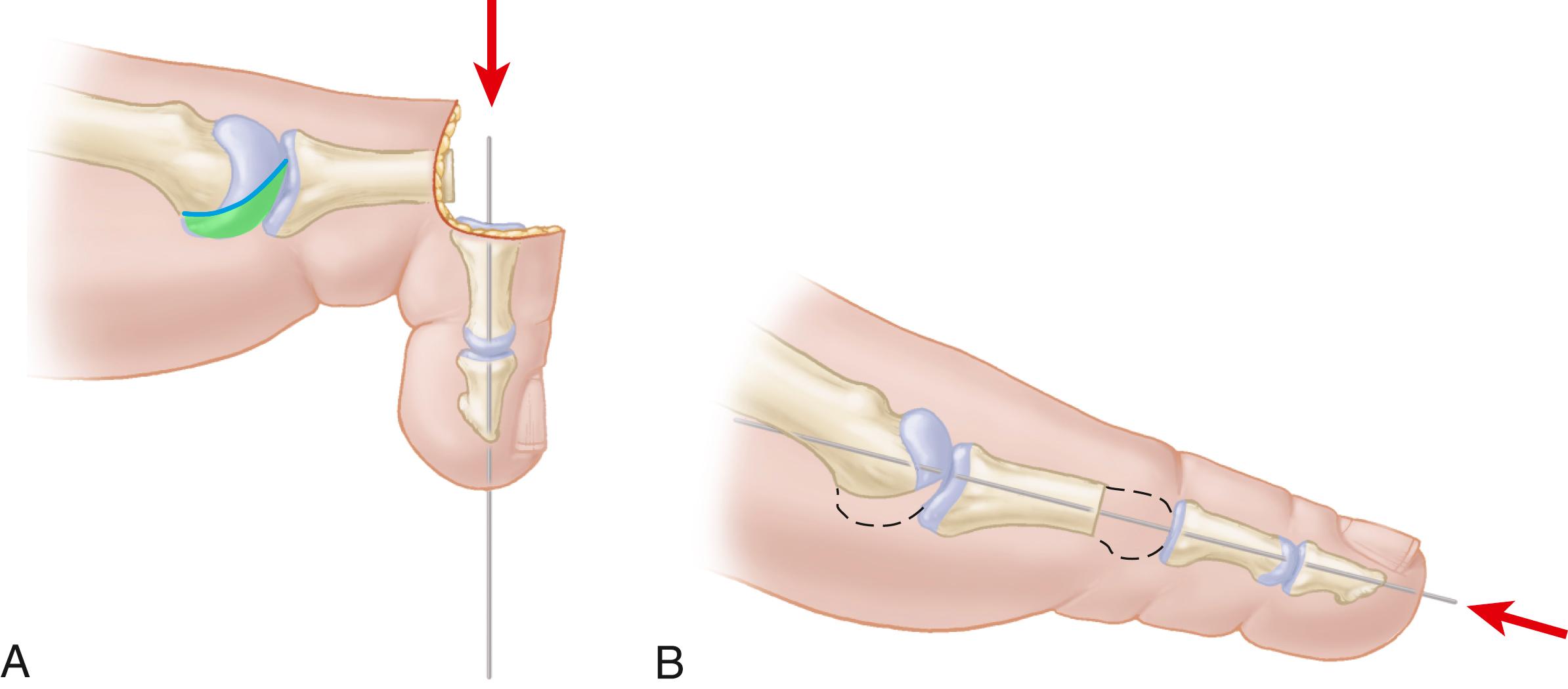
With a 1.6-mm Kirschner wire, drill two holes from the dorsal cortex to the plantar rim of the proximal phalanx, medially and laterally ( Fig. 84.11A ).
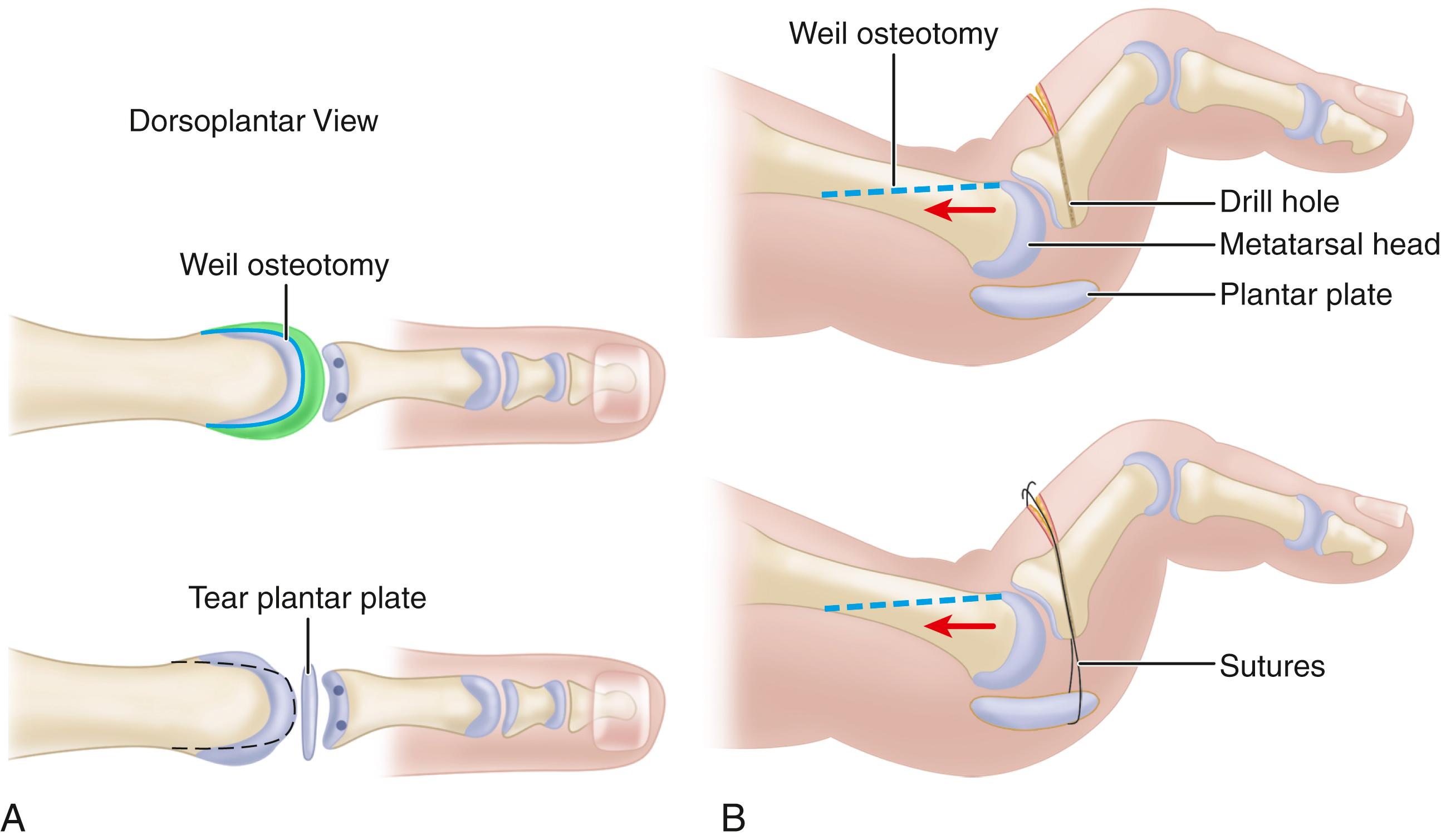
Pass a {1/10} Ethibond suture across the plantar plate proximal to the disruption and back through the holes in the proximal phalanx ( Fig. 84.11B ).
Fix the Weil osteotomy in optimal position with a 1.3-mm titanium “twist-off” screw (DePuy/Johnson & Johnson, Leeds, UK).
Tie the two suture ends over the dorsal phalangeal cortex to advance the plantar plate onto the base of the proximal phalanx.
Pass a 1.6-mm Kirschner wire through the toe and across the metatarsophalangeal joint, holding the toe in a neutral position.
The foot is kept elevated. The wound is inspected at 7 to 10 days. Weight bearing is allowed in a multipurpose medical/surgical shoe for the first 6 weeks after surgery. The Kirschner wire is removed at 4 weeks.
(COUGHLIN)
Place the patient supine on the operating table; place and inflate a tourniquet.
Make a dorsal longitudinal incision just inferior to the tendons of the extensor digitorum longus and brevis to expose the affected second metatarsophalangeal joint.
Partially release the collateral ligament off of the proximal phalanx of the metatarsophalangeal joint to improve exposure.
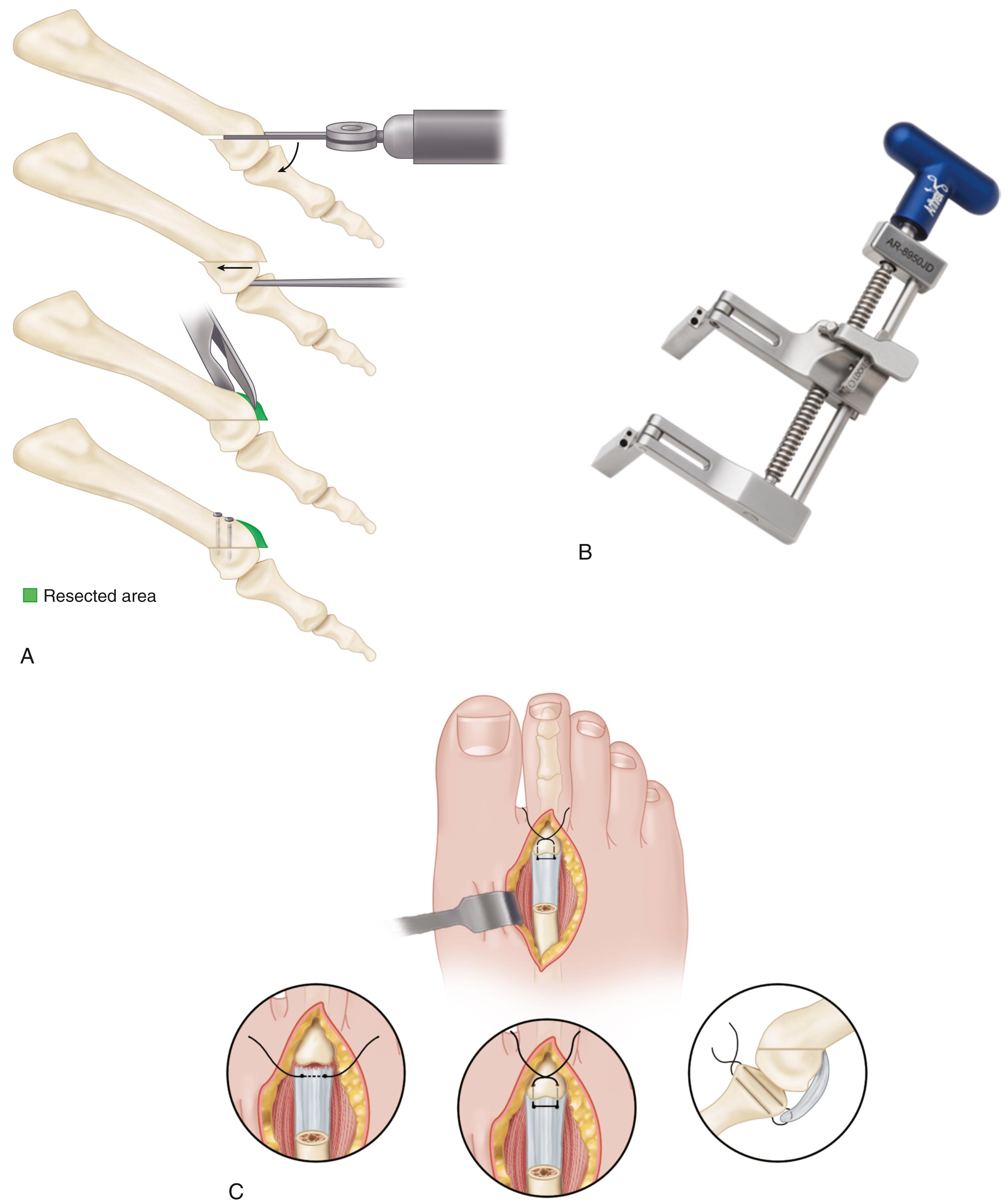
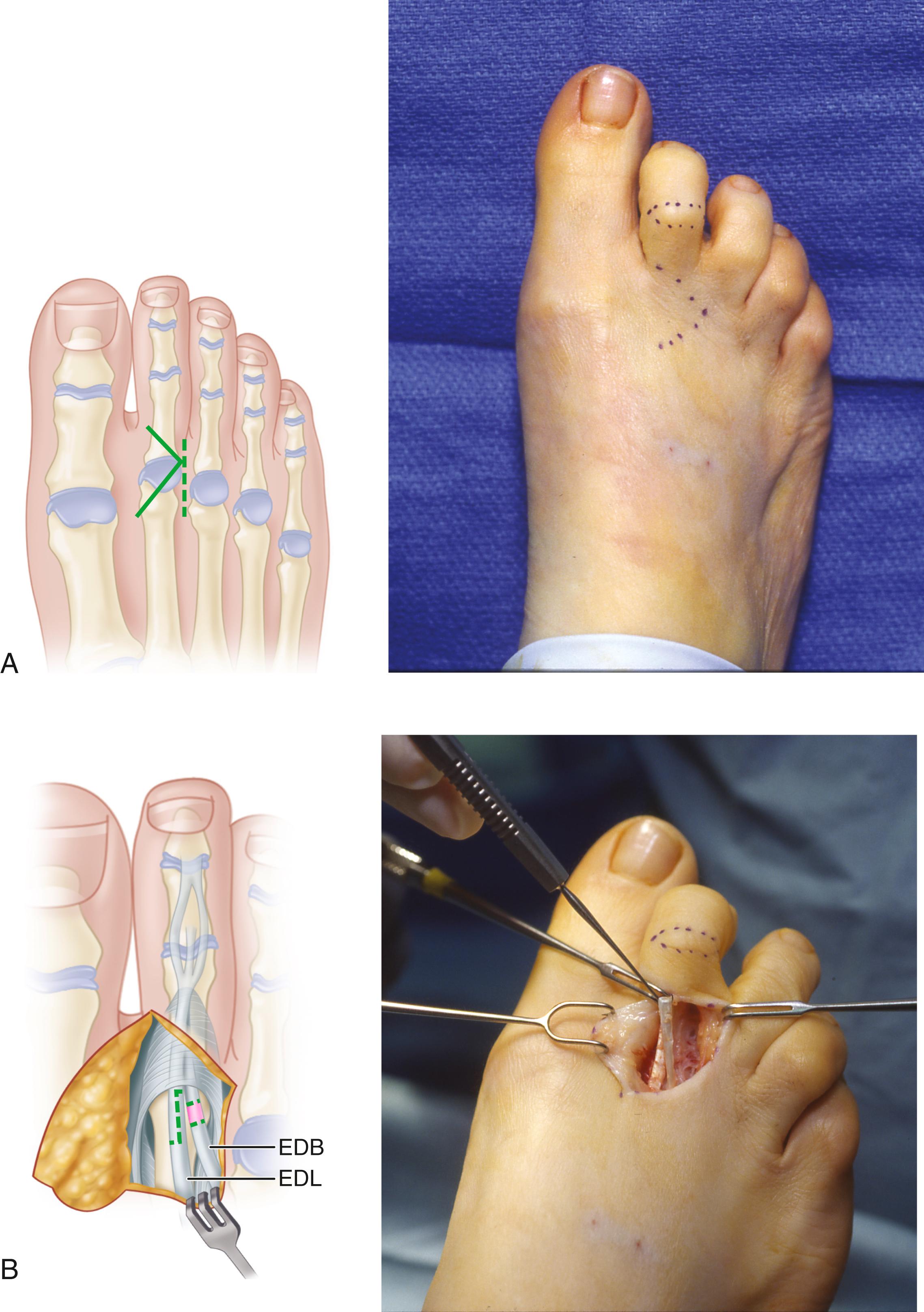
Use a sagittal saw to make a Weil osteotomy ( Fig. 84.12A ). Make the cut parallel to the plantar aspect of the foot, starting at a point 2 to 3 mm below the top of the metatarsal articular surface.
Push the capital fragment proximally about 10 mm and fix it with a temporary vertical Kirschner wire to hold it in a retracted position.
Place a second vertical Kirschner wire in the base of the proximal phalanx. Place a special miniature joint distractor (Arthrex, Inc., Naples, FL) over the vertical wires and spread them to expose the plantar plate ( Fig. 84.12B ).
Evaluate and grade the plantar plate.
Repair longitudinal tears (grade 3) with a side-to-side interrupted nonabsorbable suture.
Repair transverse tears (grades 1 and 2) by placing nonabsorbable suture in the distal plantar plate. Roughen the distal plantar edge of the proximal phalanx with a burr or curet to prepare a surface for reimplantation of the plantar plate.
Transfix the distal plantar plate just proximal to the transverse tear using a small curved needle or special curved Micro SutureLasso (Arthrex, Inc., Naples, FL) or suture punch (Mini Scorpion, Arthrex) to pass the suture within the restricted metatarsophalangeal joint surgical area of exposure.
Use a 1.6-mm drill to create two parallel holes medially and laterally on the proximal phalanx, directed from the dorsal cortex of the proximal phalanx to its plantar rim. This allows passage of a suture, plantar to dorsal, to fix the plantar plate to its insertion point at the plantar base of the phalanx ( Fig. 84.12C ).
Reduce the Weil osteotomy, shortening the toe only 1 to 2 mm. Fix the toe in optimal position with one or two small compression screws.
Hold the toe reduced on the metatarsal articular surface, in 15 degrees of plantarflexion and with tension on the sutures, which have been pulled through the holes in the proximal phalanx. Tie the sutures over the dorsal phalangeal cortex, advancing the plantar plate onto the base of the proximal phalanx.
Perform a lateral soft-tissue reefing with 2-0 nonabsorbable sutures to repair the lateral collateral ligament release.
Close the wound in usual fashion and apply a gauze-and-tape compression dressing with the toe held in 10 to 15 degrees of plantarflexion.
The dressing is changed at 1 and 2 weeks after surgery and then discontinued. The foot is placed in a compression wrap with a dynamic toe exercise strap. Ambulation is allowed in a postoperative shoe with weight bearing only on the heel. Comfortable shoes are permitted at 6 weeks after surgery. Passive and active range-of-motion exercises are begun at 2 weeks to recondition the short and long flexors and extensors of the lesser toes.
This minimally invasive distal osteotomy of the lateral metatarsal bones without a soft-tissue procedure has been used for treatment of biomechanical metatarsalgia and metatarsophalangeal joint instability when the involved joint is still reducible and there is no structural toe deformity. The advantages of this technique include being simple, not requiring a fixation device or immobilization, and it can be done with an ankle block. Although there is the potential for nonunion, osteonecrosis of the metatarsal head, and infection, none of these occurred in a study by Magnan et al. This technique is not recommended in stiff, Coughlin grade III metatarsophalangeal joint dislocations.
(MAGNAN ET AL)
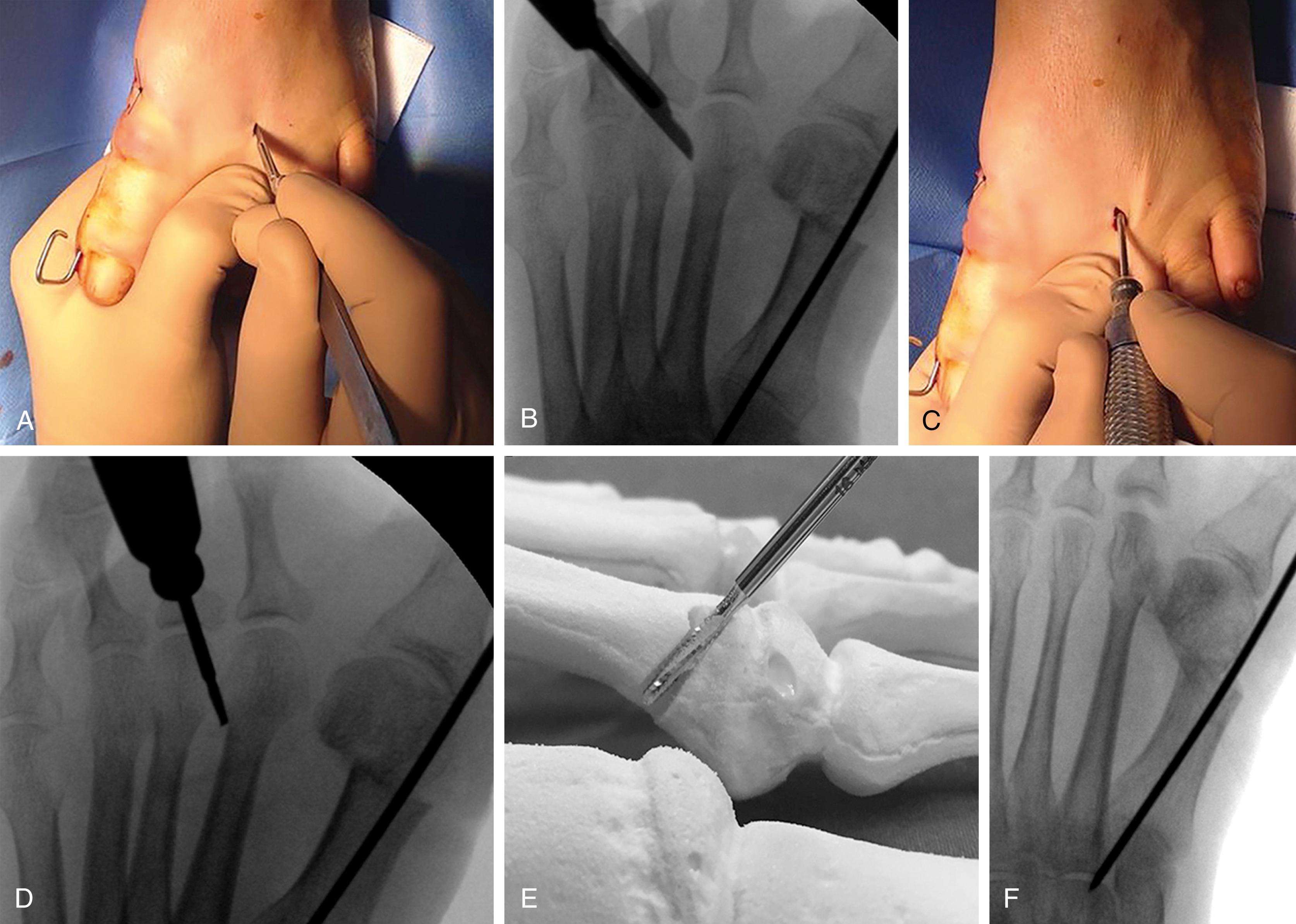
After ankle block anesthesia is administered, make a short skin incision on the dorsum of the distal metatarsal metaphysis close to the metatarsal head ( Fig. 84.13A, B ).
With a scissor inserted through the small incision, detach the periosteum at the site of the osteotomy.
Using a 2.3-mm micromotorized bone cutter, perform the osteotomy in a single plane 45 degrees from dorsal to plantar and distal to proximal on the metatarsal axis, moving down the lateral cortex of the metatarsal neck proximal to the metatarsal head ( Fig. 84.13C–F ).
Manually mobilize the toe and metatarsal head to check that the osteotomy is complete and to release all periosteal attachments that may hinder shortening and raising the distal metatarsal fragment.
An adhesive bandage is used to keep the toes aligned with flexion of the metatarsophalangeal joint and is changed every week for 6 weeks. Immediate full weight bearing is allowed 1 day postoperatively in a postoperative shoe with a flat, rigid sole. Normal shoes are allowed after 4 weeks, and exercise of the joint is encouraged.
One of the more challenging deformities of the forefoot is the medially or laterally deviated toe. Medial deviation is most often seen in crossover toe deformities, with or without associated hallux valgus, and sometimes involves multiple toes, not just the second. The valgus second toe deformity also may be associated with hallux valgus and also may involve multiple toes. In both cases, attention to the lesser toe deformity is critical because failure to correct this may lead to recurrence of the hallux deformity.
In the mildest cases of either varus or valgus deformity, simple release of the contracted collateral ligament may be all that is necessary. Imbrication of the opposite side may provide an additional measure of correction. For varus deformity, satisfactory results have been reported with the use of the extensor digitorum brevis tendon rerouted underneath the transverse metatarsal ligament. It is important to note that a competent intermetatarsal ligament is a prerequisite for this procedure. Ellis et al. described an extensor digitorum brevis reconstructive technique combined with a medial collateral ligament and partial plantar plate release for correction of multiplanar deformity of the second metatarsophalangeal joint. Also, while a shortening osteotomy of the metatarsal may be necessary to correct the deformity and instability of the metatarsophalangeal joint, this osteotomy will prevent the use of the extensor digitorum brevis transfer.
Klinge et al. described a modification of the Weil osteotomy to address this issue, and we have found it to be particularly successful and powerful in procedures involving varus or valgus angulation of the toe not corrected with simple ligament balancing. It is our preferred procedure of the following three, but we still find it useful to be familiar with a number of techniques to deal with this challenging problem. As a technical tip, when managing complex forefoot deformity, it can be useful to use a proximal thigh tourniquet and general anesthesia so that the ankle tourniquet does not produce tension on the long extensor and flexor tendons to the toe while attempting to balance alignment of the toe.
Finally, the complexity of this problem gives rise to the question of whether a simple arthrodesis might suffice in patients with more severe or recurrent deformities. Although we have no experience with this procedure, Joseph et al. reported a statistically significant reduction in pain, improvement in alignment, and full return to unrestricted weight-bearing activities in 31 patients with metatarsophalangeal joint fusions. Complications were, however, relatively frequent: 13% with nonunions, 6% with implant breakage, and 3% with soft-tissue infection.
(KLINGE ET AL.)
First, restore first ray alignment with either a modified McBride procedure (see Technique 82.1) or a transarticular soft-tissue release, followed by a chevron or scarf osteotomy (see Techniques 82.3 and 82.11). If needed to correct residual hallux valgus interphalangeus, an Akin procedure (see Technique 82.15) can be done.
To ameliorate extensor overrecruitment and extrinsic-intrinsic imbalance (tightness), transect the long extensor to the second ray proximally and cut the short extensor distally, just proximal to its insertion.
Perform a complete medial or lateral capsular and collateral ligament release to the level of, but not including, the plantar plate for varus or valgus deformities, respectively.
If residual metatarsophalangeal joint contracture remains, perform a modified Weil three-step shortening osteotomy (see Technique 84.12) to further decompress the joint, allow congruent reduction, and restore dorsal-plantar competence.
If adjacent lesser rays remain malaligned or of an inappropriate length, similar procedures should be done on them.
For persistent coronal plane metatarsophalangeal joint drift and malalignment, obtain more anatomic realignment by displacing the metatarsal head in the coronal plane before fixation.
Use a dental pick, anteater rongeur, or Freer elevator to adjust and maintain proper metatarsal head position while coronal plane alignment is checked clinically and radiographically. Make coronal plane adjustments as necessary.
For fixation, place a single 2-mm solid cortical screw in lag fashion across the osteotomy site after satisfactory reduction. Slightly offset the screw trajectory from the pure sagittal plane in the direction of translation to maximize central purchase within the metatarsal head. Take care to ensure that the metatarsal head shift resulted in a purely translational rather than an angular (coronal plane) realignment, making adjustments as necessary before fixation until the final metatarsophalangeal joint alignment is deemed anatomically congruent.
Evaluate the foot clinically and with fluoroscopy to ensure satisfactory alignment of the metatarsals and congruent reduction of the metatarsophalangeal joints.
When bony realignment is completed, transfer the short extensor to the long extensor for effective intrinsicplasty and close all incisions.
(ELLIS ET AL.)
Make an incision over the dorsal aspect of the metatarsophalangeal joint and identify the extensor digitorum brevis and longus tendons.
Lengthen the extensor digitorum longus with a Z-plasty technique and release the extensor digitorum brevis 0.5 cm proximal to the metatarsophalangeal joint.
Release the dorsal capsule and the medial collateral ligament.
If not reduced, release the plantar plate on the contracted side ( Fig. 84.15A ) until the metatarsophalangeal joint is reduced on the anteroposterior fluoroscopic view taken with the ankle in neutral and the foot and toes plantigrade to simulate gentle weight bearing.

Because the authors noted that such a release tended to overcorrect the deformity once the reconstruction was added, they have subsequently performed the release sequentially until the multiplanar subluxation was nearly but not fully corrected on fluoroscopy.
If full correction is obtained with release of one third the width of the plantar plate or less, a tendon reconstruction is not added.
If tendon reconstruction is necessary, leave the extensor digitorum brevis tendon attached distally; this eliminates the need for it to heal to bone at the proximal phalanx.
Pass the extensor digitorum brevis tendon through a drill hole in the proximal phalanx from dorsal-medial to plantar-lateral and under the soft tissue dorsal to the transverse metatarsal.
Pass the tendon back up through a second drill hole from plantar-lateral to dorsal-medial through the metatarsal neck, replicating the plantar course of the involved lateral collateral ligament ( Fig. 84.15B ).
Tension the tendon appropriately with the toe in a corrected position ( Fig. 84.15C ) and secure it over a small screw post (2 or 2.4 mm) placed in the metatarsal shaft ( Fig. 84.15D ).
If the toe remains slightly extended at the metatarsophalangeal joint, add a plantar dermodesis.
On each toe to be corrected, make a transverse plantar incision at the proximal flexion crease of the toe ( Fig. 84.16A ), taking care to preserve the digital arteries and nerves.
Retract the skin and subcutaneous tissue with small hooked retractors and expose the underlying flexor tendons and their fibrous sheaths.
Open the proximal 3 to 4 mm of pulley to expose the flexor digitorum longus immediately under it. This is best done by opening the pulley to one side and dissecting over the underlying tendons, removing a small segment of pulley. This dissection is made easier by the use of magnification loupes and a small round-end knife. Topographically, this dissection is located at about the middle third of the proximal phalanx. The central tendon should be the flexor digitorum longus; gentle, passive flexion and extension of the distal interphalangeal joint while the proximal interphalangeal joint is held straight confirms this.
While lifting the flexor digitorum longus tendon, the vinculum longum, if present, appears under tension and should be severed after electrocautery.
Make a second transverse plantar incision at the distal interphalangeal joint and perform a tenotomy of the flexor digitorum longus, taking care not to violate the plantar plate of this joint ( Fig. 84.16A ,B).
Returning to the proximal incision, hook (but do not clamp) the flexor digitorum longus with a small hemostat and deliver the distal segment into the wound. If the vincula between the two incisions are tenacious, this step might require force.
When the flexor digitorum longus is delivered from the proximal incision, inspect the wound again to ensure that the two lateral slips of the flexor digitorum brevis are intact ( Fig. 84.16C ).
Careful inspection of the flexor digitorum longus shows a shallow, linear furrow running longitudinally along its plantar surface. Using small forceps, hold one side of the delivered tendon at its free end, while an assistant holds the other, and split the tendon longitudinally along this natural cleavage plane for 1.5 to 2.5 cm ( Fig. 84.16D ).
Pull the tendon distally with the ankle plantarflexed to see clearly both sides of the tendon during this step and to prevent inadvertent sectioning of half of the tendon. Other helpful points are to hold the two segments apart only enough to fit a small pair of straight scissors in the axilla of dissection and to use the tips of the scissors.
Moisten the tendon with saline and make a second skin incision longitudinally in the midline on the dorsum of the proximal phalanx, 1.5 to 2 cm in length ( Fig. 84.16E ). The dorsal digital veins usually are to each side of this incision, but if they are in line with the incision, cauterize them.
By sharp dissection, identify the trailing edge of each lateral band of the extensor mechanism while the skin is retracted, including the superficial veins and nerves to either side, using two-pronged skin hooks.
Make 3- to 4-mm longitudinal incisions into the extensor mechanism halfway between the midline dorsally and the trailing edge of the lateral band plantarward on each side. These incisions should be at the level of the middiaphysis of the proximal phalanx (see Fig. 84.16E ).
Pass a small hemostat through one incision in the extensor mechanism to emerge into the plantar incision, staying close to bone. This technique avoids the digital neurovascular bundle.
Grasp one slip of the split flexor digitorum longus at its tip with a hemostat and bring it into the dorsal wound through the extensor mechanism.
Repeat the same procedure on the other side of the phalanx, always ensuring that the slips remain plantar to the deep transverse intermetatarsal ligament.
With an assistant holding the ankle joint at 90 degrees (neutral dorsiflexion and plantarflexion), tighten the tendon slips sufficiently to hold the metatarsophalangeal joint at neutral to 5 degrees of plantarflexion ( Fig. 84.16F ,G).
An alternative technique is to overlap the tendon slips dorsally. Occasionally, the flexor digitorum longus needs to be split further linearly. If so, the tendon slips must be returned to the plantar incision to avoid severing one half.
With the tendon slips held at the desired tension, use 3-0 or 4-0 nonabsorbable sutures to fasten each slip of the flexor digitorum longus under tension to the extensor mechanism, while the assistant continues to hold the ankle in neutral position.
Loop the tip of each slip back on itself and secure it to the trailing edge of each side of the lateral band and to itself. Section any excess tendon.
Alternatively, suture the two tendon slips to one another over the dorsum of the phalanx. This leaves a small knot beneath the skin ( Fig. 84.17 ).
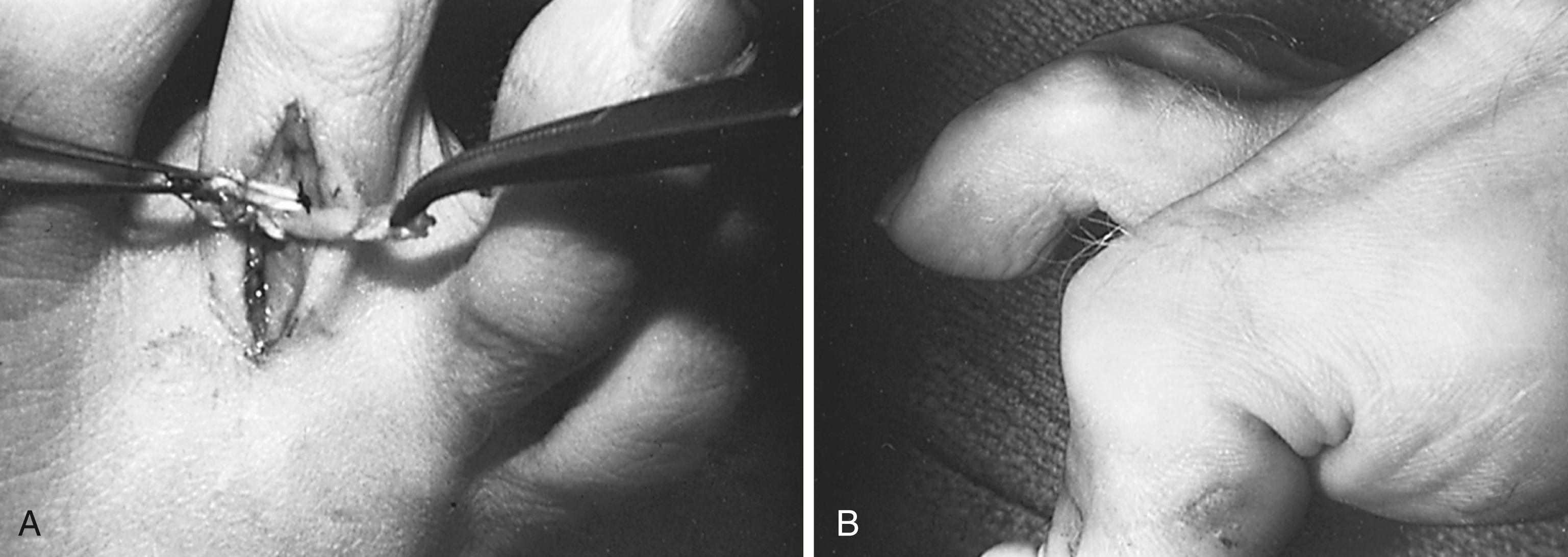
With the ankle extended to neutral, the metatarsophalangeal joint should rest in the neutral or slightly flexed position and the proximal interphalangeal joint should rest in the neutral position or in a position with less than 10 degrees of flexion.
If the same procedure is being done for the central three digits, correct the second toe first because it usually is the most severely affected. The flexor digitorum longus of the third and fourth digits will have been pulled distally through the common tendon in the midsole as the second toe flexor digitorum longus is sutured under tension. This makes tension adjustment easier in the third and fourth toes.
In a modification of the technique, after distal release of the flexor digitorum longus, it can be put through a hole in the proximal phalanx and sutured to the extensor at the appropriate tension.
Before closing the skin, remove any tourniquet and obtain hemostasis by cautery or compression. Close the wounds with 4-0 monofilament nylon or suture of the surgeon’s choice.
A short leg, well-padded cast extending past the toes is applied in the operating room. The foot is elevated for 48 to 72 hours, and bathroom privileges are allowed. Crutches are optional, and weight bearing to tolerance is allowed. The patient usually is off crutches within 1 week. The cast is removed and replaced at 2 weeks, and at 4 weeks, a deep, wide toe box, soft-vamp shoe is allowed. Active toe exercises are encouraged at 6 weeks.
(HADDAD)
Begin a dorsal approach just distal to the proximal interphalangeal joint, with a gentle curve at the level of the metatarsophalangeal joint along the lateral border of the metatarsal shafts and extending 5 cm proximal to the metatarsophalangeal joint.
Dissect the dorsal digital nerves free and protect them during dissection to preserve postoperative sensation.
Identify the extensor digitorum brevis to the musculotendinous junction proximally and place two stay sutures (3.0 Ethibond) on either side of the proposed sectioning of the tendon. Note that this is a proximal sectioning, near the musculotendinous junction ( Fig. 84.18A ).
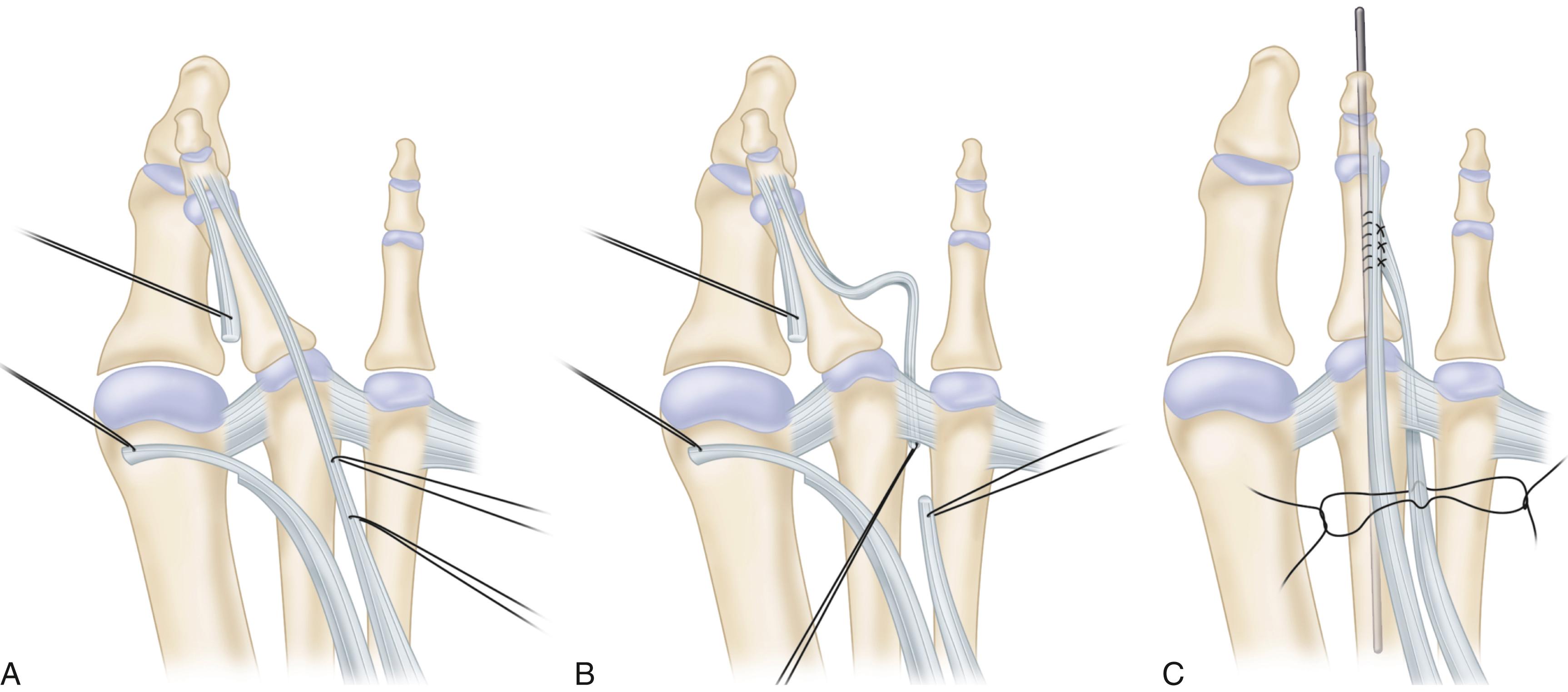
Section the tendon.
Identify the extensor digitorum brevis tendon distally to its insertion and free it from the capsular aponeurosis (extensor hood) proximally to the transverse metatarsal ligament.
Completely section the medial collateral ligament and the dorsal capsule of the metatarsophalangeal joint; make sure that the medial sectioning does not violate the plantar plate.
Use a McGlamry elevator or gouge to strip the volar plate at its origin. This will allow the plate to scar to the metatarsal proximal to its current insertion, assisting with stability.
Examine the lateral collateral ligament for rupture. If it is attenuated, excise redundant tissue. Place, but do not tie, permanent sutures in a figure-of-eight configuration to repair the lateral collateral ligament.
If a hammer toe deformity is present, perform minimal resection of the distal and proximal condyle to stimulate proximal interphalangeal fusion.
Suture the distal extensor digitorum brevis tendon to the plantar lateral base of the proximal phalanx with a permanent suture to eliminate a rotary force on the toe after transfer.
Identify the transverse metatarsal ligament between the second and third metatarsal heads. It is critical not to mistake the more dorsal fascia for the transverse metatarsal ligament because it does not have the integrity of this structure. Use a lamina spreader to place tension on this ligament.
Place a 90-degree right-angle clamp from proximal to distal deep to the transverse metatarsal ligament.
Pass the extensor digitorum brevis tendon from distal to proximal deep to the transverse metatarsal ligament by grasping the previously placed stay suture ( Fig. 84.18B ).
Tie the sutures repairing the lateral collateral ligament.
Place a 0.062-inch Kirschner wire across the metatarsophalangeal joint to hold the joint reduced. This takes the tension off the lateral collateral ligament repair by placing the toe in some valgus and plantarflexion.
Tie the tendon transfer end to end, completing the anastomosis ( Fig. 84.18C ).
Release the tourniquet and evaluate vascularity of the digit before closing the incision with a layered closure using 4-0 Monocryl and 4-0 nylon.
The pin is removed at 6 weeks after surgery, and the toe is taped into slight valgus for an additional 6 weeks.
For residual deformity in the axial plane, an osteotomy at the proximal metaphysis of the proximal phalanx can provide realignment of either valgus or varus malalignment of the toe. The technique described by Kilmartin and O’Kane is described. We prefer to use a 2- or 3-mm burr to make the osteotomy, leaving the opposite cortex intact, “greenstick” the osteotomy closed, and fix the basilar osteotomy with the Kirschner wire inserted to provide stability for the proximal interphalangeal resection done for hammer toe correction.
(KILMARTIN AND O’KANE)
Make a 3-cm “lazy-S” incision extending from the midpoint of the second toe proximal phalanx medially into the metatarsophalangeal joint.
Deepen the incision to bone, passing medial and plantar to the extensor tendon.
Divide the joint capsule to expose the base of the phalanx only; do not extend the capsular incision onto the metatarsophalangeal joint.
Use a power saw to make a cut where the flare of the base of the phalanx meets the shaft. Make the first osteotomy cut parallel with the base of the phalanx, passing through the dorsal, plantar, and medial cortices but leaving the lateral cortex intact.
Make the second distal cut parallel with the distal end of the toe so that the distal cut converges with the proximal cut, leaving the lateral cortex intact ( Fig. 84.19 ). This creates a triangular wedge, generally 3 to 4 mm wide at the base.
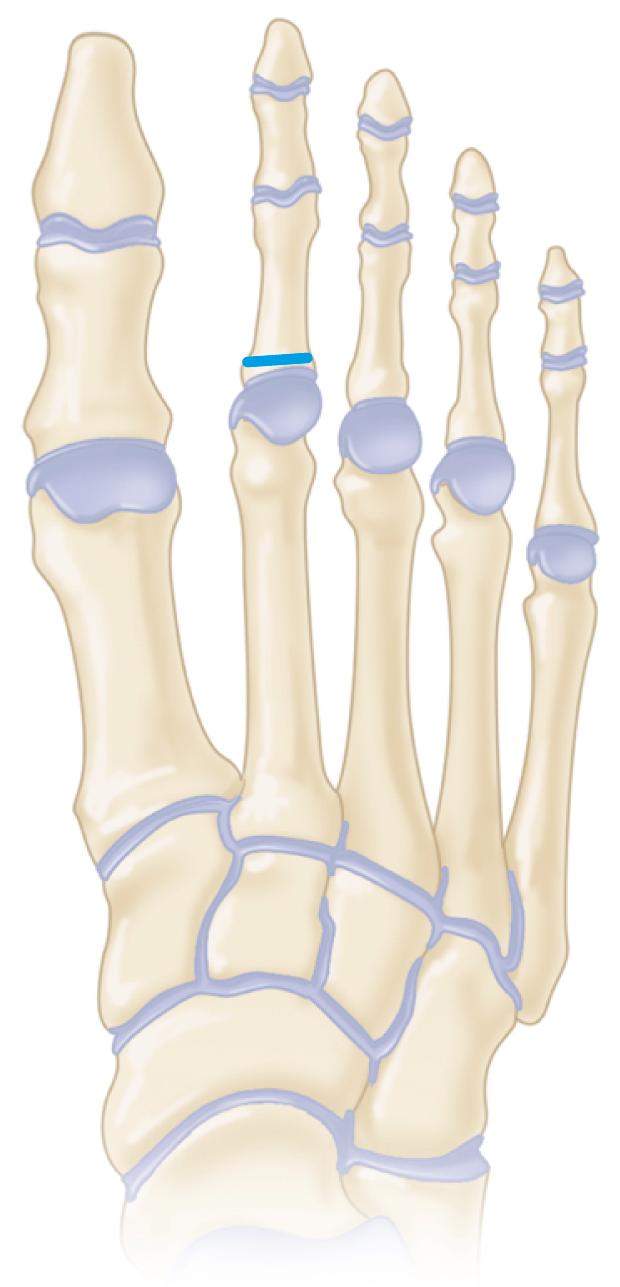
Feather the lateral cortex and close the osteotomy with finger pressure.
Close the deep structures with 3-0 Vicryl interrupted sutures and the skin with 4-0 Monocryl subcuticular sutures.
The second toe is “buddy taped” to the first toe with up to six 12-mm-wide strips of adhesive surgical tape, which are placed dorsally and plantarly on the hallux and second toe. The tape is kept in place for 2 weeks. A stiff-soled postoperative shoe is worn for 2 weeks, and then patients are allowed to return to wearing running shoes and to slowly return to normal activities.
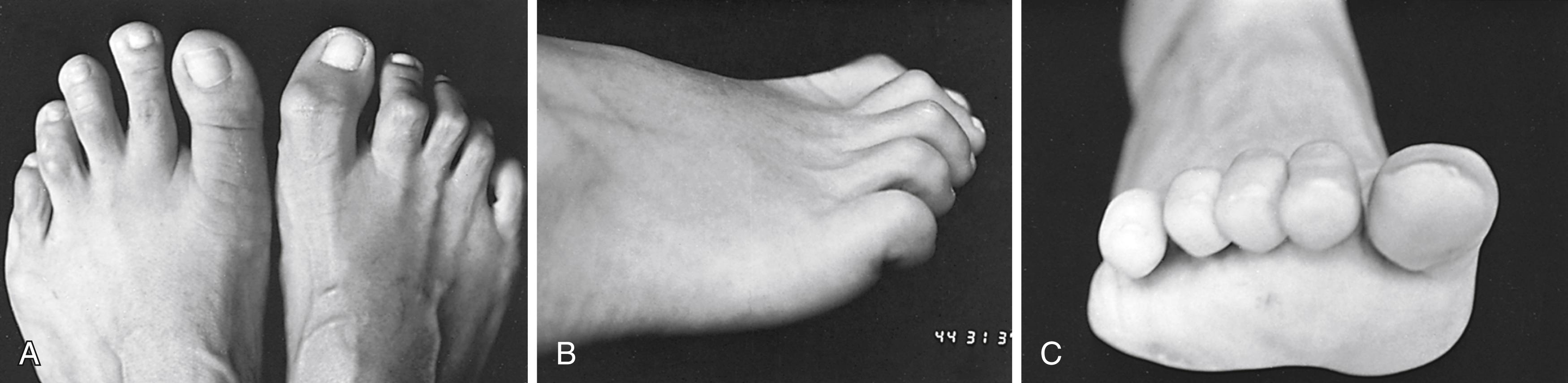
The term hammer toe is used most often to describe an abnormal flexion posture of the proximal interphalangeal joint of one of the lesser four toes ( Fig. 84.20 ). The flexion deformity may be fixed (i.e., not passively correctable to the neutral position) or flexible (i.e., passively correctable). If the flexion contracture at this middle joint of the digit is severe and of long duration, the metatarsophalangeal joint usually is deformed in the opposite direction (i.e., extension). The distal joint usually stays supple, but it also may develop a flexion or an extension deformity. The terms claw toe and hammer toe are differentiated from one another by the following: claw toes frequently are caused by neuromuscular diseases, and often a similar deformity is present in all toes, whereas in hammer toe deformity only one or two toes are involved; claw toes always have extension deformity at the metatarsophalangeal joint, but in hammer toe deformity, extension of the metatarsophalangeal joint may or may not be present; and claw toes often have a flexion deformity at the distal interphalangeal joint, but this usually does not occur in hammer toes ( Fig. 84.21 ).

Claw toes can be caused by neuromuscular diseases. The intrinsic muscles of the foot, specifically the interossei, pass plantar to the axis of rotation of the metatarsophalangeal joint, causing flexion of this joint. Loss of intrinsic function of the foot leads to an imbalance, allowing the extensor digitorum longus to extend the metatarsophalangeal joint and the flexor digitorum longus to flex the interphalangeal joints. Although the long extensors of the toes may extend the interphalangeal joints with the metatarsophalangeal joint in neutral, when an extension posture of the metatarsophalangeal joint develops, the long extensor loses its excursion and no longer can extend the interphalangeal joints. The powerful flexors of the toe, specifically the long flexor, which attaches to the base of the distal phalanx, accentuate the deformity, causing flexion of the interphalangeal joints.
Although the causes of claw toe deformity can be easily understood, most hammer toes have no underlying intrinsic imbalance. The use of electrodes to evaluate the phasic activity of the intrinsic muscles of the foot found no activity of the intrinsic muscles during the first 35% of the gait cycle. With quiet standing, intrinsic muscle activity was absent. Hammering of the toes usually is accentuated by standing, and the lack of activity of the intrinsics during quiet standing implies that loss of intrinsic function is not the cause of the deformity.
Factors commonly thought to contribute to hammer toe deformity include the long-term use of poorly fitting shoes. Crowding of the toes within an excessively tight toe box causes some deformation of the metatarsophalangeal and interphalangeal joints that over time can lead to flexible and eventually fixed deformities at these joints. Anatomic factors that can cause lesser toe deformities include a “two-bone toe” and a long second ray, which may result in buckling of the toe, and hallux valgus, causing pressure against the second toe. Other factors include connective tissue disorders and trauma.
Three areas may be painful in hammer toe deformity. The most common area is the dorsum of the proximal interphalangeal joint, where a hard corn caused by pressure from the toe box or vamp of the shoe develops. When a flexion posture or end-bearing posture of the distal interphalangeal joint is present, a painful callus develops just plantar to the nail end. This is called an end corn. Finally, a painful callus may develop beneath the metatarsal head if the proximal phalanx subluxates dorsally. In a patient with decreased sensibility, such as occurs in diabetes mellitus or myelomeningocele, ulceration and deep infection can develop at one or more of these areas of pressure, complicating the treatment plan and endangering the toe or foot. Sometimes the dorsofibular side of the second metatarsophalangeal joint is tender ( Fig. 84.22 ).
Conservative treatment of hammer toe usually is disappointing. Various pads and strappings are commercially available to reduce the deformity and relieve pressure over painful points. If the deformity is not of long duration and an extension deformity at the metatarsophalangeal joint is not present, daily manipulations and taping the toe so that the metatarsophalangeal joint is not extended occasionally can correct the flexion deformity at the proximal interphalangeal joint. This is because the extensor digitorum longus can forcefully extend the middle phalanx only if the metatarsophalangeal joint is in neutral or some degree of flexion. Recurrence is likely, however, when the passive stretching and taping cease, and most patients with symptomatic hammer toe eventually require surgery. The following procedures are not all of the operations available for treating hammer toes; rather, they are the most commonly recommended procedures that have follow-up data to support the recommendations ( Table 84.2 ).
| Deformity | Characteristics | Treatment |
|---|---|---|
| Flexible hammer toe | No fixed contracture at MTP or PIP joint | Usually nonoperative; rarely, flexor-to-extensor transfer using FDL |
| Fixed hammer toe with fixed extension of MTP | Fixed flexion contracture at PIP; MTP subluxation in extension | Resection of condyles of proximal phalanx, dermodesis; lengthening of EDL, tenotomy of EDB; MTP capsulotomy, collateral ligament sectioning |
| Fixed hammer toe with MTP subluxation | Fixed flexion contracture at PIP; MTP subluxation in extension | Plantar plate repair after Weil osteotomy |
| Crossover toe | Fixed flexion contracture at PIP; MTP subluxation in varus or valgus | Resection of condyles of proximal phalanx, dermodesis; collateral ligament/capsular repair; EDB transfer |
| Mallet toe | Fixed flexion contracture at DIP | Resection of condyles of middle phalanx, dermodesis; FDL tenotomy |
The use of soft-tissue procedures alone without bone shortening or arthrodesis may or may not result in permanent correction. In a skeletally immature foot with symptomatic flexible hammer toe or in a young adult foot with dynamic flexible deformities of one or more toes (prominent hammering only with weight bearing) that interfere with shoe wear, flexor-to-extensor transfer is indicated, based on the assumption that the flexor digitorum longus contributes to deformity. The role of the flexor digitorum longus in causing flexion contracture at the proximal interphalangeal joint has been questioned, but several authors have advocated the procedure for flexible hammer toes.
A soft-tissue procedure is most reliable in patients with planovalgus or normal arches as opposed to cavus feet. In addition, patients should be younger than 30 years old, have no deformity at the metatarsophalangeal joint (can flex the joints beyond neutral position), and have no fixed flexion deformity at the proximal interphalangeal joints. In other words, a symptomatic, idiopathic, mild, flexible hammer toe deformity in a young patient is most likely to benefit from flexor-to-extensor transfer. To decrease the frequency of “floating toe” after flexor digitorum longus transfer, Boyer and DeOrio modified the technique by placing the plantar incision for harvest of the flexor digitorum longus longitudinally at the metatarsophalangeal joint crease rather than transversely, using larger (0.54-mm) Kirschner wires for fixation, using absorbable sutures for tenodesis, and passing the transferred tendon deep to the dorsal hood rather than superficial to it. They reported no floating toe deformities in their 38 patients (79 toes) and an 89% patient satisfaction rate.
The most commonly used procedures for the correction of hammer toe are resection of the proximal interphalangeal joint, resection of the base of the proximal phalanx, resection of the distal third or fourth of the proximal phalanx, complete proximal phalangectomy, and arthrodesis of the proximal interphalangeal joint. Schrier et al. compared outcomes after proximal interphalangeal joint resection with those after arthrodesis and found no difference between the two procedures; both had good results in regard to pain and activity scores.
The following recommendations are not unique, and they are not intended to be absolute or universal in the surgical treatment of hammer toe. Only a symptomatic toe should undergo surgery. An unattractive deformity is not a strong enough indication for surgical correction. Hammer toe encompasses a spectrum of deformities, and the indicated procedure varies, depending on the stage of the deformity when first seen and the diagnosis, as follows:
No fixed contracture at the metatarsophalangeal or proximal interphalangeal joint is evident. The deformity increases on weight bearing. In a young adult with a mild deformity, a flexor-to-extensor transfer using the flexor digitorum longus is recommended, as previously described.
There is a fixed flexion contracture at the proximal interphalangeal joint and no extension contracture at the metatarsophalangeal joint. In moderate deformity, resection of the head and neck of the proximal phalanx and dermodesis are recommended. A percutaneous extensor digitorum longus tenotomy is performed in the presence of extensor tightness with the ankle held in the neutral position. A Kirschner wire may be needed to maintain reduction. We have found that resection of only the head of the proximal phalanx without arthrodesis has been more successful. Arthrodesis with permanent implantable devices is used primarily for revision surgery. Patients are counseled before surgery that some “molding” of the toe to fit comfortably between the adjacent toes can be expected. In our experience, most patients prefer to have some limited mobility of the proximal interphalangeal joint as opposed to a completely fused proximal interphalangeal joint.
In recent years, there has been a focus on alternative fixation techniques for hammer toe correction, with the goal of reducing the development of recurrent deformity of the toe. In their extensive review of 1115 procedures, Kramer et al. concluded that Kirschner wire fixation resulted in good maintenance of correction with a relatively low complication rate; they suggested that Kirschner wires remain an effective, low-cost method of fixation for hammer toe correction. Obrador et al. reported the use of two intramedullary implants for fixation to avoid complications reported with Kirschner wire fixation. Both implants provided good alignment, improved function, and pain relief; however, the devices were more expensive than Kirschner wires, and the authors noted the need for more cost-benefit studies. A recent literature review by Guelfi et al. found that complications and reoperations after use of various intramedullary fixation devices were similar to those (0 to 8.6%) after Kirschner wire fixation. However, they too acknowledged the higher price of these implants.
Good results have been reported in 90% of patients with the use of an absorbable intramedullary pin for proximal interphalangeal joint arthrodesis. Cited advantages of this technique include avoidance of pins penetrating the skin, less restriction on activity, and a decrease in complications such as floating toe. The authors cautioned, however, that the 2-mm absorbable pins may not provide adequate fixation in larger, longer toes.
There is a fixed flexion contracture at the proximal interphalangeal joint, with a fixed extension contracture at the metatarsophalangeal joint. (Subluxation or dislocation of the proximal phalanx on the metatarsal head may be present in addition to the fixed extension contracture at the metatarsophalangeal joint and fixed flexion contracture at the proximal interphalangeal joint.) In severe deformity without subluxation or dislocation of the metatarsophalangeal joint, it is necessary to resect the head and neck of the proximal phalanx through a dorsal elliptical skin window (and dermodesis), lengthen the extensor digitorum longus, tenotomize the extensor digitorum brevis, and perform a dorsal capsulotomy at the metatarsophalangeal joint. If the extension posture of the metatarsophalangeal joint is not corrected after extensor tenotomy and dorsal capsulotomy, both collateral ligaments should be sectioned, the joint should be brought to neutral position, and the extensor digitorum longus should be repaired in its lengthened position. The metatarsophalangeal joint must be reduced not only in the anteroposterior plane but also in the mediolateral plane, and the reduction of the proximal interphalangeal and metatarsophalangeal joints must be maintained with a longitudinal Kirschner wire. (A carefully applied soft dressing that holds the toe in the corrected position may preclude the use of a Kirschner wire; this dressing must be changed frequently as swelling subsides.) In severe deformity with subluxation or dislocation of the metatarsophalangeal joint, a metatarsophalangeal joint arthroplasty or distal metatarsal osteotomy (Weil) may be needed to decompress the metatarsophalangeal joint (see Technique 84.12).
Make an elliptical incision over the proximal interphalangeal joint that measures 5 to 6 mm wide and has a 2- or 3-mm lateral extension on either side (Fig. 84.23A,B) .
Remove the skin only initially and cauterize the vessels ( Fig. 84.23C ).
Remove a slightly smaller segment of extensor tendon and dorsal capsule of the proximal interphalangeal joint, leaving a 2-mm remnant of extensor tendon attached to the base of the middle phalanx. The proximal end of the extensor tendon usually retracts beneath the proximal skin flap, but it can be easily pulled distally at the appropriate time.
Flex the proximal interphalangeal joint about 20 degrees while putting traction on the distal and middle phalanges.
Using a small-blade knife, section the collateral ligaments from outside in on both sides of the joint by placing the blade between the skin and the ligament and turning the cutting edge toward the joint. The proximal interphalangeal joint can be flexed to 90 degrees ( Fig. 84.23D ), and the head and neck of the proximal phalanx is clearly exposed ( Fig. 84.23E ).
With a rongeur or small-blade power saw, remove the head and neck of the proximal phalanx and smooth any sharp points of bone with a rasp or rongeur ( Fig. 84.23F ).
Extend the toe to neutral position at the proximal interphalangeal joint and feel for tightness with abutment of the articular surface of the middle phalanx on the distal end of the proximal phalangeal remnant. If it feels tight, remove 2 or 3 mm more of bone.
Use a 3-0 or 4-0 nonabsorbable suture to enter the proximal skin edge and pass through the proximal end of the extensor tendon.
Enter the distal remnant of the extensor tendon on its joint surface and exit through the skin. By canting the stitch, a few degrees of lateral deformity also would be corrected.
Suture the corners of the wound with a simple stitch ( Fig. 84.23G ). An initial mattress stitch can be used if deemed appropriate.
A supportive forefoot dressing to the tips of the toes is crucial ( Fig. 84.24 ).

This technique usually holds the proximal interphalangeal joint in acceptable alignment with only a few degrees of flexion.
If needed, perform a percutaneous extensor digitorum longus tenotomy over the neck of the metatarsal, avoiding the dorsal veins (see Fig. 84.23F ).
When the ankle is held in neutral position, if the metatarsophalangeal joint rests in extension, the tenotomy is performed. The toe is flexed at least 60 to 70 degrees at the metatarsophalangeal joint to allow the metatarsophalangeal joint to flex to neutral position with the ankle joint at neutral in a moderate hammer toe deformity.
Occasionally, an extensor digitorum brevis tenotomy also is required. At the neck of the metatarsal, the extensor digitorum brevis tendon is immediately lateral and slightly plantarward to the extensor digitorum longus.
Use a soft dressing (2-inch gauze is helpful) and ½-inch tape to hold the toe in the desired position, wrapping it to an adjacent toe.
Weight bearing to tolerance is allowed after 48 to 72 hours of elevation of the foot. A wooden-soled shoe is worn for 4 weeks. The sutures are removed at 12 to 16 days, and a carefully applied dressing maintains the toe in the corrected position for another 2 weeks. At 4 weeks, the dressing and taping usually can be discontinued, but they should be continued another 2 to 4 weeks if the deformity has any tendency to recur. The proximal interphalangeal joint usually retains a few degrees of active motion and is gently flexed, which seems to be more pleasing than a fused, straight toe at the proximal interphalangeal joint.
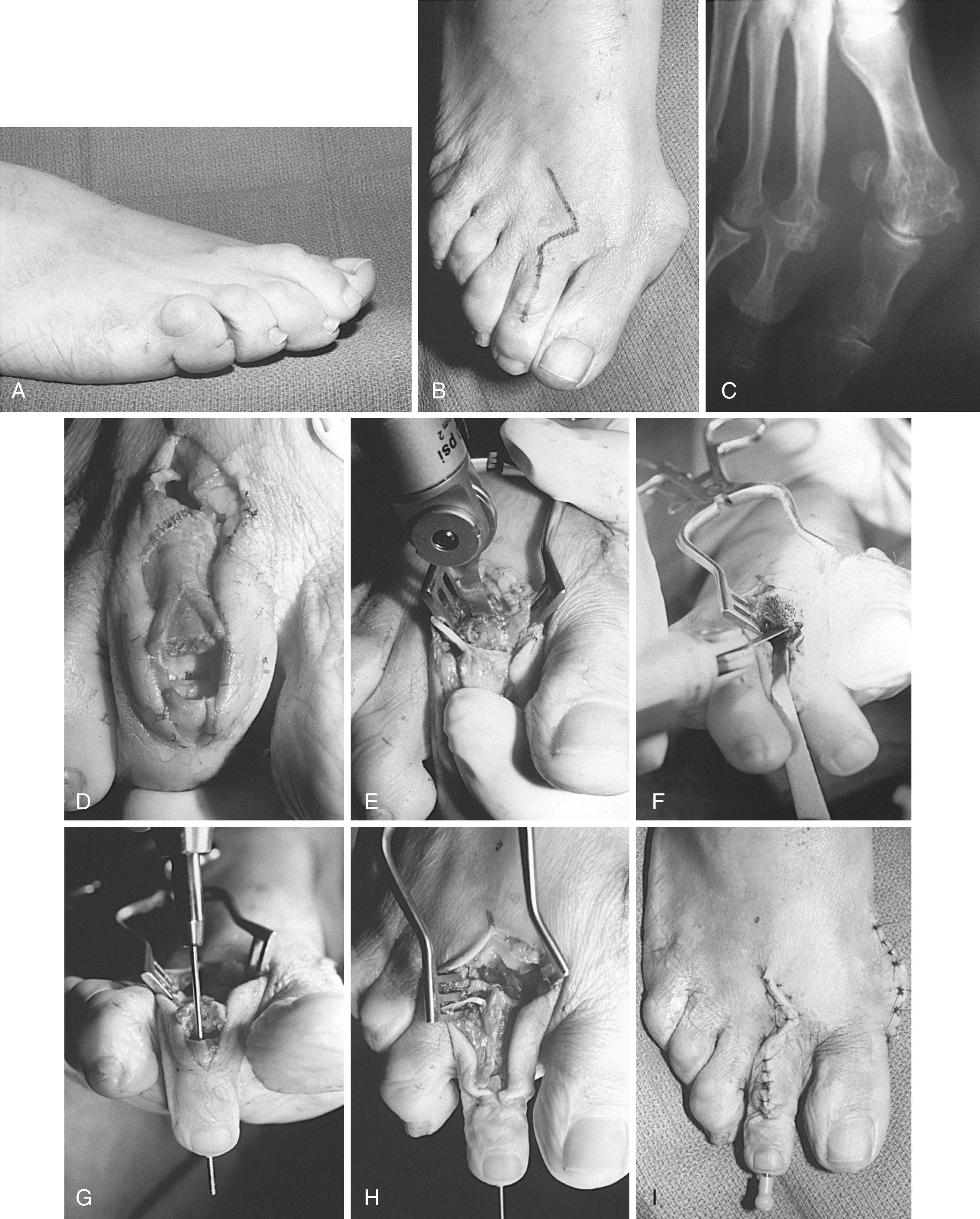
Because a severe deformity by definition has a fixed extension contracture at the metatarsophalangeal joint and a fixed flexion contracture at the proximal phalangeal joint, both joints require correction ( Fig. 84.25 ).
Begin at the metatarsophalangeal joint with a straight or angled incision centered over the fibular aspect of the metatarsophalangeal joint ( Fig. 84.26A ).
Cauterize or retract the branches of the dorsal venous arch returning from the toe to expose the extensor tendons.
The extensor digitorum brevis is slightly fibular and deep to the extensor digitorum longus. The extensor digitorum brevis joins the extensor digitorum longus and extensor expansion at the neck of the metatarsal ( Fig. 84.26B ). Before this confluence, dissect the extensor digitorum brevis from the extensor digitorum longus and remove a 2- to 3-mm segment of extensor digitorum brevis.
Perform a Z-plasty lengthening of the extensor digitorum longus. The use of a small blade (No. 67 Beaver or similar cutting edge) is helpful.
From the proximal part of the skin incision until the extensor digitorum longus joins with the extensor expansion, make a longitudinal incision into the extensor digitorum longus, exiting at a right angle at the junction of the extensor digitorum longus and the extensor expansion. Sever the tendon proximally at a right angle in the opposite direction.
Lift the tendon away from other soft-tissue attachments. This maneuver lengthens the extensor digitorum longus by 8 to 12 mm ( Fig. 84.26C ).
Usually, if the extension contracture is less than 20 to 30 degrees and there is no dorsal subluxation of the proximal phalanx on the metatarsal head, firmly flex the toe 30 to 40 degrees. If the toe rests in neutral position at the metatarsophalangeal joint with the ankle at 90 degrees, this is all that is required at this joint except suturing the extensor digitorum longus in its lengthened position with 3-0 or 4-0 absorbable suture after the proximal interphalangeal joint has been corrected.
If after the just-described procedure the toe still rests in 10 to 20 degrees of extension, perform a dorsal capsulotomy transversely while the toe is flexed 40 to 50 degrees ( Fig. 84.26C , inset ). This much flexion of the toe pulls the extensor expansion distally, giving better exposure of the dorsal capsule. The capsule may vary from a thin, filmy, pliable, synovial-like covering to a dense, thick, fibrous encapsulation of the joint, depending on the chronicity of the deformity, the number of recurrent synovial inflammatory episodes, and the congruency of the joint.
When the capsule is divided, flex the toe acutely again and return the ankle to 90 degrees, observing the resting posture of the toe. If the posture is acceptable (neutral to 10 degrees of metatarsophalangeal joint extension with the ankle at 90 degrees), all that is needed is to suture the extensor digitorum longus in its lengthened position.
If the toe still has an unacceptable extension posture, acutely flex the toe and use a small blade to incise the collateral ligaments on both sides of the metatarsal head down to, but not through, the plantar plate of the metatarsophalangeal joint. This should allow the toe to assume a neutral to slightly flexed position at the metatarsophalangeal joint even if the toe was subluxed dorsally ( Fig. 84.26D ).
Suture the extensor digitorum longus after correcting the proximal interphalangeal joint contracture.

Severe deformity with dislocation of the metatarsophalangeal joint is difficult to correct. All of the aforementioned recommendations are applicable—extensor digitorum longus lengthening, extensor digitorum brevis tenotomy, dorsal capsulotomy, and bilateral collateral ligament release—but, in addition, decompression of the metatarsophalangeal joint usually is required. This can be done on the phalangeal or metatarsal side of the joint; however, because of the difficulty in maintaining the position of the toe, even with pinning of the reduced joint for several weeks, and the probability of a metatarsal head plantar callus developing laterally, resecting the base of the proximal phalanx is not preferred. Decompression on the metatarsal side of the joint can be achieved with a metatarsophalangeal joint arthroplasty or shortening (Weil) osteotomy of the distal metatarsal.
For metatarsophalangeal joint arthroplasty, resect (contour) the metatarsal head 3 to 4 mm, including its plantar projection ( Fig. 84.27 ). This resection does not return the joint to normal, but it usually restores 10 to 20 degrees of motion in an acceptable plane, and the toe remains reduced on the metatarsal head.
Contouring the metatarsal head enough to allow reduction of the toe and passively moving the toe 30 to 40 degrees without grating or forceful impingement of the adjacent surfaces should provide an acceptable result in a difficult deformity. The position must be held 3 to 4 weeks with a medullary pin ( Fig. 84.28 ).
Pin the metatarsophalangeal joint in 10 degrees of extension with the ankle held at 90 degrees. Ensure that the joint is reduced in the mediolateral plane, again while holding the ankle at 90 degrees.
A word of caution concerning palpable grating of the “arthroplasty”: if after contouring the metatarsal head the metatarsophalangeal joint still feels tight, with the proximal phalanx grating on the contoured metatarsal head, more bone should be removed until the grating stops.
The technique of pinning varies, but one suggestion is to insert the pin antegrade through the middle and distal phalanges, exiting in the midline 2 to 3 mm plantar to the nail ( Fig. 84.29A ). Reverse the pin to drive it retrograde through the remaining portion of the shaft of the proximal phalanx (the head and neck of the phalanx have been resected through a separate dorsal elliptical incision over the proximal interphalangeal joint) ( Fig. 84.29B ).
Exit the articular surface of the proximal phalanx near its center, and, while standing at the head of the table holding the toe reduced at the metatarsophalangeal joint (as the patient would see the toe), have an assistant drill the pin into the metatarsal.
Finding the medullary canal of the proximal phalanx occasionally is difficult. Take a free 0.062-inch or 0.045-inch Kirschner wire or a small straight hemostat and open the canal of the proximal phalanx. This allows the Kirschner wire to find its way without exiting the cortex before reaching the proximal articular surface.
In moderate or severe deformity, the metatarsophalangeal joint is not pinned until the proximal interphalangeal joint contracture is corrected. This technique is the same as described in Technique 84.10.
Remove the tourniquet and obtain hemostasis.
Resuture the extensor digitorum longus in a lengthened position end to end. Bring the ankle joint to 90 degrees and put just enough tension on the proximal end of the extensor digitorum longus to bring it out to its resting length. Where the severed ends of the extensor digitorum longus overlap, excise the overlapping proximal portion and continue the repair with 3-0 or 4-0 absorbable suture.
Close the skin with 4-0 or 5-0 nonabsorbable suture and place a forefoot dressing, taking care not to constrict the vascularity of the toe.
In a chronically dislocated toe, reducing contractures at the metatarsophalangeal and proximal interphalangeal joints may place tension on the neurovascular bundles. Particularly vulnerable is the reoperated toe, with its attendant scarring and compromised dorsal venous return. If the toe looks vascularly impaired, remove the Kirschner wire and allow the toe to “settle” in a shortened position. This places additional demands on the dressing, which must be meticulously applied to hold the toe in an acceptable position.
A patient who requires extensive dissection on adjacent joints of the same toe must be advised preoperatively that loss of the toe from vascular compromise could occur.
Postoperative care is the same as for a moderate deformity except that the Kirschner wire almost always is used in a severe deformity, unless compromised vascularity prevents it. The Kirschner wire is removed at 3 to 4 weeks, and the toe is maintained in the corrected position at the metatarsophalangeal and proximal interphalangeal joints with a gauze wrap and ½-inch tape. A wooden-soled shoe usually is worn for 4 weeks, and a deep, wide, soft shoe is worn for another 4 to 6 weeks. Weight bearing to tolerance is allowed after the foot is kept elevated for 48 to 72 hours. The use of crutches is optional.
As an alternative to contouring or resection arthroplasty of the second metatarsal head for a dislocated second metatarsophalangeal joint, a shortening osteotomy of the metatarsal head and neck region is reasonable, and satisfactory results have been described. An advantage of this technique is that it preserves the articular surface while decompressing the joint, making this a more popular procedure. This procedure is especially useful if the length of the second metatarsal is excessive in relation to the first and third metatarsals. Reports in the literature suggest a small incidence of transfer metatarsalgia or recurrent instability. Stiffness of the metatarsophalangeal joint may occur postoperatively but is usually not a cause of patient dissatisfaction. Complications including floating toe, recurrence of metatarsalgia, and transfer metatarsalgia have been reported in 7% to 15% of patients. Strategies to reduce the frequency of these complications include removal of a slice of bone to prevent excessive plantar translation, repair of the plantar plate when indicated or possible (see Technique 84.1), transfer of the long flexor tendon dorsally, and, occasionally, transarticular pinning across the metatarsophalangeal joint for temporary stabilization.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here