Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Advances in pigment-specific lasers have allowed for the safe and effective treatment of various benign pigmented lesions and tattoos.
Picosecond (PS) lasers are the newest additions with current studies suggesting a superior efficacy and safety profile for treating pigmented lesions and tattoos compared with nanosecond domain quality-switched (QS) lasers.
The pigment-specific lasers most commonly used for benign pigmented lesions and tattoos include the PS alexandrite 755 nm, PS Nd:YAG 532 nm, QS ruby 694 nm, QS alexandrite 755 nm and QS Nd:YAG (532 nm and 1064 nm).
PS lasers are now considered to be the laser of choice for tattoo removal and for Nevus of Ota/Ito lesions.
Fractional photothermolysis is often optimal for treating diffuse skin pigmentation in photodamaged skin as the entire cosmetic subunits can be treated although multiple treatments are often needed and there are greater associated adverse effects.
Patients with Fitzpatrick skin types I to III generally have the best outcomes compared to darker skinned patients. Caution should be taken in patients with Fitzpatrick skin types IV to VI due to risk of postinflammatory dyspigmentation.
Black tattoos respond the best to laser therapy, while multi-colored tattoos are often more difficult to treat.
Caution should be taken when utilizing QS or PS lasers to treated cosmetic tattoos containing white or red ink due to the risk of paradoxical darkening. Test spots should be performed prior to treatment.
Proper patient and lesion selection and evaluation is crucial prior to performing laser therapy for optimal outcomes. Informed consent and pre-procedural photographs should always be obtained prior to initiating therapy.
Adverse effects of laser therapy of pigmented lesions and tattoos include hypopigmentation, hyperpigmentation, textural change, and scarring.
Postoperative care following laser therapy includes gentle cleansing, the use of a bland emollient and strict sun protection.
Advances in laser technology over the last two decades have led to greater efficacy and safety for the treatment of a variety of medical and cosmetic indications including benign pigmented lesions and tattoo removal.
Tattooing is an increasingly popular practice. Based on a survey conducted in 2015, 29% of the United States adults have at least one tattoo, an increase of 8% from 4 years earlier, and nearly half of millennials report having at least one tattoo. However, data demonstrates that almost 25% of people with tattoos regret getting them.
In this chapter, we will discuss the use of laser therapy to treat benign pigmented lesions and tattoos, including important patient considerations, recommendations for optimizing outcomes, and postoperative care. While the target of both lesions is pigment, the techniques utilized to lighten and/or remove these lesions are distinct.
Early lasers (including the argon and CO 2 lasers) used for treatment of pigmented lesions and tattoo removal were not pigment-specific and often associated with significant side effects such as dyspigmentation and scarring. In 1980 Drs. Anderson and Parrish first described the theory of selective photothermolysis, which led to a paradigm shift in laser therapy. According to this theory, use of the appropriate wavelength can allow light energy to be preferentially absorbed by a specific chromophore within the skin (i.e., melanin, tattoo ink particles) and transferred into heat energy. Different chromophores within the skin preferentially absorb specific wavelengths of light. In the case of benign pigmented lesions, the chromophore is melanin within melanocytes, keratinocytes, or dermal macrophages. In tattoos, the target chromophore is exogenously placed ink found within macrophages or extracellularly throughout the dermis. Selection of a laser with a wavelength of light that is preferentially absorbed by a certain chromophore and penetrates to the appropriate depth allows for the selective heating and destruction of the targeted chromophore.
While the wavelength will selectively target a specific chromophore, the pulse duration, or the time that the laser is fired, is also important to limit the damage to the chromophore and surrounding tissue. The pulse duration should ideally be less than or equal to the target chromophore’s thermal relaxation time (TRT), or the time required for the target to lose 50% of heat to the surrounding tissue. If the pulse duration exceeds the TRT, the heat will likely spread to the surrounding tissue, causing damage that can lead to adverse effects including scarring. Therefore, selection of the appropriate wavelength and pulse duration allows for target destruction of a specific chromophore with minimal damage to surrounding structures. Melanosomes containing melanin are small structures, about 0.5 micrometers in diameter and, therefore, have very short TRTs, estimated to be approximately 250–1000 nanoseconds. Lasers with extremely short pulse durations in the nanosecond (NS) or picosecond (PS) range are ideal to target this chromophore. Quality switched or “Q-switched” (QS) lasers emit pulses in the NS range, and PS lasers emit pulses in the PS range. In tattoos, the exogenous pigment particles are much smaller than melanosomes with correspondingly smaller TRTs. Therefore, while both QS lasers with pulse durations in the NS domain and PS lasers can be used, PS lasers provide a pulse duration with a better match to the TRT of the tattoo particles. Ho and colleagues found a pulse duration range of 10–100 PS allows for effective pigment destruction and clearance with little collateral damage to surrounding tissue. QS lasers produce rapid, pulsed bursts of energy in the NS range having both photothermal and photoacoustic effects to aid in breaking up of the pigment particles. PS lasers deliver ultrashort bursts of energy in the PS range, creating a rapid rise in temperature that results in a greater photomechanical effect with fragmentation of pigment particles. The rupture of pigment-containing cells triggers phagocytosis and the removal of pigment fragments via lymphatic drainage and scavenging by dermal macrophages. Unique histologic findings have been observed with the use of newer handpieces that fractionate the PS laser energy which may help to explain the added benefits for photorejuvenation, wrinkles and acne scars (discussed below). Tanghetti identified vacuoles, referred to as laser-induced optical breakdown (LIOB), through histologic and confocal imaging following PS laser treatment with a fractional lens array handpiece and believed these vacuoles to be responsible for stimulating repair mechanisms.
Over the past two decades, QS lasers have been the mainstay for treatment of pigmented lesions and tattoos. QS lasers used for pigmented lesions include the QS 694 nm ruby, the QS 755 nm alexandrite, and the QS Nd:YAG at 532 and 1064 nm. Melanin has a broad absorption spectrum throughout the ultraviolet, visible and near-infrared light range. Optimal wavelengths used to treat pigmented lesions would be those that are preferentially absorbed by melanin over oxyhemoglobin, another chromophore within the skin, and reach the targeted depth. Notably, absorption for melanin decreases and depth of penetration increases as the wavelength increases. Therefore, superficial pigmented lesions can be effectively treated with shorter wavelengths, while longer wavelengths are used for lesions with pigment deeper in the dermis. Longer wavelengths are also preferentially used in patients of darker skin types to decrease risk of post-procedural dyschromia as they have less epidermal damage. Likewise, for tattoos, given the location of the ink particles within the dermis, longer wavelengths are often preferred, although the appropriate wavelength also depends on the ink particle color.
Shorter wavelength long-pulsed lasers (millisecond domain) including the potassium-titanyl-phosphate (KTP) (532 nm) and the pulsed-dye laser (PDL) (585–595 nm) can also be used for superficial pigmented lesions because of their melanin absorption. They deliver laser energy over a longer pulse duration, in the millisecond range, with the same wavelengths as their QS counterparts. While the longer pulse duration may cause unacceptable nonselective thermal damage to deeper structures, they may be safely used for epidermal pigmented lesions. Longer wavelength long-pulsed lasers (millisecond domain) including ruby, alexandrite, and Nd:YAG lasers may also be used to treat larger pigmented targets in the dermis such as hair. Epidermal cooling is essential with these devices in order to protect the epidermis and dermal epidermal junction. One should not employ a millisecond domain long-pulsed laser to treat dermal pigment such as nevus of Ota or tattoo pigment.
In 2012, the US Food and Drug Administration (FDA) approved the use of the PS alexandrite laser for laser tattoo removal and the treatment of benign pigmented lesions. PS lasers have recently emerged as an even more targeted method of treating these lesions in comparison to the traditional NS domain QS lasers. The PS lasers with their incredibly short pulse duration, have a greater photomechanical effect as opposed to a photothermal effect within treated tissue, limiting collateral thermal damage to surrounding tissue. This is thought to allow for more efficient removal of pigment particles with decreased risk of post-procedural dyspigmentation. There is growing evidence that fewer treatments are required to achieve tattoo clearance with the PS lasers than with QS lasers. In addition, lower energies are used which help decrease the risk of epidermal and dermal-epidermal junction injury. Since the approval of the PS 755 nm alexandrite laser, a PS Nd:YAG (1064 nm and frequency-doubled 532 nm) has also been made available for commercial use. These new wavelengths allow for the treatment of the full spectrum of tattoo colors as well as a variety of epidermal and dermal pigmented lesions and are often the laser of choice for treating solar lentigines, melasma, dermal melanocytoses, amongst other pigmented lesions. PS lasers have been shown to be safe when used in patients with skin types III to VI; however, there remains a risk of post-procedural hypopigmentation and rebound hyperpigmentation with treatment, so caution should be taken whenever treating patients with darker skin types.
Recently, a variety of innovative optical attachments for PS lasers including the diffractive lens array (DLA) and the holographic microlens array (MLA) have been introduced that fractionate the laser beam by redistributing energy into multiple tiny high-density high fluence fractionated zones. These zones account for about 10% of the total treatment area, ensuring a significant safety profile. The DLA is often used for improving dyspigmentation (including melasma), skin texture, and fine wrinkles and is currently FDA approved for the treatment of fine wrinkles and acne scars. Similarly, the MLA has demonstrated efficacy for the treatment of fine wrinkles, atrophic acne scars, and rejuvenation based on recent studies.
Nonselective lasers can also be used to treat pigmented lesions. These include fully ablative lasers such as the 10,600 nm carbon dioxide (CO 2 ) laser, the 2940 nm erbium:yttrium-aluminum-garnet (Er:YAG) laser, and the 2740 nm yttrium-scandium-gallium-garnet (YSGG) laser. These lasers ablate or damage the epidermis and secondarily remove pigmented epidermal processes with the removal of epidermal melanocytes. While treatment with these lasers can produce excellent results, fully ablative laser resurfacing is often operator and technique dependent and the risk of postprocedural adverse effects including erythema, infection, dyspigmentation and scarring is higher than that of nonablative laser modalities. The 2940 nm Er:YAG laser has a greater absorption coefficient for water resulting in more superficial epidermal damage; therefore, leading to a better safety profile and shorter downtime than that associated with the CO 2 laser.
Fractional lasers (both ablative and nonablative) have also been used for the treatment of various pigmented lesions. Fractional photothermolysis, originally introduced in 2004 by Manstein and Anderson, involves the fractional emission of infrared light into microscopic treatment zones (MTZ) creating small columns of focal thermal injury within the skin. Each MTZ is surrounded by normal, undamaged tissue. Within each MTZ there is epidermal and dermal damage that stimulates collagen production and elastin formation. The degenerated dermal material results in the formation of microscopic epidermal necrotic debris (MENDs), which is then exfoliated. MENDs appear to serve as the transport medium for epidermal and dermal pigment across the epidermis, allowing for localized, controlled melanin release following fractional photothermolysis. Due to the presence of surrounding undamaged tissue that can aid in healing of the MTZ, there is a shorter associated downtime and decreased risk of adverse events compared to traditional ablative laser resurfacing. However, given the smaller degree (or percentage of surface area) of injury, a greater number of treatments are often required to achieve the desired results. Fractional photothermolysis has increasingly been used to treat a variety of pigmented conditions including melasma, solar lentigines, nevus of Ota, and postinflammatory hyperpigmentation (PIH). While fractional photothermolysis has shown benefit for many of these conditions, caution must be taken for deeper, dermal pigmentary processes due to the potential risk for rebound or worsening hyperpigmentation following treatment, especially in patients with darker skin types.
Intense pulse light (IPL) is a light-based device that emits filtered polychromatic light with wavelengths ranging from visible to near infrared (500–1200 nm), and therefore can also be used successfully to treat a variety of superficial benign pigmented lesions. These devices have pulse durations in the millisecond domain and therefore should be used with caution in patients with darker skin types due to increased risk of post-procedural pigmentary alterations and should not be used for tattoo removal due to increased risk of scarring. As these devices are not true lasers, they will not be discussed further in this chapter.
Check online ![]()
Prior to treatment of any pigmented lesion, it is important to obtain a thorough and detailed medical history including current medical conditions, allergies to anesthetics, and a current list of medications. If a patient is currently taking isotretinoin, laser therapy (especially those involving tissue ablation) should be delayed until the course of treatment has been completed due to potential risk of increased scarring and delayed wound healing. A history of isotretinoin use in the past 6 months, poor wound healing, PIH, keloid formation or bleeding diathesis would require caution during treatment due to the increased risk of prolonged recovery or scarring in any of these settings. A history of prior gold or silver use should be elucidated, as treatment with QS or PS lasers is contraindicated in this setting given the risk of chrysiasis—immediate and often irreversible darkening of gold-containing skin. Antiviral prophylaxis is appropriate in patients with a history of herpes simplex virus if treating near an outbreak site, especially if using ablative resurfacing lasers. A personal and/or family history of dysplastic nevi or melanoma should also raise caution prior to treatment of any pigmented lesion.
It is important to consider the patient’s skin type when treating pigmented lesions with laser devices. Patients should not be tanned when treated. Patients with darker skin types may be at increased risk of complications, particularly posttreatment dyschromia, and should be counseled appropriately. Lower fluences and longer wavelengths are preferred in patients with darker skin types to decrease the risk of subsequent hypo- and hyperpigmentation. In patients with darker skin types, pretreatment with hydroquinone 4% cream to hyperpigmented areas for 1 month and ceasing treatment 1 week prior to laser therapy is recommended. Topical corticosteroids for 3–4 days posttreatment can be used to prevent any pigmentary alteration secondary to the treatment-induced inflammation.
Realistic expectations regarding number of treatment sessions and treatment outcomes should also be established. Solar lentigines can often be successfully treated with just a few treatments; however, other pigmented lesions, like melasma, PIH, and nevus of Ota and Ito tend to be more difficult to treat, requiring multiple treatments and are associated with higher risks of incomplete clearance and rebound hyperpigmentation. Prior to tattoo removal, Kirby and colleagues published a scale to help physicians approximate the number of treatment sessions required for tattoo removal to help guide patients through the treatment process. Based on the scale, numerical values are assigned to six parameters: (1) Fitzpatrick skin type, (2) tattoo location, (3) tattoo color, (4) amount of ink in the tattoo, (5) scarring or tissue change, and (6) ink layering. The sum of the points for each parameter equate to the number of treatment sessions needed to successfully remove the tattoo, plus or minus 2.5. For patients seeking tattoo removal, it is also important to alert the patient that some tattoo pigment may remain after treatment and that hypopigmentation may occur in the treated area, creating a negative image of the original tattoo. Patients with skin types IV to VI and patients with a tan are at particularly increased risk for this outcome. The ideal patient for tattoo removal is an untanned patient with skin type I or II with a dark blue or black tattoo present for at least 1 year. Patients should be appropriately counseled regarding potential complications and adverse effects associated with treatment including post-procedural dyspigmentation, erythema, textural changes, and scarring. Pre-procedural photographs should be obtained prior to initiating therapy so that progress may be monitored during treatment.
Prior to use of a QS or PS laser, a history of gold or silver use should be elucidated, as treatment with QS or PS lasers is contraindicated in this setting given the risk of chrysiasis—immediate and often irreversible darkening of gold-containing skin.
Appropriate evaluation of the lesion to be treated is just as important as the patient evaluation. Evaluation of a pigmented lesion using a Wood’s lamp may be helpful to determine the depth of the pigment (i.e., epidermal, dermal, or mixed), as this will guide laser selection and provide implications for treatment outcomes. Prior to treatment of any pigmented lesion, it is critical that the lesion be accurately diagnosed. If any question or doubt exists regarding the nature of the lesion, a biopsy should be performed to confirm the diagnosis and to evaluate for and rule out malignancy. Lasers should never be used to treat any lesion concerning for melanoma or melanoma in situ. Additionally, the removal of dysplastic nevi with laser therapy is not recommended, despite studies showing no evidence of malignant transformation in laser-treated nevi.
Prior to treating any tattoo with a laser device, it is important to classify the tattoo as different types of tattoos have implications for the appropriate laser device as well as the number of treatments required. Tattoos can be classified as amateur, professional, cosmetic, medical, or traumatic. Amateur tattoos often contain lower concentrations of pigment and are located in various levels of the dermis. Professional tattoos generally contain dense pigment at the junction of the papillary and reticular dermis. Amateur tattoos typically contain pigment of unknown sources including ash, coal, or india ink, while professional tattoos are often composed of several ink pigments mixed together to create unique colors and shading. Commonly used pigments include cinnabar and cadmium red (red), cadmium sulfide (yellow), chromium salts (green), cobalt salts (dark blue), titanium dioxide (white), and iron oxide (red-brown or rust-colored) ( Table 3.1 ). Professional tattoos are often more difficult to remove with laser therapy due to the deeper and denser placement of the pigment and greater number of ink colors mixed together. Therefore, multiple laser modalities and several treatment sessions may be required for optimal clearance. Cosmetic tattoos, created using skin-colored tones typically contain iron oxide or titanium dioxide, are important to distinguish because of the unique risk of paradoxical darkening after QS or PS laser treatment (discussed below). Medical tattoos like those used as radiation markers are also important to distinguish. Traumatic tattoos are those that occur following a trauma or injury. It is important to understand the nature of the injury, so that the type of material implanted into the skin can be identified prior to laser therapy. Treatment of traumatic tattoos caused by fireworks with QS or PS lasers is contraindicated due to the rare risk of microexplosions of the remaining particles upon laser impact leading to cavitation and potentially atrophic scarring.
| Tattoo Color | Pigment Source |
|---|---|
| Black | Iron oxide, carbon, india ink, lead, gunpowder |
| Blue | Cobalt |
| Green | Chromium oxide, malachite green |
| Violet | Manganese violet |
| Yellow | Cadmium sulfide, ochre |
| Red | Mercuric sulfide (cinnabar), azo dyes, cadmium selenide, sienna |
| White | Titanium dioxide, zinc oxide |
| Brown | Ochre |
In addition to identifying the type of tattoo, it is essential to evaluate the ink colors within the tattoo, as there are optimal wavelengths for different tattoo ink colors ( Table 3.2 ). Depending on the colors within a tattoo, several devices with different wavelengths may be required to effectively treat the entire tattoo. Additional aspects that are important to consider include size and age of the tattoo. Smaller tattoos will typically require fewer treatment sessions to achieve clinical improvement. Older tattoos often require fewer treatments due to a degree of ink migration and clearance via lymphatics that has already occurred over time. Treatment should be delayed in the setting of inflamed tattoos, the presence of overlying infection or a concomitant active dermatologic disorder. Treatment in these situations may worsen the underlying condition, resulting in slow postoperative healing or increasing the risk of scarring.
| Laser and Wavelength | Black | Blue | Red | Green | Yellow |
|---|---|---|---|---|---|
| QS 694 nm ruby | X | X | X | ||
| QS 1064 nm Nd:YAG | X | X | X | ||
| QS 650 nm Nd:YAG | X | ||||
| QS and PS 755 nm alexandrite | X | X | X | ||
| QS and PS 532 nm Nd:YAG | X | X |
Ocular safety is a primary concern with the use of all laser systems, including pigment-specific lasers, due to the risk of iris and retinal injury. Laser light in the visible to near infrared spectrum (400–1400 nm) are part of the “retinal hazard region” and all personnel in the room during treatment must wear protective goggles. Regardless of the location on the body being treated, the patient should be given fully protective wrap-around goggles with the appropriate optical density and wavelength ranges of protection for the given laser wavelength to be worn throughout the entirety of the procedure. Laser aids, disposable adhesive eye protectors, can alternatively be utilized during treatment with nonselective, nonablative fractional lasers, which cover predominantly the upper eyelid while allowing access to the brow and infraorbital region. Additional precautions must be taken if treatment of the periorbital area near the eyelid margins or on the eyelid itself is anticipated. In these settings, a metal corneoscleral protective lens shield must be placed prior to treatment and all pulses should be fired in a direction away from the eye. It is important to note that ocular protection devices do not eliminate risk of injury. A recent review reported that eye injury occurred in 33% of cases in which eye protection including metal corneal shields were provided, likely associated with overheating of the metal corneal shields during the procedure. Therefore, other preventative measures including pulling the infraorbital skin away from the orbit during treatment and directing the laser away from the eye should also be employed to minimize complication risk. In addition, sufficient cooling of the treated area between pulses should be ensured during treatment to prevent overheating of the metal corneal shields and subsequent thermal injury.
Additionally, reflective surfaces and windows should be covered and access to the procedure room should be limited during treatment. Potentially flammable materials should be removed. Since QS and PS lasers may cause some tissue and blood splatter, protective plastic cones attached to the handpiece can be used to protect against any potential splatter.
Ocular safety is paramount for all personnel and patients in the room during laser therapy given QS and PS lasers can cause permanent retinal damage with vision loss without proper eye protection. The laser goggles used must have lenses with an optical density (OD) that block the specific wavelength being used. The lenses should provide an OD of at least 6.
Special precautions must be taken when using QS or PS lasers in the periorbital area, near the eyelid margins, or on the eyelid. A metal corneoscleral protective lens shield must be placed prior to treatment to protect the globe. First, two drops of ophthalmic tetracaine are instilled onto the conjunctiva. Then, a thin coat of ophthalmic erythromycin ointment is applied to the concave surface of the eye shield. To insert the shield, the lower lid is retracted, the patient is asked to look up, and the lower edge of the shield is inserted interior to the lower eyelid. Next, the patient is asked to look down, and the upper edge of the shield is inserted interior to the upper lid.
The area to be treated should be thoroughly cleaned and free of any make-up, personal care products or topical anesthetics, as these products can cause scatter of the light energy and prevent optimal delivery of the laser energy to the target. Additionally, various topical products remaining on the skin surface may contain ingredients with the potential to ignite when combined with the laser energy. If alcohol is used to clean the treatment area, it must be completely dried and no longer present prior to treatment.
Typically, laser devices utilized for the treatment of pigmented lesions are well-tolerated and neither infiltrative nor topical anesthesia is required. However, the location, size and depth of the lesion as well as the individual patient’s pain threshold should be taken into account when determining the need for pre-procedural anesthesia. Removal of pigmented lesions and tattoos can be quite painful, especially if a large treatment area is anticipated. In the authors’ practices, neither topical nor infiltrative anesthesia is routinely used for the treatment of lentigines and photodamage with QS or PS lasers. Local anesthesia is recommended prior to the treatment of larger tattoos or lesions with significant amounts of dermal pigment, or when ablative or nonablative fractional lasers are used. Compounded topical anesthesia offers a highly effective vehicle for pain management. Commonly used formulations include BLT (betacaine, lidocaine, and tetracaine at 7% concentrations), commercial preparations, such as LMX-4 or EMLA, 30% topical lidocaine, or mixture of 23% lidocaine/7% tetracaine. A thin layer of product is spread evenly over the treatment area and left in place for 45–60 minutes. Occlusion or the application of warm towels over the area can be used with lower-strength topical formulations to enhance the penetration of the anesthetic. However, extreme caution should be taken if the area is large, or if more potent (higher concentration) formulations are used as topical anesthetics can produce systemic toxicity. The applied anesthetic should always be completely removed prior to treatment. For medium and large tattoos, the area is often injected with 1% lidocaine with epinephrine.
Prior to treatment informed consent must be obtained after a thorough discussion of the procedure and its associated potential adverse effects. Pre-procedural photographs should be obtained prior to initiating therapy so that progress may be monitored during treatment.
When using an NS or PS laser for the treatment of pigmented lesions or tattoos, the initial desired endpoint is immediate tissue whitening or graying, which reflects cavitation of melanin or pigment particles and heat-induced gas bubble formation. The gas bubbles scatter visible light creating a white color, which may be less vivid after treatment of dermal pigmented lesions. The immediate skin whitening blocks most light from penetrating through it and gradually resolves over 20–30 minutes leaving mild residual erythema. If immediate tissue whitening is not observed following laser therapy, the laser exposure or treatment settings (i.e., laser fluence) were likely not sufficient for effective clearing of the treated pigmented lesion. At fluences below threshold, paradoxical hyperpigmentation may occur due to stimulation of melanocytes. At fluences above threshold, thermal burns with tissue sloughing, prolonged wound healing, hypopigmentation, hyperpigmentation, textural changes, and scarring can result.
Darker skin has a lower threshold for tissue whitening and a greater risk of dyschromia following laser therapy. Therefore test spots with lower fluences in darker skinned patients are recommended prior to treatment of pigmented lesions or tattoos to evaluate for hypopigmentation and hyperpigmentation. Treatments are typically performed at 4- to 6-week intervals or 6- to 8-week intervals for pigmented lesions and tattoos, respectively, although shorter intervals depending on the lesion treated may be effective. The number of treatment sessions required varies based on the lesion to be treated.
Pigmented lesions may vary in the amount, depth, and density of melanin distribution. These variations can affect the efficacy of certain laser devices and response to treatment. Lesions can be classified based on the distribution of melanin within the epidermis or dermis, which is important to consider when selecting the appropriate laser modality for treatment.
Epidermal lesions contain pigment primarily within the epidermis. In addition to NS and PS lasers that specifically target pigment, any modality that damages or removes the epidermis such as the ablative CO 2 or Er:YAG lasers will lead to removal or improvement of these lesions. Fractional laser resurfacing, both ablative and nonablative, has also been shown to improve epidermal processes (i.e., photodamage, lentigines).
Lentigo simplex is an evenly pigmented, tan to brown macule that can occur on both cutaneous and mucosal surfaces. These lesions are not associated with sun exposure and often occur in children. They can also occur in the setting of specific syndromes including LEOPARD syndrome, Carney complex, Peutz-Jeghers syndrome, and Laugier-Hunziker syndrome. Solar lentigines present as tan macules or patches often on the face, shoulders, dorsal forearms and hands of adults in the setting of chronic sun exposure. Ephelides, or freckles, are tan to brown macules occurring on sun-exposed sites and often present early in childhood. These lesions are most prominent during the summer months and fade during the winter months. While physical modalities including chemical peels and cryotherapy treatments are used in clinical practice, laser therapy has been shown to be more effective than both of these modalities. Any laser that damages the epidermis will lead to improvement in epidermal pigmented lesions with one or two treatment sessions. The mainstay lasers for these lesions are pigment-selective QS or PS lasers including the QS or PS 755 nm alexandrite, QS or PS 532 nm Nd:YAG, and QS 694 nm ruby lasers. Millisecond domain lasers and IPL devices can also be very effective in removing epidermal pigmented lesions.
NS domain QS lasers have been used to treat pigmented epidermal lesions for decades. Lasers with shorter wavelengths appear to more effectively treat epidermal lesions due to their high absorption of melanin. The QS 532 nm Nd:YAG, the QS 694 nm ruby laser, and the QS 755 nm alexandrite laser have consistently demonstrated efficacy in treating solar lentigines and lentigo simplex ( Fig. 3.1 ). While studies are more limited when evaluating the use of these devices for ephelides, the QS 755 nm alexandrite and QS 532 nm Nd:YAG lasers have demonstrated efficacy for these lesions with only one to three treatment sessions required. However, treatment outcomes for ephelides tend to be unpredictable. QS lasers have been shown to be relatively safe in most patients, although, there may be a slightly increased risk of PIH, especially in patients with darker skin types.

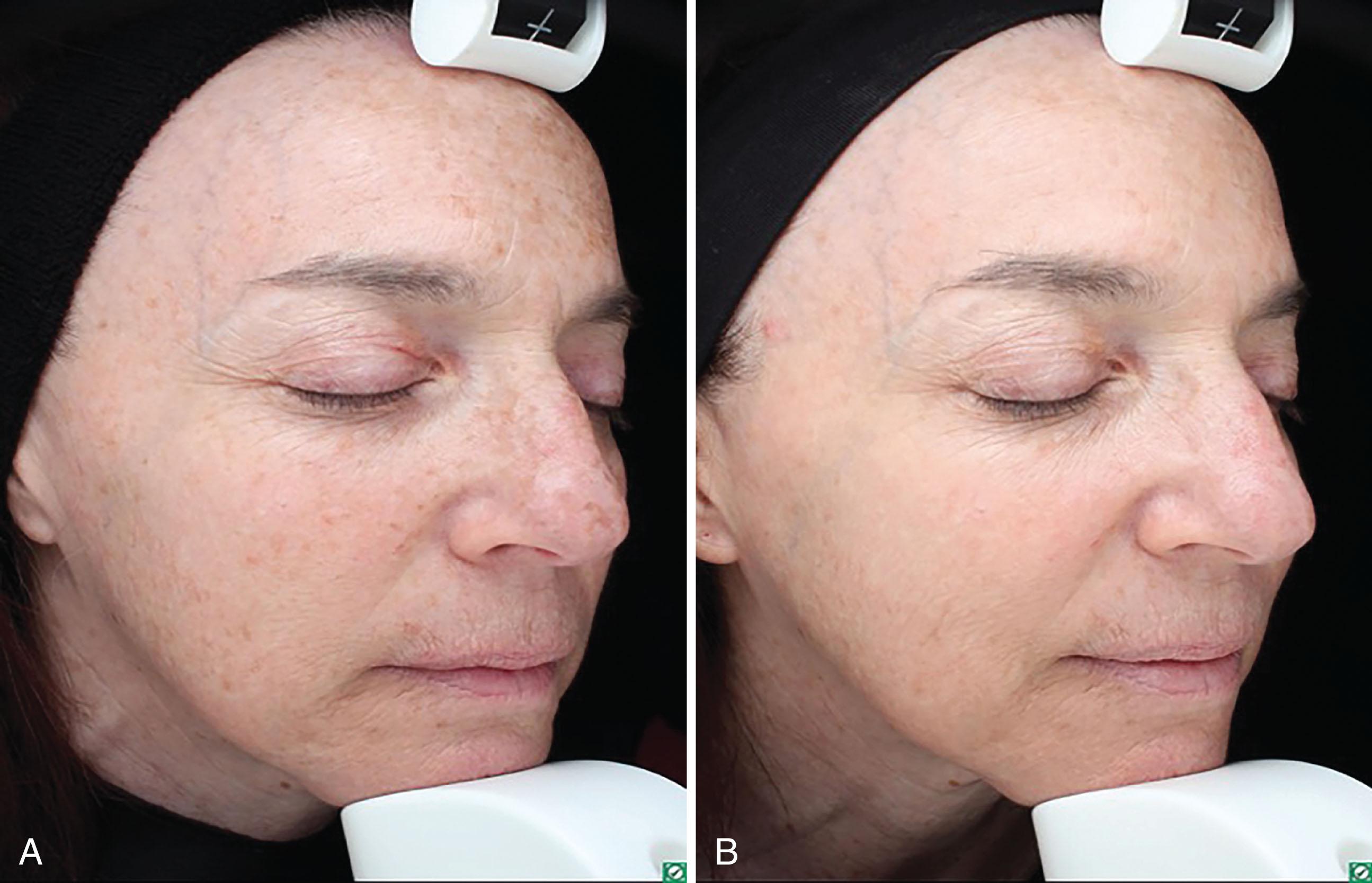
PS lasers have relatively greater photomechanical effects as opposed to the purely photothermal effects of NS domain lasers, resulting in lower energy fluences and reduced number of treatment sessions required compared to NS laser for similar clinical outcomes and possibly better safety profiles. Through histologic evaluation of laser treated skin, Negishi and colleagues observed destroyed melanosomes with surrounding structural damage after QS Nd:YAG laser treatment, whereas no surrounding structural damage was observed in PS laser treated skin samples. These same investigators treated 20 Asian females (skin types III–IV) with the 532 nm frequency-doubled PS Nd:YAG laser for lentigines and observed 93% of lesions achieved over 75% clearance after a single treatment. PIH was observed in only 4.65% of subjects. Similar studies have demonstrated low rates of postprocedural dyschromia (0.8%) following PS laser therapy. In a retrospective review, Levin and colleagues compared the safety and efficacy of the QS 694 nm ruby and the QS (532 and 1064 nm) Nd:YAG lasers with the PS 755 nm alexandrite for the treatment of pigmentary disorders including solar lentigines in patients with skin of color. All eight patients treated with the PS laser achieved 50% clearance and all associated adverse effects were mild and transient. Permanent dyspigmentation was noted in several subjects that underwent QS NS laser treatments. The PS alexandrite laser with the DLA has also demonstrated efficacy and safety, most notably for photoaging and solar lentigines, even when shorter treatment intervals were used ( Fig. 3.2 ). Novel PS lasers including the 730 and 785 nm PS lasers have similarly demonstrated efficacy for epidermal pigmented lesions, although studies are limited, and these devices are not yet widely available.
Long-pulsed lasers including the long-pulsed 755 nm alexandrite, long-pulsed PDL, long-pulsed 532 nm Nd:YAG, have also been used to effectively treat epidermal pigmented lesions and are proposed to be safe even in patients with skin of color. In a comparative study, Chan and colleagues utilized QS and long-pulsed 532 nm Nd:YAG lasers for treating lentigines in Asian skin, with both modalities demonstrating similar efficacy. However, treatment with QS lasers was associated with a significantly higher risk of PIH compared to long-pulsed lasers. Similarly, Ho and colleagues found no statistically significant difference in the efficacy of QS compared to the long-pulsed alexandrite laser, although PIH was found to be higher in Asian skin after QS laser therapy (22% for QS vs. 6% for long pulsed).
Fractional photothermolysis can be considered for these conditions if lesions are widespread, as in the case of photodamage. Ablative fractional resurfacing has demonstrated significant improvement in solar lentigines and photodamage. However, the significant clinical improvement comes with a greater risk of adverse effects and a longer downtime when compared to fractional nonablative resurfacing or pigment-selective laser therapy. The nonablative 1550 nm fractional erbium-doped fiber laser and the 1927 nm thulium fiber laser have both demonstrated efficacy in improving pigmented epidermal lesions and photodamage. The 1927 nm thulium fiber laser has a 10 times greater absorption coefficient for water and is therefore absorbed more superficially and has a greater ability to target epidermal processes. In 2010, consensus recommendations were established for the use of the 1550 nm fractional nonablative laser. The panel recommended three to five treatment sessions at 1-month intervals using fluences of 10–20 mJ and treatment levels of 7–11 for lighter skin and 4–7 for darker skin. In general, fractional nonablative laser resurfacing can lead to significant improvement in pigmented epidermal lesions with a shorter downtime and decreased risk of adverse effects when compared to ablative laser resurfacing. However, multiple treatments are typically required for optimal outcomes. There are limited studies on the use of fractional photothermolysis for the treatment of ephelides.
Overall, solar lentigines appear to be very effectively treated with millisecond, NS, and PS lasers, often only requiring one or two treatment sessions. These devices are typically preferred for significant, larger, and discrete lentigines. Darker lesions have more target for absorption and have greater clearance and lower fluences can be used with shorter pulse durations and no cryogen cooling. Recent studies suggest that PS lasers may be a safer alternative, especially in darker skinned patients. When treating multiple lesions or large areas, treating a full cosmetic unit with a fractionated laser is often beneficial. In clinical practice, lesions that achieve complete clearance with treatment rarely recur, although, new lesions may appear, and partially treated lesions may darken after UV exposure. Counseling the patient on diligent sun protection and proper skin care following the procedure are important for optimal long-term results.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here