Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The latissimus dorsi (LD) flap is a reliable option for primary autologous breast reconstruction and for salvage of failed prior breast reconstruction because of its robust perfusion, consistent vascular anatomy, and concealable donor site scar. However, the traditional LD flap is limited by its volume, and often requires augmentation with either an implant, additional autologous tissue flaps, or fat grafting to obtain the desired shape and volume.
Hokin et al, first described the use of an extended LD (ELD) flap, which incorporated lumbar fat to increase flap volume. In an attempt to avoid using a breast implant, modifications of the ELD by harvesting the entire LD muscle, lumbar fascia, and a large skin paddle have been performed. However, it has been associated with increased morbidity, with risks of wound breakdown, skin necrosis, seroma formation, and significant contour deformities of the back.
Advancements in surgical techniques with the use of progressive tension sutures, quilting sutures, and fibrin sealants to obliterate potential space at the LD and ELD donor sites have decreased rates of seroma formation. ( ![]() and
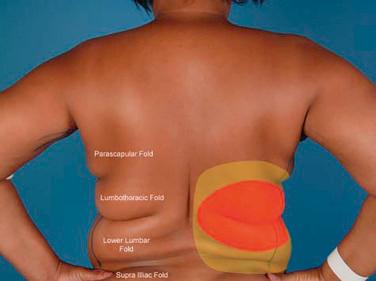
and ![]() demonstrate progressive tension sutures and quilting sutures technique. demonstrates the obliteration of empty space after performing quilting sutures at the donor site). Furthermore, a greater appreciation of the different fat compartments in the back has limited fat harvest to the thoracolumbar and lumbar compartments, thereby optimizing the contour of the back after flap harvest. The selective harvest of these fat compartments provides the patient with an ideal “hourglass” figure, while avoiding the disfigurement associated with parascapular fat harvest, and the fat necrosis with harvest of the distal suprailiac fat. The most versatile tool in volume augmentation and for the correction of contour deformities has been the incorporation of fat grafting of the mastectomy site and the LD flap. Fat grafting can be performed at the time of LD breast reconstruction or as an adjunct procedure during secondary breast reconstruction revision. (
demonstrate progressive tension sutures and quilting sutures technique. demonstrates the obliteration of empty space after performing quilting sutures at the donor site). Furthermore, a greater appreciation of the different fat compartments in the back has limited fat harvest to the thoracolumbar and lumbar compartments, thereby optimizing the contour of the back after flap harvest. The selective harvest of these fat compartments provides the patient with an ideal “hourglass” figure, while avoiding the disfigurement associated with parascapular fat harvest, and the fat necrosis with harvest of the distal suprailiac fat. The most versatile tool in volume augmentation and for the correction of contour deformities has been the incorporation of fat grafting of the mastectomy site and the LD flap. Fat grafting can be performed at the time of LD breast reconstruction or as an adjunct procedure during secondary breast reconstruction revision. ( ![]() demonstrates intraoperative fat grafting of the LD flap.) Other modifications of the LD flap for breast reconstruction include the endoscopically harvested LD, muscle-sparing LD, and the thoracodorsal artery perforator flap (TDAP).
demonstrates intraoperative fat grafting of the LD flap.) Other modifications of the LD flap for breast reconstruction include the endoscopically harvested LD, muscle-sparing LD, and the thoracodorsal artery perforator flap (TDAP).
The LD flap with fat grafting or with an implant can be an excellent choice for primary reconstruction or for salvage of a previously failed reconstruction.
Please see Box 8.1 for inclusion criteria regarding use of LD flaps for breast reconstruction. We prefer to use the LD flap in combination with fat grafting (without implants) in patients with the following characteristics:
Patient not a candidate for free flap–based breast reconstruction
Previous radiation therapy (XRT)
High BMI (BMI >35–40 kg/m 2 ) patients
Co-morbidities which preclude long surgical procedures
Conversion of implant-based reconstruction in non–free flap candidates.
Larger breasts can be reconstructed with the augmentation of the LD flap or by harvesting an ELD. The ability to perform fat grafting at the initial reconstruction can help avoid the use of an implant, keeping the reconstruction entirely autologous. The robust vascularity of the flap introduces healthy soft tissue in previously irradiated areas, and can provide excellent soft tissue coverage for implants. There are very few contraindications for the flap, which include:
Previous history of posterolateral thoracotomy
Previous injury to the thoracodorsal pedicle and nerve
Inadequate soft tissue volume at the donor sites (including LD donor site and fat graft donor site).
Inadequate abdominal soft tissue (skin and fat).
Prior abdominal surgery with contraindication for abdominal-based reconstruction (abdominoplasty or previous abdominal-based reconstruction).
Medical co-morbidities with “high risk” of complications with prolonged surgical procedures, including personal history of pulmonary embolism or deep vein thrombosis with positive thrombophilia screen.
Patient with small to moderate breast volume with standard LD.
Patient with large breast volume in high-BMI patients with ELD and fat grafting.
Patient's personal preference.
Prior radiation therapy for breast conservation therapy and not candidate for a free flap.
During the preoperative consultation, the patient's medical history is critically evaluated for their surgical candidacy. This should always include documentation of surgical history, history of nicotine use, cardiopulmonary health status, personal and family history of coagulopathy, therapeutic use of antiplatelet or anticoagulation therapy, history of general anesthesia associated complications, and body mass index (BMI). A complete breast history should be obtained, including prior breast surgeries (aesthetic and reconstructive), planned tumor extirpation method (nipple-sparing vs skin-sparing vs simple mastectomy), prior or planned axillary lymph node dissection, and plan for adjuvant therapies. Women undergoing delayed breast reconstruction are considered better surgical candidates as they have completed all planned adjuvant therapy, have been disease-free for a period of time, and are at a lower risk for infection, hematoma, and mastectomy skin flap necrosis.
A thorough physical examination involves evaluating the involved breasts for surgical scars, presence or absence of the nipple–areola complex, radiation-related skin changes and surrounding tissue quality, and relative symmetry with the contralateral breast. The abdomen, flanks and lower extremities should be examined as possible donor sites for free tissue transfer or fat grafting. The soft tissue of the back is evaluated with a “pinch” test to determine the amount of tissue which can be safely harvested without undue tension on donor-site closure ( Fig. 8.1 ). The thoracolumbar and lumbar fat compartments are readily identified by having the patient flex in the ipsilateral direction to create the natural intercompartmental creases ( Fig. 8.2 ). A pinch test can identify the most natural crease for the skin paddle design along the ipsilateral back. The orientation of the skin paddle is designed as needed to match the soft tissue deficit at the mastectomy site. A horizontal skin paddle designed at the low or mid-back results in a well-positioned final scar, hidden within the bra line, and has the highest reported patient satisfaction ( Fig. 8.3 ). Positioning the skin paddle main axis along a natural tissue crease in the back (usually horizontal or horizontal–oblique) will not only allow for a larger skin paddle harvest, but will also facilitate closure.


The functionality and anterior border of the LD muscle is verified by forceful adduction of the arm against the examiner's hand. This maneuver demonstrates the integrity of function of the LD, and helps identify the anterior border of the muscle. Digital palpation can identify the anterior groove or border of the LD muscle, and the true anterior border of the LD muscle is usually marked 1–2 cm anterior to the palpated groove. The patient should be informed that muscle harvest can occasionally result in weakness with pulling and overhead activities, which might require postoperative physical therapy to help strengthen the shoulder muscles and to improve the range of motion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here