Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patients with Crohn disease (CD) who have failed to improve with medical therapy and whose symptoms are secondary to a focal area of disease that can be resected should be considered for an operation. The clearest indications are the emergent presentations of perforation or obstruction. However, the far more common reasons for an operation are elective and require deliberation and shared decision making between the family, surgeon, and gastroenterologist. These include chronic pain, partial obstruction, and an overall decrease in quality of life from fatigue and failure to thrive. CD typically has an insidious onset. As a result, patients adjust to the slowly developing symptoms and often convey a less concerning clinical picture. Because of the slowly developing partial obstruction, patients may not report decreased appetite or early satiety, so particular attention should be directed at their weight changes, growth charts, and delayed puberty. Also, the physical exam should be directed at noticing tympany and high-pitched bowel sounds. When the pattern of symptoms and findings suggest that an operation will improve their quality of life and symptoms, imaging should be used to confirm disease focality that would make an operation feasible and reasonable. The best evaluation of the bowel is with magnetic resonance enterography, which will show areas of bowel wall thickening and provide the ability to assess peristalsis with cine images. Most frequently, the disease involves the terminal ileum (TI) with variable involvement of the ileocecal valve, cecum, and right colon. In some cases, colonoscopy may be useful for diagnostic purposes and to evaluate the ileocecal valve. However, the extent of disease in this region will not change the approach.
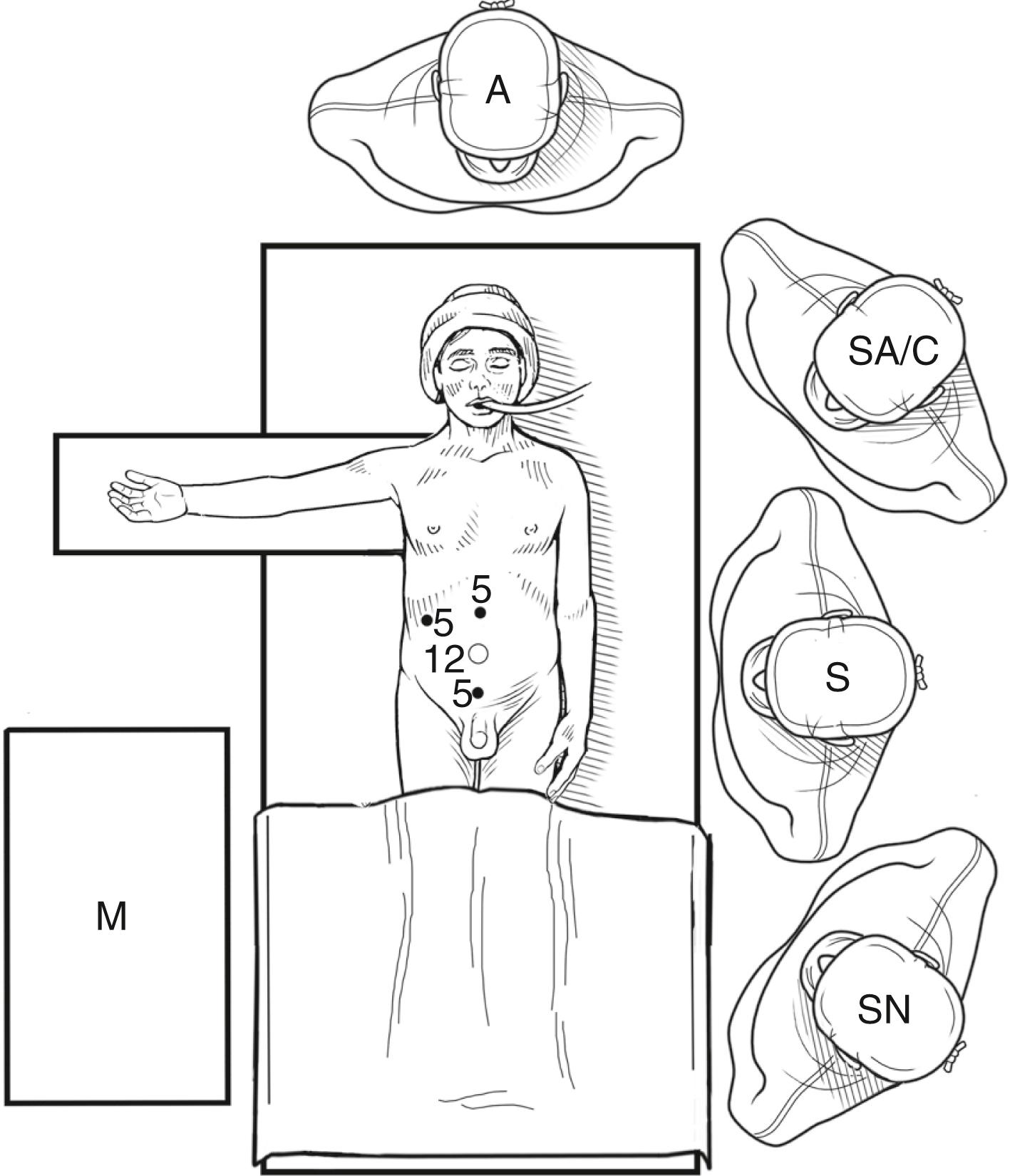
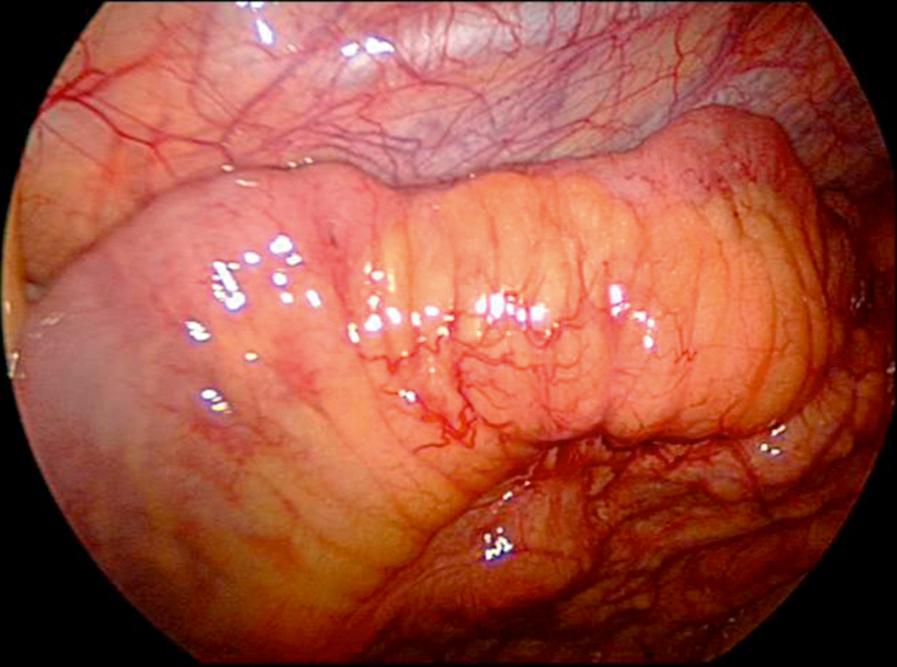
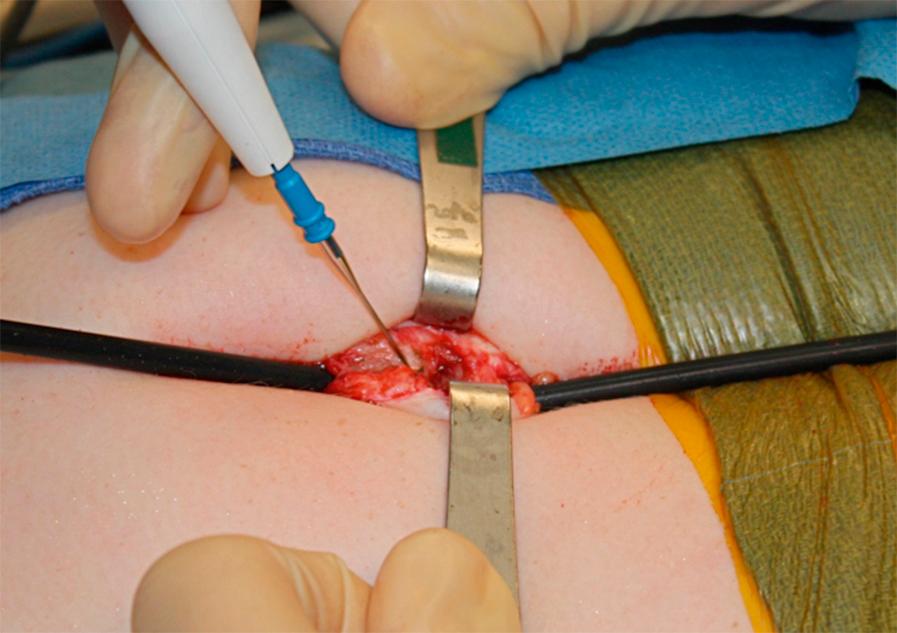
The patient is positioned supine on the operating table. The arms can be tucked, and both the surgeon and assistant are situated on the patient’s left side ( Fig. 8-1 ). The viewing monitor is placed on the right side of the table. A routine skin preparation is performed. Neither a nasogastric tube nor a urinary catheter is utilized routinely. The traditional laparoscopic approach can be performed with a camera port in the umbilicus and two 5-mm operating ports positioned in the midepigastric and suprapubic areas. This allows for complete mobilization of the right colon. A fourth 3- or 5-mm instrument can be used if needed. Usually the inflamed area is exteriorized through the umbilicus for extracorporeal resection and anastomosis. Since the ultimate length of the incision is determined by the size of the inflammatory mass, we utilize this enlarged umbilical incision up front in the form of a single-incision laparoscopic approach. This is done by making an incision through the umbilicus and extending about 1 cm above and 2 to 3 cm below the umbilicus. This umbilical incision can be smaller if the ileocecal valve is not being resected. A 5-mm port is placed through the center of the umbilicus for the camera and stab incisions in the fascia are used to insert the two working 5-mm instruments ( Fig. 8-2 ). Either these can be positioned on opposite sides of the 5-mm umbilical cannula or, occasionally, when a longer incision is used to start because of thick right colonic disease, both can be inferior to the camera port. We usually use a Maryland dissector in the surgeon’s left hand and a bowel grasper in the right. Diagnostic laparoscopy is first performed to evaluate the area to be removed ( Fig. 8-3 ) and any other areas of disease and evaluated. Next, the cecum is mobilized, which can usually be done bluntly by tearing the peritoneal attachment. The dissection should be carried cephalad to include the hepatic flexure, which is important to mobilize to ensure the right colon can be exteriorized without tension. If the lateral colonic attachments are difficult to take down bluntly, we will use scissors in the left hand with monopolar cautery. Advanced technology is not necessary for this dissection. After colonic mobilization, it is important to ensure that the TI mesentery is mobilized to identify the loose areolar tissue under the ileal mesentery. This avascular plane is almost never involved with inflammation and serves as the key to mobilizing the TI in the face of a phlegmon and/or abscess. After mobilizing the TI and entire right colon, the bowel is firmly grasped at the cecum, near the TI. Next, we remove the camera and incise the umbilical facia between instruments, thereby creating a 4- to 5-cm umbilical incision ( Fig. 8-4 ). The bowel is then delivered through umbilical incision, which may require a little more extension of the incision to safely exteriorize the inflamed intestine ( Fig. 8-5 ).


With the diseased bowel eviscerated, we divide the ileum where the thickened bowel transitions to normal using an endoscopic stapler with a purple gastrointestinal (GI) triload. Next, we divide the mesentery in a straight line toward the cecal landing zone with vascular loads and transect the cecum with a GI load. The mesenteric defect is closed with running suture through the staple line to prevent bleeding or hematoma.
The stapled anastomosis is performed by opening the antimesenteric borders and firing two longitudinal deployments of the 45-mm GI loads. The second firing closes the now-common opening without concern about impinging on the anastomosis. The surgeons then clean the field and change gloves, and the transverse staple line can be oversewn prior to reducing the ileum and right colon back into the abdominal cavity. In the rare scenario of being able to save the ileocecal valve, a hand-sewn end-to-end anastomosis may be more technically feasible. After closing the fascia and skin, much of the incision is hidden within the umbilicus ( Fig. 8-6 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here